Baby not latching after bottle feeding
How to Get Baby Back to Breast
Sometimes breastfeeding doesn’t get off to a good start and before you know it your baby is taking more and more bottles and won’t breastfeed at all. Getting a baby back to breastfeeding after a period of bottle feeding can take some patience and perseverance, but it is definitely possible. If your breast milk supply has dropped then in addition to getting baby from bottle to breast you may have to build your milk supply or relactate. This article reviews how to get baby back to breast after a period of bottle feeding.
Find an IBCLC
Search for a breastfeeding expert near you
Tips to get started
- Build your breast milk supply by regular pumping or hand expression as needed or see our Tips for Relactation
- Keep your baby well fed while he practices breastfeeding so he doesn’t learn to associate hunger and frustration with the breast. Being hungry won’t force a baby to breastfeed well.
- Stay calm—practice breastfeeding without pressure, relax your shoulders and try not to look tense, smile! Follow your baby’s cues if he seems stressed and try again at another feed.
- Be patient—it can take a while for a baby to learn something new but lots of babies have made the change from bottle to breast. Never try to force your baby to the breast as this will be counterproductive.
How to get baby back to breast
Skin-to-skin
Babies have a strong instinct to breastfeed and their instincts tend to be at their strongest when they are held close to the breast in skin-to-skin contact. Try holding your baby next to the naked breast without pressure to latch on (attach to the breast). The fewer clothes between you the better.
- Remember to take off any scratch mittens so your baby can use his hands and tune into all his natural feeding reflexes.
- Relaxing in the bath together in low lighting with your baby between your breasts can encourage feeding reflexes.

- Using a sling around the house can give your baby easy access to the breast.
- Don’t worry if your baby doesn’t try to latch during his first time skin-to-skin—the important thing is to help your baby associate the breast with a warm, relaxing and safe place to be with the opportunity to breastfeed when he is ready.
Try different breastfeeding positions
The way a baby is held at the breast can help or hinder latching. In the right position many babies can latch on all by themselves. Laid back or reclining positions can be particularly helpful with self latching. Our articles Breastfeeding Positions for Newborns and Breastfeeding Videos describe the main breastfeeding positions. If you’re not sure of the best way to hold your baby, contact your breastfeeding helper or IBCLC Lactation Consultant, it will really help to have an experienced cheer leader at your side.
Avoid using a dummy or pacifier
A dummy or pacifier encourages a different suck to the one required for a good latch on the breast and also takes the place of the breast as main comforter. Try to reduce reliance on a dummy by offering the breast and skin-to-skin contact as the comfort for your baby instead. Letting a baby suck on a clean finger can also help to introduce a baby to the feeling of skin in their mouth as a comforter instead of a silicone teat.
Try to reduce reliance on a dummy by offering the breast and skin-to-skin contact as the comfort for your baby instead. Letting a baby suck on a clean finger can also help to introduce a baby to the feeling of skin in their mouth as a comforter instead of a silicone teat.
Avoid using a bottle for some or all feeds
One way to encourage a baby to breastfeed is to reduce their reliance on a bottle teat to pave the way for a different feeding method. Alternatives such as cup feeding or finger feeding can encourage breastfeeding by helping to break a baby’s association of food with artificial teats.
- Cup feeding. Even very young babies can feed from an open cup when it is done carefully see Cup Feeding a Breastfed Baby for videos and more information.
- Finger feeding. Finger feeding involves a baby sucking a parent’s finger with a narrow gauge supplemental feeding tube held or taped alongside, through which the milk flows when baby sucks.
 The sucking technique needed for finger feeding is said to be closer to breastfeeding than bottle feeding, and finger feeding can introduce a baby to the feeling of skin in their mouth instead of a silicone teat. See What is Finger Feeding? for more information. After a little finger feeding to calm your baby and take the edge off his appetite, you could try moving him to the breast. Ensure your breast is soft and not over full to help him grasp the breast tissue to form a teat shape.
The sucking technique needed for finger feeding is said to be closer to breastfeeding than bottle feeding, and finger feeding can introduce a baby to the feeling of skin in their mouth instead of a silicone teat. See What is Finger Feeding? for more information. After a little finger feeding to calm your baby and take the edge off his appetite, you could try moving him to the breast. Ensure your breast is soft and not over full to help him grasp the breast tissue to form a teat shape.
Make a bottle feed more like a breastfeed
If you can’t avoid bottles yet, try to make bottle feeding more like breastfeeding by following these tips to bottle feed a breastfed baby. When bottle feeding is more similar to breastfeeding it can help a baby transition between the two ways of feeding more easily. The shape of the teat, the flow rate and the way you offer milk in a bottle can help or hinder breastfeeding. Some mothers hide the bottle in a cloth and keep baby next to a naked breast during their feed to help them associate the breast with milk.
Nipple shields—make a breast more like a bottle
Nipple shields are small silicone covers with holes in the tip that fit over a nipple. Because a nipple shield will feel and taste closer to a bottle teat this can be a helpful bottle-to-breast transitioning tool for babies who are already used to bottles. It may be helpful to try it when your baby is sleepy or in light sleep and with a breast full of milk. Expressing a little milk into the end of the shield will give your baby an instant reward if he latches. Some breast compressions can help keep your baby’s interest if he does latch. Breast compressions involve applying gentle pressure to your breast to stimulate milk flow—be sure to keep your fingers far enough from your nipple so that you don’t disturb your baby’s latch. See Nipple Shields Good or Bad? and What is Breast Compression? for further information.
