Baby routine feeding
Tips for the First Year
Eat, sleep, pee, poop, repeat. Those are the highlights in a day of the life of a brand new baby.
And if you’re a new parent, it’s the eating part that may be the source of many of your questions and worries. How many ounces should your baby take? Do you wake a sleeping baby to eat? Why do they seem hungry all the time? When can your child start solids?
Questions abound — and, despite Grandma’s insistence, the answers have changed since you were a tot. It’s now recommended that newborns, even formula-fed ones, eat on demand (consider it good preparation for the teenage years) and that babies wait to start solid foods until they’re 4 to 6 months old.
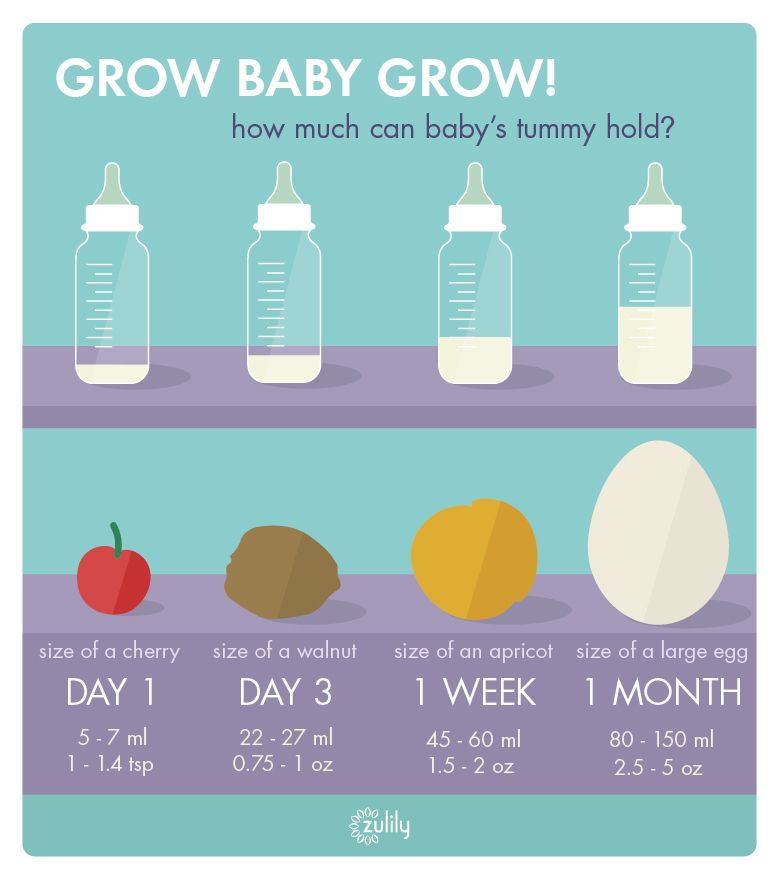
On day one of life, your baby’s stomach is the size of a marble and can only hold 1 to 1.4 teaspoons of liquid at a time. As your baby gets older, their stomach stretches and grows.
It’s hard (or impossible, really) to know how much milk your baby is taking in while breastfeeding. But if you’re bottle feeding due to any number of valid reasons, it’s a bit easier to measure.
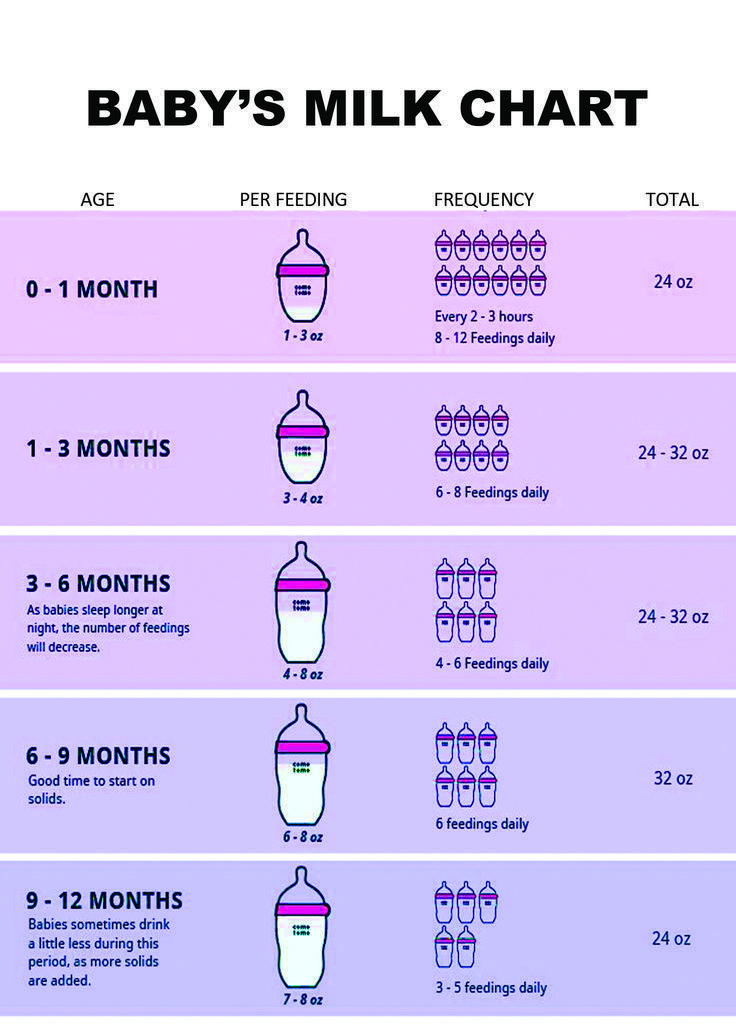
Here, from the American Academy of Pediatrics (AAP), a typical feeding schedule for bottle-fed babies.
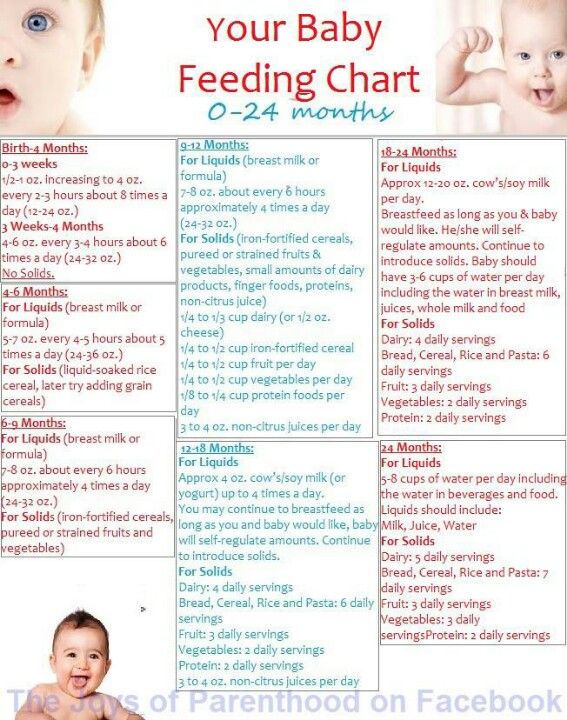
| Age | Ounces per feeding | Solid foods |
|---|---|---|
| Up to 2 weeks of life | .5 oz. in the first days, then 1–3 oz. | No |
| 2 weeks to 2 months | 2–4 oz. | No |
| 2–4 months | 4-6 oz. | No |
| 4–6 months | 4–8 oz. | Possibly, if your baby can hold their head up and is at least 13 pounds. But you don’t need to introduce solid foods yet. |
| 6–12 months | 8 oz. | Yes. Start with soft foods, like one-grain cereals and pureed vegetables, meats, and fruits, progressing to mashed and well-chopped finger foods. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. |
Every baby is unique — but one thing that’s pretty consistent is that breastfed babies eat more frequently than bottle-fed ones. That’s because breast milk is easily digested and empties from the stomach a lot quicker than formula.
