Baby goes red and blotchy when feeding
Skin rashes in babies | nidirect
It's normal for babies to develop rashes from as early as a few days old. If your baby has a rash but doesn’t show signs of illness, speak to your midwife, health visitor, or your GP. If your baby appears unwell, call your GP or GP out of hours service.
About skin rashes in babies
It's important to be aware of the symptoms of meningitis, see section below.
Also below is information on some of the most common rashes in babies. Most rashes are harmless and go away on their own.
This guide may give you a better idea of the cause of the rash. But don't use it to diagnose your baby's condition. Always speak to a health professional for a proper diagnosis.
- read about causes of rashes in older children
Baby acne (neonatal acne)
Baby acne is where pimples sometimes develop on a baby's cheeks, nose and forehead within a month of their birth.
About baby acne
- pimples tend to get worse before clearing up completely after a few weeks or months
- washing your baby's face with water and a mild moisturiser can improve the appearance of their skin
- avoid acne medicines intended for older children and adults
Pimples or blackheads that develop after three months of age (infantile acne) tend to be more severe. These often need medical treatment.
Cradle cap
Cradle cap is where yellowish, greasy, scaly patches develop on a baby's scalp.
About cradle cap
- occasionally, as well as the scalp, the face, ears and neck are also affected
- it isn't itchy and shouldn't bother your baby- if your baby is scratching or upset, they may have eczema (see below)
- it is a common condition that tends to develop within two or three months after birth
- it usually gets better without treatment in a few weeks or months
Gently washing your baby's hair and scalp with baby shampoo may help to prevent further patches developing.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked.
The most common form is atopic eczema. It mainly affects babies and children but can continue into adulthood.
About atopic eczema
- eczema in babies under six months is sometimes associated with allergies to milk and egg
- it often starts in young babies as a red, itchy rash on the face, scalp and body
- as the child gets older, it usually starts to develop in areas with folds of skin, such as behind the knees or on the front of the elbows
Creams and ointments can often relieve the symptoms.
Erythema toxicum
Half of all newborns develop a blotchy red skin reaction called erythema toxicum. This is usually at two or three days old.
It's a normal newborn rash that won't bother your baby and clears after a few days.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, viral illness.
About hand, foot and mouth disease
- it causes a blistery rash on the palms of the hands and soles of the feet, as well as ulcers in the mouth
- your baby may also feel unwell and have a fever
Treatment isn't usually needed, as the baby's immune system clears the virus. The symptoms go away after about seven to 10 days. If you're worried, see your GP.
Hives (urticaria)
Hives is also known as urticaria.
About hives
- causes a raised, red itchy rash that appears on the skin
- happens when a trigger (such as a food that your baby is allergic to) causes a substance called histamine to be released into their skin
If your baby gets urticaria during feeding, the condition may be triggered by something they've had to eat or drink. The most common foods are egg and milk, but many other foods can sometimes be the cause.
The most common foods are egg and milk, but many other foods can sometimes be the cause.
The urticaria rash is usually short-lived and can be controlled with antihistamines. If your baby gets hives repeatedly, it's important to see your GP to discuss possible allergies.
Impetigo
Impetigo is a highly contagious bacterial infection of the surface layers of the skin. It causes sores and blisters.
It's not usually serious, but you can visit your GP for a prescription of antibiotics. This should clear the infection within seven to 10 days.
Milia
About half of all newborns develop tiny (1-2mm) white spots on their face. These are called milia.
These are just blocked pores. They usually clear within the first four weeks of life.
Nappy rash
Nappy rash occurs when the skin around the baby's nappy area becomes irritated.
About nappy rash
- is often caused by exposure to wee or poo for a long period of time
- can sometimes be the result of a fungal infection or rare skin condition
You can usually reduce nappy rash by taking simple steps to keep your baby's skin clean and dry. You can use a barrier cream if needed. Antifungal cream may be necessary if the rash is caused by a fungal infection.
You can use a barrier cream if needed. Antifungal cream may be necessary if the rash is caused by a fungal infection.
- read more about nappies and nappy rash
Ringworm
Ringworm is a common fungal skin infection. It causes a ring-like red rash almost anywhere on the body (the baby's scalp, feet and groin are common areas).
It's usually easily treated using over-the-counter creams.
Ask your pharmacist if you need advice about treatment.
Scabies
Scabies is a common infestation of the skin that can affect people of all ages.
About scabies
- it's caused by tiny mites that burrow into the skin
- it's often spread between family members, so when babies get scabies it's usually because someone else in the family had it recently
- babies with scabies develop tiny and very itchy spots all over the body, including on the soles of the feet, armpits and genital area
Treatment with creams that kill the scabies mite needs to be given to the whole family at the same time for it to be effective.
Visit your GP if you think your baby has scabies. It's not usually a serious condition, but it does need to be treated.
Your GP will discuss treatment with you. The treatments most widely used are a cream and lotion.
Slapped cheek syndrome
Slapped cheek syndrome is a viral infection particularly common in children and babies.
About slapped cheek syndrome
- it typically causes a bright red rash on both cheeks and a fever
- most babies won't need treatment, as slapped cheek syndrome is usually a mild condition that passes in a few days
Sweat rash (miliaria)
A heat rash is sometimes called miliaria or prickly heat. It may flare up when your baby sweats. For example, because they're dressed in too many clothes or the environment is hot and humid.
It's a sign your baby's sweat glands have become blocked.
They may develop tiny red bumps or blisters on their skin, but these will soon clear without treatment.
Meningitis
Meningitis is an infection of the protective membranes that surround the brain and spinal cord (meninges).
About meningitis
- the classic rash associated with meningitis usually looks like small, red pinpricks at first
- it then quickly spreads over the body and turns into red or purple blotches
- it is a blotchy rash that doesn't fade when a glass is rolled over it (this won't always develop)
Meningitis warning signs
It's important to be aware of the warning signs of meningitis in your baby, which include:
- becoming floppy and unresponsive, or stiff with jerky movements
- becoming irritable and not wanting to be held
- unusual crying
- vomiting and refusing feeds
- pale and blotchy skin
- loss of appetite
- staring expression
- very sleepy with a reluctance to wake up
- fever
Some babies develop a swelling in the soft part of their head (fontanelle).
