Red cheeks baby food allergy
Can Food Allergies Cause Redness for Baby? Ready, Set, Food!
Redness can be a symptom of a food allergy. But it could be another type of skin rash. Learn how to tell when redness is caused by a food allergy, and how to tell the difference between a food allergy reaction and other types of skin redness.
Redness can be a symptom of a food allergy. It’s often accompanied by other allergic reaction symptoms, like hives. If your child experiences redness and no other symptoms, it still could be a sign of a food allergy. But it could be another type of skin rash. Today, we’ll cover how to tell when redness is caused by a food allergy, and how to tell the difference between a food allergy reaction and other types of skin redness.
Redness from a Food Allergy
Like all other symptoms of a food allergy reaction, if a food allergy causes redness, it will appear seconds to minutes after someone eats the food they are allergic to, and almost always within two hours.
Most often, the redness caused by a food allergy will surround hives, also known as a food allergy rash. Hives are the most common symptom of a food allergy reaction. They are raised, itchy bumps that are usually red, and that are often surrounded by a red flare.
Hives tend to appear in clusters, and could appear anywhere on the skin. They could either appear in one concentrated area or all over the body.
Clusters of hives may cause skin areas to look blotchy. If areas of baby's skin look red and blotchy, check to see if parts of these blotches are raised. If they have raised areas, they are probably hives.
(Please read this article for more details on identifying a food allergy rash.)
But sometimes, food allergies cause skin redness without hives. This redness may appear around the mouth area, or on other areas of the face, because this is near where baby first came in contact with the allergen. If so,the red spots will also be itchy.
Someone’s nose may also turn red during a food allergy reaction. This will be accompanied by itchiness, and likely be accompanied by congestion.
And skin redness could appear on other areas of the body, usually with other food allergy symptoms.
If your child already has eczema, a food allergy reaction may cause the red, itchy rash of eczema to flare up, or get noticeably worse. However, food allergies don’t cause eczema to newly appear, and eczema flare-ups can be due to any number of causes.
Most concerningly, a food allergy reaction may cause swelling. If a food allergy causes swelling, it often causes redness in the swollen area, because of extra blood flow in the swollen area. Food allergies can cause swelling (and resulting redness) on the face, lips, eyes, or throat. Throat swelling and redness is a sign that an allergic reaction has turned severe.
How to know if a food allergy caused redness?
Even though food allergies cause these types of redness, redness on the face or elsewhere on the body doesn’t always mean that your child is experiencing a food allergy reaction.
Pay attention to:
- Whether your child is experiencing other symptoms of an allergic reaction, such as hives and vomiting
- Whether the redness (and other symptoms) appeared soon after your child ate a certain food---seconds to 2 hours after consumption
- Whether the redness looks, emerges, or behaves like another type of rash
- How long the redness lasts --- hives and other food allergy redness usually lasts several hours, up to a maximum of 24-48 hours.
Symptoms Of Food Allergies
If your child experiences redness along with other food allergy symptoms, they are probably experiencing a food allergic reaction.
Remember: symptoms of a food allergy appear seconds to minutes after eating a food, and almost always within 2 hours after eating a food.
Also, symptoms of a food allergy reaction can vary from one reaction to the next. So, if someone experiences hives or other redness during one reaction, that doesn’t mean that they’ll experience the same symptoms during future food allergy reactions.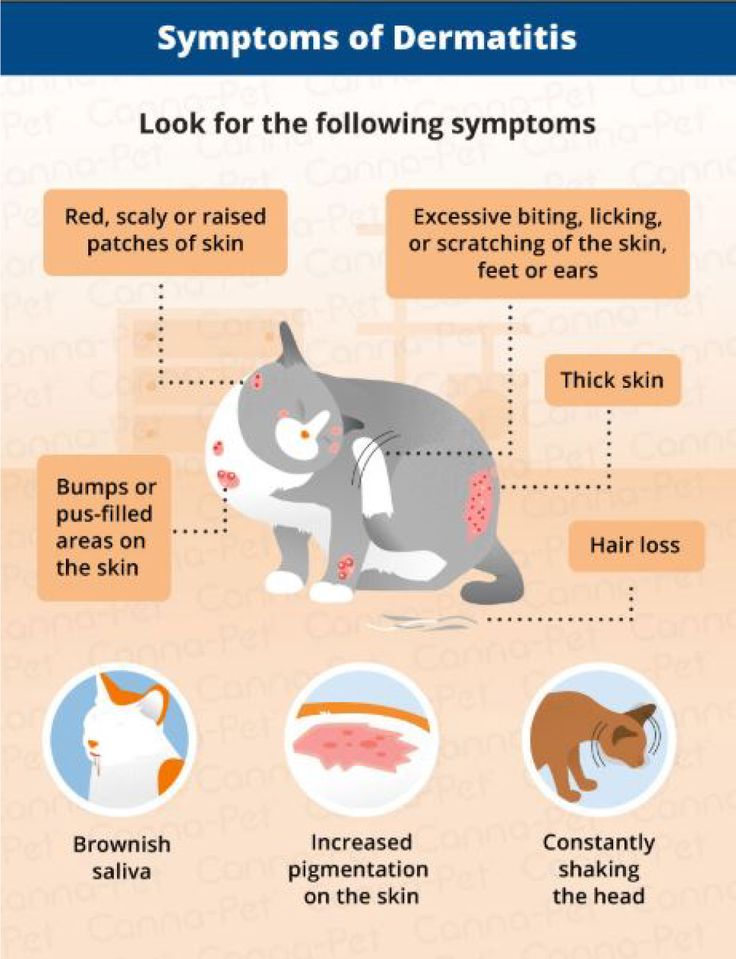
It’s also important to know whether a food allergy symptom is mild or severe, so you know how to respond. We’ve bolded the food allergy symptoms that usually involve redness below, so you can easily tell if they are mild or severe.