Some mothers have had success with latching by placing a bottle teat over their nipple for a practice session. Make sure this doesn’t rub and make you feel sore.
Make sure this doesn’t rub and make you feel sore.
A sleepy baby may latch
When your baby is in a light sleep or not frantically hungry bring him skin-to-skin next to a full breast; he may latch in his sleep. Or hold your baby for a full sleep cycle in your arms and offer the breast when you see the earliest feeding cues. It can help if you can initiate the let-down (milk release) before your baby goes on to the breast so that there is an instant reward of milk. If your baby latches, some gentle breast compressions can increase milk flow. A dark and quiet room can be helpful to avoid distractions for your baby. See Bed-Sharing With Baby for safety information if you are considering bed-sharing.
Try switching between bottle and breast
Switching from a bottle to the breast half way through a feed has worked for some mothers by slipping the bottle teat out of baby’s mouth and quickly moving them onto the breast before they notice. If baby hesitates at the feel of skin in their mouth a little gentle rocking or movement can encourage them to continue with the latch.
Use play and humour
For a slightly older baby, using new positions in a playful way may help turn breastfeeding into more of a casual fun thing, rather than an activity that creates tension and anxiety. Trying different positions and places for latching on—in the bath, the garden, kitchen, while walking about, in a dark room, even dangling a breast over him when he is on the floor (while you both giggle)—may all help make it more of a fun thing to do. Sometimes being inventive and making a silly game involving breastfeeding may work.
Watch other mothers and babies breastfeed
It can be helpful to spend time with other breastfeeding mothers for support and ideas. An older baby may be interested to copy other babies breastfeeding.
ⓒEmily WalkerOnce your baby latches…
Full breast or empty breast?
Try to strike a balance between offering a soft breast which will be easier for a latch, and a breast that is full enough to give an instant reward of plentiful milk. Shaping your breast ie compressing it/flattening it slightly to fit your baby’s mouth can help your baby latch (i.e. the same way you might flatten a big sandwich full of lettuce before you take a bite). See Latching Tips for further help.
Shaping your breast ie compressing it/flattening it slightly to fit your baby’s mouth can help your baby latch (i.e. the same way you might flatten a big sandwich full of lettuce before you take a bite). See Latching Tips for further help.
Stay relaxed
The first time your baby latches to the breast will be very exciting, you may find you tense up or hold your breath. Try to relax and act like this is natural and nothing special! You could sway slightly or rock your baby gently at this point. Some mothers have tried singing or chatting to their baby while their little one latches. The next step is providing an instant reward for any suckling, either via a full breast and an already initiated let-down or by breast compressions or with a supplemental nursing system (see below). As soon as your baby is taking good volumes at the breast try to phase out using the bottle for any top-ups so your baby can learn to breastfeed without nipple confusion.
Supplemental nursing system
If your milk supply is very low, supplementing at the breast with a homemade or commercial supplemental nursing system can help transition baby back to breast once they begin to latch. If your baby is latched correctly the thin feeding tube of the supplementer runs alongside the nipple or nipple shield delivering plenty of breast milk or formula. This helps give your baby a positive association with the breast as a food source and will also stimulate your own supply simply by baby being latched on. It can be fiddly and take some practice, and bear in mind an older baby may be aware of the tube at first. See Breastfeeding With a Supplemental Nursing System for more information.
If your baby is latched correctly the thin feeding tube of the supplementer runs alongside the nipple or nipple shield delivering plenty of breast milk or formula. This helps give your baby a positive association with the breast as a food source and will also stimulate your own supply simply by baby being latched on. It can be fiddly and take some practice, and bear in mind an older baby may be aware of the tube at first. See Breastfeeding With a Supplemental Nursing System for more information.
Finish at the breast
If your baby is still having supplements by bottle but has started to latch, it can sometimes work well to offer most (but not all) of the supplemental feed first and then finish with a breastfeed. This way a baby learns to fall asleep full and contented at the breast. As your supply increases and baby’s technique improves less supplement can be offered before the feed so that the bottle is gradually phased out.
If breastfeeding hurts…
Working with an IBCLC lactation consultant when you are trying to get your baby back to the breast can be a great support. There may be good reasons why breastfeeding didn’t work out the first time and it can help a great idea to talk these through. Maybe it was because breastfeeding hurt because your baby was in a shallow latch, or you didn’t think you had enough milk, or you had flat or inverted nipples. Knowing answers to common problems can help prepare you for any blips in your bottle-to-breast journey. Your lactation consultant will be able to make suggestions to improve latch, positioning and tongue function.
There may be good reasons why breastfeeding didn’t work out the first time and it can help a great idea to talk these through. Maybe it was because breastfeeding hurt because your baby was in a shallow latch, or you didn’t think you had enough milk, or you had flat or inverted nipples. Knowing answers to common problems can help prepare you for any blips in your bottle-to-breast journey. Your lactation consultant will be able to make suggestions to improve latch, positioning and tongue function.
Trouble shooting
Baby crying, arching and pulling away?