Trust your instincts. If you think your baby has meningitis, see your GP or GP out of hours service immediately or go to your nearest emergency department.
- find out more about skin rashes in babies on the NHS website
More useful links
- How to use your health services
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
What do you want to do?report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.
Enter your feedback
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Why Does My Baby's Face Turn Red When Breastfeeding?
There could be many reasons for your breastfed baby’s face to turn red when breastfeeding. It’s important to note that each newborn baby is different, so what affects one child may not affect the other.
Consider the following:
#1. It Could Be The Food Allergies
It Could Be The Food Allergies What a mom consumes during breastfeeding can affect the child. Breastfeeding moms need to maintain a healthy diet and be aware of the food that can cause allergic reactions.
For example, eating eggs can cause red spots on some children’s skin. So, next time you notice a change in the color of your child’s cheeks or red spots on your face, observe what you recently ate. You can eliminate the food allergens from the diet to eliminate this issue and see if it helps!
If it’s hard to figure out in the beginning, try eliminating one thing at a time from your diet and see if it changes the situation. Also, discussing this situation with your healthcare provider is best, especially when trying to maintain a healthy diet while breastfeeding.
#2. It’s A Heat RashAnother reason causing your little munchkin’s cheeks to turn red is probably the heat rash. However, it could be a natural response as your newborn baby’s facial muscles are active while consuming breast milk supply.
You can see it disappearing in a few minutes if it’s a heat rash. However, it’s also vital to dress your child according to the weather. For example, you may pack the baby in layers, and the baby may feel sweaty while breastfeeding.
Also, work on the room temperature as it has to be suitable for your baby’s age. According to the Sleep Foundation, a room temperature above 22 degrees Celsius or 72 degrees Fahrenheit could be too warm for babies.
Understand what’s most comfortable for your baby’s skin. For example, your baby may be allergic to the blanket or the clothes you wear. It’s hard to find the exact cause right away, but monitoring and observing your surroundings may help.
#3.OverheatingRed spots on your baby’s cheeks can occasionally be a sign of an underlying medical problem that you might not notice right away. It’s possible that one of these issues is overheating.
You see, a baby may already be experiencing this issue prior to a feeding session for a variety of reasons. Infant overheating can be caused by:
Infant overheating can be caused by:
- Room temperature is high
- Sleeping next to your parents
- Too many blankets
- The excessive layering of clothing
Naturally, it’s simple to determine if a baby is too warm to be comfortable. A mom who doesn’t get enough sleep, however, might be too worn out to recognize overheating symptoms. She will therefore begin nursing her child, at which point she will notice that his face has become red.
#4. EczemaInfants frequently develop eczema, especially in the first few months of life. On the baby’s skin, this condition manifests as red, crusty patches.
The joints of the arms and legs as well as the cheeks are the most common locations for these red spots to appear on the body. Of course, eczema is easily treatable, and the majority of infants recover from it quickly.
It’s difficult to determine whether the red spots on your baby’s face are caused by eczema or another type of rash. Always talk to your doctor before beginning treatment in this situation.
Always talk to your doctor before beginning treatment in this situation.
Therefore, it might not be appropriate to ask “Why does my baby’s face turn red when breastfeeding” in this situation. This is because breastfeeding has nothing to do with eczema. However, due to friction and increased body heat, the red spots on a baby’s face could aggravate.
However, you might be interested in learning what causes eczema. Sometimes it’s just in the blood. Therefore, your baby will have a higher chance of developing eczema if you or your partner do.
On another note, babies with issues with the skin barrier may develop eczema. In this situation, their skin has a tendency to keep moisture out while letting germs in. That’s a different possibility, then.
#5. Blood Sugar SpikeLet’s start with the most fundamental explanation for why many babies’ faces become slightly redder after eating. Blood sugar levels rise when a baby drinks breast milk because milk contains carbohydrates.
Additionally, some studies have shown that secondhand sugars can enter the baby through breast milk. The result is that the blood vessels enlarge, briefly causing the baby’s face to flush. Of course, none of this is a problem. The redness should go away after a short while following the feeding session.
#6. It’s A Skin RashYour baby could be having a skin rash. There are many possibilities, your baby has skin allergies, for example, eczema or atopic dermatitis, or the skin is too dry because of the weather conditions.
If your baby has a skin rash, it’s best to find the underlying cause of such a response. Also, your baby may feel itchy on the affected area, and scratching may lead to sores that can cause more infection, causing the area to appear red.
It’s also wise to keep an eye on your baby’s poop. If the baby is active and comfortable, there isn’t anything to worry about your child. However, if the baby shows signs of distress, dehydration, or other accompanying symptoms along with the rash, notify your healthcare provider and take effective measures. Again, even though there is information online, only a doctor can tell what’s going on!
Again, even though there is information online, only a doctor can tell what’s going on!
The exact underlying cause could be hard to find, but you can talk to your doctor and try different things to find a viable solution. For example, if it’s the heat rash, it won’t be an issue; if it’s because of food allergens, you can eliminate some variety of food from the diet and see if it helps.
What to do if your baby has a red rash on the cheeks?Ask your doctor to suggest a suitable medicine for the baby’s skin. It could be a skin rash or an allergic reaction to the food a mom consumes. You can expect it to disappear in a few minutes if it’s a heat rash.
Is the baby’s red rash on the cheeks a cause for concern?If you observe a rash appearing red on your baby’s cheeks, it could be a heat rash. If it disappears, it’s not concerning, but if the rash is itchy and you find your baby scratching the cheeks, crying, and there are open sores in the rash, talk to your doctor to recommend a medicine, cream, or lotion to ease the itch or pain.
If you are consuming a food item that doesn’t suit your baby, you may notice your baby having a gas, constant crying, diarrhea, and possibly a skin rash. Let your doctor know about it and eliminate food allergens from the diet to be on the safe side.