Breastfed babies
There’s no rest for the weary. According to La Leche League International, you should begin nursing your baby within 1 hour of birth and provide about 8 to 12 feedings daily in the first few weeks of life (yeah, we’re exhausted for you).
At first, it’s important not to let your baby go more than 4 hours without feeding. You’ll likely need to wake them up if necessary, at least until breastfeeding is well established and they’re gaining weight appropriately.
As your baby grows and your milk supply amps up, your baby will be able to take in more milk in less time at one feeding. That’s when you might start to notice a more predictable pattern.
- 1 to 3 months: Your baby will feed 7 to 9 times per 24 hours.

- 3 months: Feedings take place 6 to 8 times in 24 hours.
- 6 months: Your baby will feed around 6 times a day.
- 12 months: Nursing may drop to about 4 times a day. The introduction of solids at about 6 months helps to fuel your baby’s additional nutritional needs.
Keep in mind that this pattern is just one example. Different babies have different paces and preferences, along with other factors that influence the frequency of feedings.
Bottle-fed babies
Like breastfed babies, bottle-fed newborns should eat on demand. On average, that’s about every 2 to 3 hours. A typical feeding schedule may look like this:
- Newborn: every 2 to 3 hours
- At 2 months: every 3 to 4 hours
- At 4 to 6 months: every 4 to 5 hours
- At 6+ months: every 4 to 5 hours
For both breastfed and bottle-fed babies
- Don’t give liquids other than formula or breast milk to babies under a year old. That includes juices and cow’s milk.
 They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup.
They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup. - Don’t add baby cereal to a bottle.
- It can create a choking hazard.
- A baby’s digestive system isn’t mature enough to handle cereal until about 4 to 6 months of age.
- You could overfeed your baby.
- Don’t give your baby any form of honey until after their first birthday. Honey can be dangerous for a baby, occasionally causing what’s called infant botulism.
- Do adjust your expectations based on your baby and their unique needs. Premature babies are likely to follow feeding patterns according to their adjusted age. If your baby has challenges like reflux or failure to thrive, you may need to work with your doctor on the appropriate feeding schedule and amount they should be eating.
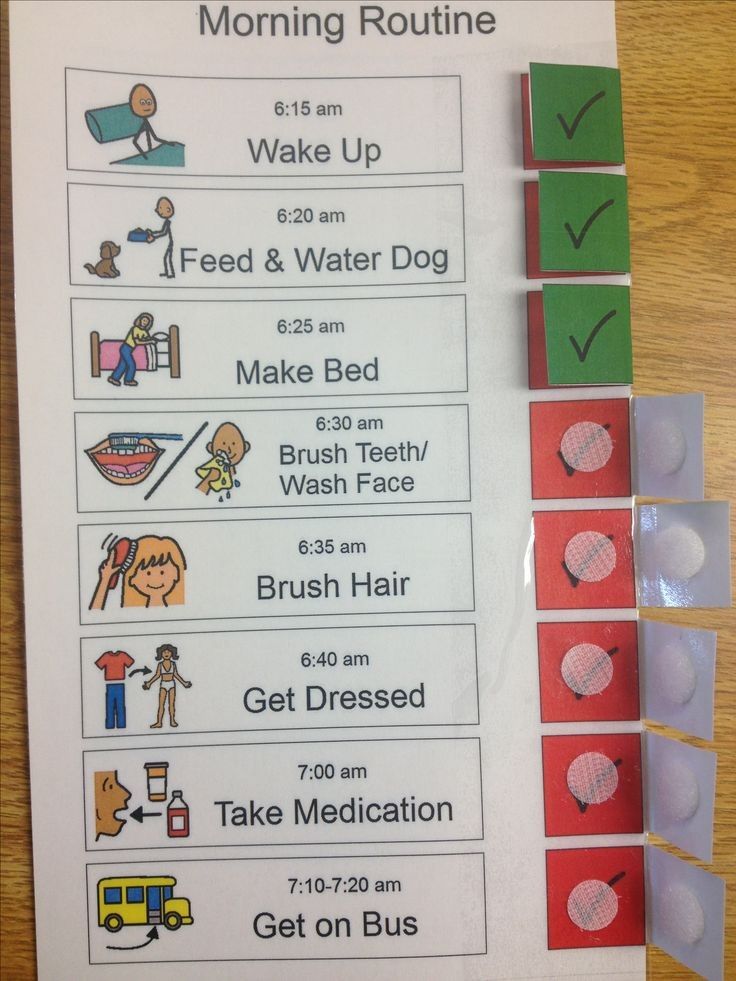
Schedules are the holy grail of every parent. Your child will naturally start to fall into a feeding pattern as their tummy grows and they can take in more breast milk or formula at one sitting. This may begin to happen between 2 and 4 months of age.
This may begin to happen between 2 and 4 months of age.
For now, though, focus on learning your baby’s hunger cues, such as:
- rooting around your chest, looking for a nipple.