Sometimes a baby may seem quite distressed by breastfeeding or even the thought of breastfeeding. He might arch his back and pull away from the breast every time his mother tries to latch him, he may get very upset and cry. This might happen when a baby associates a negative experience with breastfeeding such as being pushed onto the breast when he is upset/crying or having their head held in position when they are trying to get away from the breast.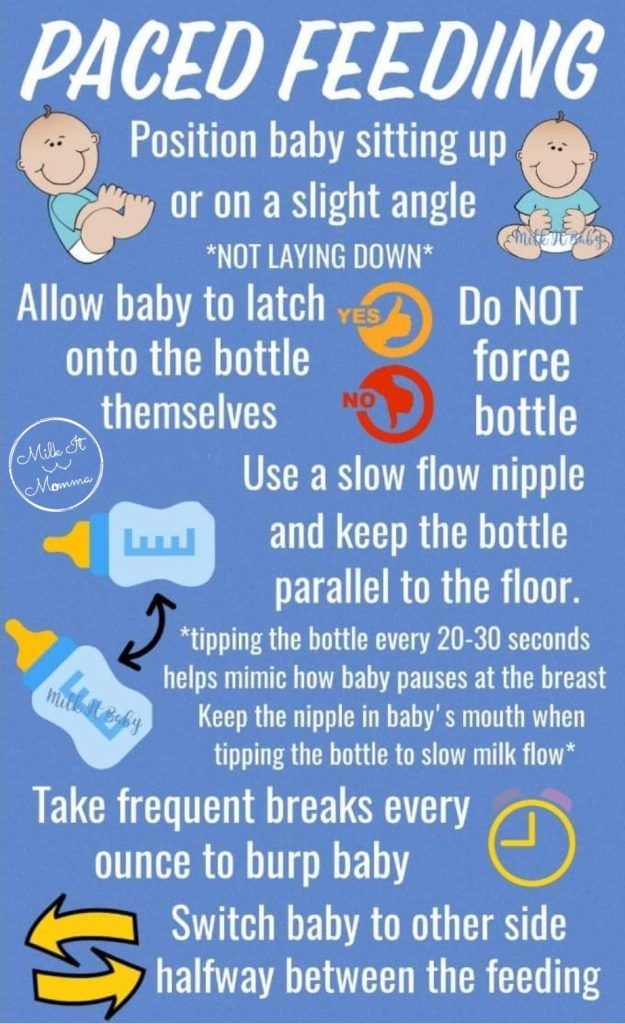 Sometimes well meaning health professionals can cause this by their attempts to make a baby to breastfeed. Or a mother may inadvertently perpetuate it by repeating the technique. Once a baby is upset, a mother will get upset too and the tension around breastfeeding can be reinforced with every feed. Taking a short break from trying to breastfeed can help to break this negative pattern.
Sometimes well meaning health professionals can cause this by their attempts to make a baby to breastfeed. Or a mother may inadvertently perpetuate it by repeating the technique. Once a baby is upset, a mother will get upset too and the tension around breastfeeding can be reinforced with every feed. Taking a short break from trying to breastfeed can help to break this negative pattern.
Take a break
Taking a break from trying to breastfeed for a few days might feel counterproductive, but making breasts a happy place (mamaandbabylove.com) can reset your baby’s bad memories. Substitute breastfeeding efforts with lots of skin-to-skin contact without any pressure on your part to get your baby to latch. Try breastfeeding again in a few days using breastfeeding positions that give your baby more control of how and when to latch. Christina Smillie describes a step by step approach in her handout Time Off to “Reboot” the Baby and Get Over Breast Distress.
Stay calm
Babies breastfeed best when they are calm and alert. Choose a moment to try breastfeeding when your baby is calm, and help your baby stay calm by talking to him, reassuring him, maintaining eye contact and staying calm yourself 1.
Choose a moment to try breastfeeding when your baby is calm, and help your baby stay calm by talking to him, reassuring him, maintaining eye contact and staying calm yourself 1.
Summary
Just as many breastfed babies can be persuaded to take a bottle, it is possible to get a baby to take the breast after a period of bottle feeding. It can take some patience and perseverance but there are several tips and tricks to try even if your baby is several weeks or months old.
Footnotes & References
-
Breast Distress, Breast Refusal, Oral Aversion and Total Freakout, Christina Smillie, LCGB Conference 2017
What is Finger Feeding? - Breastfeeding Support
Finger feeding involves a baby receiving breast milk or formula via a very narrow feeding tube while they suckle your finger. When a baby sucks on finger and tube together with their tongue in the right position, and with their lips making a seal on the finger, milk is drawn up the feeding tube from a container of milk. A curved tip syringe can also be used to drip milk into a baby’s mouth alongside the finger instead of a tube. Finger feeding is an alternative to using a bottle or cup if a baby needs a supplement and it can also be used as a suck training technique. This article looks at the ways finger feeding can be useful, how to do it, and the pros and cons with this technique.
When a baby sucks on finger and tube together with their tongue in the right position, and with their lips making a seal on the finger, milk is drawn up the feeding tube from a container of milk. A curved tip syringe can also be used to drip milk into a baby’s mouth alongside the finger instead of a tube. Finger feeding is an alternative to using a bottle or cup if a baby needs a supplement and it can also be used as a suck training technique. This article looks at the ways finger feeding can be useful, how to do it, and the pros and cons with this technique.