What can new moms do about breastfeeding?Breastfeeding can be challenging for new moms. Classes can help, or talking to a professional is another possibility. You can ask your doctor to guide you more about it. It’s also wise to learn about milk supply and how to increase it. Understanding the do’s and don’t can help you in many ways.
How to get rid of the baby’s rash when breastfeeding?It’s best to wait and see if the rash disappears on its own in a few minutes. You can expect a heat rash to disappear. On the other hand, if it’s a skin rash, you may need to use a medication or lotion recommended by your doctor.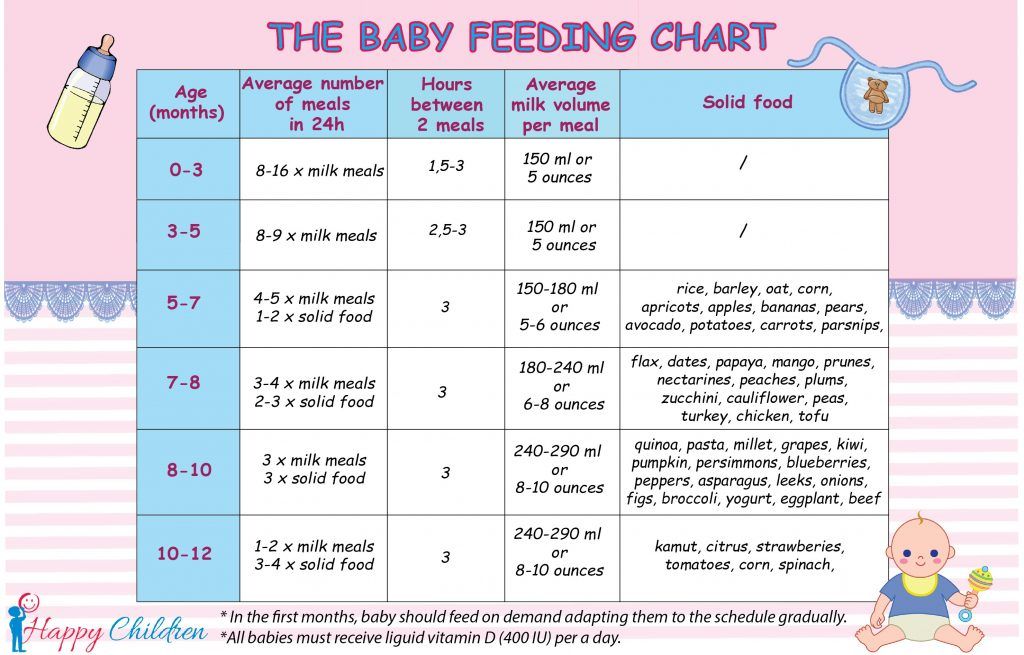
After the first week of life, breast milk jaundice symptoms frequently appear. The skin and eye whites may become discolored in a yellowish hue and fatigue.
Wrapping It UpThere are many reasons for your baby’s face to turn red when breastfeeding; for example, it could be a heat rash, skin allergy, or a reaction to food allergens. In any case, it’s best to talk to your doctor and get medication, cream, or lotion suitable for your baby’s age and skin. Eliminate the food allergens from your diet and see if it helps. Try different things and see what suits your child and resolves the issue!
Reference:https://kidshealth.org/en/kids/egg-allergy.html
https://www.mymilkybaby.com/why-does-my-babys-face-turn-red-when-breastfeeding/
https://www.mustelausa.com/blogs/mustela-mag/red-cheeks-baby
Diathesis - health articles
From the age of 3 months, limited bright red spots may appear on the child's cheeks, which subsequently become covered with a thin crust.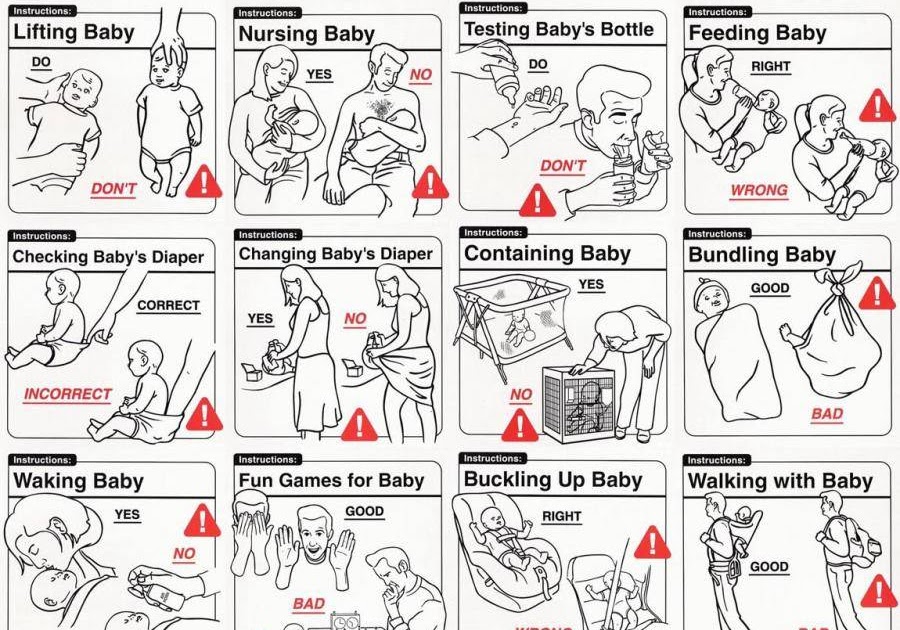 In these places, itching and soreness are felt. These are the so-called milk crusts or milk scab - one of the characteristic manifestations of improper metabolism - exudative diathesis. It is also called allergic diathesis.
In these places, itching and soreness are felt. These are the so-called milk crusts or milk scab - one of the characteristic manifestations of improper metabolism - exudative diathesis. It is also called allergic diathesis.
