Baby projectile vomiting after feeding
Children and vomiting - Better Health Channel
Summary
Read the full fact sheet- Mild vomiting is normal in most babies and improves over time.
- Most babies need only simple treatment, or none at all.
- Changing feeding and sleeping positions may help.
- Medicine should not be given unless prescribed by your doctor.
- Give a child who is unsettled after vomiting a drink or a little food.
- If your child seems unwell or shows any worrying symptoms, see a doctor.
Vomiting can be part of many illnesses in children and babies. It is not usually a major concern as long as your child seems well in other ways.
Vomiting is common for babies and young children. Vomiting occurs when food is brought back up from the stomach. The amount of vomit can often seem larger than it actually is.
Types of vomiting
There are different types of vomiting, including:
- Possetting – this is when your baby vomits up small amounts after a feed.
- Reflux – this vomiting is common in babies. It is caused when the valve at the top of the stomach accidentally opens. The contents of the stomach come back up the food pipe (oesophagus) slowly. Reflux does not harm babies. They usually grow out of it by the time they are walking.
- Projectile vomiting – this is when your baby brings up the stomach contents in a forceful way. The amount of milk or food can seem large on the floor, but is usually only the amount of the last feed. Babies may projectile vomit occasionally, but if it happens after every feed, see your doctor right away as it may be due to a blockage caused by thickening of the muscle at the outlet of the stomach.
Causes of vomiting
Vomiting is usually caused by:
- minor infections like 'gastro' or the common cold
- gastro-oesophageal reflux
- motion sickness from travelling in a moving vehicle.

Sometimes, vomiting may be part of a more serious illness. Children may vomit if they have an infection, such as a urinary tract infection or meningitis, a bowel obstruction or appendicitis. If vomiting progresses to fever and diarrhoea, it will usually be caused by a virus infection. If this persists for 12 hours or more, dehydration is likely. so see your doctor or local hospital emergency department without delay.
Treatment for vomiting