Sign Up to the Newsletter
Get breastfeeding articles in your inbox
Advantages of finger feeding
When a baby needs supplementary feeds, some authors feel that finger feeding may help to preserve the breastfeeding relationship compared to cup feeding or bottle feeding. Reasons include:
- Finger feeding uses a similar sucking technique to breastfeeding ie the same muscles are used and both methods allow the baby to control the flow of milk and pace the feed.
 1
1 - Finger feeding promotes skin-to-skin contact (between tongue and finger) and the finger tip reaches the same position deep in the mouth as the nipple (Wambach and Spencer, 2021).
- Finger feeding avoids introducing nipple confusion or bottle preference before breastfeeding is well established which can sometimes happen with the use of artificial teats. Note: Although there are differences between breastfeeding and bottle feeding, bottle preference and nipple confusion can be minimised by these Tips to Bottle Feed a Breastfed Baby and see Best Bottle for a Breastfed Baby? If used regularly, babies could equally have “finger preference” and reject the breast in favour of a finger feed.
When is finger feeding useful?
Finger feeding can be useful in a number of situations:
#1 To feed a baby
- Finger feeding keeps a baby well fed if they are not latching (attaching) to the breast, not breastfeeding well, or refusing a bottle.

- Separation from mother. If a breastfed baby is separated from their mother, finger feeding could be a feeding option to consider alongside cup feeding, syringe feeding or bottle feeding. One study of 53 babies showed preterm babies who were finger-fed had less milk loss, and fewer complications compared with cup feeding.2
#2 When baby won’t latch
- If a baby can’t latch to the breast yet, finger feeding may help to prepare a baby for breastfeeding3 because the sucking technique needed is similar to that which will be used at breast. For more reading see When Baby Won’t Breastfeed.

- Finger feeding can be used to wake up a non-latching sleepy newborn baby to give them some calories4 or to calm a hungry and frustrated baby and take the edge off their appetite before latching. Note: a baby who is very sleepy or has low stamina from being underweight may struggle to take adequate volumes with finger feeding as a sole method of supplementation and careful use of a bottle and teat may be more appropriate.
#3 Improving sucking skills
Because finger feeding has similarities to breastfeeding, finger feeding is sometimes suggested as a suck training technique to improve sucking skills or tongue function (see below).5 Finger feeding is said to reinforce good breastfeeding technique because:
- Baby has to keep his tongue down and forward in his mouth to cover his gums
- Baby uses a wide open mouth on the finger to recreate a deep latch—use your largest finger
- Baby has to suck actively to bring milk up the tube, just as he does at the breast to initiate a let-down (milk ejection reflex)
- Baby can control the flow of milk, if he doesn’t suck there will be a pause in milk flow
- Baby becomes familiar with the feel of skin in their mouth rather than a silicone teat.

#4 Respite from sore nipples
Finger feeding can be used for a day or two if a mother’s nipples are too sore and damaged to breastfeed to give them a chance to heal without introducing bottles. However, Jack Newman, a Canadian paediatrician and breastfeeding expert, cautions against interrupting breastfeeding unless absolutely necessary as sometimes a baby can be reluctant to go back to the breast.6 Breastfeeding can often continue uninterrupted with sore nipples once positioning has improved the latch. See Causes of Sore Nipples and Treatments for Sore Nipples for help for sore nipples.
Finger feeding is when a baby gets milk from a narrow feeding tube while they suckle on a finger or thumbDisadvantages of finger feeding
- Finger feeding is not appropriate for all babies. Some babies may find it difficult to get milk via the tube.
 Underweight babies may not have enough stamina to use the tube effectively. Alternatives include cup feeding or see our Tips to Bottle Feed a Breastfed Baby. If the baby can breastfeed, then additional milk can be given via feeding tube directly at the breast, see Supplementing at the Breast.
Underweight babies may not have enough stamina to use the tube effectively. Alternatives include cup feeding or see our Tips to Bottle Feed a Breastfed Baby. If the baby can breastfeed, then additional milk can be given via feeding tube directly at the breast, see Supplementing at the Breast. - Cleaning the tubes properly is difficult and could put your baby at risk of an infection. See Homemade Supplemental Nursing System for more information about cleaning homemade systems and see below.
- It can be quite awkward to finger feed especially if milk leaks in a homemade system and it can be difficult to source feeding tubes. Some babies figure out a way to suck on the tube like a straw rather than use a breastfeeding technique.
- The flow of milk may be too fast or too slow—however flow rate can be increased with a larger diameter tube, using two tubes, or by holding the container of milk above baby’s head. Flow can be decreased with a smaller diameter tube or lowering the position of the container.

- A sore mouth? If the tube is held on top of a finger it could rub against the roof of your baby’s mouth (the hard palate) potentially causing soreness. Having the tube running along the side of your finger may help so that the tube enters the corner of baby’s mouth instead of running across the hard palate.
- A finger is not the same as a breast, more research is needed on the safety and long term implications of finger feeding. For some babies finger feeding may negatively affect breastfeeding. Pushing a finger too far into baby’s mouth, or the tube extending further than a finger tip could cause gagging or discomfort. It’s important to watch your baby closely for signs of stress or they could start to resist anything entering their mouth—including a breast (oral aversion).
