Baby food recommendation
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
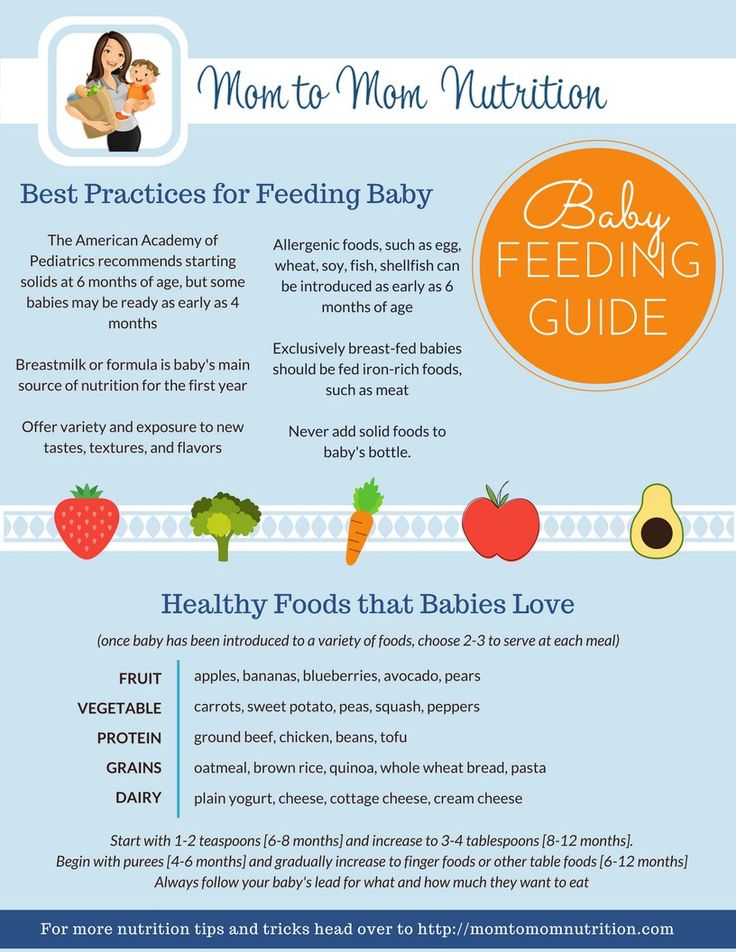
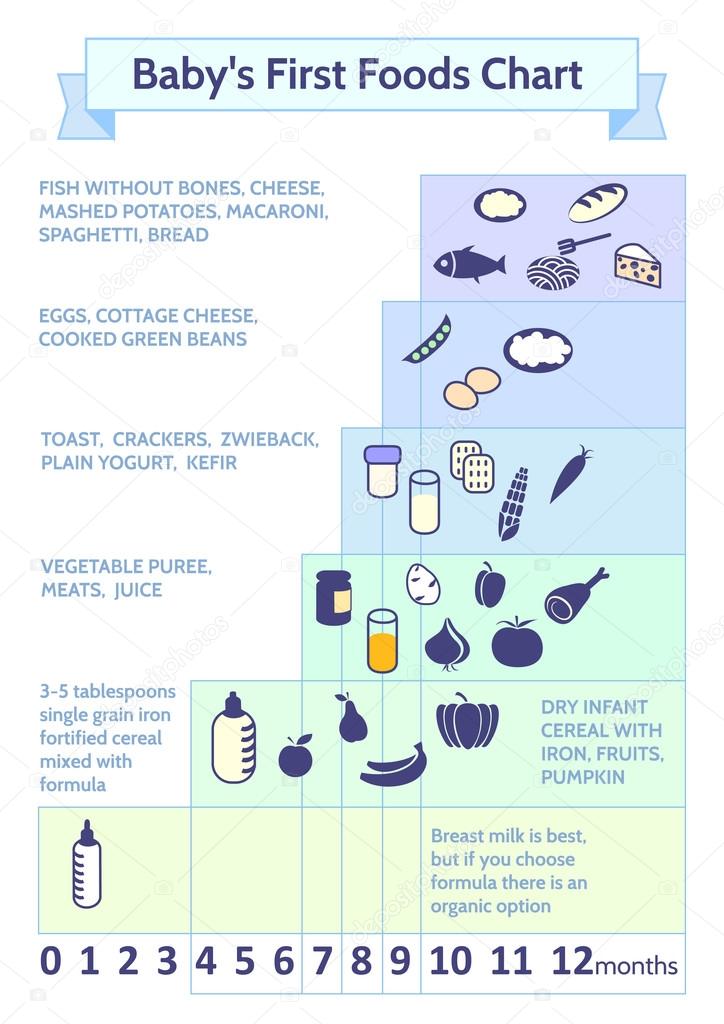
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old. Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
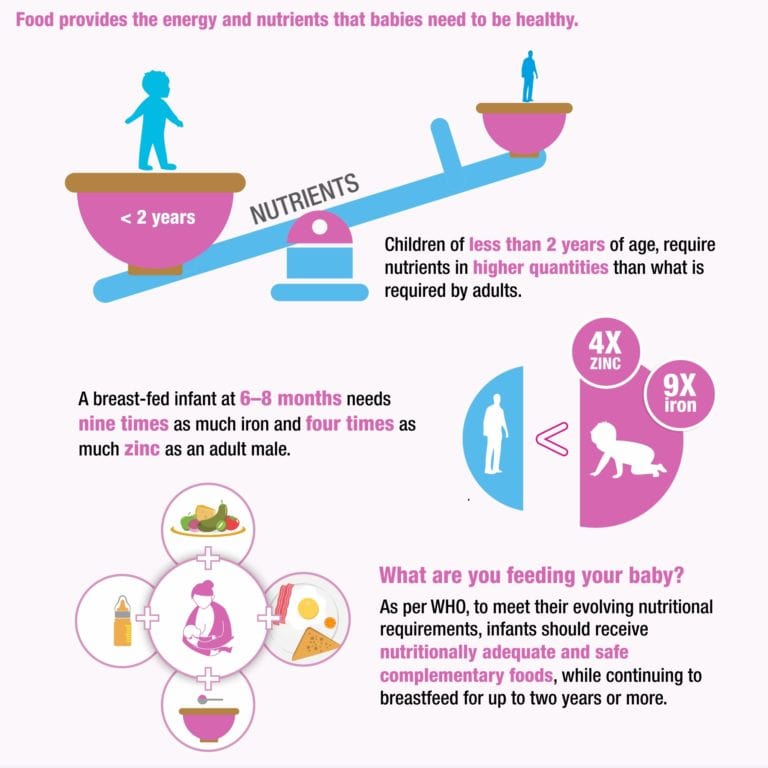