- putting their fist in their mouth
- smacking or licking their lips
- fussing that can escalate quickly (don’t wait until your baby’s hangry to feed them)
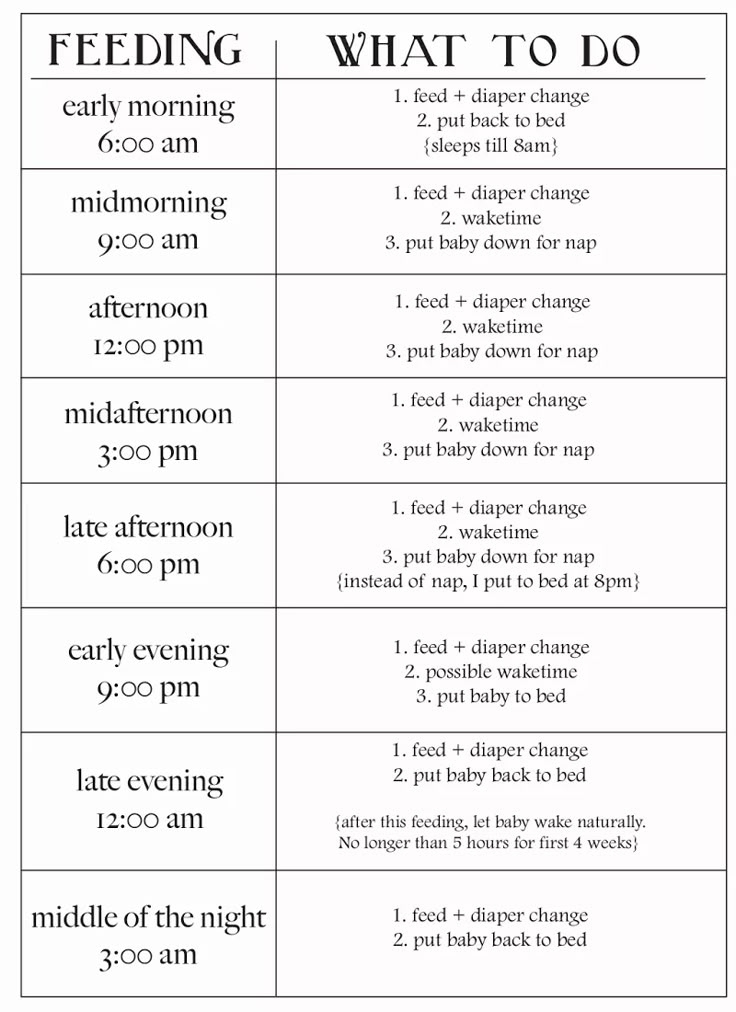
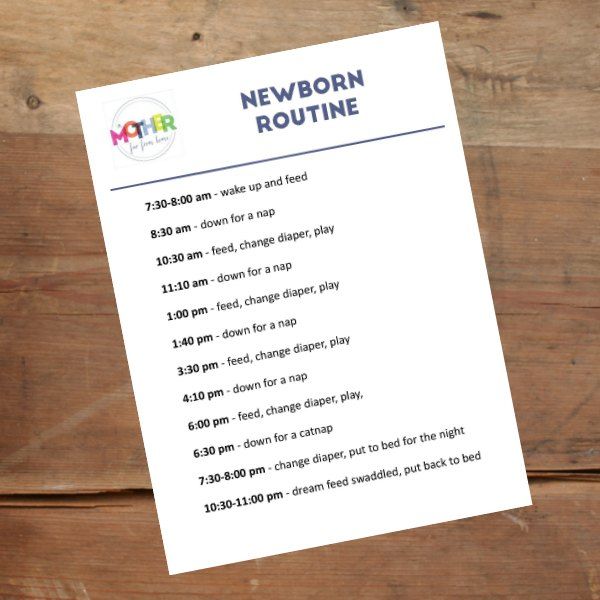
Once your baby is a few months old, you may be able to introduce a sleep/feed schedule that works for you.
Let’s say, for example, your 4-month-old wakes every 5 hours for a feeding. That means if you feed at 9 p.m., your baby wakes around 2 a.m. But if you wake and feed the baby at 11 p.m., just before you go to bed, they may not rouse until 4 a.m., giving you a decent chunk of nighttime winks.
In general, if your baby seems hungry, feed them. Your baby will naturally eat more frequently during growth spurts, which typically occur around 3 weeks, 3 months, and 6 months of age.
Some babies will also “cluster feed,” meaning they’ll feed more frequently during certain periods and less at others. For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
Worried about overfeeding? While this isn’t really possible to do with an exclusively breastfed baby, you can overfeed a baby who’s taking a bottle — especially if they’re sucking on the bottle for comfort. Follow their hunger cues, but talk to your pediatrician if you’re worried your little one may be overeating.
Your baby is probably ready for solids if they’re 4 to 6 months old and:
- have good head control
- seem interested in what you’re eating
- reach for food
- weigh 13 or more pounds
Which food to start with? The AAP now says it doesn’t really matter much in what order you introduce foods. The only real rule: Stick with one food for 3 to 5 days before offering another. If there’s an allergic reaction (rash, diarrhea, vomiting are common first signs), you’ll know which food is causing it.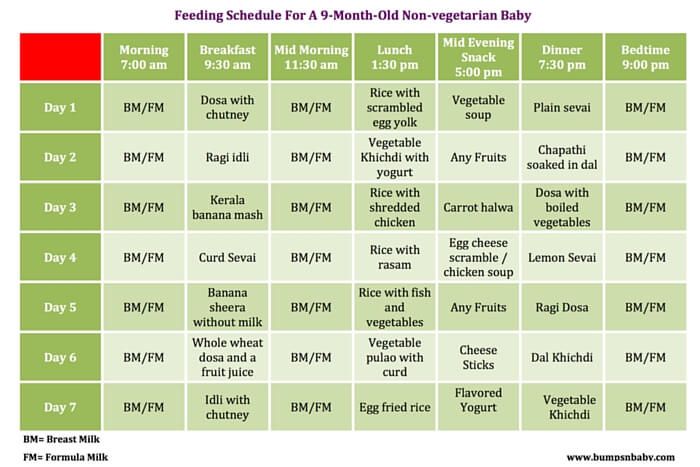
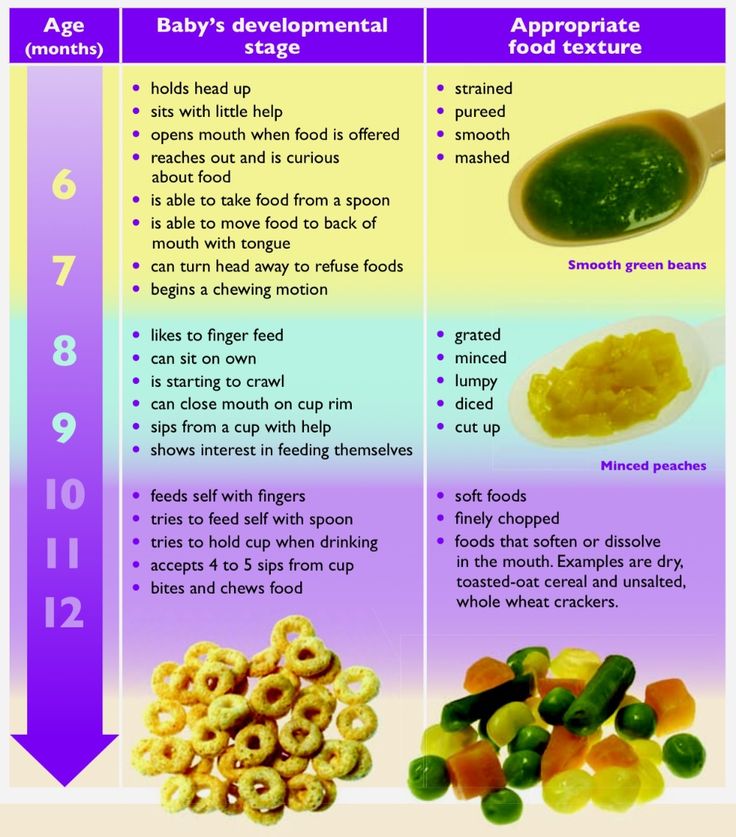
As your baby grows, move from pureed baby food to ones that have more texture (for example, mashed banana, scrambled egg, or well-cooked, chopped pasta). This generally happens around 8 to 10 months of age.