A step by step guide to finger feeding
Finger feeding is best shown in person by your IBCLC lactation consultant or health care professional. Detailed instructions for finger feeding can be found in Jack Newman’s article Finger and Cup Feeding or in Supporting Sucking Skills in Breastfeeding Infants or Breastfeeding and Human Lactation (2021. p 196). Information for using the Hazelbaker™ FingerFeeder can be found on fingerfeeder.com
Detailed instructions for finger feeding can be found in Jack Newman’s article Finger and Cup Feeding or in Supporting Sucking Skills in Breastfeeding Infants or Breastfeeding and Human Lactation (2021. p 196). Information for using the Hazelbaker™ FingerFeeder can be found on fingerfeeder.com
The steps for finger feeding with a feeding tube include:
- Trim long finger nails and wash your hands prior to finger feeding.
- Hold your baby so that he can comfortably suckle your finger when it is held flat in his mouth. Baby’s head should be stable and slightly tilted back (Wambach and Spencer, 2021).
- Hold the rounded end of a small feeding tube (e.g. 5fr or 6fr) along the side of your finger or tape it in position if preferred, the end of the tube should be close to but not extend past your finger tip. Use a large finger or thumb to fill a baby’s mouth like the breast (Wambach and Spencer, 2021).

- Check that the opposite end of the tube is submerged in your expressed breast milk or formula and that the cap on this end of the tube is open.
- Encourage a wide gape—by brushing your finger against your baby’s lips. Never force a finger into your baby’s mouth always encourage the gaping reflex first.
- Slide your finger gently along your baby’s hard palate so that the soft pad of your finger tip is uppermost and resting against the roof of your baby’s mouth. Let your baby take your finger into his mouth as far as he is comfortable—avoid going too far to cause gagging or discomfort. Your baby will normally grasp the finger with his tongue and suck it deeply into his mouth so that the finger pad rests towards the back of his mouth at the junction of the hard and soft palates—some authors call this the “S-spot”.7 The nail side of your finger should be centred against the tongue.
 If your baby seems to gag on even your finger tip, contact your IBCLC lactation consultant.
If your baby seems to gag on even your finger tip, contact your IBCLC lactation consultant. - Check your baby’s lips are not folded in, the top lip should rest on your finger making a seal and the lower lip be turned out. Pull on the chin gently just enough to bring the lip out if it is tucked in. If baby doesn’t have good lip seal, milk may leak from the mouth.
- Try to keep your finger straight or flat to help encourage the correct tongue position and without applying pressure to the roof of your baby’s mouth, only maintain gentle contact. Good contact with the centre of baby’s tongue and his hard palate recreates the right position of the breast and nipple in baby’s mouth.
- Your baby will receive milk via the feeding tube at his own pace and the milk will gradually be drained from the bottle or container. Milk delivery is stopped when the tongue pulls back or the back of the tongue is humped against the finger, and resumed when the tongue tip is brought back over the gum ridge and the back of the tongue drops slightly.
 If your baby isn’t motivated to keep sucking long enough to draw milk up the tube, the tube can be prefilled with milk by inserting a blunt ended syringe of milk into the cap at the end of the tube.
If your baby isn’t motivated to keep sucking long enough to draw milk up the tube, the tube can be prefilled with milk by inserting a blunt ended syringe of milk into the cap at the end of the tube. - Monitor baby for signs of stress (frowning, finger splaying, turning away) and check whether they are coping well with organising sucking, swallowing and breathing when feeding with the tube in place. Check that the tube is not rubbing against the roof of your baby’s mouth.
Finger feeding variations with a syringe
- A blunt ended syringe can be used to house the supplement at the end of the feeding tube. The advantage of this system is that the feeder can slowly push the plunger down on the filled syringe to maintain a steady flow of milk when baby is sucking; pausing as needed for baby to swallow or rest.
- A curved tip syringe can also be used to introduce milk along your finger while baby suckles.
The disadvantage of using a syringe is that it can be difficult to hold baby and negotiate finger feeding and pushing the syringe at the same time without another pair of hands. The feed may need to be interrupted to refill the syringe and it is important to regulate the flow of milk carefully so as not to choke or overwhelm the baby.
The feed may need to be interrupted to refill the syringe and it is important to regulate the flow of milk carefully so as not to choke or overwhelm the baby.
Finger feeding for suck training
Suck training is when exercises are used to improve a baby’s immature or suboptimal sucking technique to help them breastfeed (or bottle feed) more effectively. This may involve stroking movements/massage of the tongue or gums and finger feeding can also be used as a suck training exercise. Advocates of suck training feel it can help to optimise feeding reflexes eg the way the tongue moves during feeding and familiarise a baby with the desired position of the nipple deep in baby’s mouth. Conversely, authors Wambach and Spencer point out that some practitioners feel that suck training is invasive and controlling and should never be used.8
There are many versions of suck training that individual therapists favour but no standard protocols (Wambach and Spencer, 2021 p80). Decisions on specific exercises are best discussed with speech and language therapists (SALT), your lactation consultant or see the latest editions of text books such as Breastfeeding and Human Lactation and Supporting Sucking Skills in Breastfeeding Infants for a detailed overview.
Decisions on specific exercises are best discussed with speech and language therapists (SALT), your lactation consultant or see the latest editions of text books such as Breastfeeding and Human Lactation and Supporting Sucking Skills in Breastfeeding Infants for a detailed overview.