Mild food allergy symptoms
- Hives (raised, red itchy bumps) concentrated in one area of the body
- Skin redness in one area
- Red rash on the face
- Itchy, red, and watery eyes
- Swelling of the eyes, lips, or face (swelling may cause redness)
- Worsening eczema, if baby already has eczema (red skin rash)
- Occasional vomiting
- Itchiness
- Sneezing
- Congestion
- Some stomach pain
- Some nausea
- Mild coughing
How To Respond To A Mild Food Allergy Reaction
Stop feeding your child the food that you believed was the cause of the reaction.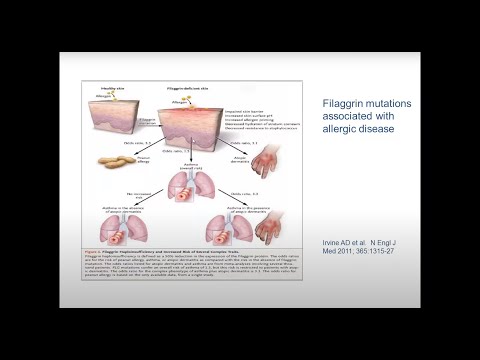 Then, contact your pediatrician or an allergist. If your doctor recommends a specific dose of antihistamine, you can give your child the antihistamine to treat a mild allergic reaction. Monitor your child closely, because there’s a chance that a mild allergic reaction could turn severe.
Then, contact your pediatrician or an allergist. If your doctor recommends a specific dose of antihistamine, you can give your child the antihistamine to treat a mild allergic reaction. Monitor your child closely, because there’s a chance that a mild allergic reaction could turn severe.
Severe food allergy symptoms
- Hives (raised, red itchy bumps) that spread to many areas of the body
- Swelling of the throat (may cause the throat to turn red)
- Tightness of the throat
- Difficulty swallowing
- Swelling of the tongue
- Difficulty breathing or shortness of breath
- Noisy breathing or wheezing
- Repeated, significant coughing
- Pale appearance
- Trouble vocalizing
- Change in voice or cry
- Repeated vomiting
- Diarrhea
- Dizziness
- Fainting
- Drop in blood pressure
- Rapid heartbeat
- Loss of consciousness
- Feeling floppy (only in infants and young children)
How To Respond When An Allergic Reaction Is Severe
When the symptoms of a food allergy reaction are severe and involve more than one organ system, this is known as anaphylaxis. Anaphylaxis can be life-threatening. Give epinephrine (use an Epi-Pen) immediately, and urgently call 911, if your child shows signs of anaphylaxis. Epinephrine is the only medicine that can stop anaphylaxis.
Anaphylaxis can be life-threatening. Give epinephrine (use an Epi-Pen) immediately, and urgently call 911, if your child shows signs of anaphylaxis. Epinephrine is the only medicine that can stop anaphylaxis.
The National Institute of Allergy and Infectious Diseases (NIAID) provides more information on food allergy symptoms and management:
Other Skin Conditions That May Cause Redness
If your child has redness on their face, but otherwise seems fine (with no other symptoms of a food allergy, such as hives and vomiting), they may have another type of skin rash or skin condition.
This is true even if the redness looks blotchy --- a red, blotchy rash that is not raised could be a type of eczema.
If baby has redness on their skin once, with no other symptoms, and the redness and other symptoms never return shortly after your child eats the same food, the redness is probably caused by something other than a food allergy.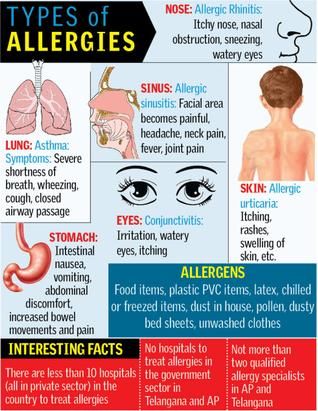
This is because food allergy reactions are consistent and repeatable. When someone has a food allergy, they will have some sort of allergic reaction symptoms every time they eat that food.
Here are some skin conditions that cause redness, and that are completely different from a food allergy reaction.
Eczema (Atopic Dermatitis)
Eczema (atopic dermatitis) causes baby’s skin to develop a red rash that is dry, rough, flaky, and itchy. An eczema rash usually appears on the face and skin creases, but could appear anywhere on the body. This rash may appear blotchy, but it will never have raised bumps (hives).