The first signs of diathesis could appear in a child earlier in the form of persistent diaper rash (not passing even with careful care), profuse prickly heat (even with slight overheating) and, finally, in the form of gray-yellow greasy crusts on the scalp and eyebrows.
With diathesis, a child develops hypersensitivity to certain food and medicinal substances. Therefore, the usual care and feeding for such a child is insufficient, it is necessary to make appropriate adjustments to them.
Causes and symptoms
It is difficult to single out any one cause of diathesis - as a rule, it develops under the combined influence of several reasons, the most important of which is hereditary predisposition, as well as: poor nutrition of a woman during the gestation period.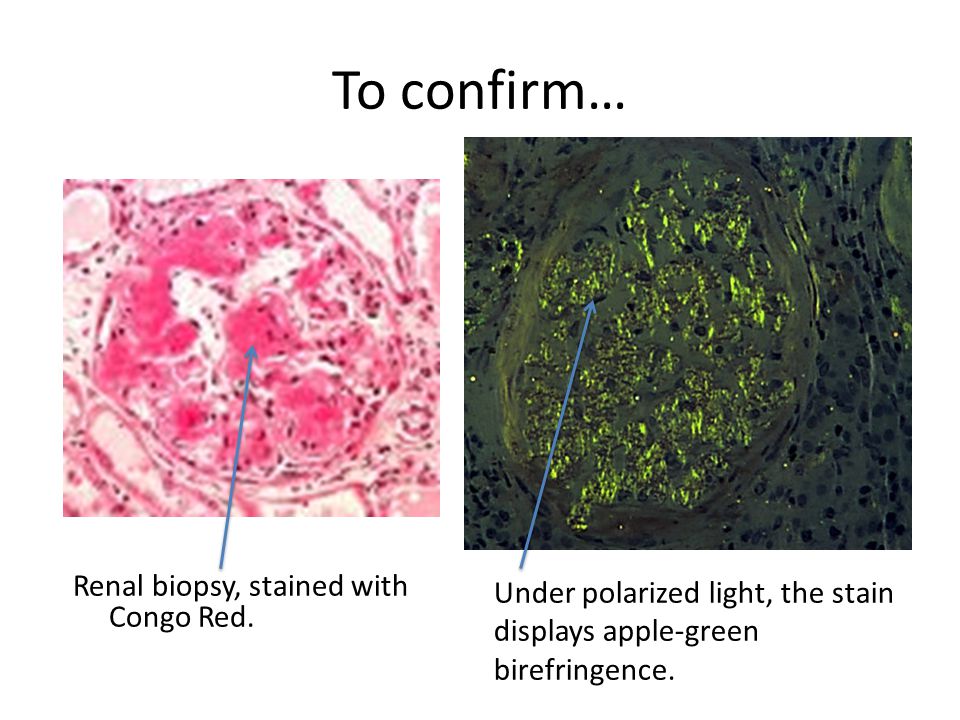
Food allergies and allergies to external irritants (dry air, wool, dust, etc.) are most common in young children. The body responds with changes in the functioning of the gastrointestinal tract, mucous organs and respiratory organs, and the skin.
The most common manifestation is skin rash. In most cases, they occur after the allergen enters the body. Food allergies often manifest themselves in babies whose digestive system is imperfect and cannot absorb foods that provoke allergies. Usually, such symptoms appear up to three years - then the allergy either goes away on its own or goes into a chronic phase.
Outwardly, the rashes are redness, small white crusts and scabs that appear after scratching itchy places. Since the itching is very strong, children cannot resist scratching the affected areas, and this in turn leads to long-term non-healing wounds. The most common places that are affected by diathesis are the elbow and popliteal folds, neck, cheeks, hands.
Diagnostics
Since diathesis is not an independent disease and diagnosis, children with various manifestations of constitutional anomalies can be patients of a pediatrician, pediatric dermatologist, pediatric endocrinologist, pediatric nephrologist, pediatric allergist-immunologist, pediatric rheumatologist, pediatric neurologist, pediatric otolaryngologist, pediatric homeopath etc.
Of the methods of laboratory diagnostics for diathesis, a general analysis of urine and blood is used; biochemical analysis of urine; determination of blood levels of glucose, cholesterol, phospholipids, uric acid, catecholamines; immunological studies, examination of feces for dysbacteriosis, etc.
In case of lymphatic-hypoplastic diathesis, it becomes necessary to conduct ultrasound of the thymus, lymph nodes, liver, spleen, adrenal glands, X-ray of the chest organs.
Treatment
Since the vast majority of allergens are of food origin, the treatment of diathesis in babies begins with the establishment of a balanced diet. Here it is appropriate to emphasize how important breastfeeding is for the baby. Firstly, human milk proteins are 100% devoid of allergic properties, they are easily broken down by the baby's enzymes; secondly, breast milk contains a lot of secretory immunoglobulin A, which protects the intestinal mucosa from large molecules of allergens; thirdly, milk contains enzymes for digesting its own components and, finally, it is the best prevention of dysbacteriosis.
Here it is appropriate to emphasize how important breastfeeding is for the baby. Firstly, human milk proteins are 100% devoid of allergic properties, they are easily broken down by the baby's enzymes; secondly, breast milk contains a lot of secretory immunoglobulin A, which protects the intestinal mucosa from large molecules of allergens; thirdly, milk contains enzymes for digesting its own components and, finally, it is the best prevention of dysbacteriosis.
Formula-fed and formula-fed babies should reduce their intake of cow's milk protein as much as possible. It is necessary to ensure that the mixtures used are adapted, up to 1/3 -1/2 of the daily diet can be fermented milk mixtures. Even if such feeding causes allergic reactions, the child should be transferred to mixtures prepared on the basis of soy.