Cautions for suck training exercises
- Carry out suck training under the guidance of your IBCLC lactation consultant or other experienced health care professional eg a speech and language therapist (SALT). It is important to rule out positioning, attachment, mother’s anatomy, baby’s oral anatomy or even whether baby is very underweight to explain any breastfeeding issues before embarking on suck training. A therapist will choose appropriate exercises for specific suck issues.
- Mouth and tongue exercises should always be gentle and enjoyable for a baby. It’s important to be sensitive to your baby’s responses and stop an exercise if your baby is not enjoying it.
 Irritating your baby with intrusive exercises in his mouth could cause him to refuse anything in his mouth including a breast (called oral aversion).
Irritating your baby with intrusive exercises in his mouth could cause him to refuse anything in his mouth including a breast (called oral aversion). - If finger feeding exercises don’t help or a baby doesn’t seem to enjoy the exercises, another strategy should be considered. Contact your IBCLC lactation consultant.
The need for a full assessment
Finger feeding can be used as a form of suck training to help improve the way the tongue moves during feeding and encourage the tongue forward in the baby’s mouth (tongue extension) (Watson Genna, 2017; Marmet and Shell, 1984). A baby who doesn’t bring his tongue forward to cup the breast will find it harder to maintain suction on the breast and if the tongue isn’t extended over the lower gum ridge during a breastfeed, the mother may feel a biting sensation or complain of sore nipples. However there can be many simple explanations for “biting” or soreness hence the need to first rule out other causes of sore nipples with your breastfeeding specialist such as poor positioning, shallow attachment at the breast, high muscle tone, fast-flow, tongue-tie or hunger, before using sucking exercises.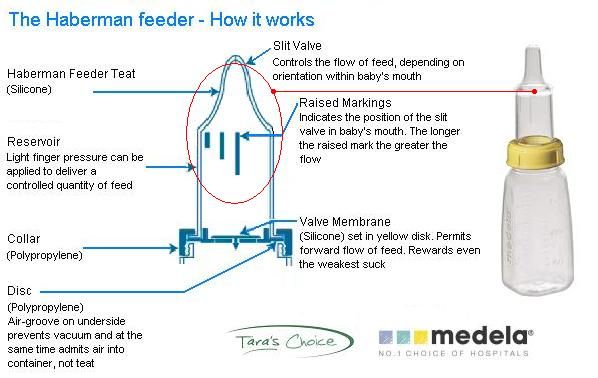
Where can I get a finger feeding supplementer?
It is possible to buy a purpose made finger feeder online called the Hazelbaker™ FingerFeeder (email [email protected]) or to use the tubes from a Medela Supplemental Nursing System. The instructions for making a homemade finger feeding tool for short term use can be found in Homemade Supplemental Nursing System. The equipment and the first four steps of “setting up” are the same as when making a homemade at-breast supplemental system.
Where can I get feeding tubes for a homemade system?
Your IBCLC lactation consultant may carry feeding tubes for finger feeding and plastic syringes to clean them, or they may know of a local supplier. Many medical suppliers in UK sell individually wrapped sterile feeding tubes (nasogastric tubes) by the box however it can be difficult for parents to source small numbers of tubes. Note: using a nasogastric tube for finger feeding is not using a device according to the manufacturer’s intended use. Nasogastric tubes are intended to carry milk to babies internally via the back of their nose and throat to the stomach. This means parents use tubes for finger feeding at their own risk without the protection of a manufacturer’s guarantee.
Nasogastric tubes are intended to carry milk to babies internally via the back of their nose and throat to the stomach. This means parents use tubes for finger feeding at their own risk without the protection of a manufacturer’s guarantee.
How can I clean the tubes?
While commercially made supplementers are made to withstand sterilising—disposable feeding tubes from a homemade system are not intended for reusing in this way and won’t stand up to boiling or steam sterilisation. See Homemade Supplemental Nursing System for cleaning information—tubes can be rinsed out straight after use by using a syringe in the end-cap to push cooled, previously boiled, water through the tube several times to remove milk.9 Some authors advocate flushing the tubes through with hot soapy water after removing the visible milk, and finally rinsing well.10 Residual water can be forced out of the tube by shaking the tube in a lasso action. Some mothers store washed tubes in a refrigerator between uses. Instructions for cleaning commercial devices will be supplied with the equipment or online e.g. see How Do I Clean the Hazelbaker™ FingerFeeder?
Some mothers store washed tubes in a refrigerator between uses. Instructions for cleaning commercial devices will be supplied with the equipment or online e.g. see How Do I Clean the Hazelbaker™ FingerFeeder?
Replace tubes regularly
If you are using a disposable feeding tube it should be replaced with a new tube frequently, some mothers use a new tube each feed or every day. If they are cleaned thoroughly however, Dr Jack Newman 11 suggests tubes can be washed and reused for a few days before replacing.
Baby receives milk via the feeding tube at his own paceIs long term finger feeding safe?
