Baby pulls nipple during feeding
Baby Twiddling Your Nipple? It’s Actually Totally Normal
If you’re a breastfeeding parent, you may have felt prepared for sore nipples as your body adjusted to breastfeeding. You may have even been mentally prepared for some potential bites when your little one started teething.
One thing that might never have crossed your mind, though, is the awkwardness of your little one flicking and playing with the nipple they aren’t sucking on!
You may be relieved to know that this habit, commonly referred to as twiddling, isn’t uncommon.
But you’re probably still curious: Why does it happen? When does it start? What should you do about it? We’ve got your answers below.
Twiddling your breasts while breastfeeding is a natural action for many older babies. No one teaches them this, so why do they do it?
Although there’s not a lot of research about twiddling, one theory is that it helps increase breast milk production and let-down speed (how quickly or slowly milk releases from your breast).
As your baby grows, they want more milk and they want it to come out faster. Because twiddling stimulates your nipples, it can help make that happen.
Additionally, twiddling may offer your little one comfort. Physical touch is extremely comforting to people of all ages, but young children especially benefit from it.
As proof of the comfort twiddling can provide, many parents note that if their child is feeling anxious, overwhelmed, or otherwise in need of some TLC, they’ll also try to twiddle the breast of a parent who’s not breastfeeding.
Frequently, twiddling starts around 6 months, but it may start earlier or later.
There’s no exact age when twiddling begins, and it may be affected by a variety of developmental and environmental factors. These include diminishing milk supply or your little one learning how to use a pincer grasp.
Your baby may even go in and out of twiddling phases as they grow!
While very young newborn babies tend to be sleepy and need to concentrate on latching and sucking, older babies tend to fidget more while they feed.
As your little one becomes more mobile and alert, they may notice your other breast is within reach and want something to do with their hands.
Some babies and toddlers will even continue twiddling after they’ve been weaned, so you’ll want to keep an eye out for your little one wanting to play with your chest even if they’re no longer being breastfed.
Just as there’s no one age to expect twiddling to begin, there’s no perfect answer for how to handle it. Some breastfeeding parents choose to ignore it, if it isn’t bothering them too much.
For others, twiddling can be painful, associated with irregular menstrual cycles, or evoke strong feelings they’d prefer to avoid. In these cases, they take action to stop it.
How to stop it
If you decide you’d like your baby to stop twiddling, you can try several tactics, including:
- Use a piece of clothing or blanket to cover the breast your baby isn’t nursing from (out of sight, out of mind). You can also try covering the exposed nipple with your hand or finger, if that’s easier for you.

- Wear a chunky necklace or offer something else your little one can fiddle with instead.
- Hold and massage your baby’s hands during breastfeeding sessions.
- Talk to your baby about gentle touch and how certain kinds of touch can be painful to you.
- If you’re practicing side lying breastfeeding, you might consider feeding from the higher breast. This will make it harder for your baby to touch the lower one.
It’s totally fine to have different policies for twiddling in public versus at home.
No matter what you decide to do about the twiddling, you’ll need to be consistent and start sooner rather than later. After all, it’s much easier to distract and teach new behaviors before twiddling becomes a habit!
Twiddling is certainly not uncommon, so if your baby is doing it, no worries!
But if you’d like them to stop, be consistent and patient in teaching them how to treat your body during breastfeeding. You may also want to have a few toys handy to keep their little hands busy during feeding sessions.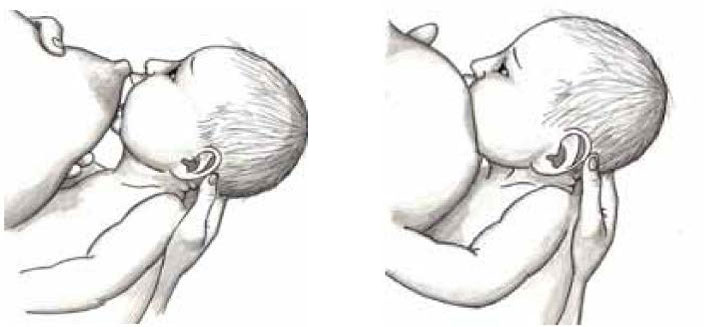
Remember: Breastfeeding is an ever-evolving journey. Your newborn baby may have struggled to latch, and now as your child ages, keeping them relaxed and focused during feeding sessions may be the hardest part.
With some gentle guidance, your baby will learn to follow your lead.
Baby Twisting and Pulling While Breastfeeding? Here's What to Do
Is your baby twisting and pulling while breastfeeding? Learn how to stop breastfed babies from squirming so much and being fussy and frantic during feeds.
See if this sounds familiar:
About five minutes into your feeding time, your newborn baby starts twisting and writhing at your breast, almost as if she’s upset. All this pulling hurts, and you’re forced to pull her off. Except when you do, she still acts hungry and is even more upset.
You realized that breastfeeding isn’t as easy as you expected, what with having a baby who keeps pulling off and re-latching. What should be a relaxing way to bond has turned into a frantic and frustrating experience.
What should be a relaxing way to bond has turned into a frantic and frustrating experience.
What to do with baby twisting and pulling while breastfeeding
Rest assured mama that you’re not alone, and that you haven’t failed in any way. A fussy baby, especially in the late afternoon and early evening, is normal and common. This is when our milk supply can be at its lowest (allowing the baby to suckle longer without receiving excessive milk flow).
The first place to turn to is your baby’s doctor or lactation consultant. She’ll be able to spot issues you may miss, like an ear infection or reflux that could be causing your baby to twist her head or squirm so much.
If all is clear, check out these tips that can help both of you nurse comfortably:
1. Calm your baby down first
Trying to encourage a fussy baby to stop twisting and pulling while breastfeeding can feel like a lost cause, especially in the early days. And in many ways, it is. Imagine being in a similar state and being continually asked to do something.
Instead, focus on calming him down and providing comfort, even if that means pausing your feeding session.
Maybe that means rocking him on the yoga ball or walking him around the room. Try swaddling him in a blanket, placing him on a swing, or carrying him in a baby wrap. In other words, calming him down is your goal, and feeding him comes second.
Similarly, try to stay calm as well. Babies can sense how we feel, and it’s not easy to nurse if we’re upset with them. Focus on remaining calm, remembering the bigger picture, and knowing that this won’t last forever.
Free email challenge: Feeling stuck in motherhood? Want to enjoy raising your kids again? Join my newsletter and sign up for the Motherhood Motivation 5-Day Challenge! You’ll get one actionable tip a day that will make you think (and act) about motherhood differently:
2. Limit distractions
I still remember placing my hand near my baby’s face as I nursed him. Why? He was so curious about what he was seeing that I had to block his view just so he’d keep feeding.