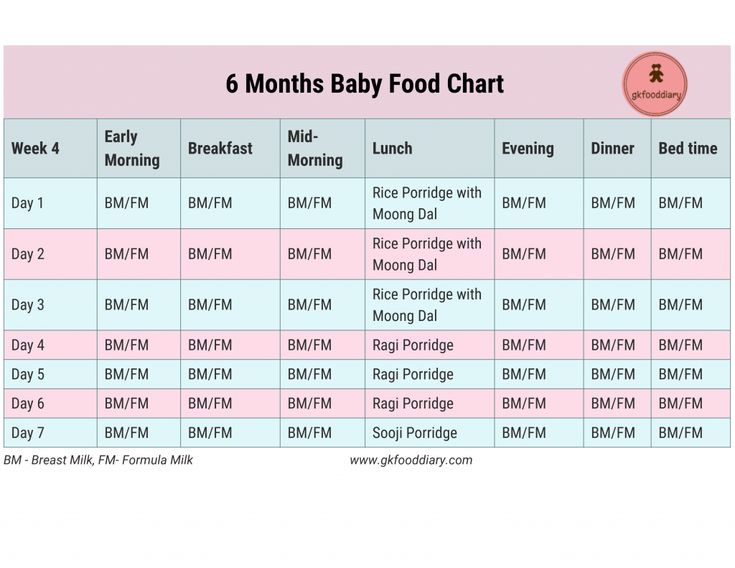
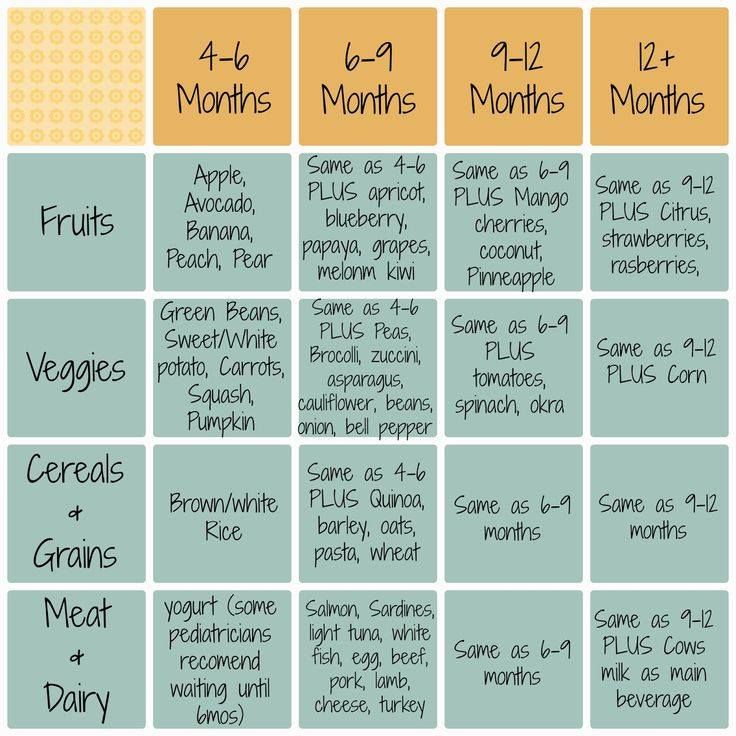
Further, when introducing cereals and vegetable puree, they should be prepared not with milk, but on the basis of a mixture suitable for the baby or vegetable broth, and for drinking, use kefir (from 7 months), yogurt (from 8 months), other fermented milk products.
Foods that individually cause allergic reactions are excluded from the diet of the baby and the nursing mother (in addition, nursing mothers should not overload their diet with fresh milk products - it is better to replace them with sour-milk ones).
It has been proven that the condition of children with allergic diathesis worsens with excessive consumption of carbohydrates. Sugar in the diet should be replaced with fructose (in a ratio of 1 to 0.3, since fructose is sweeter).
Medications are sometimes given to children with food allergies. This, above all, concerns vitamin therapy. During the period of exacerbation of allergic reactions, short courses of various antihistamines are carried out. I would like to remind you that the doctor who observes the child and knows the dynamics of his disease should prescribe the treatment.
Proper care of affected skin is very important. With dry skin, baths with wheat bran, children's medical cosmetics (milk, cream) with skin-moisturizing components give a good effect. Diaper rash is lubricated with special creams with a high content of zinc oxide or anti-inflammatory substances. With pronounced weeping, a decoction of oak bark can be added to the bath.
Diaper rash is lubricated with special creams with a high content of zinc oxide or anti-inflammatory substances. With pronounced weeping, a decoction of oak bark can be added to the bath.
Allergy in children. What do you need to know?
Often on the skin of young children there are spots, sores - a rash, and unfortunately, in the vast majority of cases this is an allergy. What is this attack?
Allergy is an inadequate reaction of the body to a completely normal substance. The causes of allergies are different and not always clear (hereditary predisposition to allergies, metabolic features, aggressive environmental influences). In the body of a child, when ordinary, for many other people, harmless substances enter, painful manifestations begin - allergic inflammation of the skin, mucous membranes.
Allergy is the body's reaction to a foreign protein, as well as to some non-protein substances (so-called haptens), which enter the blood from the digestive system, combine with blood proteins there, as a result of which these own proteins acquire foreign properties.
Most often, the first "foreign" protein in a baby's diet is cow's milk protein. His child receives when feeding with milk mixtures. Then the danger lurks with the introduction of complementary foods. Allergens can also enter the child during breastfeeding, if they are present in the diet of a nursing mother.
So-called obligate allergens are now well known, ie. foods with high allergenic properties: fish, chicken eggs and meat, nuts, citrus fruits, strawberries, etc. (see table).
Black currants
melon, grapes, pomegranates, pineapples
cocoa, chocolate, coffee
tomatoes, beets
wheat, rye
Rabbit
Red crus
Peaches
Apricots
Potatoes
Buckwheat
Oats, rice, corn
Peas, beans, beans, soybeans
Bananas
906Rosehip
Konina
Baranina
zucchini, Patissons, pumpkin (light tones)
White cabbage, Broccoli
Cucumbers
9004 BEALE
BEALE TRAROROP Blueberry
Gooseberry
Plum
Watermelon
Almond
Dill
In addition to products with high allergenic properties, there may be individual, allergenic properties. absolutely any food products for each specific child.
absolutely any food products for each specific child.
