Baby sleepy and not feeding
Breastfeeding a Sleepy Baby - Breastfeeding Support
Newborn babies feed a lot and sleep a lot. But what if a baby seems to sleep all the time or keeps falling asleep as soon as they start breastfeeding? Can a baby be too sleepy? This article looks at newborn sleep, how often babies need breast milk and how to feed a sleepy baby. It is a companion article to How Often Should a Newborn Feed?
Find an IBCLC
Search for a breastfeeding expert near you
How long do newborn babies sleep?
Newborn babies sleep a lot, they may sleep for 18 hours out of every 24—usually for two to three hours at a time1 with perhaps one longer sleep of four to five hours2 . It is common for a baby to be particularly sleepy in the first 24 hours after birth 3.
How often should a newborn feed?
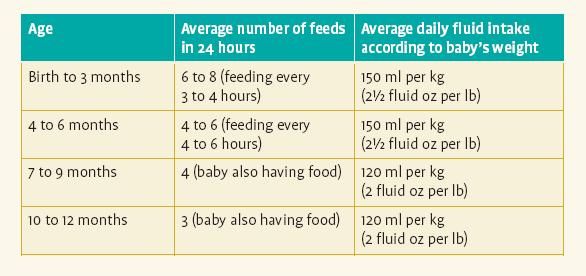
A breastfed baby generally feeds every two to three hours or more around the clock because breast milk is quickly digested and they only have small amounts at a time. For much more information see How Often Should a Newborn Feed? The excerpt below explains:
Excerpt from
How Often Should a Newborn Feed? Breastfeeding Support, 2019
Newborn babies sleep a lot, they may sleep for 18 hours out of every 24—usually for two to three hours at a timeBreast milk is easily and quickly digested—even as quickly as one hour—and babies have tiny tummies so they need to feed little and often. It is usually recommended that a baby has at least 8-12 feeds in 24 hours i.e. that they breastfeed every two to three hours from the start of one feed to the start of the next and this ties in with a newborn’s sleep patterns. Some babies may feed more frequently e.g. every hour at first.
How long should a newborn sleep without feeding?
How long a baby should sleep in one go will usually depend on how much milk they are getting at the breast during a breastfeed. How much milk a baby can get will depend on how much milk a breast can store (breast storage capacity), the latch (the way a baby attaches to the breast) and how many total feeds the baby has during any given 24 hour period. Feeding in clusters with occasional longer periods of sleep is normal especially when there are at least 8-12 feeds over a 24 hour period. If a baby is waking for lots of frequent feeds and feeding actively with plenty of swallows of milk and plenty of wet and dirty nappies and gaining weight, they can usually be left to sleep and feed on demand to their own timetable. If not, then reminding and encouraging a sleepy baby to breastfeed every two to three hours during the day and every four hours at night can be important to avoid them being underfed.
How much milk a baby can get will depend on how much milk a breast can store (breast storage capacity), the latch (the way a baby attaches to the breast) and how many total feeds the baby has during any given 24 hour period. Feeding in clusters with occasional longer periods of sleep is normal especially when there are at least 8-12 feeds over a 24 hour period. If a baby is waking for lots of frequent feeds and feeding actively with plenty of swallows of milk and plenty of wet and dirty nappies and gaining weight, they can usually be left to sleep and feed on demand to their own timetable. If not, then reminding and encouraging a sleepy baby to breastfeed every two to three hours during the day and every four hours at night can be important to avoid them being underfed.
Can babies be too sleepy?
Yes, sometimes babies can be too sleepy and if they are not getting enough milk because they are so sleepy or not feeding very well they can begin to sleep even more and feed even less. A baby who is not feeding frequently or not feeding well may become more and more difficult to rouse. If a baby is very sleepy, they could be at risk of higher than normal weight loss or poor weight gain, higher than normal levels of jaundice and a sleepy baby is a big risk factor for low milk supply because removing milk from the breasts regularly is an important signal to make more milk. If a baby continues to be sleepy and not feed well after a mother’s milk comes in, there is a higher risk of the mother’s breasts getting engorged or getting mastitis. Mastitis or engorgement can make a mother feel very poorly and reduce a milk supply further.