Most babies and children vomit easily and recover quickly. After vomiting, your child may be hungry and thirsty. Give plenty to drink so your child does not become dehydrated. If your child keeps on vomiting and looks unwell, see your doctor. Do not use medication to try and stop the vomiting.
Reflux vomiting can be prevented or reduced
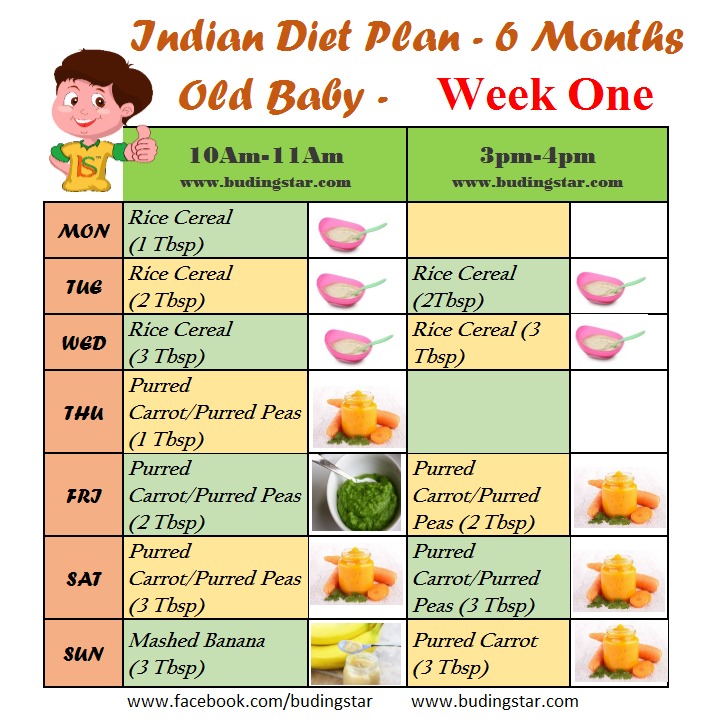
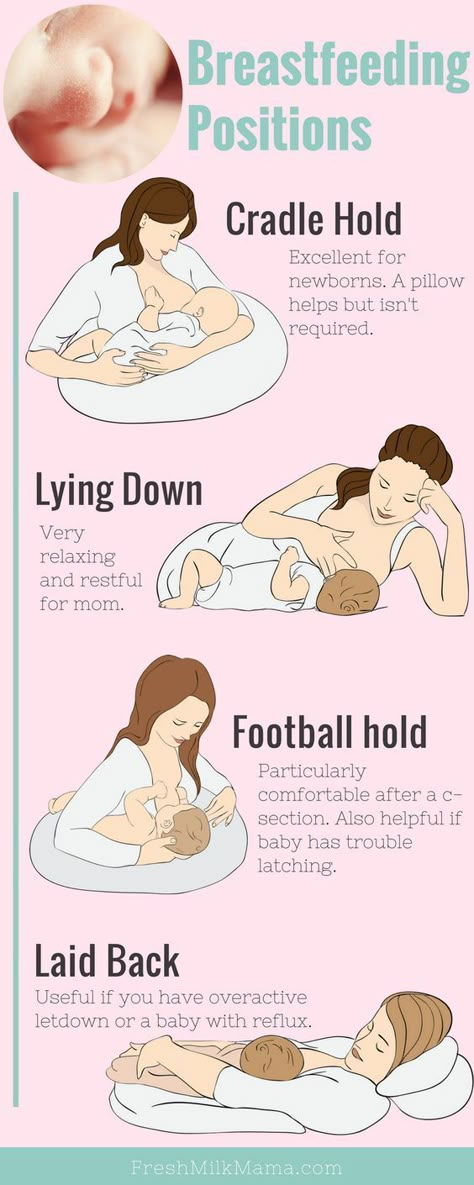
Different positions for feeding or in bed can help reduce your baby’s chance of vomiting. You can try to:
- Feed your baby in an upright position.
- Prop your baby up after feeds.

- Lay your baby on the left side.
- Avoid bouncing your baby after feeding.
To help with mild reflux, you can thicken your baby’s food with cornflour or infant food thickener. If your child is uncomfortable after vomiting or will not settle, try giving milk or water. This will wash any acid back into the stomach. Some babies get heartburn, which is a burning sensation in the chest. They may be unsettled after feeding or when lying flat. Your doctor can suggest an antacid to relieve heartburn.
When to see your doctor
Take your baby to the doctor if any of these symptoms occur:
- poor weight gain because of the loss of feeds in vomiting
- coughing or choking spells
- blood or yellow-green bile in the vomit
- heartburn
- vomiting increases or becomes forceful after every feed
- your baby seems unwell.
Where to get help
- Your doctor
- NURSE-ON-CALL Tel. 1300 60 60 24 – for expert health information and advice (24 hours, 7 days)
- Your local maternal and child health nurse
- The 24 hour Maternal and Child Health Telephone Service.
 Tel.13 22 29
Tel.13 22 29 - Your local hospital emergency or casualty department
Things to remember
- Mild vomiting is normal in most babies and improves over time.
- Most babies need only simple treatment, or none at all.
- Changing feeding and sleeping positions may help.
- Medicine should not be given unless prescribed by your doctor.
- Give a child who is unsettled after vomiting a drink or a little food.
- If your child seems unwell or shows any worrying symptoms, see a doctor.
This page has been produced in consultation with and approved by:
Pyloric Stenosis (for Parents) - Nemours KidsHealth
What Is Pyloric Stenosis?
Pyloric stenosis is a condition that can affect the gastrointestinal tract in babies. It can make a baby vomit forcefully and often, and can lead to other problems, such as dehydration. Pyloric stenosis needs medical care right away.
What Happens in Pyloric Stenosis?