Your child needs certain vitamins and minerals to grow healthy and strong.
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.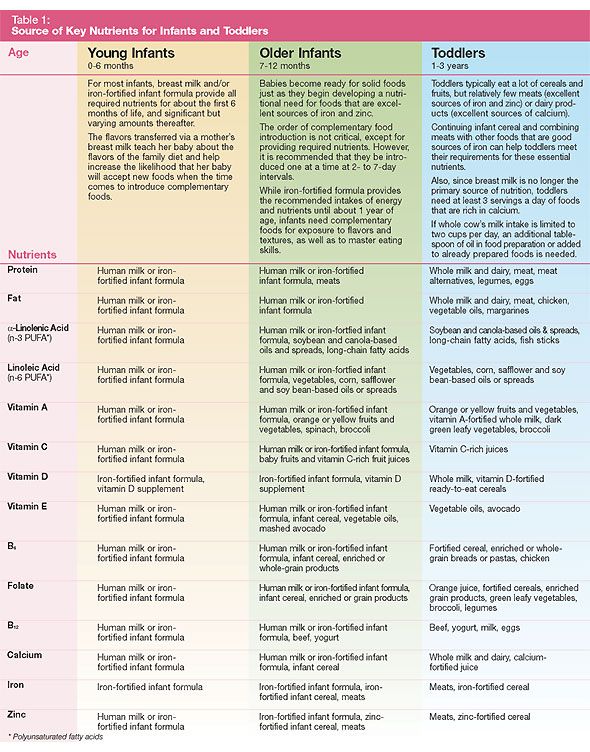
How Should I Prepare Food for My Child to Eat?
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.

- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.
- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
Infant Food and Feeding
Based upon evidence, a number of desired behaviors were identified as critical to helping families foster healthy active living for their infant. For each desired behavior you can explore the evidence, learn what parents told us about these behaviors, identify opportunities to promote healthy behaviors at the point of care, review how to start conversations and access messages and resources to support families. Also available to inform your counseling is the Onset and Patterns of Risk Behaviors during Infancy Timeline located above this section.
For each desired behavior you can explore the evidence, learn what parents told us about these behaviors, identify opportunities to promote healthy behaviors at the point of care, review how to start conversations and access messages and resources to support families. Also available to inform your counseling is the Onset and Patterns of Risk Behaviors during Infancy Timeline located above this section.
Breastfeeding
- Exclusive breastfeeding for approximately 6 months.
- Continue breastfeeding until the baby's first birthday or longer while mutually desired by mother and baby.
-
- Breastfed babies who are breastfed for at least 6 months are less likely to be overweight.
- The duration of breastfeeding also is inversely related to the risk of obesity.
- A reduction of 40% in the incidence of type 2 diabetes mellitus is reported, reflecting the long-term positive effect of breastfeeding on weight control and feeding self-regulation.

- 80% of mothers expect to breastfeed yet only 14% are exclusively breastfeeding at 6 months.
- Critical periods for breastfeeding cessation are transition home from hospital, 6-8 weeks, transition back to work, and between 6-8 months due to self-weaning and/or introduction of solids.
-
- Breastfeeding was harder than they expected. Many tried but did not maintain.
- Surprised to learn that breastfeeding can impact obesity and many felt this info could impact decisions around duration.
-
- Support new mothers in breastfeeding. Provide lactation services at your office or know about sources of lactation support in your community.
- Provide ongoing encouragement for breastfeeding at well visits. Ask patients about challenges or concerns.
- Let mothers know It is wonderful that they are breastfeeding their baby.
 And that breastfeeding is great for their baby and has health benefits for them too.
And that breastfeeding is great for their baby and has health benefits for them too. - If mothers are returning to work assure them that with careful planning and a few resources they can make breastfeeding work.
- Remind families that babies reap the benefits of breastfeeding for their entire first year!
-
Newborn, early months:
- It is so great that you are breastfeeding your baby. It can be very rewarding but challenging too. How is breastfeeding going for you? Do you have any concerns about breastfeeding your baby?
- Can you tell me about a typical feeding experience? Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby?
For 2 or 4 month visit:
- It is wonderful that you are continuing to breastfeed your baby. Are you exclusively breastfeeding?
- Are you returning to work? Many women continue to successfully breast feed after returning to work.
 Tell me about your feelings about this. Are there any questions I can answer to help you during this time of transition?
Tell me about your feelings about this. Are there any questions I can answer to help you during this time of transition? - Are you having any challenges maintaining exclusive breastfeeding?
For 6 and 9 month visit:
- It is wonderful that you are still breastfeeding. Is there anything can I do to support you in your breastfeeding?
-
HALF Message(s):
Lots of parents are surprised to find out that babies who are breastfed for at least 6 months are less likely to be overweight or obese as they get older. Breastfeeding can be a lot of work, but it’s a great way to bond with your baby and help him stay healthy.HALF Resources:
For realistic parent derived strategies for breastfeeding refer parents to the following sections on healthychildren.org/growinghealthy:Quick Tips: Keep Your Child Healthy widget.
Simply select Breastfeeding to generate the results.Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Bottle Feeding
Practice appropriate bottle feeding practices:
- Avoid bottle propping
- Only breastmilk or formula in bottle unless otherwise directed by physician
-
- Inadequate feeding practices associated with bottle feeding of infant formula or use of bottle feeding as a methods to soothe infants can contribute to greater energy intake.
- It is not uncommon for mothers add cereal to the bottle in the belief that doing so will help the infant sleep longer.
- A substantial number of families introduce solids early especially if they perceive the infant as fussy.

- Inattention to a child’s hunger and satiety cues has been associated with infant overfeeding.
-
- Other family members and friends were influencers and provided “evidence” that cereal in the bottle helped baby sleep.
- Parental exhaustion/desire for sleep is a big motivator to add cereal to the bottle.
-
- If parent reports fussiness, counsel parent about importance of responding with an array of strategies, not just feeding.