Your supermarket offers a variety of baby food products, but if you want to make your own, keep it sugar and salt free. Additionally, at this stage, don’t feed your baby anything that could be a choking hazard, including:
- hard foods, such as popcorn or nuts
- hard, fresh fruits, like apples; cook to soften or chop into very small pieces
- any meat that isn’t well cooked and very well chopped (this includes hot dogs)
- cheese cubes
- peanut butter (though talk to your pediatrician about this one — and the benefits of introducing diluted peanut butter before the age of 1)
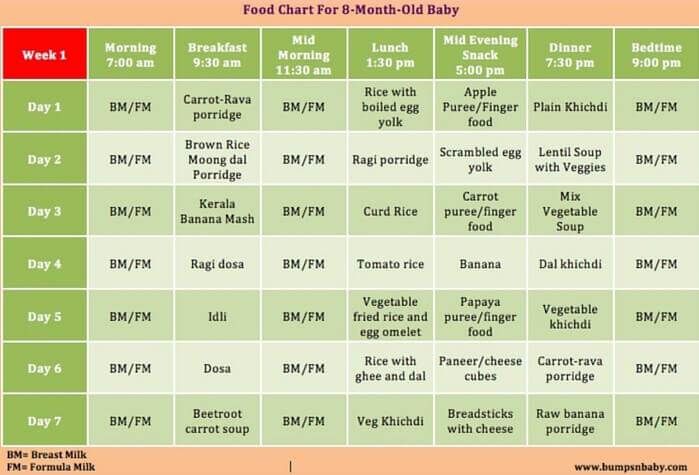
As your baby nears their first birthday, they should be eating a variety of foods and taking in about 4 ounces of solids at each meal. Continue to offer breast milk or formula. By 8 months, babies are drinking about 30 ounces a day.
By 8 months, babies are drinking about 30 ounces a day.
Oh yeah, and buy some stock in a company that makes stain-fighting laundry detergent. It’ll pay for college.
Babies aren’t cookie cutter. Some will gain weight easily, while others will have problems. Things that can affect a baby’s weight gain include:
- having a birth defect like a cleft lip or palate, which creates problems feeding
- having a milk protein intolerance
- being premature
- being fed with a bottle versus the breast
A 2012 study of more than 1,800 babies found that the infants who were fed with a bottle — regardless of whether the bottle contained breast milk or formula — gained more weight in the first year than babies who nursed exclusively.
Your baby’s doctor is the best one to advise you on a healthy weight range for your baby.
How, when, and what to feed a baby are top worries of every parent — but there’s good news: Most babies are pretty good judges of when they’re hungry and when they’re full — and they’ll let you know it.
You just need to present them with the right choices at the right time and pay attention to their cues. If you have any questions or concerns, your pediatrician is there to help you along the way.
Newborn and Baby Feeding Chart in the 1st Year
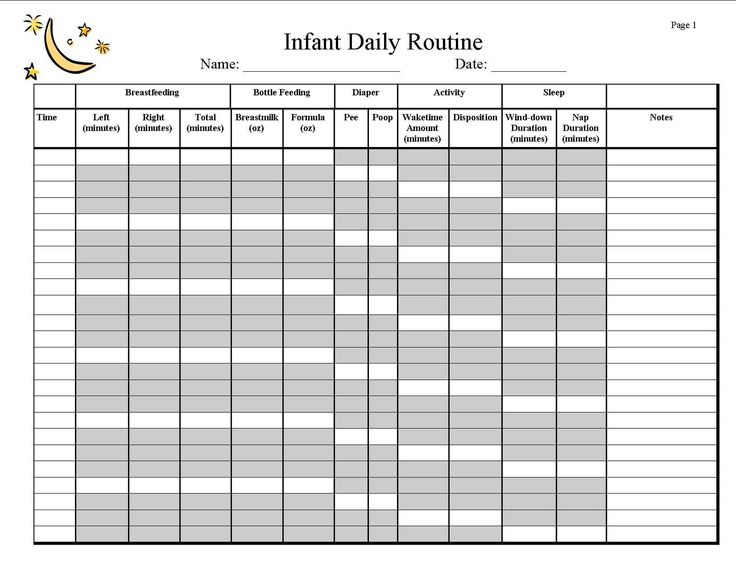
Whether you’re a first-time parent or a seasoned caregiver, figuring out why your baby is crying can feel like a guessing game. Fortunately, paying attention to your baby’s daily feeding schedule can help reduce some of the guesswork.
By following a feeding schedule, you might be able to avoid some of the fussiness associated with hunger, and you’ll be able to more easily tell whether he’s more likely to be wet or tired instead.
Whether your little one’s a newborn, a 6-month old, or even a 1-year-old, read on to find out how to come up with a feeding schedule and adjust it to your baby’s needs as he grows and develops.
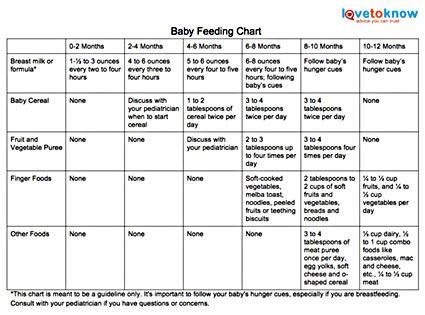
Baby Feeding Chart at a Glance
As you watch for those delightful baby milestones — from first smiles and giggles to sitting and crawling — it can be hard to keep track of everything related to your baby’s feeding schedule. Fortunately, you don’t have to. We've assembled all the necessary details in the chart below, including feeding frequency and portion information.
Fortunately, you don’t have to. We've assembled all the necessary details in the chart below, including feeding frequency and portion information.
related baby tool
Keep an eye on your baby’s average growth by tracking height, weight, and head circumference with our simple tool.
Fill out your baby's details*:
What is your child*
Boy Girl
This is a mandatory field.
Age (between 0 and 24 months)
This is a mandatory field.
Weight (lbs.)
This is a mandatory field.
Height (in.)
This is a mandatory field.
Head circumference (in.)
This is a mandatory field.
*Input details of your baby’s last measurements. **Source: World Health Organization
**Source: World Health Organization
Feeding Schedule for Breastfed Newborns
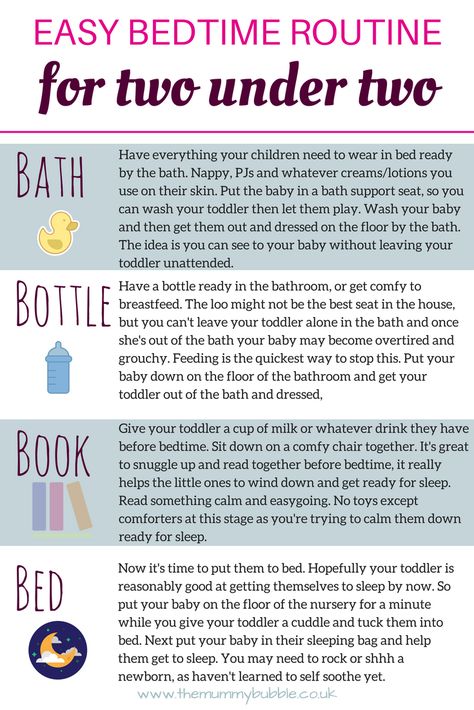
From the moment your baby is born, she begins to grow at a surprisingly quick pace. To fuel her development and keep her well fed, be prepared to nurse about every two to three hours.