Food and other stomach contents pass through the pylorus, the lower part of the stomach, to enter the small intestine.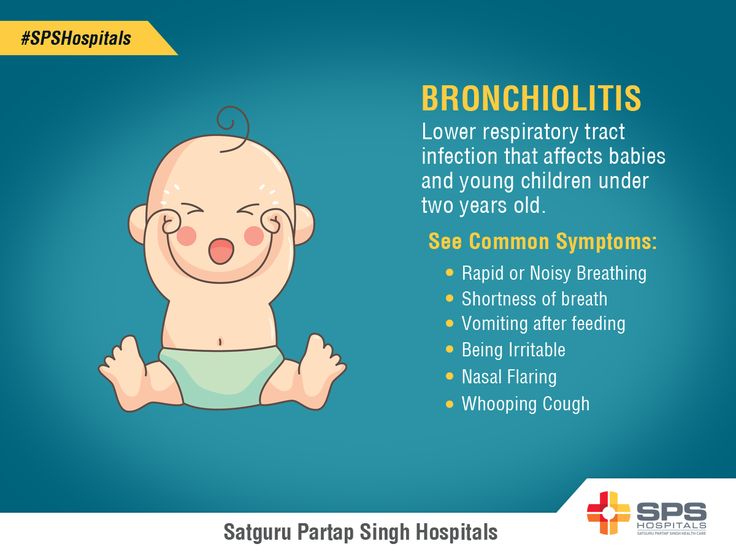 Pyloric stenosis (pie-LOR-ik stih-NOE-sis) is a narrowing of the pylorus. When a baby has pyloric stenosis, this narrowing of the pyloric channel prevents food from emptying out of the stomach.
Pyloric stenosis (pie-LOR-ik stih-NOE-sis) is a narrowing of the pylorus. When a baby has pyloric stenosis, this narrowing of the pyloric channel prevents food from emptying out of the stomach.
Pyloric stenosis (also called infantile hypertrophic pyloric stenosis) is a type of gastric outlet obstruction, which means a blockage from the stomach to the intestines.
Pyloric stenosis affects about 3 out of 1,000 babies in the United States. It's more likely to affect firstborn male infants and also runs in families — if a parent had pyloric stenosis, then a baby has up to a 20% risk of developing it. Most infants who have it develop symptoms 3 to 5 weeks after birth.
What Causes Pyloric Stenosis?
It's thought that babies who develop pyloric stenosis are not born with it, but have progressive thickening of the pylorus after birth. A baby will start to show symptoms when the pylorus is so thick that the stomach can't empty properly.
The cause of this thickening isn't clear.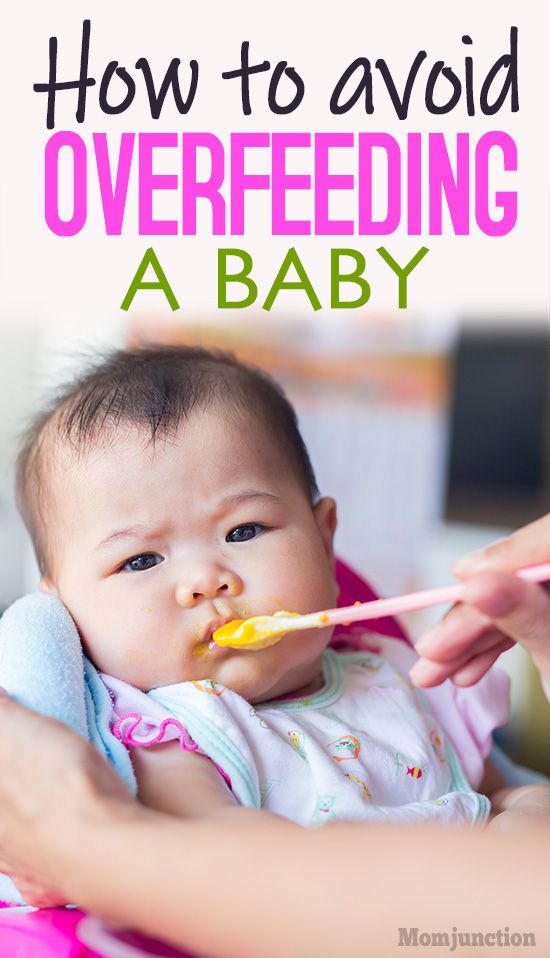 It might be a combination of several things. For example, use of erythromycin (an antibiotic) in babies in the first 2 weeks of life or antibiotics given to moms at the end of pregnancy or during breastfeeding can be associated with pyloric stenosis.