When baby’s skin is exposed to certain irritants, their eczema will flare up (become worse). Some irritants that could cause baby’s skin to flare up include soaps, detergents, dyes, fragrances, abrasive fabrics, and anything that causes the skin to dry out. If a baby has eczema and a food allergy, eczema could also flare up when they eat the food that they are allergic to.
Contact Dermatitis
Contact dermatitis flares up when the skin reacts to something it touches (including soaps, perfumes, lotions or poison ivy). It could show up as a red rash, blisters, or dry skin. It is considered a type of eczema, but it is different from atopic dermatitis. Contact dermatitis usually clears up when the skin irritant is removed.
Baby Acne
Baby acne appears as hard red bumps (pimples), sometimes surrounded by small red inflamed areas of the skin. It looks very similar to teen and adult acne. You may also see whiteheads on the bumps.
Baby acne usually appears on the face, neck, back, or upper chest. It’s never accompanied by any other symptoms, and doesn’t cause discomfort in the majority of cases.
There are two types of baby acne, and both present in the same way.
The first type is neonatal acne, and it is very common.Neonatal acne usually starts to develop between 2 and 4 weeks of age (but could develop any time before 6 weeks of age), and usually clears up by 4 months of age.
The second type of acne develops after six weeks of age, and is known as infantile acne. It is less common than neonatal acne. Infantile acne usually appears between 3 and 6 months of age, and clears up after several months to a year.
Both types of baby acne usually last for much longer than the typical food allergy redness lasts for.
Heat Rash
Heat rash suddenly appears on a child’s body when it’s hot outside. It looks like baby acne or a red, prickly rash. It will usually appear on areas of someone’s body that heat up most rapidly: the face, armpits, wrists, and legs. It may be itchy, but it won’t be accompanied by any other symptoms.
Early Allergen Introduction and Redness
The safest time to introduce your baby to allergenic foods is during their first year of life, as food allergy reactions in infants tend to be mild.
Research led by Dr. Jonathan Spergel (Head of Allergy, Children’s Hospital of Philadelphia) has shown that infants have far fewer reactions that require an Epi-pen than older children, and that no food allergy deaths have occurred in children under the age of one.
Our Chief Allergist and Board Certified Allergist Katie Marks-Cogan M.D, explains how early allergen introduction is inherently safe:
Ready, Set, Food! is an easy and safe way to start feeding your baby allergenic foods early. Most babies will not have an allergic reaction when introducing a new food, and the few reactions that do occur tend to be mild or moderate. This is consistent with research findings that show under age 1 is the safest time to introduce allergenic foods.
Still, if your baby shows signs of an allergic reaction soon after eating Ready, Set, Food!, including redness, talk to your pediatrician or an allergist for guidance. Even if you think your baby’s redness is from a food allergy, you can take comfort in knowing the reaction is likely to be mild.
--------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.
Does My Baby Have A Food Allergy Rash?
What is a food allergy rash, and what causes it? How do you know if your child has a food allergy rash? How to manage a food allergy rash, and how long does it usually last? We’ll cover everything families need to know about food allergy rashes in this definitive guide.
In our parent's guide to food allergy rashes, we'll answer the following most asked questions:
- What is a food allergy rash, and what causes it?
- How do you know if your child has a food allergy rash?
- What are the symptoms of a mild, moderate or severe allergic reaction?
- Where can food allergy rashes appear?
- How to manage a food allergy rash, and how long does it usually last?
- How do you test for a food allergy?
- How do you introduce allergens safely?
We’ll cover everything families need to know about food allergy rashes in this definitive guide.
What is a Food Allergy?
Normally, our immune systems protect our bodies from viruses, bacteria, and other foreign invaders that could harm us.
But when someone has a food allergy, their immune system mistakenly treats the proteins in a certain food (or foods) like these foreign invaders, and over-defends the body against these proteins. Their immune system makes special antibodies --- specific IgE antibodies --- that detect the food proteins and help fight them off.
These IgE antibodies trigger symptoms of an allergic reaction whenever the person eats a food they are allergic to. For example, if someone is allergic to peanut, they have IgE antibodies that detect and fight off peanut proteins, and that trigger allergic reaction symptoms (including a possible food allergy rash) whenever they eat peanuts.
Types of Food Allergic Reactions - Mild, Moderate, and Severe
Food allergy reactions can range from mild to severe, and can sometimes be life-threatening. Keep in mind, though, that a mild reaction can sometimes become severe. Also, symptoms of a food allergy reaction can vary from reaction to reaction. So, it’s impossible to predict what symptoms your child will develop each time they have an allergic reaction to food.
Keep in mind, though, that a mild reaction can sometimes become severe. Also, symptoms of a food allergy reaction can vary from reaction to reaction. So, it’s impossible to predict what symptoms your child will develop each time they have an allergic reaction to food.
Symptoms of a food allergy reaction usually occur seconds to minutes after someone eats a food they’re allergic to, and almost always occur within a few hours of eating the food.