- If parent reports sleeping problems, counsel about bedtime routines, healthy sleep practices, and realistic sleep expectations based upon baby's age.
- Let parents know that it is important that it will get better.
- Encourage parents to make feeding time responsive and pleasant for them and their baby.
-
- It can be difficult when a parent and baby are not getting enough sleep.
 Can you tell me how this is going for you?
Can you tell me how this is going for you? - It can be difficult when a baby cries a lot. How is it going with your baby? Would you like to talk about some ways to soothe your baby that don’t involve feeding?
- Can you tell me about what feeding time is like for you and your baby?
- Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby.
- How would you describe your baby? Is she content, fussy, sleepy, etc?
- It can be difficult when a parent and baby are not getting enough sleep.
-
HALF Message(s):
Some parents (and grandparents!) worry that young babies aren’t getting enough to eat. But there’s no need to worry — babies under age 6 months get everything they need from breast milk or formula.HALF Resources:
For realistic parent derived strategies for bottle feeding refer parents to the following sections on healthychildren.org/growinghealthyAlso take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Food Introduction
- Introduce solid foods around 6 months of age
- Expose baby to a wide variety of healthy foods
- Also offer a variety of textures
-
- A substantial number of families introduce complementary solid foods around 3-4 months, especially if the infant is perceived as fussy.
- Formula fed infants are at more risk for early introduction of solids.
- Introduction to solids prior to 4 months is associated with increased weight gain and adiposity, both in infancy and early childhood.
- Research indicates that it is important to expose children to a wide variety of flavors and textures.
- Many babies and toddlers need to be exposed to foods multiple times before accepting them.
- Babies and toddlers are more likely to eat foods they see their peers and parents eating.

-
- Other family members and friends were influencers and provided false evidence that introducing solids helped calm fussy babies.
- Parental frustration and desire for happy babies were big motivators to introduce solids.
- Parents cited the concern about wasting food.
- Many parents assumed once their child rejected a food that it meant their child did not like that food.
- Concept of offering a food 10-15 times before acceptance was confusing.
-
- If parent reports fussiness and/or sleeping problems, counsel about the importance of appropriate complimentary food introduction. Share potential calming and soothing strategies for infants, as well as coping strategies for parents.
- Encourage parents to wait until around 6 months to introduce solids.
- Remind parents that this is a very important time and the kinds of foods your baby eats now help him to enjoy healthy foods later.

- Counsel about the importance of introducing a wide variety of foods, especially vegetables and fruits. As the infant grows, it is important to expose the baby to variety of textures.
- Explain that sometimes it takes a baby 10-15 tries over time before they will actually accept a new food.
- Explain that this 10-15 tries is over a period of months and to not get discouraged.
- To address concerns about waste, discuss strategies that limit wasted food, such as not feeding directly from a jar but removing a small serving from a jar to a different container.
- You can reassure parents that it is okay if the infant doesn’t like something the first time, and it is important to keep offering it.
-
- Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby.
- How would you describe your baby? Is she content, fussy, sleepy, etc?
Well Visit 2 and 4:
- Can you tell me a little about your plans to introduce your baby to solid foods?
6 month visit:
- It is wonderful that your baby is ready to embark or beginning to eat solid food.
 It is an exciting milestone! Do you have any concerns or questions
It is an exciting milestone! Do you have any concerns or questions - Tell me a little bit about your experiences so far.
- Can you tell me about your feeding experiences so far? Are you having fun? Do you have any concerns?
- Can you describe what foods your baby likes and dislikes?
- What do you do when your baby seems to dislike or not try a new food?
- How do you introduce new foods to your baby?
-
HALF Message(s):
Lots of parents are excited to start their babies on solid foods. Others are nervous. Starting to eat solid foods (like baby cereal and baby food) is an important part of your baby’s development. Did you know that babies who start eating solid food too early are more likely to be overweight or obese in childhood and adulthood? This is one more important reason to wait until your baby is really ready before giving him solid foods.HALF Resources:
- For realistic parent derived strategies for solid food introduction refer parents to the following sections on healthychildren.
 org/growinghealthy
org/growinghealthy - Quick Tips: Keep Your Child Healthy widget. Simply select Starting Solid Foods to generate the results.
- Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
HALF Message(s):
Introducing your baby to new foods can be both fun and frustrating. Some parents worry about wasting food and money if their babies don’t like a lot of foods at first. Good news: a new eater only needs 1-2 tablespoons of each food and will gradually increase to 3-4 tablespoons as she gets older. By getting your baby used to lots of different foods, you’ll help him build a healthy diet for life. - For realistic parent derived strategies for solid food introduction refer parents to the following sections on healthychildren.
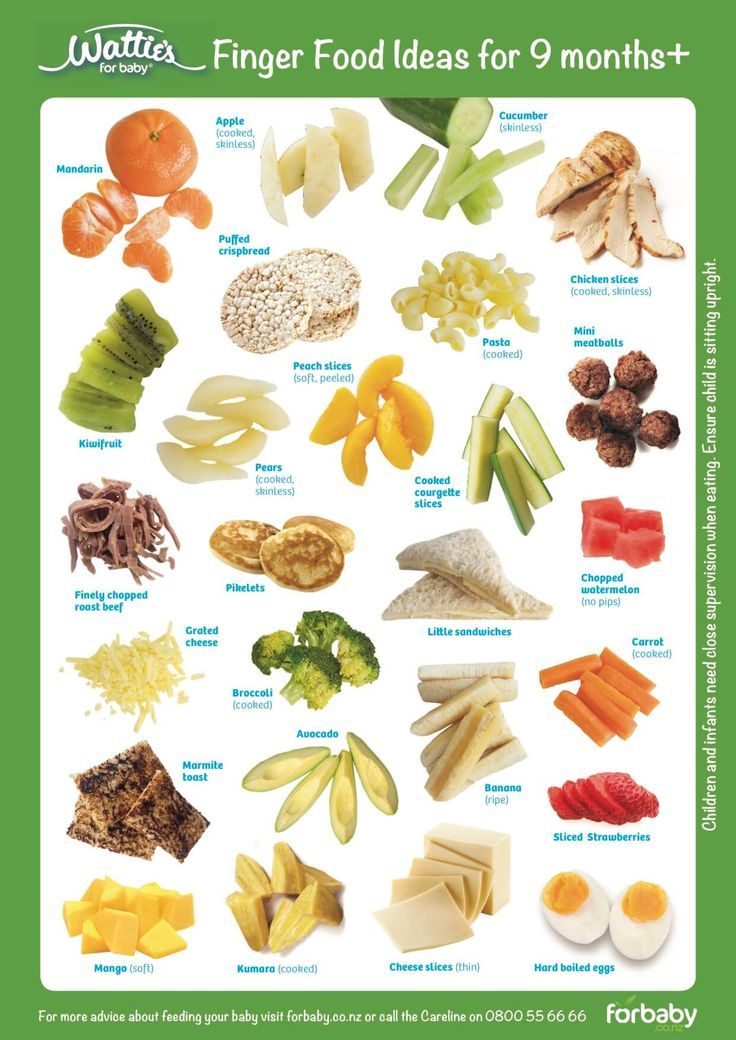
Healthy Snacking
- After 9 months, offer 2-3 healthy and nutritious snacks per day
- Maintain fruit and vegetable consumption after finger foods are introduced
-
- Almost all older infants snack regularly, but the quality of the snacks is variable.

- The most common snack foods are often finger foods such as cereal, cookies, crackers, and French fries.
- Eating at regular intervals helps to foster self-regulation and reduces overeating.
- At 9 months, there is a considerable drop in fruit and veggie consumption, and an increase in non-nutritive finger and snack foods.
- Almost all older infants snack regularly, but the quality of the snacks is variable.
-
- Many parents (especially grandparents) seem to associate snack time with “treat” time.
- Parents generally were positive about introduction of finger foods but many opted for prepackaged foods that were portable and not choking hazards.
-
- Counsel on appropriate feeding recommendations and the importance of regular healthy and nutritious meals and snacks.
- When discussing routines, mention the importance of planning for regular and healthy snacks.
- Explain that snacks are an opportunity to provide critical nutrients babies need.
- Counsel that snack and meal times should be supervised and ideally occur seated at a table, not in transit (i.e. stroller or car seat).
- By 9 months, counsel on the importance of maintaining fruits and veggies as part of the baby's diet.