Finger feeding information does not seem to be based on any extensive research studies and relies on the experience of practitioners in the field who have used this technique. A breast widens a baby’s palate in a way that a bottle teat or finger can’t and tubes are difficult to clean properly. There is a risk of oral aversion if finger-feeding is not done respectfully.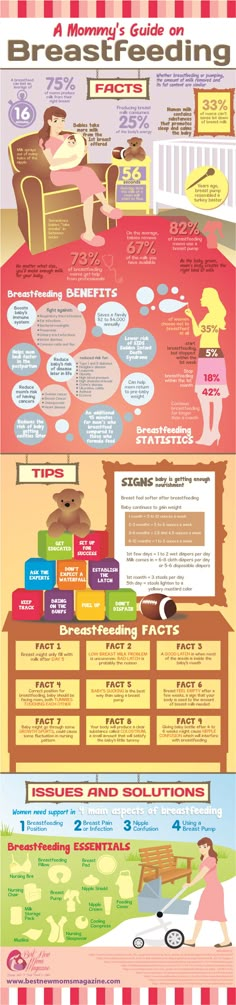 Until more research is available it would seem appropriate to limit finger feeding to short term use for encouraging a baby back to breast and suck training exercises under supervision. Alison Hazelbaker explains:
Until more research is available it would seem appropriate to limit finger feeding to short term use for encouraging a baby back to breast and suck training exercises under supervision. Alison Hazelbaker explains:
Excerpt from
FAQs, 2009, fingerfeeder.com
Breastfeeding still remains the ideal way to feed babies. Finger-feeding should be used only as a means to correct sucking problems or to keep the baby well fed until he or she can go to breast.
One study in Australia 12 found that finger-feeding as part of the feeding regimen ensured that a larger percentage of babies in the NICU were able to transition to breast successfully, whereas their bottle-feeding counterparts were less likely to do so. No other study has looked at finger-feeding.
Summary
Finger feeding is when a baby gets milk from a narrow feeding tube while they suckle on one of your fingers.![]() Variations include dripping milk into baby’s mouth with a curved tip syringe while they suckle on a finger, or pushing milk along the feeding tube into baby’s mouth via a reservoir of milk in a syringe. Finger feeding a baby can be an alternative to using a bottle or cup if a baby isn’t breastfeeding yet or needs supplements, and it can also be used as a suck training technique to improve a baby’s sucking skills. There isn’t any substantial research on the safety of finger feeding and most information has been provided through the experience of lactation consultants who have used finger feeding in their work. It is recommended to carry out finger feeding under the guidance of your IBCLC lactation consultant or other health care professional.
Variations include dripping milk into baby’s mouth with a curved tip syringe while they suckle on a finger, or pushing milk along the feeding tube into baby’s mouth via a reservoir of milk in a syringe. Finger feeding a baby can be an alternative to using a bottle or cup if a baby isn’t breastfeeding yet or needs supplements, and it can also be used as a suck training technique to improve a baby’s sucking skills. There isn’t any substantial research on the safety of finger feeding and most information has been provided through the experience of lactation consultants who have used finger feeding in their work. It is recommended to carry out finger feeding under the guidance of your IBCLC lactation consultant or other health care professional.
Footnotes & References
-
Wambach and Spencer. Breastfeeding and Human Lactation. 6e 2021 p 195
-
Moreira et al. Comparison of the finger-feeding versus cup feeding methods in the transition from gastric to oral feeding in preterm infants.
 J Pediatr (Rio J) 93(6):585-591, 2017
J Pediatr (Rio J) 93(6):585-591, 2017 -
Karabayir N, Mertturk Potak E, Karaman S, et al. (April 11, 2022) The Finger Feeding Method and Relactation. Cureus 14(4): e24044. doi:10.7759/cureus.24044
-
Finger and Cup Feeding, Jack Newman and Edith Kernerman, updated 2021
-
Buldur et al. Comparison of the Finger Feeding Method Versus Syringe Feeding Method in Supporting Sucking Skills of Preterm Babies. Breastfeeding Medicine. 2020
-
Finger and Cup Feeding, Jack Newman and Edith Kernerman,updated 2021
-
Training Neonates To Suck Correctly, Maternal Child Nursing, Marmet and Shell, 1984
-
Breastfeeding and Human Lactation, Wambach and Spencer, 2021 p80
-
Breastfeeding and Using a Supply Line, Royal Women’s Hospital, 2018
-
Counseling the Nursing Mother, Lauwers and Swisher, 2011
-
Lactation Aid, Jack Newman, updated 2021
-
Implementing the Baby Friendly Hospital Initiative: the role of finger feeding, Oddy and Glenn, 2003
What to do if the baby refuses to breastfeed after a bottle
Number of views: 17456
Sucking habit is inherent in babies by nature. A newborn who has been put to the breast knows what to do to get milk. In almost all children, this mechanism turns on automatically. In some cases, when the mother has problems, baby is first given a bottle of , after which baby refuses breast categorically. A similar problem can also arise if a nursing mother needs to leave and in her absence the baby will be fed with expressed milk from a bottle.
A newborn who has been put to the breast knows what to do to get milk. In almost all children, this mechanism turns on automatically. In some cases, when the mother has problems, baby is first given a bottle of , after which baby refuses breast categorically. A similar problem can also arise if a nursing mother needs to leave and in her absence the baby will be fed with expressed milk from a bottle.
Why baby won't latch on after a bottle
A bottle with a nipple is a breast substitute. But in fact, the process of sucking mother's breast is completely different from drinking from a bottle . A baby who is fed from a regular bottle is forced to activate completely different mechanisms and muscle groups than when breastfeeding.
A regular nipple is harder or too soft than a mother's breast. A bottle-fed baby often begins to pinch the nipple with his gums, and in the case of a bottle with a narrow neck, the baby stops making a wide latch - it is impossible to do a similar maneuver with a mother's nipple.