Symptoms of a mild or moderate allergic reaction may include:- A food allergy rash concentrated in one area of the body (red, raised bumps)
- Redness in an area of the skin
- Vomiting
- Swelling of the face, eyes or lips
- Itchiness
- Itchy, watery eyes
- Congestion
- Sneezing
- Some stomach pain
- Some nausea
- Mild coughing
- Worsening eczema
- A food allergy rash that spreads to many areas the body
- Swelling of the tongue
- Swelling or tightness of the throat
- Repeated, significant coughing
- Wheezing/noisy breathing
- Difficulty breathing /shortness of breath
- Change in voice or cry
- Struggling to vocalize
- Difficulty swallowing
- Repeated vomiting
- Pale appearance
- Diarrhea
- Dizziness
- Fainting
- Drop in blood pressure
- Rapid heartbeat
- Loss of consciousness
- Feeling floppy (infants/young children only)
Signs Of Anaphylaxis
When the symptoms of a food allergy reaction are severe and involve more than one organ system, the reaction is classified as anaphylaxis.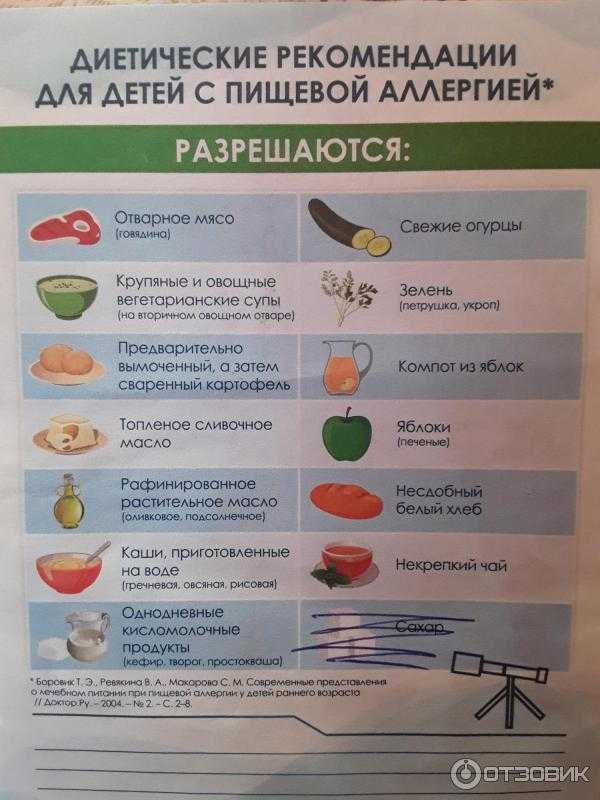 Anaphylaxis can be life-threatening. Call 911, and give epinephrine (use an Epi-Pen) immediately, if your child shows signs of anaphylaxis.
Anaphylaxis can be life-threatening. Call 911, and give epinephrine (use an Epi-Pen) immediately, if your child shows signs of anaphylaxis.
The National Institute of Allergy and Infectious Diseases (NIAID) provides more information on food allergy symptoms and management:
All About Food Allergy Rashes
A food allergy rash is the most common symptom of a food allergic reaction, especially in babies and children. It is also often the first symptom to appear (but not always). It could appear anywhere on the skin.
What does a food allergy rash look like?
A food allergy rash is raised, very itchy, and usually red or pink. It creates red, raised bumps on the skin. These bumps are usually rounded, and often have red flares around them. They are usually called hives, but are sometimes called wheals, urticaria or nettle rash.
They are usually called hives, but are sometimes called wheals, urticaria or nettle rash.
In people with darker skin, a food allergy rash will also appear as raised, itchy bumps. But often, the bumps do not appear red at all, and instead have the same color as the person’s skin is normally. You also probably won’t see red flares around the bumps. (In some cases, a food allergy rash may still have a subtle red hue, or a darker red hue, when it appears on a person with brown or Black skin.)
Why do food allergies cause a rash?When someone eats a food they’re allergic to, their IgE antibodies detect the proteins from that food. The IgE antibodies prime tissue cells (called mast cells) and blood cells to release a chemical called histamine, and other chemicals, as a way to defend against those proteins.
When the histamine and other chemicals get released, this causes blood vessels to widen (dilate) and become leaky. Fluids get released under the skin as a result, leading to inflammation under the skin. This leads to the raised food allergy rash on the skin.
This leads to the raised food allergy rash on the skin.
Food allergy rashes can be concentrated in one or two areas of the body, or can spread throughout the body.
Places that food allergy rashes often appear include the face, arms, hands, legs, feet, stomach area, and back. But they could appear anywhere on the skin.
Each individual bump (wheal) from the rash can be as small as a few millimeters or as large as several inches across.
But a rash area may be much larger, because food allergy rash usually appears as batches or clusters of bumps. And someone could develop multiple rash areas at a time.
If a food allergy rash is concentrated in one area, the food allergy reaction is mild. But if the rash spreads to many areas of the body, this is a sign of a severe allergic reaction.
How long does a food allergy rash last?Like other food allergy symptoms, a food allergy rash can appear seconds to hours after someone eats a food they're allergic to.
A food allergy rash usually lasts for several hours after food allergy reaction symptoms first appear. Sometimes, it can last for up to 24-48 hours.