- Discuss strategies to use healthy finger foods as snack foods, rather than just prepackaged snack items.
- Snacks are an important part of the baby's nutrition. Suggest that parents offer a fruit and/or veggie for at least one snack every day.
- Discuss potential choking hazards and strategies to offer healthy foods in bite size portions.
-
- What kinds of foods do you offer your child for snacks?
- What kinds of foods does your child want for snacks?
- What part do snacks play in your eating plan for your child?
- How do you feel about snacks as treats or rewards?
- How often does he have snacks? What other kinds of foods do you offer?
- How does your child respond to being offered fruits? Vegetables?
- What do you do if your child refuses to eat fruits and/or vegetables?
- What kind of snacks does your child get in child care? What about when they are staying with grandparents or with other family members?
-
HALF Message(s):
Have fun with finger foods. Let your baby try feeding herself. Offer healthy snacks 2-3 times per day.
Let your baby try feeding herself. Offer healthy snacks 2-3 times per day. HALF Resources:
- For realistic parent derived strategies on healthy snacking and finger foods refer parents to the following sections on healthychildren.org/growinghealthy
- Quick Tips: Keep Your Child Healthy widget. Simply select Healthy Snack and Routines and Schedules to generate the results.
- Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Foster Self-feeding
- Babies are encouraged to use spoons and fingers to feed themselves
- Babies are encouraged to drink from a cup starting at 6 months of age
- Parents recognize hunger and satiety cues
-
- Babies have an innate ability to self-regulate their food.

- Responsive feeding helps foster self-regulation.
- Babies have an innate ability to self-regulate their food.
-
- Parents identified time and cleanliness as the two big barriers to self-feeding.
- Wasting food is another concern.
-
- Discuss responsive feeding, hunger and satiety cues with parents.
- Encourage parents to foster babies self-feeding by using fingers, spoons, and cups. Explain that using their hands and trying to use a spoon are important parts of how a baby learns to self-feed and regulate how much they eat.
- Acknowledge that self-feeding can sometimes be messy and take a bit longer. Strategize with parents about setting certain meals and snacks aside for their child to hone these skills, and remind parents when they opt to feed their child to be aware of fullness cues.
-
- How is your baby doing with a spoon?
- Can you describe how you go about encouraging your baby to feed herself?
- What is it like at mealtimes when your baby feeds herself? How do you feel about it, and how does your baby feel about it?
- What would be helpful to you and your baby to encourage self feeding?
-
HALF Message(s):
Let your baby try feeding herself as soon as she’s ready — usually around 8 or 9 months old.
HALF Resources:
- For realistic parent derived strategies on self-feeding refer parents to the following sections on healthychildren.org/growinghealthy
- Food and Feeding Infants
Healthy Drinks
- Babies should drink breastmilk or formula for the first year of life
- Try to avoid introducing juice until child is a toddler. If juice is introduced, wait until 6-9 months and limit consumption to 4-6 ounces
- Avoid introduction of sugar-sweetened beverage
-
- Almost 80% of babies 6-9 months drink juice regularly.
- Children who consume such fruit juices have higher energy intakes.
-
- In general, parents thought 100% juice was a healthy choice.
- Parents thought that the oral health angle was impactful when discussing risks of sugared beverages.
- Some parents mentioned elimination issues as a reason to or not use juice drink.
- Other family members and eating out were two factors parents identified as contributing to the introduction of juice or other sugar sweetened beverages
.
- In general, parents thought 100% juice was a healthy choice.
-
- Remind parents that breastmilk, formula and water are the best beverage choices at this time. Suggest that water is a great choice for practicing drinking from a cup and encourage families to foster use of cups over bottles and sippy cups.
- If they want to introduce juice, help parents understand what a 4-6 ounce serving looks like, and that this is the amount for one day.
-
- Does your child drink juice? How much do you offer?
- How do you feel about your child drinking sugar sweetened beverages like soda, sports drinks, and juice?
- What beverages does your family drink at meals and between meals? What about when eating out?
- When you eat out, what beverages does your child drink?
- What beverages does your child drink at child care? With other friends and family members?
-
HALF Message(s):
Breast milk and formula are the best choices for your baby. When it’s time for him to start using a cup (around 6 to 9 months), give him breast milk, formula, or water.