Many foods have common allergenic particles, so the so-called "cross" allergy should be considered: milk ↔ beef ↔ digestive enzymes; mold fungi ↔ kefir ↔ cheese ↔ yeast baked goods ↔ fruits of the last season; plant pollen ↔ fruits ↔ berries.
Allergens can enter the child's body not only with food, but also through breathing, through contact with the skin. However, in the 1st year of life, the first allergic "attack" on the baby is his food.
The severity of skin lesions may vary. The most minimal manifestations are oily seborrheic scales on the scalp, slight redness and dryness of the cheeks. Already these signs should alert parents, because. indicate an allergic mood, a child's tendency to allergies, the need to follow a diet.
Skin manifestations of food allergy are varied and may be acute or chronic.
A disease when, after eating a causally significant product, blisters suddenly appear on the skin as if from a nettle burn - this is urticaria .
These blisters may appear once, or periodically disappear and appear in a new place.
When allergic inflammation also affects mucous membranes, edema develops ( Quincke's edema - this is the diagnosis).
In infants, it most often occurs on the lips, cheeks, eyelids, scrotum, hands and feet. The most dangerous swelling of the larynx, manifested by coughing, hoarseness, shortness of breath. Without emergency assistance, death from suffocation is possible.
With such a form of food allergy as strophulus , red inflamed bumps (papules) appear on the skin of the trunk, limbs, buttocks, face, or bumps with a bubble inside (vesicles), the baby is worried about severe painful itching.
Scratching the skin leads to bacterial infection ( pyoderma ).
A more severe form of acute allergy - polymorphic-exudative erythema : various elements of the rash appear on the skin, often large, confluent, rounded or irregular in shape, red-pink and even bluish, migrate over the skin.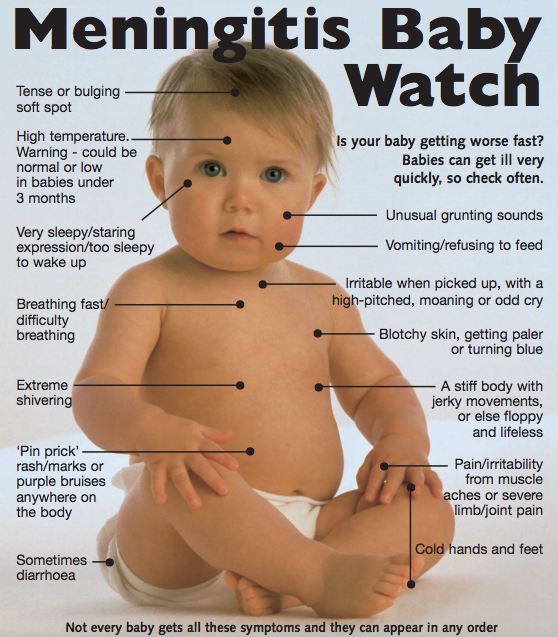
Against the background of these elements of the rash, blisters can also form!
In case of even more severe course ( Stevens-Johnson syndrome ) blisters on the skin are large, multiple, the epidermis of the skin exfoliates, the mucous membranes of the oral cavity, nose, eyes, genital organs are affected, pronounced symptoms of intoxication are observed, the child's condition is severe.
The disease is deadly, often accompanied by the addition of a secondary infection, the development of sepsis.
Chronic inflammation of the skin of an allergic nature - atopic dermatitis - also has a variety of manifestations.
It usually begins at 2-4 months, more often when the child is transferred to artificial feeding. Usually the first manifestations are on the skin of the face: redness and peeling of the cheeks, or red spots with peeling on the forehead, cheeks, temples, chin. Bubble elements may appear on the face and scalp, which burst after a while, causing profuse wetting, then blood crusts form.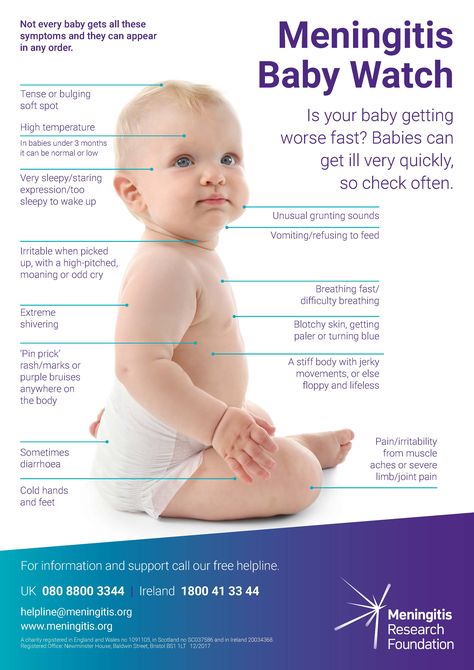 Over time, elements of the rash appear on the skin of the extremities, can be on the buttocks, on the trunk. Skin lesions may be accompanied by itching, aggravated in a hot room, at night, with the child's anxiety. In some children, persistent diaper rash is an early sign of a food allergy, even with careful skin care.
Over time, elements of the rash appear on the skin of the extremities, can be on the buttocks, on the trunk. Skin lesions may be accompanied by itching, aggravated in a hot room, at night, with the child's anxiety. In some children, persistent diaper rash is an early sign of a food allergy, even with careful skin care.
Atopic dermatitis proceeds in waves, exacerbations occur when a child eats a causally significant allergen. "Guilty" is usually 1-2 products, multiple (polyvalent) allergy in infants is rare. Removing the “guilty” product from the diet of an infant or a nursing mother has a positive effect on the skin condition and helps in diagnosis. To confirm the diagnosis, to identify causally significant allergens, an allergological examination is performed.
Often, skin manifestations of food allergy are combined with disorders of the gastrointestinal tract. There may be abdominal pain (intestinal colic), stool disorders, vomiting. Signs of allergic lesions of the respiratory system in the first year of life are much less common than manifestations from the skin and digestive tract, however, some children develop allergic rhinitis, bronchial asthma, and laryngitis already in infancy.