By the time she’s a week old, your little one may begin to nap for longer periods, giving you more time between feedings. If she’s sleeping, you can maintain your baby’s feeding schedule by waking her up gently when it’s time to feed.
Tips to keep in in mind if you’re breastfeeding:
The length of time between feedings is measured from when your baby begins nursing, not when she stops.
Ensure your little one latches on properly. This can be difficult when you’re starting out, especially for first-time moms, but over time your baby may begin to latch comfortably. Speaking to a lactation consultant could be helpful.
As your baby grows she may nurse at a faster rate.
Alternate between breasts during each feeding.
Look for signs that your baby is full. She may turn away from the breast, nurse at a slower rate, or lose interest. Once she seems full, end the feeding
Your baby’s healthcare provider may recommend adding vitamin D oral supplements to your baby’s diet. Follow the provider's instructions to ensure your baby gets the proper dosage.
Nursing your baby on demand or every couple of hours around the clock can seem like a lot—and it is! At the newborn stage, your baby can’t take in much milk in a single sitting, so frequent feeding is needed to make sure she's getting enough. Later on, as your baby's daily routine (including her sleep and awake time) becomes more predictable, you'll have an easier time following a regular feeding schedule.
Feeding Schedule for Formula-Fed Newborns
Formula-fed newborns will need about two to three ounces (60 – 90 milliliters) of formula per feeding to start with. Newborns, fed from bottles are able to take in more during a feeding than a breastfed infants. This allows you to space out feedings by about three to four hours.
Newborns, fed from bottles are able to take in more during a feeding than a breastfed infants. This allows you to space out feedings by about three to four hours.
As your baby reaches her 1-month milestone, she will need at least four ounces per feeding to get the nourishment she requires. Your newborn’s feeding schedule will gradually become more predictable over time, and you’ll need to adjust the amount of formula as she grows.
3-Month-Old Feeding Schedule
Now that you and your baby have begun to develop a routine, it can be difficult to make slight alternations. However, as your baby grows and her feeding needs change, you’ll need to adjust your baby’s feeding schedule accordingly.
For Your Breastfed Baby
At 3 months, your baby is becoming more active, will begin to breastfeed less often, and may sleep for longer periods of time at night.
You may have to nurse just six to eight times per day at this stage (or about every three to four hours).
If your baby’s healthcare provider sees that he’s gaining weight and growing at a regular pace, then he’s probably getting the right amount of nutrition.
The number of wet and soiled diapers is also a great indicator as to whether or not he is eating well. Your baby should have about four to six wet diapers a day.
See your baby’s healthcare provider if you’re concerned that your little one may not be getting enough to eat.
For Your Formula-Fed Baby
As your little one continues to grow, you’ll notice that he wants to eat more during each feeding and begins to sleep for longer intervals at night.
Slight adjustments to your 3-month old’s feeding schedule may include:
Increasing the amount of formula to about 5 ounces per feeding
Giving your baby formula about six to eight times per day
Switching the newborn nipple size or style on your baby’s bottles to make it easier for him to drink from the bottle.
6-Month-Old Feeding Schedule
At this stage, your baby’s healthcare provider may recommend you expand your baby’s diet to include solid foods. With these menu additions on the horizon, having a 6-month-old feeding schedule will come in handy!
With these menu additions on the horizon, having a 6-month-old feeding schedule will come in handy!
When a baby ready to try solid foods, a single grain baby cereal mixed with breast milk or formula has traditionally been the first solid food to be introduced, followed by pureed vegetables and fruits. However, there's no medical evidence that indicates introducing foods in any special order offers any benefits.
Keep in mind that solids are only a supplement at this stage, and that breast milk or formula is still your baby’s most important source of nutrition. Continue to include about 32 ounces of breast milk or formula in your 6-month-old’s feeding schedule of three to five feedings per day to ensure your baby gets the necessary vitamins and minerals.
You may be able to start weaning your baby off of night feedings; however, every baby is unique. Speak to your baby’s healthcare provider to see if it’s time to cut down on nighttime feedings and to learn what you can do to encourage the process.
7 to 9-Month-Old Feeding Schedule
Months seven through nine can be a good time to add a greater variety and quantity of solid foods to your baby’s diet. He may need fewer daytime feedings, now — about four to five.
Purees of meats, veggies, and fruits are recommended at this stage. Introduce your baby to these new flavors as single ingredient purees then gradually add combinations to his meals.
Your baby may slowly begin to wean off breast milk or formula as his growing body demands solid foods for nutrition.
There is no correct time to wean off breast milk or formula. Speak to your baby’s healthcare provider to learn more about the cues and signs that can let you know when your baby is ready for more solid foods.
10 to 12-Month-Old Feeding Schedule
Exploring new textures may now be a big part of your little one’s meals. As he grows, he may begin to self-feed with finger foods such as cut-up bananas, dry cereal, and pasta and even demand certain flavors that he enjoys more.
As you continue to replace breast milk or formula with solids, your baby’s healthcare provider can help determine how to balance out your baby’s meals.
Blends of different foods can be introduced during mealtime and added to your baby’s feeding schedule. Your baby may eat about three to four times per day. Be sure to avoid offering foods that pose choking hazards such as grapes, peanuts, and popcorn.
Finger feeding can be fun for your little one. Always be sure that his food is cut up into pieces that are small enough for him to be able to pick up and chew without being at risk of choking. After some practice, he’ll be on his way toward wholesome, independent eating habits.
1-Year-Old Feeding Schedule
Now that you’re celebrating your baby’s first birthday, it’s also time to celebrate his feeding accomplishments. Your baby’s feeding schedule can now include almost all the healthy and nutritious foods you eat, with a few minor exceptions such as raw honey and choking hazards like nuts.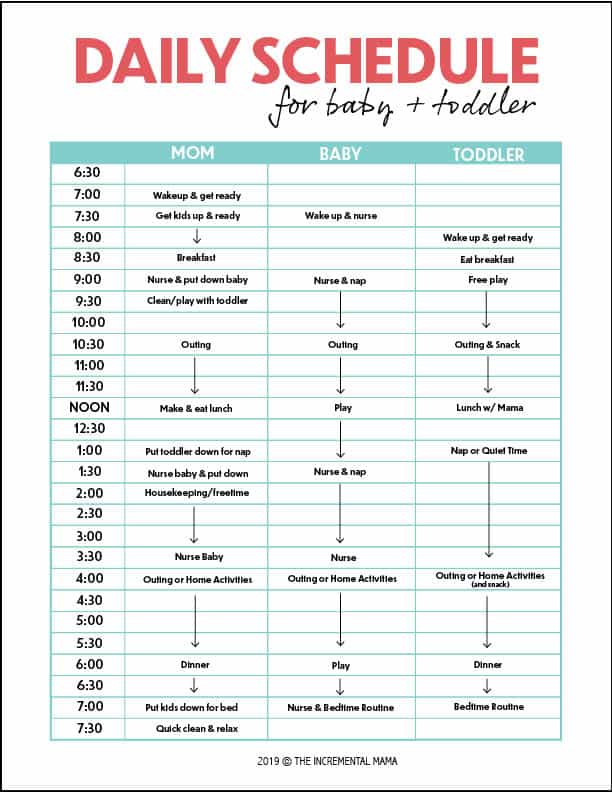
Your baby may be eating less frequently now, as he is able to take in more food in one sitting. Give your 1-year-old approximately three meals and about two or three snacks a day.