Because one reason your baby keeps pulling back might be because he’s distracted by what he sees and hears in his surroundings. Try to limit distractions during feeding sessions.
For instance, find a quiet spot to nurse, away from the rowdiness of the kids or the bright lights of the living room. Dim the lights, shut the curtains and turn on a fan or heater for white noise. Don’t engage with him too much, and avoid cooing, talking, or making eye contact while he eats.
3. Burp your baby frequently
A baby who twists, pulls, and grunts during a feeding session might have gas trapped and feel uncomfortable. If yours continues to squirm, pause feeding and try to burp her instead.
You might hold her in an upright position over your shoulder (make sure her tummy, not her head, is pressed on your shoulder). Try sitting her on your lap and supporting her face, neck, and chest with one hand while you burp her on the back with the other.
Take a minute or two to see if burping can help relieve her gas and encourage her to feed more steadily.![]()
Check out these baby burping tricks.
4. Try different feeding positions
Is your go-to feeding position just not cutting it? Try experimenting with different ways to nurse your baby! Perhaps the “cradle hold” you’d always relied on feels uncomfortable for him at this moment.
If so, you might try the football hold by nursing him on one side and positioning his feet toward your back. Or you could try lying down next to him and see if he prefers feeding next to you.
And make sure that he’s feeding at a slight angle where his head is above his tummy. For instance, don’t feed him flat on his back, as this can make him feel uncomfortable while he nurses.
5. Break your baby’s suction
Perhaps the most painful part about your baby twisting and pulling while breastfeeding is the sudden release of your breast. She doesn’t just ease her lips open—nope, she yanks with all her might. This sudden unlatching pulls on your nipples and makes the experience even more excruciating.
One way to ease the pain is to have your finger ready to break that suction before she pulls herself off. Keep your clean pinky finger next to her mouth and, when you sense that she’s about to unlatch or twist her head, insert your finger to help break the suction.
What to do when breastfeeding hurts, even with a good latch.
6. Alternate with a pacifier
Try this little trick: If you notice your baby twisting and pulling, offer a pacifier. After 10 or 20 sucks on the pacifier, see if she’ll then take to your breast more steadily.
This can help her relax, especially if she loves sucking on the pacifier throughout the day. Or she realizes that she isn’t receiving breast milk from the pacifier and can be more willing to nurse from your breast instead.
7. Lessen a heavy letdown
Do you have heavy milk production, especially at the beginning of a feeding session? The fast flow of milk might be too much for the baby to take in, causing her to squirm and pull away.
Help make swallowing easier by expressing excess milk beforehand. Either express the milk with your hand and catch it with a towel or bottle, or set aside a minute or so to pump into bottles or bags.
Another option is to nurse by leaning back instead of upright. Gravity can help slow the fast flow and provide your baby with enough milk she can keep up with.
Conclusion
If you’re frustrated with your baby twisting and pulling while breastfeeding, know that it’s okay to feel that way. While you may logically know that this won’t last forever, this may be lasting longer than you expected or hoped for.
That said, hopefully you’ve learned a few tricks that might help his behavior. Focus on calming him down so that he’s more likely to nurse peacefully. Limit distractions that might be pulling his attention away. Burp him frequently to ease gas discomfort, and try different breastfeeding positions as well.
Break his suction before he yanks himself off, and see if offering a pacifier could help “reset” his feeding and relax him.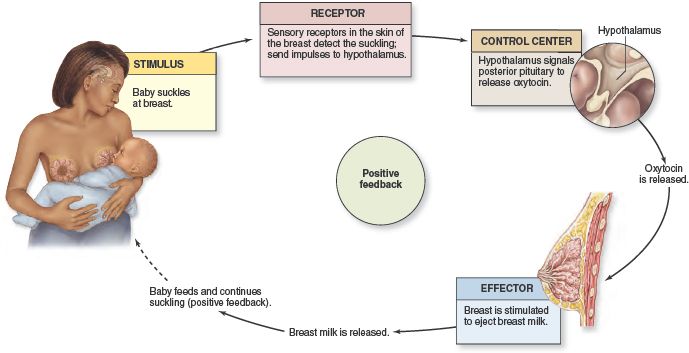 And finally, ease a fast letdown so he can swallow comfortably.
And finally, ease a fast letdown so he can swallow comfortably.
No more fussiness, mama—now you can feed in long, calm stretches once and for all.
Get more tips:
- Breastfeeding Secrets Every Mom Should Know
- When Does Breastfeeding Get Easier?
- Scared to Breastfeed? 7 Reasons to Tame Your Fear
- Breastfeeding Motivation to Keep You Going
- Essential Breastfeeding Supplies You Need to Have
Don’t forget: Join my newsletter and sign up for the Motherhood Motivation 5-Day Challenge:
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
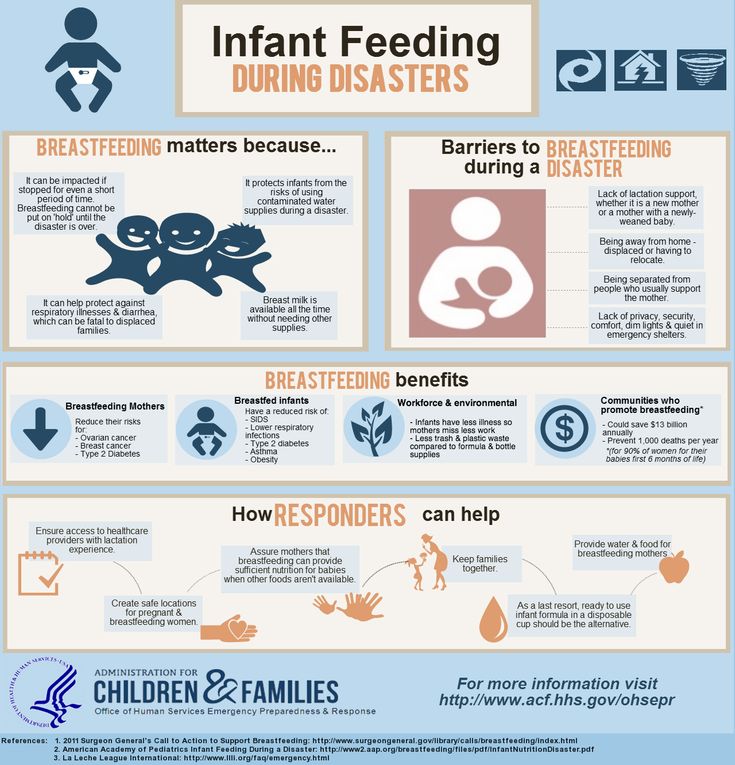
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
- Check how the baby latch on.