Do all food allergy reactions produce a raised rash?Even though food allergy rashes are a common allergy symptom, they may not appear during every food allergy reaction. Sometimes, a food allergy can turn areas of the skin red and/or itchy, but won’t produce the raised food allergy rash (hives).
Also, a food allergy rash is different from the rash that eczema causes. But food allergies can make eczema rashes worse (cause eczema to flare up). Learn the differences between a food allergy rash and an eczema flare-up here.
How to Manage a Food Allergy Rash
If your child develops any food allergy rash (or any other food allergy symptoms), immediately stop feeding them the food that you believe was the cause of the reaction.
The other steps in managing a food allergy rash vary depending on how severe the allergic reaction is.
Managing a Mild Food Allergy Rash
How to manage mild food allergy rashes, concentrated in small clusters on one area of the body?
If a doctor has explicitly recommended a dosage of antihistamine, you can give your child the antihistamine (such as Benadryl or Zyrtec) to treat mild hives. Antihistamine helps stop the release of the histamine that triggered the rash, in the case of a mild or moderate allergic reaction.
If your doctor hasn’t recommended a dosage of antihistamine, call your pediatrician or allergist to alert them about the hives, and ask about next steps.
Either way, continue to monitor your child in case their mild allergic reaction turns severe.
Hydrocortisone cream may also help to relieve the itchiness of the rash, although it won’t make the rash go away.
Managing a Severe Food Allergy RashIf your child develops a significant food allergy rash all over their body, but no other symptoms of a food allergy reaction, call your doctor immediately.
Continue to monitor your child for other symptoms of a food allergy reaction, because if other severe symptoms emerge, your child will have anaphylaxis. If you have epinephrine (an Epi-Pen), give your child an injection. An antihistamine will not be able to stop this severe, widespread rash.
If your child develops a food allergy rash all over their body, and it’s accompanied by severe symptoms in at least one other organ system, your child is experiencing life-threatening anaphylaxis and needs emergency assistance.
Inject epinephrine (an Epi-Pen) immediately, and call 911. Epinephrine is the only medicine that can stop anaphylaxis --- antihistamines cannot stop this severe reaction.
A Note About Food Allergic Reactions and Children
Many people wonder about the differences between food allergy reactions in children vs. adults.
Food allergy rash is one of the most common food allergy symptoms in children and adults. The way it appears in every age group is also largely the same. In fact, food allergies generally cause the same set of symptoms in children as they do in adults.
In fact, food allergies generally cause the same set of symptoms in children as they do in adults.
But even though food allergies cause similar symptoms across all age groups, the most common types of food allergies are different in children vs. adults.
In young children (5 years of age and younger), cow’s milk, egg, and peanut allergies are the most common food allergies. According to one study by Dr. Ruchi Gupta, these three foods are responsible for around 80% of food allergies in young children.
In addition to milk, egg, and peanut allergies, tree nut allergies are also very common in children age 14 and under.
Out of these four food types, peanut and tree nut allergies are most responsible for severe reactions in children, but any food has the potential to cause a severe reaction.
In contrast, the most common food allergy in adults is shellfish allergy, which is largely an adult allergy. Finned fish allergies are another common adult allergy --- and finned fish allergies also tend to develop in adulthood.
Check out our previous article for more on food allergies in children vs. adults.
Food Allergy Testing
If your child develops a rash after they eat a certain food, and it looks similar to the food allergy rash we’ve described above, remember that food allergy testing is the only way to determine whether your child truly has a food allergy. So, it’s best to make an appointment with an allergist for testing.
Food allergies can be diagnosed through three types of tests: a skin prick test, a blood test, and an oral food challenge.
A skin prick test: An allergist pricks your child’s forearm with a needle containing food protein from the suspected problem food. Then, they monitor your child to see if an allergic reaction develops around the area where their skin was pricked.
A blood test: An allergist checks your child’s blood for IgE antibodies that respond to certain food proteins.
An oral food challenge: Your child eats small amounts of the suspected problem food under an allergist’s supervision, to see if they develop an allergic reaction. This is the most accurate way to diagnose a food allergy.
This is the most accurate way to diagnose a food allergy.
Introducing Allergens Safely
New clinical guidelines recommend introducing babies to common allergy-causing foods during their first year of life, as a way to help them safely enjoy these foods in the future.
As the U.S. Department of Agriculture (USDA) recommends in their new dietary guidelines, “Potentially allergenic foods (e.g., peanuts, egg, cow milk products, tree nuts, wheat... and soy) should be introduced when other complementary foods are introduced to an infant’s diet.”
Ready, Set, Food! can help you easily and safely introduce these common allergy-causing foods to baby, following the new clinical guidelines. And since the first two stages of our system fully dissolve into a bottle of breastmilk or formula, you can start introducing your baby to peanut, egg, and milk as early as 4 months of age, even before they’re ready for solids.
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.