It might be a combination of several things. For example, use of erythromycin (an antibiotic) in babies in the first 2 weeks of life or antibiotics given to moms at the end of pregnancy or during breastfeeding can be associated with pyloric stenosis.
What Are the Signs & Symptoms of Pyloric Stenosis?
Symptoms of pyloric stenosis typically begin when a baby is around 3 weeks old. They include:
- Vomiting. The first symptom is usually vomiting. At first it may seem that the baby is just spitting up often, but then it tends to become projectile vomiting, in which the breast milk or formula is ejected forcefully from the mouth, in an arc, sometimes over a distance of several feet. Projectile vomiting usually takes place soon after the end of a feeding, although in some cases it can happen hours later.
The vomited milk might smell curdled because it has mixed with stomach acid. The vomit will not contain bile, a greenish fluid from the liver that mixes with digested food after it leaves the stomach.

Despite vomiting, a baby with pyloric stenosis is usually hungry again soon after vomiting and will want to eat. It's important to know that even with the vomiting, the baby might not seem to be in great pain or at first look very ill.
- Changes in stools. Babies with pyloric stenosis usually have fewer, smaller stools (poops) because little or no food is reaching the intestines. Constipation or poop with mucus also can happen.
- Failure to gain weight or weight loss. Most babies with pyloric stenosis will fail to gain weight or will lose weight. As the condition gets worse, they might become dehydrated.
Dehydrated infants are less active than usual, and they may develop a sunken "soft spot" on their heads and sunken eyes, and their skin may look wrinkled. Because less pee is made, they can go more than 4 to 6 hours between wet diapers.
- Waves of peristalsis. After feeds, increased stomach contractions may make noticeable ripples, which move from left to right over the baby's belly as the stomach tries to empty itself against the thickened pylorus.
It's important to call your doctor if your baby has any of these symptoms.
Other conditions can cause similar problems. For instance:
- gastroesophageal reflux (GER) usually begins before 8 weeks of age. GER involves lots of spitting up (reflux) after feedings, which can look like vomiting. But most babies with GER don't have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops.
- a milk protein allergy also can make a baby spit up or vomit, and have diarrhea. But these babies don't have projectile vomiting.
- gastroenteritis (inflammation in the digestive tract that can be caused by viral or bacterial infection) also can cause vomiting and dehydration. But babies with gastroenteritis usually also have diarrhea with loose, watery, or sometimes bloody stools. Diarrhea usually isn't seen with pyloric stenosis.
How Is Pyloric Stenosis Diagnosed?
The doctor will ask detailed questions about the baby's feeding and vomiting patterns, including what the vomit looks like.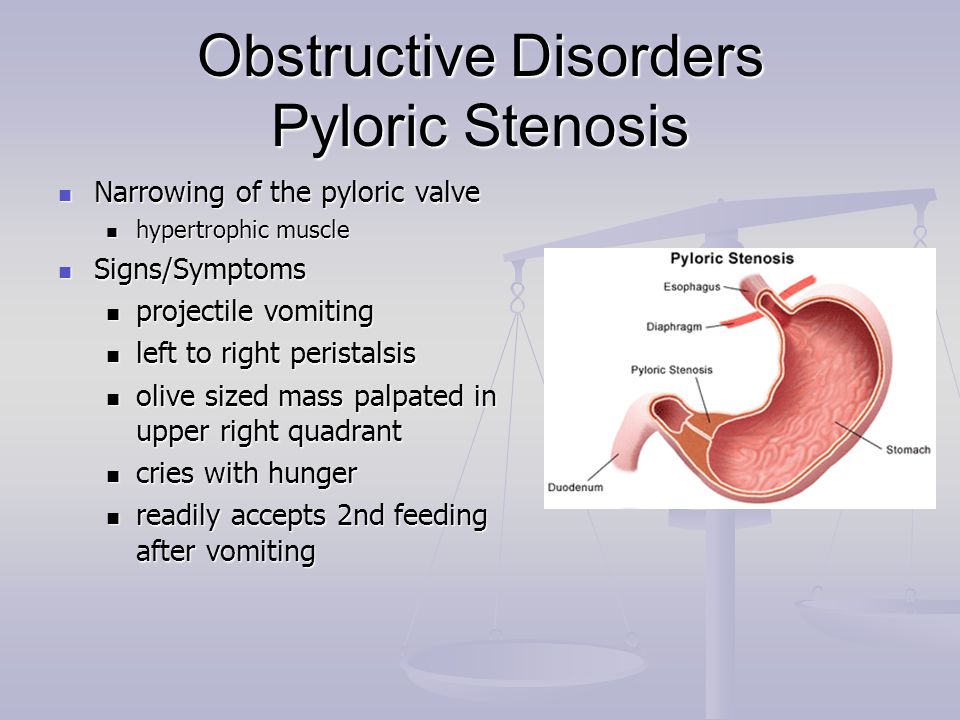 The doctor will do an exam, and note any weight loss or failure to maintain growth since birth.