This is the time to add cow’s milk to your baby’s diet. However, too much milk is not always good, and should be kept to about 16 to 24 ounces per day if your baby is able to tolerate lactose. Check with your baby's healthcare provider if you have any questions about how and when to introduce cow's milk.
You can continue to nurse your baby if you wish. There is no correct time to wean him off of breast milk; rather, it is recommended that to continue breastfeeding for as long as it is right for you and your little one. Consult with your baby’s healthcare provider if you have questions about the weaning process.
As your baby grows and develops, his feeding needs will change. Having a baby feeding schedule at the ready can help you track your baby’s mealtimes and anticipate when he’ll start to be hungry.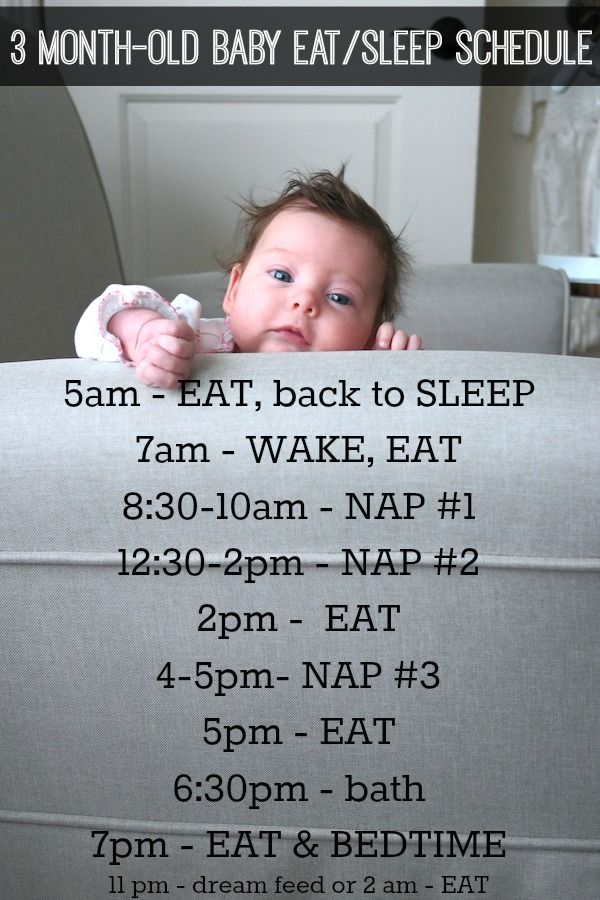
This is just one of the ways you can help keep your little one happy and developing well. Having a feeding schedule in place also gives you some extra freedom to spend more time enjoying his many milestones.
Of course, if at any time you have questions or concerns, reach out to your baby’s healthcare provider for personalized guidance and advice.
How to help improve breastfeeding: questions and answers
-
Milk rivers and jelly banks are an image of a magical and abundant country from folk tales. Probably, there are fewer allergy sufferers in this marvelous region, because the role of breastfeeding (HF) in the primary prevention of atopic (allergic) diseases is undoubted. How to make milk rivers drink and feed the baby, and bring only joy to mom and dad? We will answer the most frequent disturbing questions of novice parents.
Is the baby getting enough milk?
There are only 2 reliable signs that there are NO: weight gain less than 500g / month (for the first half of life) and a small amount of urine (less than 6-8 urination per day).
 For a newborn baby, the criterion that nutrition has improved is the restoration of weight in the second week of life after a natural (in the language of doctors - physiological) loss of body weight at birth.
For a newborn baby, the criterion that nutrition has improved is the restoration of weight in the second week of life after a natural (in the language of doctors - physiological) loss of body weight at birth. How to help a mother who thinks she doesn't have enough milk
To understand why the mother lacks confidence, it is necessary to listen to her and give truthful information about how lactation (milk production) and the feeding process occurs, what is the normal behavior of the child. During the conversation, it is necessary to accept the mother’s opinions and feelings about breast milk and feeding, note all the good points in the feeding technique and in the development of her child, check the correct attachment to the breast (correct possible shortcomings by providing practical assistance to the mother), evaluate the effectiveness of suckling (tell the mother !) and give tips to help you cope with fatigue. It is often helpful and even necessary to talk to family members.
Why might a baby not get enough breast milk?
The most common causes are related to breastfeeding and the condition of the mother - these can be:
- delayed start of feeding (optimally - the first application of at least half an hour in the first 20 minutes after birth, right in the delivery room),
- infrequent feedings or short feedings (feeding "by the clock", "by the rules"), especially - no feedings at night or night breaks for more than 5 hours,
- poor attachment to the breast (see below) and ineffective suckling,
- giving a child before 4-6 months of other foods, other drinks, using bottles with a pacifier (if necessary, it is better to feed from a cup), pacifiers,
- maternal self-doubt/anxiety/stress,
- rejection of the baby, dislike of breastfeeding, fatigue, pain during feeding (eg, fissures, thrush),
- taking combined contraceptives (estrogens in their composition suppress lactation; nursing mothers need drugs selected by a doctor), taking diuretics = diuretics (including tea and coffee), smoking, the onset of a new pregnancy in the mother.

Rare causes are those associated with the condition of the child: illness, developmental anomalies, in which there are difficulties with effective sucking and fatigue, weakness.
There are factors that definitely do not affect the amount of milk: age of the mother, premature birth, operative birth (caesarean section), menstruation, sexual life, return to work (if the child continues to suckle frequently or the mother expresses milk regularly), the age of the child , large families or the birth of twins / triplets, a simple (regular) diet.
How can I help increase lactation?
You have to let nature work on it. The mechanisms of lactation are very reliable, unless the mother and her immediate environment interfere with their anxiety.
Firstly, the mother needs to eat, drink and rest enough, and let the child be next to her, so that it is the mother who does everything for him now.
Secondly, when feeding, the mother needs to learn to relax, using these wonderful minutes to focus on the baby, eye-to-eye and skin-to-skin contact, gaining good thoughts and feelings about the baby.
 It will be useful for mom to drink something warm, soothing (but not coffee) before applying, sit comfortably in a warm corner, warm the chest (for example, a warm shower, a warm compress on the chest), and not be distracted by the phone and TV. Therefore, at first, it is useful to slightly distance the family and take a bunch of useful things in the kitchen, around the house and beyond; this will give mom and baby time and peace - what you need for mom's lactation hormones to work.