When it’s time for him to start using a cup (around 6 to 9 months), give him breast milk, formula, or water. HALF Resources:
- For realistic parent derived strategies on healthy drinking refer parents to the following sections on healthychildren.org/growinghealthy
- Quick Tips: Keep Your Child Healthy widget. Simply select Bottle Feeding and Healthy Snacks to generate the results.
- Food and Feeding Infants
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Last Updated
07/06/2021
Source
American Academy of Pediatrics
2.4.5. Baby food \ ConsultantPlus
- Home
- Documents
- 2.4.5. Baby food
Attention! Since January 1, 2021, the mechanism of the "regulatory guillotine" has been in effect. As a general rule, within the framework of state control (supervision), it is not allowed to assess compliance with the mandatory requirements contained in the regulatory legal acts of the Government of the Russian Federation and federal executive bodies that entered into force before January 1, 2020, as well as in legal acts of executive and administrative bodies of state power RSFSR and USSR. Failure to comply with such requirements cannot be grounds for bringing to administrative responsibility (see Federal Law of July 31, 2020 N 247-...
Failure to comply with such requirements cannot be grounds for bringing to administrative responsibility (see Federal Law of July 31, 2020 N 247-...
Reference information: "Sanitary and epidemiological regulation" (The material was prepared by ConsultantPlus specialists)
2 .4.5. Baby food
| Designation | Document or authority that approved health requirements |
| SanPiN 2.3/2.4.3590-20 "Sanitary and epidemiological requirements for public catering" Attention! The validity of the document is limited to 01/01/2027 For more see >>> | Decree of the Chief State Sanitary Doctor of the Russian Federation of October 27, 2020 N 32 |
| Guidelines MP 2.3.0171-20 "Specialized diet for children and adults in self-isolation or quarantine at home due to COVID-19" | Chief State Sanitary Doctor of the Russian Federation 10. |
| Guidelines MP 2.4.0180-20 "Parental control over the organization of hot meals for children in educational institutions" | Chief State Sanitary Doctor of the Russian Federation 05/18/2020 |
| Guidelines MR 2.4.0179-20 "Recommendations on catering for students in general education organizations" | Chief State Sanitary Doctor of the Russian Federation May 18, 2020 |
| Methodological recommendations "Practical aspects of the organization of rational nutrition of children and adolescents, the organization of nutrition monitoring" | Chief State Sanitary Doctor of the Russian Federation 08/10/2018 |
| Guidelines MR 2.4.5.0128-18 "Organization of nutrition for children during mass events" | Chief State Sanitary Doctor of the Russian Federation May 15, 2018 |
| Guidelines for catering for students and pupils of educational institutions | Order of the Ministry of Health and Social Development of Russia N 213n, Ministry of Education and Science of Russia N 178 dated 11. |
| Guidelines "Recommended assortment of food products for sale in school canteens" | Rospotrebnadzor 08/24/2007 N 0100/8606-07-34 |
| Methodological recommendations "Sample menus of hot school breakfasts and lunches for catering for children 7 - 11 and 11 - 18 years old in public educational institutions" | Rospotrebnadzor 24.08.2007 N 0100/8605-07-34) |
| Methodological recommendations "Recommended average daily food packages for children 7 - 11 and 11 - 18 years old" | Rospotrebnadzor 08/24/2007 N 0100/8604-07-34 |
| Guidelines "Assortment and conditions for the sale of food products intended for additional nutrition of students in educational institutions" | Interdepartmental Scientific Council for Pediatrics, Interdepartmental Scientific Council for Hygiene and Health Protection of Children and Adolescents, Protocol of 02. |
| Recommendations "Assortment of basic food products recommended for use in the nutrition of children and adolescents in organized groups (kindergartens, educational institutions of general and correctional type, orphanages and boarding schools, institutions of primary and secondary vocational education)" | Ministry of Health of the Russian Federation 04.04.1999 N 1100/904-99-115 |
| Norms of nutrition for children in health and recreation institutions of general and sanatorium type, incl. for parents with children | Resolution of the Executive Committee of the Council of the FNPR dated May 27, 1993 N 6-6 |
| Guidelines MR 2.4.5.0107-15 "Organization of nutrition for children of preschool and school age in organized groups" | Chief State Sanitary Doctor of the Russian Federation November 12, 2015 |