Why a child has red cheeks and how it is connected with teeth: doctors answer
Why a child has red cheeks
As explained by the pediatrician of JSC "Medicina" (clinic of Academician Roitberg), a member of the Union of Pediatricians of Russia Maryam Sayfulina, hyperemia of the cheeks (red blush) - this is not necessarily a sign of the disease:
“In children, flushing of the cheeks may occur as a result of overheating or hypothermia. Often, even at a temperature of -10°C/-15°C, especially in windy weather, the tender cheeks of babies can turn red and become rough. nine0005
However, redness may appear on the child's cheeks regardless of temperature conditions. Many parents note that children have red cheeks when eating certain foods.
Many parents note that children have red cheeks when eating certain foods.
Pediatrician confirms that skin manifestations of this nature often depend on the diet of the child. So, the causes of redness on the cheeks of a child may lie in allergies.
From dry air to allergies and adenoids: why babies sleep with their mouths open
About why a child sleeps with his mouth open, why it can be dangerous...
September 24 16:27
“In 80% of cases, cheek hyperemia in a young child is associated with an allergic mood in the form of diathesis. Allergic mood can manifest itself even in children who are breastfed. For example, if a mother ate foods that can provoke an allergic reaction, such as an orange or orange juice, then the child's cheeks may turn red. Here you need to pay attention and talk with parents in order to refrain from eating red, orange, citrus products,” warns Maryam Sayfulina. nine0005
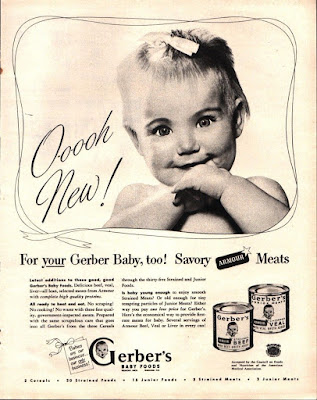
The pediatrician indicated that formula-fed cow's milk protein can also cause redness on the baby's cheeks. However, the doctor emphasizes that it is not at all a matter of special formulas for feeding, because they are, as a rule, adaptive and hypoallergenic:
However, the doctor emphasizes that it is not at all a matter of special formulas for feeding, because they are, as a rule, adaptive and hypoallergenic:
“As soon as new complementary foods and mixtures are introduced after six months, the child may develop flushing of the cheeks. This is due to the fact that many products contain cow's milk protein, and this is one of the main causes of hyperemia, dry skin, peeling and roughness on the cheeks. nine0005
One of the main reasons why a child has red cheeks is an allergy to cow's milk protein. Therefore, when a child is bottle-fed, we recommend parents to exclude products containing cow's milk protein from the child's diet.
In addition, according to Dr. Saifulina, similar skin manifestations can be observed in children with constipation, since with irregular emptying of the intestine, toxins from it are absorbed back into the blood, and this is reflected in the structure and color of the skin, including the cheeks. nine0005
As explained by the pediatrician, contact dermatitis can also cause reddening of the child's cheeks.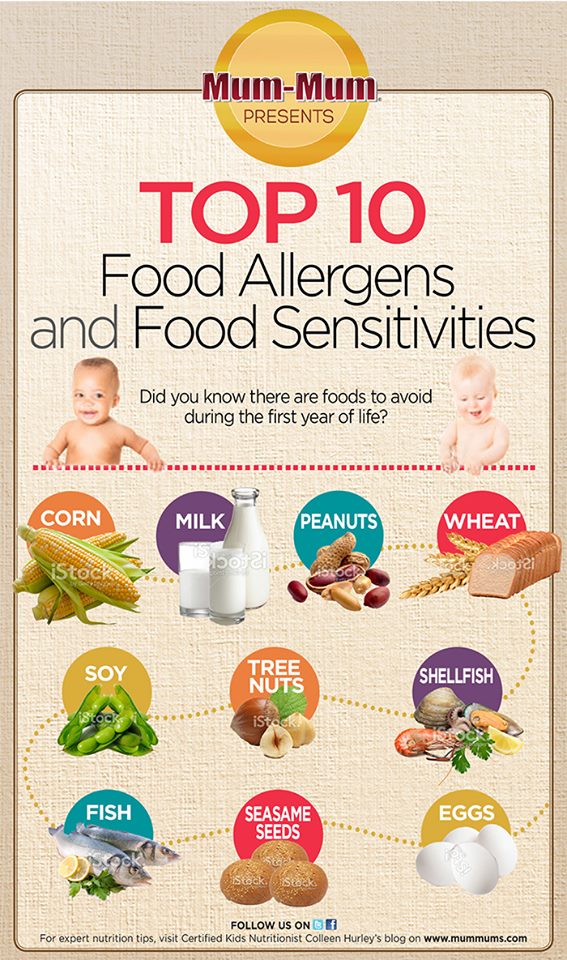 For example, hyperemia can be provoked by touching a pillowcase or linen after washing with a new powder, if it turned out to be allergenic.
For example, hyperemia can be provoked by touching a pillowcase or linen after washing with a new powder, if it turned out to be allergenic.
close
100%
“Sometimes there is a respiratory allergy that can occur on pets - dogs, cats, or fish food. This allergic reaction is manifested not only by nasal congestion, but also by reddening of the cheeks, ”explains Maryam Sayfulina. nine0005
If redness appears on the child's cheeks, the pediatrician recommends that parents consult a doctor, because this is not always the result of overheating, hypothermia or allergies. In some cases, such a symptom may hide a serious disease, for example, a pathology of the cardiovascular system.