It will be useful for mom to drink something warm, soothing (but not coffee) before applying, sit comfortably in a warm corner, warm the chest (for example, a warm shower, a warm compress on the chest), and not be distracted by the phone and TV. Therefore, at first, it is useful to slightly distance the family and take a bunch of useful things in the kitchen, around the house and beyond; this will give mom and baby time and peace - what you need for mom's lactation hormones to work. The most important advice is to allow the baby to breastfeed as often as possible: as soon as he shows interest (this is called "baby-initiated feeding"), in the first 1-2 months - approximately every 2 hours during the day and every 4-5 hours at night. To increase or maintain lactation, even pumping (imitation of another attachment to the breast) can be useful: the mother's body will respond to an increase in “demand” with an increase in “supply”. It is IMPORTANT not to limit either the frequency or duration of breastfeeding!
The second most important tip is to make sure that the baby is attached to the breast correctly and suckles effectively (see below).

How do you know if a baby is properly attached to the breast and suckles effectively?
Just watching the feeding process. Breastfeeding is a skill that mom and baby learn together, both sides of the process learning. And we - doctors and sympathetic family members - can help our "students". Here is the cheat sheet:
Signs that everything is RIGHT Signs that there are DIFFICULTIES with attachment - when suckling, the baby's mouth is wide open,
- his lower lip is turned out,
- the child's tongue "hugs" the mother's breast from below, it is visible,
- baby's cheeks are round,
- the child covers with his mouth not only the nipple, but almost the entire areola, and especially from below (the areola may be more visible above his upper lip).
- sucking slow, deep, with pauses,
- can see and/or hear swallowing,
- the mother is comfortable, she is relaxed, calm, looking at the child, stroking him, “cooing”
- breasts appear round during breastfeeding,
- the child's body is pressed against the mother's, his chin (and often his nose) touches the chest, the child's head and body lie in the same plane,
- the mother supports the baby by the buttocks (important in the first months of life)
- the child's mouth is not wide open, lips are pulled forward,
- lower lip not turned out,
- child's tongue not visible,
- cheeks tense and drawn in,
- the areola is more visible under the child's mouth
- sucking - fast only,
- smacking and clicking can be heard,
- the mother is uncomfortable: her shoulders are tense, she bends over the child,
- mother and child do not look at each other, the mother shakes the child, touches him little, supports only the head and shoulders, presses her finger on the chest
- the child's body is not pressed against the mother, his chin does not touch her chest, the child's neck is turned
- breasts seem to be stretched out during feeding,
- Possible breast engorgement, milk duct obstruction, mastitis, cracked and sore nipples, flat and inverted nipples
How to deal with breast engorgement, blockage of the milk duct, the initial stage of mastitis?
Signs of breast engorgement: the breast is painful, swollen, dense (especially the nipple), milk does not flow out, the skin may become shiny, reddened, body temperature may rise up to a day.
 What to do? - Do not let the breast "rest"! If the baby is able to suck - feed often, help to properly attach the baby to the breast (if the baby is not able to suck - express milk manually or with a breast pump). To facilitate feeding - before feeding (pumping): a warm compress or shower, massage of the neck and back, light self-massage of the mammary glands, and after feeding - a cold compress on the mammary glands to reduce swelling.
What to do? - Do not let the breast "rest"! If the baby is able to suck - feed often, help to properly attach the baby to the breast (if the baby is not able to suck - express milk manually or with a breast pump). To facilitate feeding - before feeding (pumping): a warm compress or shower, massage of the neck and back, light self-massage of the mammary glands, and after feeding - a cold compress on the mammary glands to reduce swelling. For blockage of the milk duct and mastitis: first improve the outflow of milk. To do this: first of all, correct poor attachment to the breast, eliminate the pressure of clothing (underwired bra) or fingers (incorrect support of the breast during feeding) on the mammary gland, try to change positions during feeding, breastfeed more often (option - pumping) , before feeding and at the beginning of feeding, do a light self-massage of the breast towards the nipple, a warm compress on the chest; if there are nipple cracks, start their treatment.
 Then discuss the need for medication with your doctor.
Then discuss the need for medication with your doctor. When is expressing milk useful? And in general - is it necessary to express "to the last drop" after each feeding?
Pumping as a routine recommendation (to everyone and everyone, after each feeding, “to the last drop”) is not necessary! However, you may come across a situation where the skill of pumping is very useful to you, in particular:
- to alleviate the condition and help the baby adjust to the breast during engorgement
- with lactostasis, blockage of the milk duct
- when feeding is difficult - with inverted nipples, difficulties in coordinating sucking, or immaturity / prematurity / low birth weight, if the baby is sick and cannot suckle independently (what is the "banal" rhinitis!) or "refuses to breastfeed"
- to maintain lactation while the mother or child is seriously ill
- to maintain lactation and leave breast milk to the baby when the mother needs to be away or at work
- to form a “gold reserve” in your freezer and build self-confidence.

In what situations is breastfeeding still contraindicated?
The World Health Organization names only six situations when a different way of feeding a child should be chosen, namely:
- Mother has psychosis
- The mother has an open form of tuberculosis
- Mother has HIV/AIDS
- The mother was treated with cytostatics; antithyroid drugs; taking radiopharmaceuticals.
- The child is planned for adoption (adoption).
- The child has metabolic disorders: phenylketonuria, galactosemia.
At the end of this article I will say: breastfeeding is such a short period in the life of your baby, but extremely important and full of meanings. The theme is almost inexhaustible! The main thing - with questions, anxieties and doubts, listen to yourself, pick up the baby's signals, look for reliable information in reliable sources. It is good if there are girlfriends / relatives with successful (recent) breastfeeding experience, an interested caring pediatrician, a breastfeeding consultant.
 As a fallback - books by William and Martha Sears.
As a fallback - books by William and Martha Sears. I wish you enjoy the GW!
Yasnova Yu.A., allergist-immunologist
Return to the list
Answers to statements about observance of rights in childbirth
Dear pregnant women and women planning pregnancy!
Due to the increase in the number of similar applications received “On taking into account the rights and interests in childbirth” to the administration of the Healthcare Institution “5th City Clinical Hospital” Minsk, we give the following explanations.Labor management and methods of delivery in the maternity hospital of the 5th City Clinical Hospital are carried out in accordance with the Clinical Protocol "Medical supervision and medical care for women in obstetrics and gynecology" (2018), and also comply with WHO recommendations (2018). Now a few comments and clarifications on the points of your statements:
“Ensure the presence and participation of my partner, who is my birth representative, during the entire birth process for continuous support throughout the birth.
 If possible, first contact my partner with questions upon admission to the maternity hospital, during childbirth as a representative or intermediary in effective communication, if I myself cannot answer them, I do not come into contact with you while in active labor.
If possible, first contact my partner with questions upon admission to the maternity hospital, during childbirth as a representative or intermediary in effective communication, if I myself cannot answer them, I do not come into contact with you while in active labor. – Participation and presence of a partner during childbirth is possible if there is a contract for partner childbirth, a certificate for attending courses to prepare for childbirth and a health certificate of the partner.