 An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue. - Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment.
 Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly. - Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not improve after a few days. Persistent inflammation of the nipples may indicate an infection that requires prompt treatment.

Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead.
 This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.

Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night.
 Such frequent feeding helps to establish the production of breast milk.
Such frequent feeding helps to establish the production of breast milk. - Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins.![]() Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.

Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk. The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm.
 The torso of the baby will be located diagonally on you.
The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014.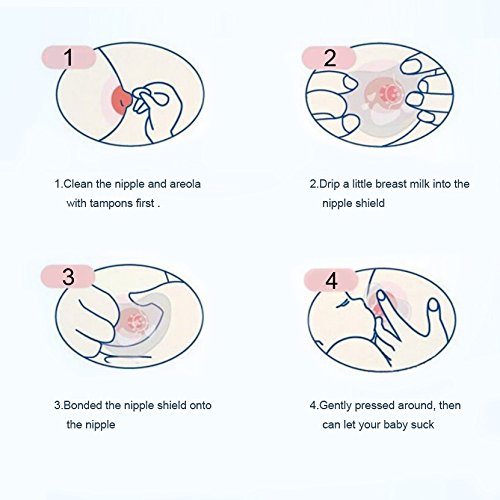 Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 of 07/19/10
** RU No. ФСЗ 2010/06525 of 17/03/2021
about breastfeeding - this is a collection of prejudices. They are so common that in many books for expectant mothers and in magazines for parents, it is actions based on prejudice that are described as correct and necessary.
“Breastfeeding is something incredibly difficult, almost no one is able to breastfeed for a long time, everyone always has a lot of problems and one sheer inconvenience”
There is nothing easier, more convenient, more pleasant for mother and child, and, by the way, cheaper than properly organized breastfeeding. But for that to be the case, breastfeeding needs to be learned. The best teacher in this matter may not be a book or a magazine for parents, but a woman who has been breastfeeding her child for a long time, more than a year, and receiving positive emotions from this. There are women who breastfeed for a long time and perceived it as a punishment. For example, one mother fed a child for 1.5 years and for all these 1.5 years she pumped after each feeding, and when she decided that she was enough and decided to wean the child, she had mastitis due to wrong actions. Now she tells everyone that breastfeeding is hell. She didn't feed her baby properly for a single day.
"Breastfeeding spoils the shape of the breast"
It is true that breastfeeding does not improve the shape of the breast, but the breast changes during pregnancy. It is then that it increases and becomes heavier, and, if its shape contributes to this, it “sags”.
Breast changes during lactation. Approximately 1-1.5 months after birth, with stable lactation, it becomes soft, produces milk almost only when the baby suckles. After the end of breastfeeding, 1.5-3 or more years after the birth of the baby, involution of the mammary gland occurs, lactation stops. Iron "falls asleep" until the next time. Under natural conditions, the end of breastfeeding always coincides with a decrease in the baby's need for breastfeeding. The chest remains soft, inelastic. The shape of the breast largely depends on the presence of adipose tissue in it, the amount of which decreases during prolonged breastfeeding. After the end of breastfeeding, adipose tissue is gradually restored. If a woman does not feed a child, the involution of the mammary gland occurs within the first month after childbirth. The shape of the breast still does not return to its pre-pregnancy state. And if you think about it and figure out why a woman has breasts at all? It's for breastfeeding.
The shape of the breast still does not return to its pre-pregnancy state. And if you think about it and figure out why a woman has breasts at all? It's for breastfeeding.
"Breastfeeding spoils the figure"
Many women are afraid to gain weight while breastfeeding. But usually a woman gains weight mainly during pregnancy, and not when she is nursing. Moreover, if before pregnancy she tried to meet certain fashionable standards, for example, 90-60-90, during pregnancy she returns to her weight, her genetically incorporated physiological norm (and it may be far from fashionable standards) + the well-known 7-10kg per uterus, fetus, amniotic fluid, increased volume of circulating blood and a little bit more for various little things. Weight gain during pregnancy can be significant. Many women begin to lose weight after 6-8 months of feeding, and gradually, in the second, third year of feeding, she “drops” everything that she has accumulated. It turns out that the figure from breastfeeding often just improves.
Very often it turns out that a woman, having stopped breastfeeding 1.5-2 months after giving birth, begins to gain weight. Perhaps this is due to the resulting hormonal imbalance, tk. no woman is designed for such a rapid cessation of lactation.
"You have to prepare the breast for feeding." And then various recommendations follow, from sewing hard rags into the bra to advice to the husband at the end of pregnancy to “dissolve the ducts” of his wife
There is no need to prepare the breast for feeding, it is so arranged by nature that by the time of birth it is quite ready to feed the child. Cloths, for example, can cause skin irritation. Any manipulation of the nipple at the end of pregnancy can lead to very undesirable consequences due to the stimulation of the oxytocin reflex: stimulation of the nipple - release of oxytocin - contraction of the muscles of the uterus under the influence of oxytocin - the uterus is "in good shape" - and, as the worst option, stimulation of premature labor. And in general, has anyone seen a cat with a rag in a bra, or a monkey doing a hardening shower massage?
And in general, has anyone seen a cat with a rag in a bra, or a monkey doing a hardening shower massage?
“With a flat, let alone inverted nipple, breastfeeding is impossible”
Strange as it may seem to people who have never breastfed, a baby's nipple is just a point from which milk flows. If the child sucks in the correct position, then the nipple is located at the level of the soft palate and does not participate in the actual sucking. The child sucks not the nipple, but the areola, massaging, decanting it with the tongue. A breast with a flat or inverted nipple is difficult for a baby to hold in his mouth while suckling and it is more difficult for him to suck on it. Mom should show patience and perseverance in the first days after the birth of a child. Any child is perfectly trained to suck even the most uncomfortable, from our point of view, breast.
The nipple changes shape during sucking, stretches and takes on a more comfortable shape for the baby, usually in 3-4 weeks. There are also various devices called "nipple formers". They are put on immediately after feeding, when the nipple is slightly extended by the efforts of the child and worn until the next application. The nipple formers hold the nipple in an extended position. But even without these things it is quite possible to do.
There are also various devices called "nipple formers". They are put on immediately after feeding, when the nipple is slightly extended by the efforts of the child and worn until the next application. The nipple formers hold the nipple in an extended position. But even without these things it is quite possible to do.