The doctor noted that in some cases in children, flushing on the cheeks may accompany an infectious disease (viral or bacterial). With elevated body temperature or with the manifestation of intoxication (for example, with intestinal infections, loose stools, vomiting may be observed). In such cases, it is necessary to consult a doctor. nine0005
In such cases, it is necessary to consult a doctor. nine0005
Why cheeks turn red during teething
Anna Pyatibratova, pediatric dentist at SM-Dentistry warns parents that teething in a child may be accompanied by reddening of the cheeks:
“The age of the first teeth eruption is six months. The last teeth erupt at two and a half years. But these are averages and everyone is individual. However, as a rule, at about six months, parents may notice that the child's cheeks are reddened. Behind this symptom, teething may be hidden. nine0005
Most often, reddening of the skin of the chin and cheeks occurs due to the active work of the salivary glands or prolonged mechanical impact.
When teething, the gums begin to itch, and the child tries to eliminate severe itching. He sucks his fingers, fists, which increases salivation. The flowing saliva dries up on the skin, causing it to become irritated, cracked and red.
From incorrectly selected glasses to a tumor: why a child has a headache
About why children have a headache, what drugs are allowed to use. ..0005
..0005
September 03 09:29
However, the causes of redness on the cheeks of a child can be varied. Parents are interested in how this symptom is not confused, for example, with an allergy.
“When teething, we always pay attention to the gums. It is enlarged, swells, reddens. Sometimes an erupting tooth is visible through it. If the child does not have concomitant diseases and you did not give a new product on the eve of the appearance of redness, most likely we are dealing with teething, ”explains Dr. Pyatibratova. nine0005
close
100%
How to smear red cheeks in a child
Allergist-immunologist Elena Guchapsheva explains that the decision will depend on the reason why the child has red cheeks:
it can be attributed to the influence of external factors - such as cold and heat, increased salivation. In young children, thermoregulation is imperfect and requires correction.
The doctor gives advice on how to act if the child has skin manifestations due to the ambient temperature. nine0005
nine0005
- If the child is hot, he should be dressed in lighter clothes, preferably made of natural fabrics that allow air and moisture to pass through.
- If the child is cold, he needs to be warmed up. At least 20-40 minutes before going out, apply a protective cream to exposed areas of the body. There are many of them on the market, many are marked cold. The main thing is to take into account age indicators when choosing a remedy. For children's skin, for example, Morozko, Rosy Cheeks, Mustella cold cream, Avene cold cream, Uriage Barrierderm, Libre derm cold cream, Vitex winter care (winter care) are suitable. nine0005
According to Elena Guchapsheva, teething can lead to increased sensitivity of the skin:
“Profuse salivation and itching of the gums lead to irritation of children's skin. If parents see dryness, then moisturizing baby creams can be used (for example, Bepanten, D-panthenol, Lipobase baby cream), if the skin is wet, then preference should be given to zinc-containing creams (for example, Zinocap, Cynovit ”, “Tsindol”).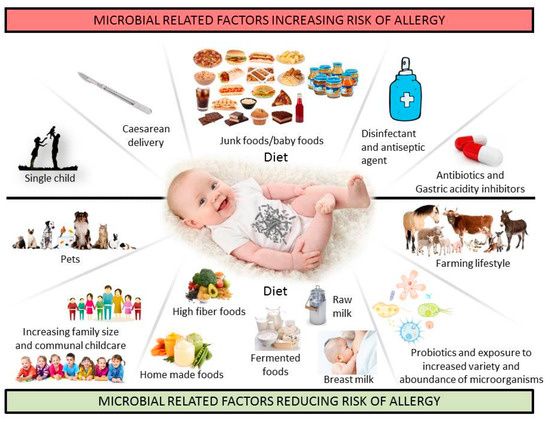
From taking vitamins to inflammation in the intestines: why a child has green feces
Why do babies have green stools, does it depend on how the baby is fed, what foods...
13 September 08:19
⠀
“Allergies can be discussed if parents notice that the rash is persistent, accompanied by itching and aggravated by eating certain foods by a child or mother while breastfeeding. And also when using powders, creams, conditioners, after visiting places where there are animals and plants. The skin should be taken care of with the help of creams that are called "emollients" (for example, Atopic cream, Emolium, Topicrem, BELUPO Aflocrem, Baby Balance, Mustela stelatopia, BABE baby emollient cream, Avene atopic, Aqua Dermica). Hormonal ointments and creams can only be used after being prescribed by an allergist or dermatologist,” warns Dr. Guchapsheva. nine0005
An allergist-immunologist emphasizes the importance of contacting a doctor in time. Especially if the child has a rash with signs of acute respiratory infections (erythema infectiosum): runny nose, fever, aching joints, swelling and redness of the cheeks, whims:
"More often caused by parvovirus, sometimes it is called" slap syndrome ". Also, the rash can be on the body, chest and neck.
Also, the rash can be on the body, chest and neck.