How can you protect your baby from food allergies? And what if it already exists?
The ideal food for your baby, invented by nature itself, is breast milk! It is advisable to make every effort to preserve and maintain lactation in the mother when a child appears. The gastrointestinal tract of a newborn is more permeable, liver and intestinal enzymes are immature, which is why babies are so prone to food allergies, and therefore the later the child begins to learn new foods, the less likely they are to become allergic to them. It has been proven that breastfeeding only up to 6 months fully meets the needs of the child and reduces the likelihood of sensitization. Naturally, during breastfeeding, the mother should adhere to a hypoallergenic diet. If it is impossible to breastfeed children with food allergies, the doctor will select a hypoallergenic mixture, depending on age, severity of skin manifestations, fortunately, the choice of such mixtures is now quite large.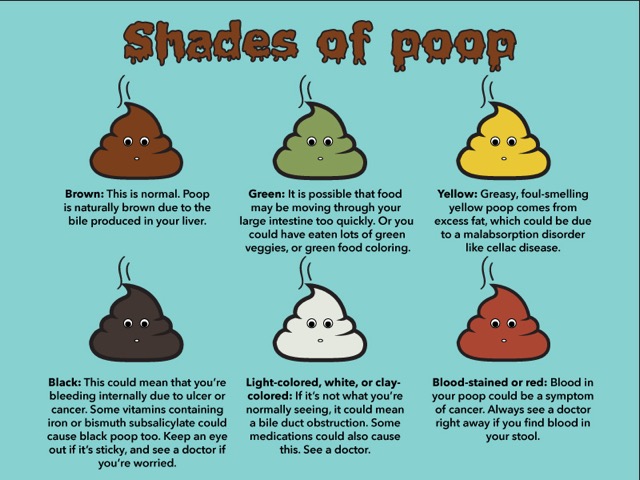
When introducing complementary foods, a number of rules should be followed. We are the first to offer the child one-component dishes (only from one product). If an allergic reaction occurs, it will be easy to calculate the “culprit” and exclude it from the diet. Dairy-free, gluten-free (rice, buckwheat, corn) porridge is recommended as the first porridge, which we cook with breast milk or a hypoallergenic mixture. We also offer single-component vegetable and fruit dishes. We choose products according to the so-called “traffic light rule”: green - you can (for example, zucchini, cabbage, apples), yellow - with caution (peaches, bananas, pumpkin), red - you can’t (carrots, tomatoes, strawberries). From meat products, rabbit, horse meat, lean pork, turkey are preferred. Children with food allergies in the first year of life are not introduced into the diet of cottage cheese, chicken yolk, and fish. Sweets should be limited, if it is impossible to completely abandon sugar, it is recommended to add fructose to food.
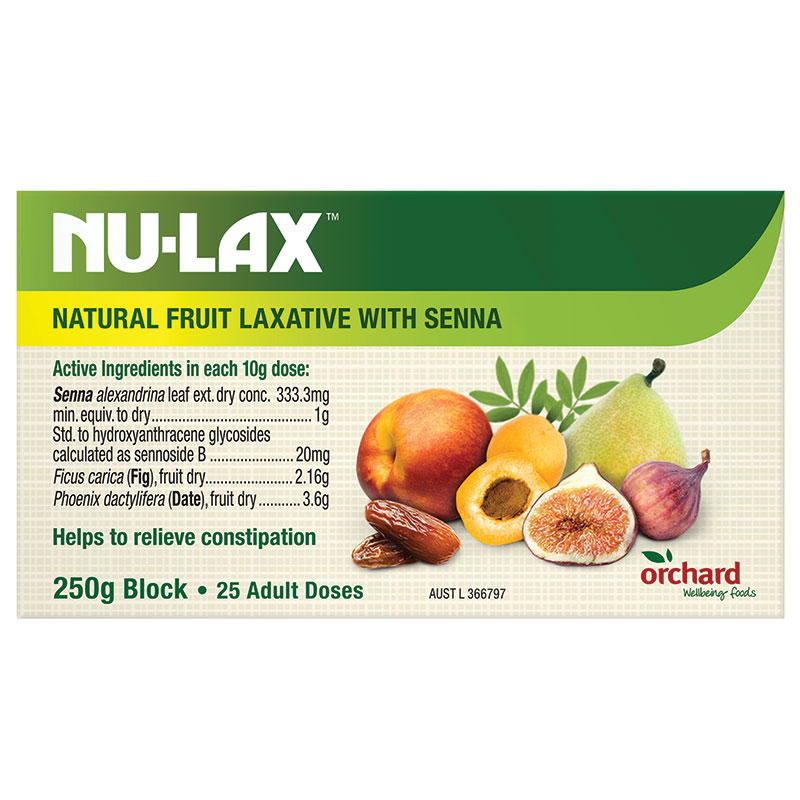
The child's diet must be balanced, overfeeding is unacceptable the immature digestive tract of the child will not cope with the “excess” food, the absorption of undigested, incompletely split substances into the blood will occur, which will contribute to allergies. For the same reason, it is necessary to strictly monitor the timely bowel movements of your baby.
In children of the first year, food sensitization is the starting point. Against its background, in the future, an allergy to household, epidermal, then to pollen allergens is often formed. For prevention of expanding the spectrum of allergens it is important to reduce or eliminate them from the environment of the child, i.e. create a healthy hypoallergenic atmosphere in your home . What it is?