It is very important for a mother with flat or inverted nipples to ensure that her baby never suckles anything but her mother's breast after birth. The child of such a mother, having sucked on a bottle or a pacifier, quickly realizes that this is a more convenient object for sucking and begins to refuse the breast. In this situation, mom will need even more patience and perseverance.
"You can't keep a newborn at the breast for more than 5 minutes, otherwise there will be cracks"
The child should be kept at the breast for as long as he needs. Feeding ends when the baby himself releases the breast.
If we talk about cracks, there are only three groups of causes that lead to their formation
- Mother washes her breasts before each feeding.
 If she does this (and even with soap, and even anoints with brilliant green after feeding - a favorite pastime in Russian maternity hospitals, for example) - she constantly washes off the protective layer from the areola, which is produced by special glands located around the nipple, and dries the skin. This protective lubricant exists just to prevent the loss of moisture in the delicate skin of the nipple, it has bactericidal properties and inhibits the growth of pathogenic microorganisms and, which is especially important for the child, smells about the same as amniotic fluid. The sensitive skin of some women cannot tolerate such exposure for a long time and begins to crack, even with proper attachment of the baby.
If she does this (and even with soap, and even anoints with brilliant green after feeding - a favorite pastime in Russian maternity hospitals, for example) - she constantly washes off the protective layer from the areola, which is produced by special glands located around the nipple, and dries the skin. This protective lubricant exists just to prevent the loss of moisture in the delicate skin of the nipple, it has bactericidal properties and inhibits the growth of pathogenic microorganisms and, which is especially important for the child, smells about the same as amniotic fluid. The sensitive skin of some women cannot tolerate such exposure for a long time and begins to crack, even with proper attachment of the baby. -
Causes related to the incorrect position and behavior of the baby at the breast: the baby is not properly attached and sucks in the wrong position. And if this is true, then 5 minutes after 3 hours is enough for the formation of abrasions, and then cracks.
 The baby may latch on correctly, but in the process of suckling, he may perform various actions that can lead to cracking if the mother does not know that these actions need to be corrected and not allowed to behave like this. It must be remembered that the child has not suckled before, and does not know how to do it (he knows only the general principle of sucking). Unfortunately, most mothers also do not know how a baby should behave at the breast; they have never, or almost never seen it. What shouldn't a child be allowed to do? "Move out" to the tip of the nipple. This happens especially often if, during sucking, the child does not stick his nose into his mother's breast. If the mother feels that the grip is changing, she should try to press the baby with her nose to her chest. Very often this is enough for the child to “put on” correctly.
The baby may latch on correctly, but in the process of suckling, he may perform various actions that can lead to cracking if the mother does not know that these actions need to be corrected and not allowed to behave like this. It must be remembered that the child has not suckled before, and does not know how to do it (he knows only the general principle of sucking). Unfortunately, most mothers also do not know how a baby should behave at the breast; they have never, or almost never seen it. What shouldn't a child be allowed to do? "Move out" to the tip of the nipple. This happens especially often if, during sucking, the child does not stick his nose into his mother's breast. If the mother feels that the grip is changing, she should try to press the baby with her nose to her chest. Very often this is enough for the child to “put on” correctly.
If this does not help, the nipple must be removed and re-inserted correctly. The baby should not suckle the breast incorrectly for a single minute. He doesn’t care how to suck, he doesn’t know that he hurts his mother, he doesn’t know that the wrong position does not allow him to suck out enough milk, he doesn’t know that with the wrong position there is not enough stimulation of his mother’s breast and there will not be enough milk production. You can not let the child play with the nipple. A child who has learned to slide down on the tip of the nipple sometimes begins to pass the nipple back and forth through the parted jaws. Mom, of course, it hurts or is unpleasant, but in most cases, mothers allow this to be done “If only he sucked ...” they say ... Why? It often happens that children who do not feel the touch of the breast with their nose during sucking, or do not feel it very well, begin to make search movements with the nipple in their mouth. Here you need to gently press the baby to your chest so that he understands that he is already in place and there is nothing more to look for. Sometimes, especially if the mother has long and large nipples, the baby grabs the breast in several steps, “climbing” up in several movements.
He doesn’t care how to suck, he doesn’t know that he hurts his mother, he doesn’t know that the wrong position does not allow him to suck out enough milk, he doesn’t know that with the wrong position there is not enough stimulation of his mother’s breast and there will not be enough milk production. You can not let the child play with the nipple. A child who has learned to slide down on the tip of the nipple sometimes begins to pass the nipple back and forth through the parted jaws. Mom, of course, it hurts or is unpleasant, but in most cases, mothers allow this to be done “If only he sucked ...” they say ... Why? It often happens that children who do not feel the touch of the breast with their nose during sucking, or do not feel it very well, begin to make search movements with the nipple in their mouth. Here you need to gently press the baby to your chest so that he understands that he is already in place and there is nothing more to look for. Sometimes, especially if the mother has long and large nipples, the baby grabs the breast in several steps, “climbing” up in several movements. This also happens in cases where the child has already sucked on the pacifier and does not open his mouth well. The nipple is injured so very quickly. To avoid this, it is necessary to properly insert the nipple into the wide-open mouth, bringing the nipple itself past the jaws, as deep as possible. Moms don't know how to breastfeed properly.
This also happens in cases where the child has already sucked on the pacifier and does not open his mouth well. The nipple is injured so very quickly. To avoid this, it is necessary to properly insert the nipple into the wide-open mouth, bringing the nipple itself past the jaws, as deep as possible. Moms don't know how to breastfeed properly.
A typical picture for maternity hospitals with separate stay is as follows: a baby was brought to the mother for 30 minutes, the baby held everything correctly and sucked well for these 30 minutes, he would still suck, but they came to pick him up and the mother pulls (slowly or quickly) his nipple from mouth. Six such pulls per day is enough for the development of abrasions. You can take the nipple only after opening the jaw with the little finger (quickly insert the tip of the finger into the corner of the mouth and turn it - it does not hurt at all and no one suffers).
Diseases of the skin of the nipples. Most often, mothers are faced with a fungal infection of the skin of the nipples - "thrush". In this situation, the skin most often looks "irritated", it can peel off, itch, cracks may appear, even despite proper application, there may be pain during and after sucking, piercing pains along the milk ducts. This problem is usually solved with the use of specific treatment and also has nothing to do with the topic of preparing the breast for feeding or the time the baby is at the breast.