"I refuse to shave the perineum and pubic area during natural childbirth, enemas upon admission to the maternity hospital."
- Shaving the perineum and pubic area, whether in childbirth or not, is a personal hygiene product and method. This is not practiced in our maternity hospital.
“Perform labor without medical intervention to speed it up, if my condition and the condition of the fetus is acceptable (oceitocia, etc.
 ) and anesthesia without my asking for it during labor (except in cases of vital indications).
) and anesthesia without my asking for it during labor (except in cases of vital indications). If it is necessary to use medical procedures and injections of drugs for me or my child (for vital indications), please notify me of the purpose of their use, the name of the drug (procedure), indications, contraindications, side effects and obtain my written informed consent to them holding.
Please do not perform routine fetal cardiotocography or continuous cardiotocography (preferably only if the fetus is at risk), do not lie down if it makes me uncomfortable, but be able to sit or stand, move, sit on a fitball, choose poses according to their feelings in childbirth; in other cases, listen to the heartbeat with a stethoscope) and do not conduct frequent vaginal examinations (if necessary, 2-3 examinations, do not use routine washing of the vagina with medical solutions).
Do not open the amniotic sac to induce labor. If it is necessary to use amniotomy in the active phase of the first stage of labor, please obtain my written informed consent for its implementation.

I refuse routine or free perineal incision (any perineal incision), provided that it does not endanger the life of my child and there is no indication for me personally, of which I have been informed and changed my mind.
- Any medical manipulations, diagnostic measures, injections are prescribed according to indications (that is, not for everyone) and are carried out after your information and the consent of the woman in labor.
“Please give me the opportunity to move freely and change positions during the contractions (including using a fitball and other devices).
Please give me the opportunity to take a comfortable position for me during the attempts, taking a comfortable vertical position for me, since in this position each attempt requires less effort and the child during childbirth reduces the likelihood of injury. If it is impossible to carry out the straining period outside the maternity chair, put the back of the chair at an angle.

I ask for obstetric support in natural straining during the period of fetal expulsion, which is facilitated by not giving birth lying on your back, the ability to change positions in search of a comfortable attempt and allow gravity and the body to move the child in a natural way, breathing at the contraction instead of pushing on command, refusal of manual pressure on the abdomen in attempts to facilitate childbirth.
- During all stages of childbirth, you can choose any position that is convenient for you. But we clarify that a position that is convenient for you in the second stage of labor may not allow the medical staff to control the obstetric situation and the condition of the fetus, which can lead to late diagnosis and, consequently, to late assistance. In addition, the upright position at the end of the second period increases the risk of perineal tears involving the rectum.
“Do not clamp or cut the cord until the pulse is over (about .
 10 to 15 minutes, the cord will look almost empty, whitish and hard by then) and leave the baby at the level of my pelvis for that time. This is necessary so that the child can fully receive all the blood that is in the placenta due to him.
10 to 15 minutes, the cord will look almost empty, whitish and hard by then) and leave the baby at the level of my pelvis for that time. This is necessary so that the child can fully receive all the blood that is in the placenta due to him. After clamping the umbilical cord, put the baby on my stomach and cover us with a blanket - for direct bodily contact and postpone all procedures for 1 - 2 hours (measurements, tests), if his condition allows - for the period of imprinting (establishing contact with mother ), the formation of the microbiome, the ability to attach to the breast after birth and the stimulation of breastfeeding, the prevention of hypothermia or overheating.
- According to WHO recommendations, after the birth of a child without clamping the umbilical cord, it is laid out on the mother's stomach to ensure the temperature regime ("thermal chain") and to establish skin-to-skin bodily contact. The pulsation of the umbilical cord does not last so long (1-3 minutes), the time interval is individual.
 Our maternity hospital uses the Delayed Cord Transection Technology.
Our maternity hospital uses the Delayed Cord Transection Technology. “Do not use nasal or oral suction if the baby was born with clear amniotic fluid and has begun to breathe on its own. Do not wash or wipe off the baby's primordial lubrication immediately after birth, bathing no earlier than 24 hours later. Do not treat your eyes and genitals with antibacterial drugs. Examination of the child is carried out only externally.
- Aspiration of the contents of the upper respiratory tract is not performed if the amniotic fluid is clear and the baby breathes on its own, the primordial lubrication is not washed off and wiped off immediately after birth, and the healthy baby is not bathed. A neonatologist conducts the first examination of a newborn immediately after birth, on the mother's belly, in compliance with all the rules of thermal protection. A full medical examination, weighing, measurement can be delayed and carried out during the first hour of life.

“Do not use oxytocin to release the placenta, do not pull the cord, do not squeeze out postpartum blood. If there are no acute indications, do not manually separate the placenta, at least for an hour (the child, sucking on the breast, allows the natural discharge of the placenta). Don't do prolonged uterine massage."
- Separation and excretion of the placenta is a natural process. Without indications (bleeding), the medical staff does not interfere in this process. The WHO-recommended "active management of the third stage of labor" is not used in our maternity hospital. But delaying the release of the placenta for 30 minutes is a clear indication for its removal, as this increases the likelihood of life-threatening postpartum hemorrhage.
“Do not separate me from my child unless there is a vital indication. I want to be with him at all times immediately after he is born, and my labor partner can provide the necessary assistance with this for 2 hours prior to transfer to the postpartum ward.
 If there is an urgent need for separation within 2 hours after birth or later, let it be a period of no more than 30 minutes. My labor partner may be with the baby if necessary prior to transfer to the postpartum ward.”
If there is an urgent need for separation within 2 hours after birth or later, let it be a period of no more than 30 minutes. My labor partner may be with the baby if necessary prior to transfer to the postpartum ward.” - Under conditions that do not require assistance to you and / or your baby, the newborn is with you for 2 hours in the delivery room in skin-to-skin contact.
“I refuse to vaccinate my child (hepatitis B and tuberculosis (BCG).”
- Refusal of preventive vaccination is documented in the patient's medical records and signed by the patient (the person specified in part two of Article 18 of the Law of the Republic Belarus "On Health Care") and the attending physician and is the right of the patient
“I stop supplementing and supplementing my baby if I am physically able to breastfeed my baby: I am conscious after giving birth and able to feed my baby on my own.”
- Supplementary feeding for a child is prescribed individually by a neonatologist in cases requiring additional nutrition, when there is a threat to the health of the child in the absence of adequate feeding.
"All procedures, swaddling, examination by a neonatologist, taking tests, must be carried out only in my presence."
- In the maternity hospital, a neonatologist examines a newborn child in the presence of the mother, unless the newborn child is being treated in the intensive care unit or the mother's condition does not allow her to be present during the examination of the newborn. Blood sampling for tests and procedures are carried out in the presence of the mother, if she wishes.
"Refusing fluorography in the postnatal ward."
- Fluorography in the postpartum period is not performed in the maternity hospital.
“Early discharge at will, not earlier than 24 hours, without waiting for the umbilical cord to fall off.”
- Discharge from the maternity hospital is carried out no earlier than 3 days of the postpartum period, which is associated with the need to examine the newborn (after 60 hours of life) and adhere to the vaccination schedule.