Also with breastfeeding, the baby opens his mouth wide and he has to make special peristaltic movements with his tongue to stimulate lactation. When the first feeding is done with a bottle, the child perceives this as the norm, and the breast seems to him a foreign object. Approximately the same problem awaits families where the baby is temporarily fed only from a bottle. As a result, the baby has "nipple confusion" .
How can the problem be solved?
Almost every parent has to use a baby bottle. There are bottles on the market today that are designed specifically for breastfeeding babies. Specially designed physiological nipples minimize the likelihood that the baby will refuse the breast. An example of such products is the Japanese brand Pigeon feeding bottles with an innovative physiological nipple that allows the baby to reproduce natural sucking movements. They differ from ordinary bottles in such qualities as:
- Wide base nipple - baby has to open her mouth as wide as breastfeeding
- Textured surface base of the nipple - allows the lips and tongue to easily glide over the surface like the skin of the breast (regular smooth silicone tends to stick).

- The diameter of the nipple matches the sucking hole - the Pigeon brand has four sizes nipples for babies of different ages
- Hole of the correct diameter - you have to suck as hard as your mother's breasts
- Special vent valve prevents air from entering the nipple, minimizing colic in the baby from swallowing air
- Sucking works the same muscles as breastfeeding.
Such a bottle will not create a problem with breast rejection and the mother will be able to go about her business without weaning her baby from breastfeeding, but at the same time she must monitor the constant support of lactation (!).
Pigeon bottles and nipples have been clinically tested to support breastfeeding at the Scientific Center for Children's Health of the Russian Academy of Medical Sciences (2013).
Breast milk is not only food for the baby, but also a way to calm down, to feel close contact with the mother. After breastfeeding is restored, you can also start using Pigeon bottles with an innovative nipple if you need to supplement.
After breastfeeding is restored, you can also start using Pigeon bottles with an innovative nipple if you need to supplement.
Have you experienced similar problems? Please share your opinion and experience in the comments!
comments powered by HyperComments
Bottle and breast: how to combine
Mother's milk is the best food for a newborn: it promotes the growth and development of the baby, supports his immunity. But sometimes there is a need for additional use of mixtures. In this case, breastfeeding and the bottle must be combined correctly - then the child will receive the necessary amount of nutrients, and mixed nutrition will not harm him.
When is the need for mixed feeding
The decision to supplement breastfeeding with the use of mixtures is the best solution when the mother of a newborn has to be away often and / or for a long time. If a woman does not want to express milk or cannot provide the required amount of it, the use of special nutrition, which involves bottle feeding, will help out.
The second reason why lactation is supplemented with the use of a mixture is the high appetite of the child, in which the baby does not have enough mother's milk. But there are also cases when the newborn has a normal, not increased appetite, but the woman does not produce enough milk, and the baby is not saturated. In this case, experts recommend breastfeeding and bottle feeding.
Why can a baby stop breastfeeding after a bottle? Differences in the way pacifiers and breasts are taken
The main reasons why babies may refuse mother's milk in favor of bottle feeding:
- Breast imperfections (tight, inverted nipples).
- Diseases of the tongue (this is important, because due to it the child absorbs mother's milk, and with the help of the cheeks - infant formula).
- Maternal irritability experienced by the newborn during breastfeeding.
- Sharp, unfamiliar smell from mother's skin.
- Improper attachment of the infant to the breast during feeding.

- Changes in the taste of mother's milk (for example, if a woman consumes spices, alcohol, coffee), which makes such food unpleasant for the child.
- Stress factor.
- Teething period.
If there is a need to return to breastfeeding, one way to teach to breastfeed after a bottle is to make the use of formula from a container less comfortable. To do this, you need to replace the nipple with a container, choosing the option with a smaller hole. To draw in the mixture, the baby will have to make extra efforts, while drinking mother's milk is an easy, convenient process.
If the baby does not latch on after the bottle, no effort is required to latch onto the nipple. This will lead to irritability, which can harm the condition of the breast and oral cavity of the newborn. It is more advisable to use simple but effective methods of how to return breastfeeding after a bottle - maintaining bodily contact with the baby, avoiding the use of pacifiers, sleeping together. Mom needs to understand that breastfeeding should be restored gradually, since a sharp refusal to use the mixture will have a stressful effect on the newborn. Also, so that the child does not wean from the mother's breast, it is necessary to supplement it not from a bottle, but from a sterile measuring syringe (without a needle). The adaptation of the child to the previous (natural) nutrition will come faster if the newborn has as much contact with the mother as possible during the day.
Mom needs to understand that breastfeeding should be restored gradually, since a sharp refusal to use the mixture will have a stressful effect on the newborn. Also, so that the child does not wean from the mother's breast, it is necessary to supplement it not from a bottle, but from a sterile measuring syringe (without a needle). The adaptation of the child to the previous (natural) nutrition will come faster if the newborn has as much contact with the mother as possible during the day.
Advice on how to start giving a bottle
Mothers who want to properly organize supplementary feeding should take into account the following nuances:
1. First of all, milk should be given to the newborn, and only after that - the mixture from the bottle.
2. The volume of the first supplementary feeding should not exceed 10-30 grams. This is necessary for the full adaptation of the baby to a new type of food.
3. At night, it is better not to bottle feed the baby.