| Guidelines "Organization of therapeutic nutrition in children's hospitals" | Ministry of Health of the Russian Federation November 10, 2000 |
| Guidelines "Feeding children in preschool institutions in the northern regions of the country" | USSR Ministry of Health 07/05/1985 N 11-14 / 24-6 |
| Methodological recommendations "Feeding children in orphanages" | USSR Ministry of Health 06/02/1985 N 11-14 / 26-6 |
| Guidelines "Nutrition for chronic diseases of the digestive system in children" | Ministry of Health of the USSR 06/19/1984 N 11-14 / 13-6 |
| Guidelines for catering students in dispensaries | USSR Ministry of Health 05. |
| Guidelines for the determination of organochlorine pesticides in raw materials for the production of powdered infant formula | USSR Ministry of Health 09/22/1975 N 1350-75 |
2.4.4. Organizations of recreation and health improvement for children and adolescents 2.4.6. Occupational health of children and adolescents
Union of Pediatricians of Russia
0011
Nutrition for children aged 1 to 3 years
The period from 1 to 3 years of life is a crucial stage in the transition to an adult type of nutrition, which has certain features. In order to ensure that all the necessary nutrients enter the child's body and at the same time prevent an excess of individual nutrients, nutrition should be balanced and varied.
The daily amount of food for children aged 1 to 1.5 years should be 1000-1200 g, from 1. 5 to 3 years - 1200-1500 g, the amount of food in one feeding should not exceed 300-350 ml. The diet consists of three main meals per day and two snacks. It is considered optimal when breakfast is 25% of the total energy density of the diet, lunch is 30–35%, dinner is 20%, and additional meals are about 10%. In general, the child can eat the same food as the rest of the family.
5 to 3 years - 1200-1500 g, the amount of food in one feeding should not exceed 300-350 ml. The diet consists of three main meals per day and two snacks. It is considered optimal when breakfast is 25% of the total energy density of the diet, lunch is 30–35%, dinner is 20%, and additional meals are about 10%. In general, the child can eat the same food as the rest of the family.
In the diet of a child of 1-3 years of age must be present daily : animal or poultry meat, dairy and sour-milk products, vegetables, fruits, bread, cereals, vegetable and butter; fish and eggs are included in the diet 2-3 times a week.
Cereal products: bread - 2-3 servings per day, cereals and side dishes - 1 time per day
Fruit and/or vegetables: at least 5 times a day
Dairy products: at least 3 servings per day (including those used to make cereals, yoghurts, fermented milk drinks, cottage cheese, infant formula or breast milk).
Domestic pediatricians recommend, when compiling a diet for children aged 1–3 years, preference should be given to specialized children's dairy products of industrial production that meet high quality requirements and safety indicators for this age. Most children's dairy products are additionally enriched with vitamins and/or minerals and other biologically active components, taking into account the physiological needs of children of this age. At the same time, in foreign recommendations, children over 1 year old are offered the gradual introduction of whole cow's milk, which is rich in fats necessary for proper growth and development, the absorption of vitamins A and D, the development of the brain and nervous system of the child.
Most children's dairy products are additionally enriched with vitamins and/or minerals and other biologically active components, taking into account the physiological needs of children of this age. At the same time, in foreign recommendations, children over 1 year old are offered the gradual introduction of whole cow's milk, which is rich in fats necessary for proper growth and development, the absorption of vitamins A and D, the development of the brain and nervous system of the child.
Meat dishes: 2-3 times a day
Fish dishes: 2-3 servings per week
Eggs: 2-3 per week
Dietary fats: 3-4 teaspoons of butter and/or vegetable oils per day
When cooking, use the minimum amount of salt and sugar, and do not add them to industrial products.
Offer your child a variety of foods and let them choose their own. Children love to eat on their own, so if possible, offer food that the child can eat with their hands.
It is important to remember that a baby can choke on pieces of food, so whatever you give your baby should be crushed or cut into small pieces that can be easily chewed.

 04.2020
04.2020  03.2012
03.2012  07.2002 N 4
07.2002 N 4  10.1979 N 2059-79
10.1979 N 2059-79