The doctor will do an exam, and note any weight loss or failure to maintain growth since birth.
The doctor will check for a lump in the abdomen. If the doctor feels this lump, which usually is firm and movable and feels like an olive, it's a strong indication that a baby has pyloric stenosis.
If pyloric stenosis seems likely, the doctor probably will order an abdominal ultrasound. The enlarged, thickened pylorus will show on ultrasound images. The doctor may ask that the baby not be fed for several hours before an ultrasound.
Sometimes doctors order a barium swallow instead of an ultrasound. Babies swallow a small amount of a chalky liquid (barium). Then, special X-rays are done that let the doctor check the pyloric area for any narrowing or blockage.
The doctor also might order blood tests to check levels of electrolytes (minerals that help keep fluids balanced and vital organs working properly). An electrolyte imbalance often happens due to the ongoing vomiting of stomach acid and dehydration, and needs to be corrected.
How Is Pyloric Stenosis Treated?
When an infant is diagnosed with pyloric stenosis, either by ultrasound or barium swallow, the baby will be admitted to the hospital and prepared for surgery. Any dehydration or electrolyte problems in the blood will be corrected with intravenous (IV) fluids, usually within 24 hours.
Doctors do a surgery called pyloromyotomy (pie-lor-oh-my-OT-uh-me) to relieve the blockage. Using a small incision (cut), the surgeon examines the pylorus and separates and spreads the thick, tight muscles. This relaxes and opens those muscles.
The surgery can also be done through laparoscopy. This technique uses a tiny scope placed through a small cut in the belly button, letting the doctor see the area of the pylorus. Using other small instruments placed in nearby incisions, the doctor can complete the surgery.
Most babies return to normal feedings fairly quickly, usually 3 to 4 hours after the surgery. Because of swelling at the surgery site, a baby may still vomit small amounts for a day or so.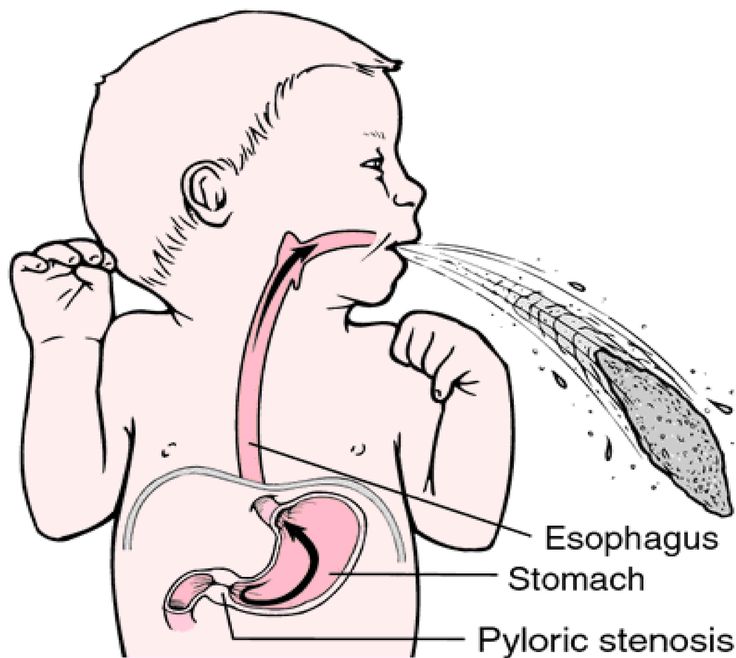 If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If you're breastfeeding, you might worry about continuing while your baby is hospitalized. The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
After a successful pyloromyotomy, your baby won't need to follow any special feeding schedules. Your doctor will probably want to examine your child at a follow-up appointment to make sure the surgical site is healing properly and that your baby is feeding well and maintaining or gaining weight.