Smoking is not allowed in the room where the child is. Yes, and exits to smoke on the balcony, the corridor is not a salvation, because. on his skin, hair, clothes, with exhaled air, a smoking adult brings a whole bunch of substances toxic to a child to a child.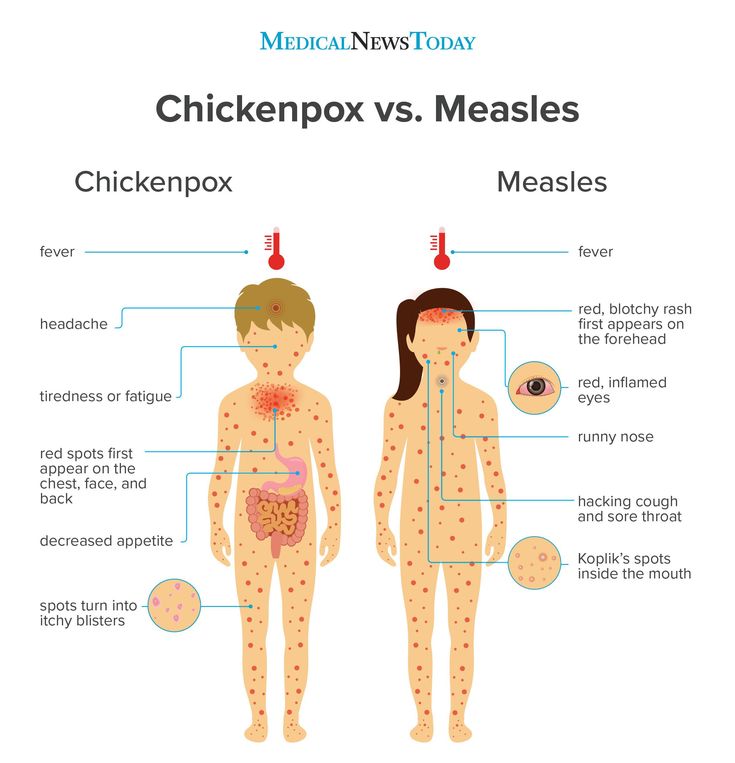 To approach a child after smoking, an adult needs to take a shower, change clothes, and brush their teeth. Isn't it easier (and healthier for everyone) to quit smoking?
To approach a child after smoking, an adult needs to take a shower, change clothes, and brush their teeth. Isn't it easier (and healthier for everyone) to quit smoking?
Dust needs to be controlled at home as this is a favorite habitat for dust mites, whose scales are a powerful allergen. Therefore, surrounded by a child, a TV and a computer, carpets, fleecy upholstered furniture are unacceptable. Soft toys are undesirable, they need to be washed periodically and placed in a freezer to kill ticks.
For the same reason, baby's bedding should be synthetic-filled, not down, feather or wool, and should be dried daily and cleaned periodically with anti-mites (acaricides).
Clothing made from wool and animal fur must be avoided, and synthetics are also undesirable. The best for baby's skin is 100% cotton or linen. To wash children's things, you need to use special children's hypoallergenic products, preferably liquid ones (because they rinse out better). After washing, the last rinse is recommended to be carried out in chlorine-free water - filtered or boiled.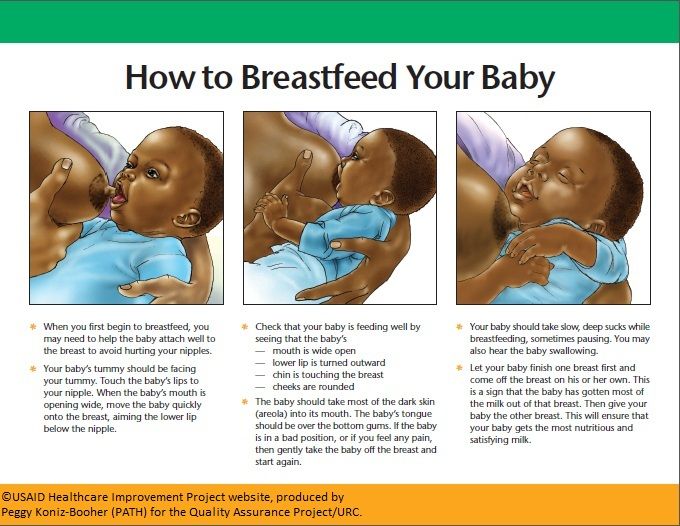 In the same way, it is desirable to wash the things of adults that come into contact with the skin of a child, for example, when they take him in his arms.
In the same way, it is desirable to wash the things of adults that come into contact with the skin of a child, for example, when they take him in his arms.
No pets allowed.
Keep your child away from pollen producing plants. Molds live in the land of indoor plants (and they are allergenic!), so flowerpots must be removed from the child's room. Also, mold on the walls is unacceptable.
In children with atopic dermatitis, proper skin care is of great importance , moisturizing is especially important. The baby is shown daily hygienic baths, skin softening after bathing and several times during the day with special care products. Moisturizers and emollients should be applied to the skin of the child as many times during the day as necessary. For hygienic care, special products of various cosmetic series are recommended, for example, Bioderma, Ducret, Aven (France). Bathe the child daily. The duration of bathing should be at least 15-20 minutes (this is necessary to saturate the stratum corneum of the skin with water), t about water 35-36 about hot water exacerbates the skin process. Chlorinated water should be defended, followed by heating or adding boiling water. Ordinary children's toilet soaps and shampoos are unsuitable; special soaps are needed, for example, with cold cream, which do not have a drying and degreasing effect. After bathing, the skin should be blotted with a towel without wiping dry, and within 3 minutes after bathing, without leaving the bathroom, apply a moisturizing and softening care product to slightly damp skin.
Chlorinated water should be defended, followed by heating or adding boiling water. Ordinary children's toilet soaps and shampoos are unsuitable; special soaps are needed, for example, with cold cream, which do not have a drying and degreasing effect. After bathing, the skin should be blotted with a towel without wiping dry, and within 3 minutes after bathing, without leaving the bathroom, apply a moisturizing and softening care product to slightly damp skin.
For the skin of a child with allergic manifestations, a cool, humid atmosphere is favorable , so it is recommended to ventilate the room often, wash the floor frequently, and maintain high humidity (a household air humidifier is optimal). The number of clothes on the child should be minimal. It is desirable to walk on the street as much as possible!
Medical treatment is of secondary importance, because The most important thing in an allergic disease is the elimination of the cause.