In this situation, the skin most often looks "irritated", it can peel off, itch, cracks may appear, even despite proper application, there may be pain during and after sucking, piercing pains along the milk ducts. This problem is usually solved with the use of specific treatment and also has nothing to do with the topic of preparing the breast for feeding or the time the baby is at the breast.
“While there is no milk, it is necessary to drink more water”
The first day after childbirth, liquid colostrum forms in the breast of a woman, on the second day it becomes thick, on 3-4 days transitional milk may appear, 7-10-18 days - milk become mature. Colostrum is scarce and thicker than milk. This is the main argument in most Russian maternity hospitals in favor of supplementing and feeding the child (otherwise he allegedly suffers from hunger and thirst).
If a child needed large volumes of liquid immediately after birth, then nature would arrange the woman in such a way that she would be flooded with colostrum immediately after childbirth. But the child does not need extra water at all. All he needs he gets from colostrum and milk! The water that is given to the child while the mother has colostrum literally “washes away” the colostrum from the gastrointestinal tract, depriving the baby of the action of colostrum necessary for him. Water is given from a bottle, which leads to "tangled nipples" in the baby and may lead to refusal of the breast. Water causes a false feeling of fullness and reduces the need for suckling in a child. If we give a child 100 g of water per day, he sucks 100 g less milk (this applies not only to a newborn). The kidneys of a newborn are not ready for a large load of water and begin to work with overload. The list of arguments against can be continued, but these are enough.
But the child does not need extra water at all. All he needs he gets from colostrum and milk! The water that is given to the child while the mother has colostrum literally “washes away” the colostrum from the gastrointestinal tract, depriving the baby of the action of colostrum necessary for him. Water is given from a bottle, which leads to "tangled nipples" in the baby and may lead to refusal of the breast. Water causes a false feeling of fullness and reduces the need for suckling in a child. If we give a child 100 g of water per day, he sucks 100 g less milk (this applies not only to a newborn). The kidneys of a newborn are not ready for a large load of water and begin to work with overload. The list of arguments against can be continued, but these are enough.
“While there is no milk, it is necessary to supplement the child with formula, otherwise he will lose weight, starve”
The child is not designed to receive anything other than colostrum and milk. In the first days after birth, one colostrum is enough for him. Weight loss in the first day of life is a physiological norm. Newborns lose up to 6-8% of their birth weight in the first two days of their lives. Most children regain their weight or begin to put on weight by 5-7 days of life. Supplementary feeding with a mixture in the first days of a child's life is nothing more than a gross interference in the functioning of the baby's body. You can call this intervention a metabolic catastrophe. But in most Russian maternity hospitals, this is completely ignored!
Weight loss in the first day of life is a physiological norm. Newborns lose up to 6-8% of their birth weight in the first two days of their lives. Most children regain their weight or begin to put on weight by 5-7 days of life. Supplementary feeding with a mixture in the first days of a child's life is nothing more than a gross interference in the functioning of the baby's body. You can call this intervention a metabolic catastrophe. But in most Russian maternity hospitals, this is completely ignored!
In addition, the introduction of supplementary feeding is carried out through a bottle, which very quickly leads to "tangled nipples" and the baby refuses the breast. Sometimes one or two bottle feedings are enough to stop a baby from breastfeeding! The mixture causes a feeling of fullness, lingers in the stomach for a long time, the child has a reduced need to suckle the breast, which leads to a decrease in breast stimulation and a decrease in milk production.
“I feed my baby on demand! He demands from me in 3. 5 hours!”
5 hours!”
Feeding on demand means putting the baby to the breast for every disturbance or search. The baby needs breastfeeding around every sleep, he falls asleep at the breast and when he wakes up, he is given the breast. A newborn child in the first week of his life can indeed be applied relatively rarely - 7-8 times a day, but in the second week of life, the intervals between applications are always reduced. During wakefulness, the child can ask for a breast up to 4 times per hour, i.e. every 15 minutes! Usually a child fed on demand is applied in the first month of life 12 or more times a day, usually 16-20 times. If a child in the first months of life is applied less than 12 times, then the mother either does not notice his modest requests, or ignores them (meaning a healthy, physiologically mature child).
In the overwhelming majority of cases, at the moment when the child begins to ask for a breast more often, the mother decides that the child is starving and introduces supplementary feeding. And the child asks for breasts not at all because he is hungry. He constantly needs a sense of confirmation of physical contact with his mother. During his life in his mother's belly, he is very used to the following: warm, crowded, I hear my heart beating, my lungs breathe, my intestines growl, I smell and taste amniotic fluid (filling the baby's nose and mouth), almost all the time I suck a fist (studies suck). Only in these conditions the baby feels comfortable and safe. After childbirth, he can get into such conditions only if his mother takes him in her arms, puts him on her breast, and then he will again feel cramped, warm, he will hear familiar rhythms, start sucking and feel the familiar smell and taste (the smell and taste of milk are similar to the taste and smell of amniotic fluid). And a newborn child wants to get into such conditions as often as possible. And a modern mother is waiting, she can’t wait, when the intervals between feedings will increase, when will the child start eating in 3.
And the child asks for breasts not at all because he is hungry. He constantly needs a sense of confirmation of physical contact with his mother. During his life in his mother's belly, he is very used to the following: warm, crowded, I hear my heart beating, my lungs breathe, my intestines growl, I smell and taste amniotic fluid (filling the baby's nose and mouth), almost all the time I suck a fist (studies suck). Only in these conditions the baby feels comfortable and safe. After childbirth, he can get into such conditions only if his mother takes him in her arms, puts him on her breast, and then he will again feel cramped, warm, he will hear familiar rhythms, start sucking and feel the familiar smell and taste (the smell and taste of milk are similar to the taste and smell of amniotic fluid). And a newborn child wants to get into such conditions as often as possible. And a modern mother is waiting, she can’t wait, when the intervals between feedings will increase, when will the child start eating in 3. 5-4 hours, when will he stop waking up at night ??? Hurry!!! And, usually, to the timid attempts of the child to ask for a breast, he answers with a pacifier, a rattle, gives some water, talks, entertains. The child is most often applied to the breast only when he wakes up. And he quickly agrees with this position. The child always takes the mother's position. But here a “pitfall” awaits mother and baby - insufficient breast stimulation and, as a result, a decrease in the amount of milk.
5-4 hours, when will he stop waking up at night ??? Hurry!!! And, usually, to the timid attempts of the child to ask for a breast, he answers with a pacifier, a rattle, gives some water, talks, entertains. The child is most often applied to the breast only when he wakes up. And he quickly agrees with this position. The child always takes the mother's position. But here a “pitfall” awaits mother and baby - insufficient breast stimulation and, as a result, a decrease in the amount of milk.