Pyloric stenosis should not happen again after a pyloromyotomy. If your baby still has symptoms weeks after the surgery, there might be another medical problem, such as gastritis or GER, so let your doctor know right away.
When Should I Call the Doctor?
Pyloric stenosis is an urgent condition that needs immediate treatment. Call your doctor if your baby:
Call your doctor if your baby:
- has lasting or projectile vomiting after feeding
- is losing weight or not gaining weight as expected
- is less active than usual or is very sleepy
- has few or no stools (poops) over a period of 1 or 2 days
- show signs of dehydration, such as more than 4 to 6 hours between wet diapers, a sunken "soft spot" on the head, or sunken eyes
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" . nine0003
When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" . nine0003
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent. nine0003
They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent. nine0003
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood. nine0003
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses. nine0003
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way. nine0003
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way. nine0003
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop. nine0003
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician. nine0003
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause.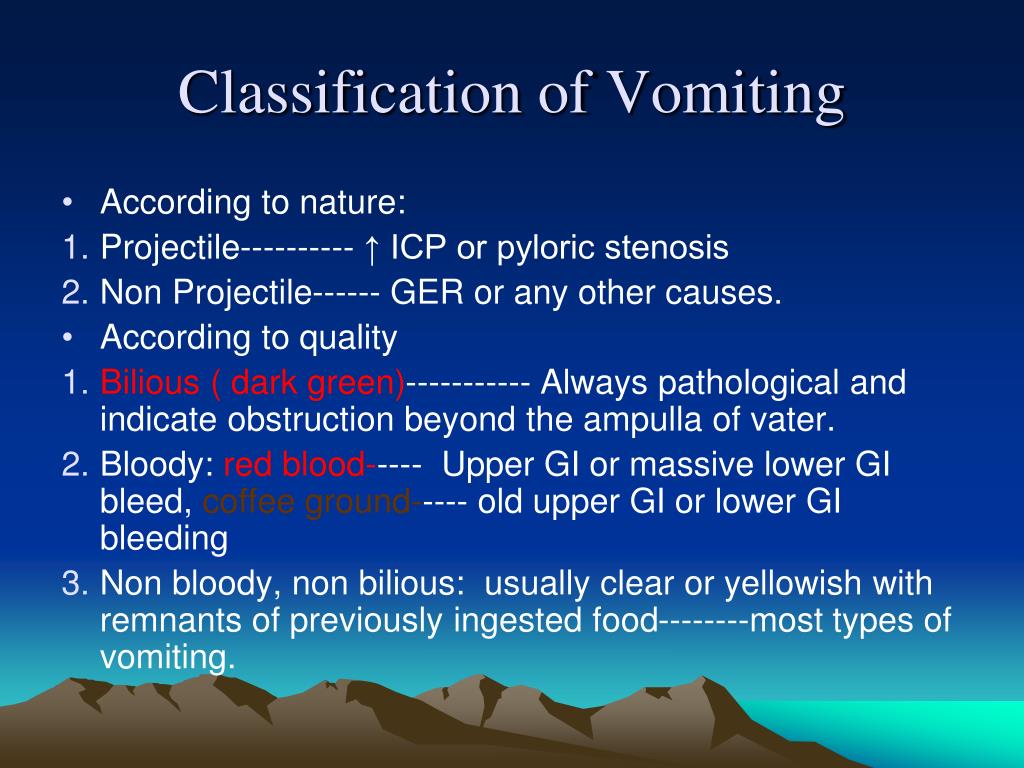 To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment. nine0003
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment. nine0003
Regurgitation and vomiting in children
Regurgitation syndrome is one of the most common reasons parents of young children visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc. nine0003
nine0003
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes. nine0003
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life. nine0003
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.