Passes, like acute respiratory infections, within five to ten days and is treated like a virus. It is necessary to give the child plenty of water and apply the symptomatic treatment prescribed by the pediatrician. nine0005
The doctor also notes that redness can appear when the skin is infected - after an injury, exposure to bacteria and other pathogens: “More often this happens with cuts, scratches, or if dry skin is covered with cracks. Parents should be especially wary if the rash is only on one cheek, there is a seal, swelling. Here you need to consult a pediatric surgeon, a dermatologist, and maybe an infectious disease specialist.
Diathesis, red cheeks - atopic dermatitis?
When children come to an appointment with red cheeks, red spots with peeling on the arms and legs, manifestations of atopic dermatitis, then parents often do not know why their child has such problems. nine0005
Most often, mothers in such cases associate manifestations of dermatitis with "Moscow water", which "does not suit" them.
However, it must be admitted that food allergies are most often manifested in infants and, in the vast majority of cases, the culprit is cow's milk, or rather, cow's milk proteins (proteins).
If the child receives artificial nutrition, then the basis of such mixtures is cow's milk proteins (whey and casein fractions of proteins). Thus, when receiving milk formula, the child receives the corresponding allergen in large volume. nine0005
If the baby is breastfed, cow's milk proteins enter the baby's body through breast milk.
Studies have shown that 95% of women have beta-lactoglobulin in breast milk, one of the most allergenic proteins in cow's milk.
However, it should be emphasized that children who are breastfed (naturally) suffer from food allergies much less often, which is associated, among other things, with a lower content of such components in breast milk. nine0005
The basis for the treatment of manifestations of food allergies, intolerance to cow's milk proteins, is the selection of proper nutrition.
When a child is breastfed and symptoms of intolerance to cow's milk proteins are noted, the mother is often advised to adhere to a strict dairy-free diet, when all dairy products are excluded from the diet, including cheese, kefir, cottage cheese, etc., and not just whole milk, as sometimes think. Since such dietary recommendations are quite difficult to maintain, especially for us, the inhabitants of the middle lane, where the culture of dairy nutrition is widespread, it is very important that these prescriptions have a real basis. nine0005
However, it is impossible not to admit that there is an improvement in the condition of the child's skin, the work of his digestive tract with the correct correction of nutrition. Hence even such a term as "diet diagnostics" appeared, i.e., when, after the exclusion of certain products, we see a positive result, which confirms the diagnosis, and "diet therapy", when continuing to follow the recommendations on proper nutrition, it is possible to achieve a good therapeutic effect.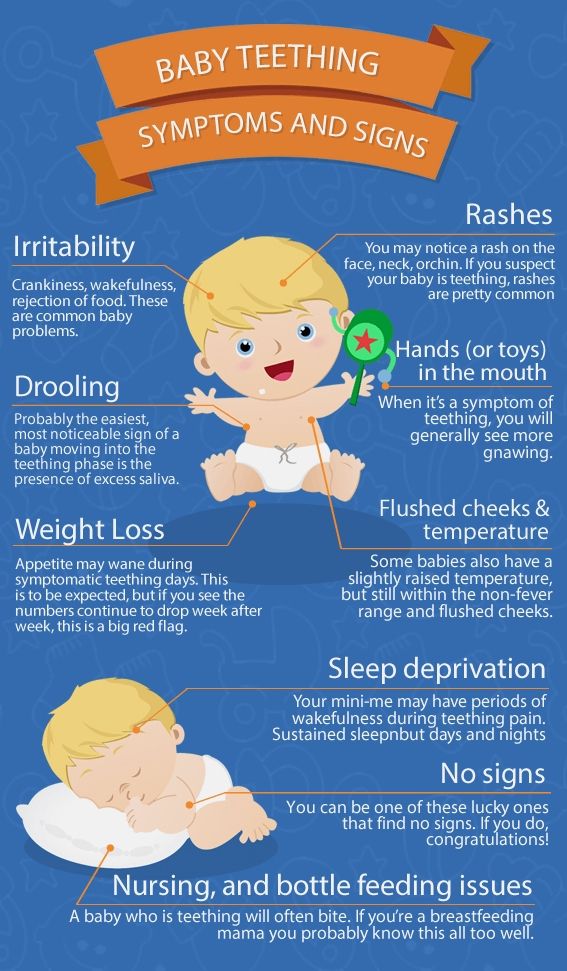
One of the frequently asked questions of parents: "Is it possible to transfer a child with intolerance to cow's milk proteins to goat's milk?" nine0005
The answer is not entirely reassuring. In the vast majority of children, when trying to replace a formula based on cow's milk with a "goat" formula, it is not possible to achieve remission and subsidence of the symptoms of the disease.
For the rational nutrition of formula-fed children with manifestations of allergy to cow's milk proteins, therapeutic specialized nutrition based on hydrolyzed (split) components is used. In such mixtures, the protein is divided into smaller components, down to the smallest particles - amino acids. Such therapeutic nutrition should be selected by a pediatrician in close cooperation with an allergist-immunologist. nine0005
Another important aspect of the treatment of atopic dermatitis is topical therapy. And it is necessary to start in this case with a basic, long-term moisturizing of the skin with specialized means - emollients.