“Feeding on demand is a nightmare! It is impossible to sit and feed the child for days!”
That's what mothers who can't breastfeed say. With properly organized feeding, mom is resting! She lies, relaxed, hugs the baby, the baby sucks. What could be better? Most women cannot find a comfortable position, they sit, they hold the child awkwardly, their back or arm numbs, if they feed lying down, it usually “hangs” over the child on the elbow, the elbow and back become numb. Moreover, if the child does not take the breast well, it hurts the mother . .. What kind of pleasure can we talk about here? In the first month - one and a half after childbirth, when the child is applied chaotically, without a pronounced regimen, sucks often and for a long time, the mother can feel good only if breastfeeding is organized correctly, it is convenient for the mother to feed, she knows how to do it standing, lying down and sitting, and even moving.
.. What kind of pleasure can we talk about here? In the first month - one and a half after childbirth, when the child is applied chaotically, without a pronounced regimen, sucks often and for a long time, the mother can feel good only if breastfeeding is organized correctly, it is convenient for the mother to feed, she knows how to do it standing, lying down and sitting, and even moving.
“After each feeding, you must express the rest of the milk, otherwise the milk will be wasted”
No, you do not need to express after each feeding if breastfeeding is properly organized. If you feed your baby 6 times a day and do not express, indeed, milk can disappear very quickly. If you express after each feeding, then you can support lactation for some time. The terms are different, but rarely it is more than six months, cases of feeding on such behavior for more than a year are rare.
When feeding a baby on demand, the mother always has as much milk as the baby needs and there is no need to pump after each application. In order for the newborn to completely suck out the breast, it is applied to one breast for 2-3 hours, and to the other for the next 2-3 hours. Somewhere after 3 months, when the child is already applied relatively rarely, he may need a second breast in one attachment, then the next time he is applied to the one that was last.
In order for the newborn to completely suck out the breast, it is applied to one breast for 2-3 hours, and to the other for the next 2-3 hours. Somewhere after 3 months, when the child is already applied relatively rarely, he may need a second breast in one attachment, then the next time he is applied to the one that was last.
There is one unpleasant “pitfall” in regular pumping after feeding, which even most doctors are not aware of. It's called lactase deficiency. When a mother expresses after a feed, she expresses just the “hind” fatty milk, which is relatively poor in milk sugar, lactose. She feeds the child mainly with the anterior portion, which accumulates in the breast between rare feedings. There is a lot of lactose in the anterior portion. The child is fed "only lactose", the gastrointestinal tract of the child after some time ceases to cope with such volumes of lactose. Lactase deficiency develops (Lactase is an enzyme that breaks down lactose - milk sugar, it begins to be missed). This is one of the reasons for the development of lactase deficiency; the second, for example, is this: the mother gives the child two breasts in one feeding. But about this separately.
This is one of the reasons for the development of lactase deficiency; the second, for example, is this: the mother gives the child two breasts in one feeding. But about this separately.
“You should give your baby two breasts at one feeding.”
No, it is not necessary to give two breasts. A newborn baby can be applied for 1.5-3 hours to one breast. Then 1.5-3 hours to another (for example, the baby woke up, sucked a little and didn’t want to anymore, but after 30 minutes he wanted to suck a little more. After 20 minutes, he sucked longer and fell asleep; all these attachments were from one breast; when the baby wakes up, you can offer him another breast). We need this so that the baby sucks the breast to the end, and receives "front" and "hind" milk in a balanced amount. If the baby is transferred to the other breast in the middle of feeding, he will receive less fat-rich hind milk. He will suck mainly the front portion from one breast and add the same from the other. Foremilk is rich in lactose, and after a while the baby can no longer cope with the load of lactose.![]() Lactose intolerance develops.
Lactose intolerance develops.
Transferring a baby from one breast to another can cause hyperlactation in some women, and if the mother also expresses both breasts after each feeding ... There are such mothers. Curtailing excess milk is sometimes more difficult than adding missing ... In some cases, feeding at one feeding from two breasts is necessary to stimulate lactation when there is a shortage of milk. A growing baby, most often after 3-4 months, may need two breasts in one feeding. Then the next application begins with the breast that was last.
“The more liquid you drink, the more milk”
There are mothers who try to drink as much as possible, sometimes up to 5 liters of liquid per day. And a nursing mother should drink only as much as she wants. By thirst. Mom shouldn't be thirsty. And if water is drunk on purpose, and even more than 3-3.5 liters per day, lactation can begin to be suppressed.
“Sucking the fist is very harmful”
The whole end of pregnancy the child sucked the fist, so he learned to suck. Fist sucking is one of the inborn habits of a newborn. After childbirth, the baby begins to suck on the fist as soon as it enters his mouth. At 3-4 months, the fist is the first thing that the baby can put into his mouth on his own. He can do things on his own!!! This is amazing! And at this age, many babies begin to actively suck their fingers and fists. There is nothing wrong with this. Mom only needs to watch the baby a little. If a baby plays with a fist, then he sucks, then he stops, he can not be distracted from this activity. If the baby begins to actively suck the fist, then the baby wants to suck for real, offer him a breast. If the need to suckle the baby is fully satisfied by the breast, then the baby stops sucking the fist by 5-6 months. (Then, at 6-7 months, he begins to “look for teeth”, but this is a completely different behavior). The cam baby sucks almost the same as the breast, opening its mouth wide. Some babies have a very funny behavior when, having stuck to the chest, the baby tries to put his fist in his mouth .
Fist sucking is one of the inborn habits of a newborn. After childbirth, the baby begins to suck on the fist as soon as it enters his mouth. At 3-4 months, the fist is the first thing that the baby can put into his mouth on his own. He can do things on his own!!! This is amazing! And at this age, many babies begin to actively suck their fingers and fists. There is nothing wrong with this. Mom only needs to watch the baby a little. If a baby plays with a fist, then he sucks, then he stops, he can not be distracted from this activity. If the baby begins to actively suck the fist, then the baby wants to suck for real, offer him a breast. If the need to suckle the baby is fully satisfied by the breast, then the baby stops sucking the fist by 5-6 months. (Then, at 6-7 months, he begins to “look for teeth”, but this is a completely different behavior). The cam baby sucks almost the same as the breast, opening its mouth wide. Some babies have a very funny behavior when, having stuck to the chest, the baby tries to put his fist in his mouth . ..
..
"My baby needs a pacifier"
The baby is not designed by nature to suckle anything other than the breast (and the fist, in a pinch). A child is always taught to use a pacifier. There are children who immediately push out the pacifier with their tongue. And there are those who begin to suck it. There are mothers who hold the pacifier with their finger so that her child does not push it out. Usually, the first time a baby gets a dummy is when he showed concern and the mother does not know how to calm him down. To calm down, the child needs to suck on the breast, well, they didn’t give him a breast, they gave him something else, he will have to suck what they give ...
“A child often asks for breasts, which means that he is hungry, there is not enough milk for him”
As mentioned above, a newborn child asks to be breastfed often, not at all because he is hungry. He wants to suck, he wants to mom. He constantly needs confirmation of psycho-emotional and physical contact with his mother.
“Sufficient milk or not, we will find out on control feeding”
We will not learn anything on control feeding (the child is weighed before and after feeding, the difference is calculated and find out how much he sucked for feeding). Because:
- A baby who feeds on demand constantly sucks different portions of milk. In one application 5 ml, in another - 50, in the third - 150. You can get 5 ml. (I once weighed my daughter after 30 minutes of suckling. She gained 14 g. In the first month of her life, she gained 1200 g - and what would the district pediatrician tell me if this was control feeding in the clinic?)
- The newborn is designed to receive small portions of milk, but often. The vast majority of newborns in the conditions of feeding 6-7 times a day still suck out small portions of milk, and not 6 times 120 ml. And of course they don't eat. They start gaining poorly or stop gaining weight, or lose weight altogether.
Sufficient or not enough milk can be determined in two ways:
Wet diaper test. (This is a test for wet diapers, not for used diapers, because you need to know exactly the number of urination). If a child older than 7 days pees more than 6-8 times a day, his urine is light, transparent, odorless, then he receives a sufficient amount of milk. Usually the child pees during wakefulness every 15-30 minutes. If a mother uses diapers, but wants to find out if there is enough milk or not, she needs to remove the diapers from the child for three hours. If the baby pees 3-4 times or more in three hours, then you can not count further. If you peed 3 times or less, we count for 6 hours. If in six hours he peed 4-5 times or more, you can not count further, if less than 4, we count further. And so on… Weekly weight gain (for a child older than 7 days) should be between 125 and 500 g.
(This is a test for wet diapers, not for used diapers, because you need to know exactly the number of urination). If a child older than 7 days pees more than 6-8 times a day, his urine is light, transparent, odorless, then he receives a sufficient amount of milk. Usually the child pees during wakefulness every 15-30 minutes. If a mother uses diapers, but wants to find out if there is enough milk or not, she needs to remove the diapers from the child for three hours. If the baby pees 3-4 times or more in three hours, then you can not count further. If you peed 3 times or less, we count for 6 hours. If in six hours he peed 4-5 times or more, you can not count further, if less than 4, we count further. And so on… Weekly weight gain (for a child older than 7 days) should be between 125 and 500 g.
“If applied frequently, the baby will suck everything out quickly, the breast is soft all the time – there is no milk. It is necessary to “save” milk for feeding”
When feeding a child on demand, the breast becomes soft about a month after the start of feeding, when lactation becomes stable. Milk begins to be produced only when the baby suckles. The breast is never “empty”, in response to the sucking of the child, milk is constantly produced in it. If the mother is trying to fill her breasts for feeding, waiting for the breasts to “fill up”, she gradually reduces the amount of milk by such actions. The more mother attaches the child, the more milk, and not vice versa.
Milk begins to be produced only when the baby suckles. The breast is never “empty”, in response to the sucking of the child, milk is constantly produced in it. If the mother is trying to fill her breasts for feeding, waiting for the breasts to “fill up”, she gradually reduces the amount of milk by such actions. The more mother attaches the child, the more milk, and not vice versa.
“The stomach needs to rest”
But the child's stomach doesn't work very well. Milk there only curdles and is quickly evacuated to the intestines, where the actual digestion and absorption takes place. This is the prejudice from the old song about feeding according to the schedule after 3 hours. The newborn does not have a clock. No mammal makes even intervals in feeding its newborns. The body of the child is adapted to the continuous flow of mother's milk, and he does not need to rest at all.
“After each feeding, keep the baby upright for 20 minutes.”
Do not hold the baby upright after each feeding, especially if the baby has fallen asleep. Most of the time the baby lies on its side. If he burps a little, then the diaper just changes under his cheek. It is necessary to hold the artificial man vertically so that he does not spill the 120g poured into him. And we are talking about babies who are fed on demand and receive small portions of mother's milk. In addition, the cardiac sphincter of the stomach needs training, which it can only receive if the child is lying down.
Most of the time the baby lies on its side. If he burps a little, then the diaper just changes under his cheek. It is necessary to hold the artificial man vertically so that he does not spill the 120g poured into him. And we are talking about babies who are fed on demand and receive small portions of mother's milk. In addition, the cardiac sphincter of the stomach needs training, which it can only receive if the child is lying down.
“You need to sleep at night”
At night, you need to not only sleep, but suck your breast. Most newborn children are so arranged that they sleep from 10-11 pm to 3-4 am, then they begin to wake up and ask for breasts. In a child of the first month of life, applications in the morning hours (from 3 to 8) are usually 4-6. Night feedings with properly organized breastfeeding look something like this: the baby got worried, the mother put it to the breast, the baby sleeps sucking and the mother also sleeps, after a while he lets go of the breast and sleeps more soundly. And such episodes happen in a night 4-6. All this is easy to organize if the mother sleeps with her child, and for this she needs to be able to feed lying down in a comfortable position.
And such episodes happen in a night 4-6. All this is easy to organize if the mother sleeps with her child, and for this she needs to be able to feed lying down in a comfortable position.
If the baby sleeps separately from the mother, in his own bed, then he stops waking up for morning feedings, sometimes already a week after birth, sometimes by 1.5-2 months. Most modern mothers take this with relief, because. for them, finally, the night running back and forth, nodding while sitting in a chair or on a bed over a sucking child, and some also pumped at night ... And here they are waiting for a pitfall called insufficient stimulation of prolactin and, as a result, a decrease in the amount of milk . A mother and her child are a wonderful self-regulating system. While the baby has a need to suck in the morning, his mother produces the maximum amount of prolactin, just from about 3 to 8 in the morning.
Prolactin is always present in the female body in small amounts, its concentration in the blood increases significantly after the baby begins to breastfeed, most of all it is obtained in the morning hours from 3 to 8 in the morning. Prolactin, which appeared in the morning, is engaged in the production of milk during the day. It turns out who sucks at night, stimulates his mother's prolactin and provides himself with a decent amount of milk during the day. And whoever fails to suckle at night, he can quite quickly be left without milk during the day. No mammal takes a nightly break from feeding its young.
Prolactin, which appeared in the morning, is engaged in the production of milk during the day. It turns out who sucks at night, stimulates his mother's prolactin and provides himself with a decent amount of milk during the day. And whoever fails to suckle at night, he can quite quickly be left without milk during the day. No mammal takes a nightly break from feeding its young.
“I lost my milk because of my “nerves””
Milk production depends on the hormone prolactin, the amount of which depends on the number of times the baby is latched on and nothing else. The experiences of the mother on any occasion do not affect him. But the release of milk from the breast depends on the hormone oxytocin, which is engaged in the fact that it contributes to the contraction of muscle cells around the lobules of the gland and thereby contributes to the flow of milk. The amount of this hormone is very dependent on the psychological state of the woman. If she is frightened, tired, in pain or in any other discomfort during feeding, oxytocin stops working and milk stops flowing from the breast. A child cannot suck it out, a breast pump does not express it, and it cannot come out with its hands ...
A child cannot suck it out, a breast pump does not express it, and it cannot come out with its hands ...
The manifestation of the “oxytocin reflex” was observed by every breastfeeding woman: when a mother hears the crying of a child (and not necessarily her own), her milk begins to leak. The body tells the mother that it is time to apply the baby. In a situation of stress or fear, nothing like this is observed. (Relationship to the ancient instinct of self-preservation: if a woman runs from a tiger and she smells of leaking milk, the tiger will find and eat her faster, so while she runs in fear through the jungle with a child under her arm, the milk will not leak when she gets to the safety of the cave - and calmly settle down to feed the child, the milk will come again.)
Modern stressful situations work like those tigers. In order for milk to flow out again, you must try to relax during feeding, think only about the child. You can drink soothing herbs, shoulder massage, calm conversation helps well. Anything to help you relax. And most modern mothers are not able to relax during feeding, it is uncomfortable for them to sit or lie down, it can be painful to feed - all this prevents the manifestation of the oxytocin reflex - milk remains in the breast, which leads to a decrease in lactation.
Anything to help you relax. And most modern mothers are not able to relax during feeding, it is uncomfortable for them to sit or lie down, it can be painful to feed - all this prevents the manifestation of the oxytocin reflex - milk remains in the breast, which leads to a decrease in lactation.
"The baby is too fat, it is necessary to limit the number of feedings and give water"
A breastfed child gains 125 to 500 g per week, or 500 to 2000 g per month. Usually, by 6 months, a child born with a weight of 3-3.5 kg weighs about 8 kg. The rate of gain is very individual, there is never any talk of "overfeeding", children who are actively gaining weight grow rapidly in length and look proportionate. Children who gain 1.5-2 kg per month in the first half of life, usually sharply reduce weight gain in the second half of the year and can weigh 12-14 kg by the year. There is never a need to limit the number of feedings, much less to give water.
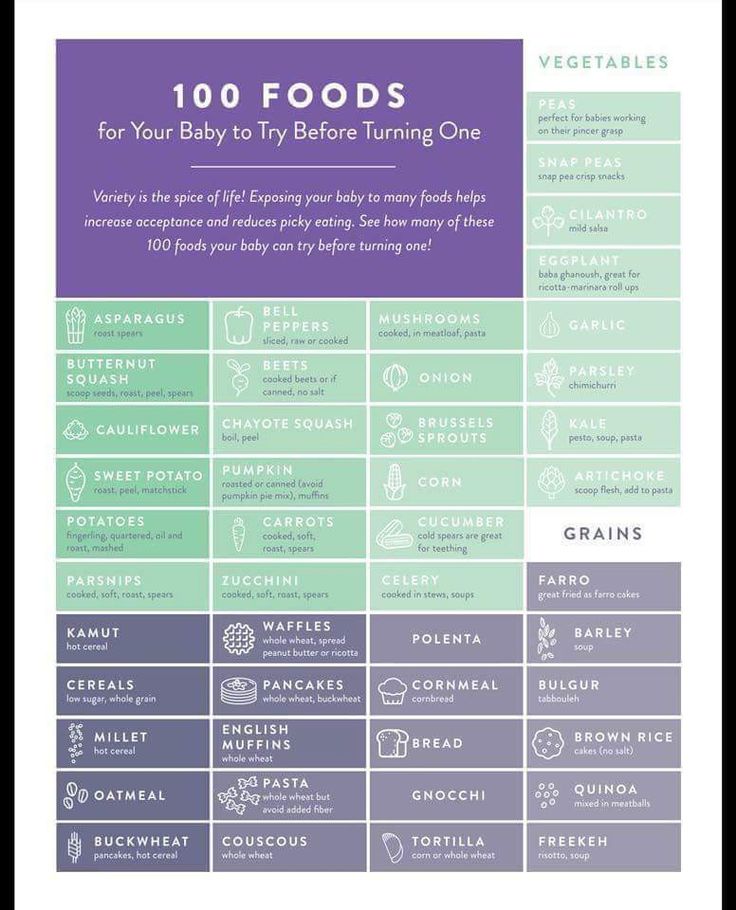
“Baby lacks nutrients, needs complementary foods from the age of 4 months”
The need for other food manifests itself in a child of about 6 months of age, when he begins to actively wonder what everyone is eating there. And if a mother takes a baby to the table with her, he begins to actively take an interest in the contents of his plate. This behavior is called active food interest, and it indicates that the child is ready to get acquainted with new food and can begin it. Nevertheless, breast milk remains the main food of the child in the first year of life, and in many cases even at the beginning of the second, contains absolutely all the nutrients the child needs and much more.
And if a mother takes a baby to the table with her, he begins to actively take an interest in the contents of his plate. This behavior is called active food interest, and it indicates that the child is ready to get acquainted with new food and can begin it. Nevertheless, breast milk remains the main food of the child in the first year of life, and in many cases even at the beginning of the second, contains absolutely all the nutrients the child needs and much more.
"A nursing mother should have a strict diet"
Food should be habitual. It is preferable not to use exotic foods in the diet that are not characteristic of the "native" climatic zone. A breastfeeding mother may have interesting nutritional needs, and they must be met in the same way as the desires of a pregnant woman. A woman should eat according to her appetite, and not stick food for two into herself. And, of course, you need to try to eat healthy food. Do not use products containing preservatives, dyes and other unhealthy substances.