A baby who is not feeding frequently or not feeding well may become more and more difficult to rouse. If a baby is very sleepy, they could be at risk of higher than normal weight loss or poor weight gain, higher than normal levels of jaundice and a sleepy baby is a big risk factor for low milk supply because removing milk from the breasts regularly is an important signal to make more milk. If a baby continues to be sleepy and not feed well after a mother’s milk comes in, there is a higher risk of the mother’s breasts getting engorged or getting mastitis. Mastitis or engorgement can make a mother feel very poorly and reduce a milk supply further.
Encourage a sleepy baby to feed
Encouraging a sleepy baby to have regular breastfeeds and helping them to stay awake long enough to finish a feed will both protect the mother’s milk supply and keep baby well fed to protect their health (see below).
Why might a baby be too sleepy?
Reasons for being particularly sleepy might include:
- A difficult birth or birth interventions such as ventouse, forceps or if a mother has received any pain relieving drugs that have affected baby.
- Prematurity, health issues or other medical reasons can make a baby sleepy.
- Breastfeeding problems. If a baby is not getting enough milk they will have less energy and this can quickly make them more sleepy. Sometimes a baby may seem to be breastfeeding but actually they are sleeping with the breast in their mouth and not swallowing anything or very little.
- Jaundice (yellowing of the skin due to a build up of bilirubin) can make a baby sleepy and is more likely in a baby who is not getting enough milk creating a vicious cycle.
- Overstimulation. If a baby is overstimulated by excessive handling by strangers or even family members, bright lights or constant loud noise they might tend to shut down and go to sleep to escape.
- Missed feeding cues. When a baby is swaddled 4, has a pacifier, is too warm or is not in close contact with his mother there is a higher chance of missing feeding cues so that a baby sleeps for longer and feeds less.
- Severe breast engorgement. Severe breast engorgement after the birth may hinder baby getting milk and any unrelieved engorgement will tend to reduce a milk supply. If less milk is available a baby may become sleepier. Conversely, if a baby is already very sleepy and not feeding well there is a higher chance that a mother may experience painful engorgement (swollen breasts full of milk) leading to a vicious cycle of sleepy baby getting less milk, breasts reducing supply due to the engorgement, less milk for baby and so on. See our articles on Engorged Breasts and Engorgement Relief When Milk Won’t Flow for more information to deal with engorgement.
How can I wake my sleepy baby to feed?
If your baby is not waking at least 8-12 times in 24 hours he may need reminding when to feed. Ideas to wake and feed a sleepy baby include:
Ideas to wake and feed a sleepy baby include:
- Look for light sleep and feeding cues. A baby can breastfeed in light sleep and it’s easier to latch or wake a baby in light sleep i.e. when his eyes are moving under his closed eyelids (rapid eye movement or REM) and he is starting to move, fidget or fuss in his sleep. Other feeding cues include a baby sucking his fists or fingers, opening his mouth and turning his head from side to side to search for the breast (rooting). It can be helpful to cluster feed in these light sleep/more active periods.
- Hold your baby. Sometimes just picking up and holding your baby in a breastfeeding position will motivate him to begin rooting and latch on (attach to the breast). Holding your baby as much as possible allows you to spot those moments when your baby is in light sleep and try to latch him on.
- Skin-to-skin. Remove your baby’s clothes so that he is skin-to-skin or lightly dressed against his mother’s chest.
 Being held in skin-to-skin contact in a tummy down position against a mother’s chest is a great position to trigger a baby’s feeding reflexes. In this position, babies will often start actively searching for the breast using their hands and mouth even if they are not fully awake. Skin-to-skin contact can therefore encourage more breastfeeds5. The mother’s body will keep baby warm, a blanket can be draped over mother and baby as needed. See Why Skin to Skin? for more explanation of how helpful this technique can be used at any time in the early weeks not just after the birth. Remember to remove any scratch mittens.
Being held in skin-to-skin contact in a tummy down position against a mother’s chest is a great position to trigger a baby’s feeding reflexes. In this position, babies will often start actively searching for the breast using their hands and mouth even if they are not fully awake. Skin-to-skin contact can therefore encourage more breastfeeds5. The mother’s body will keep baby warm, a blanket can be draped over mother and baby as needed. See Why Skin to Skin? for more explanation of how helpful this technique can be used at any time in the early weeks not just after the birth. Remember to remove any scratch mittens. - Change baby’s nappy. Changing a baby’s nappy will often rouse them. Some parents combine this with gentle massage of hands and feet.
- Different positions. Try holding your baby in different breastfeeding positions to see if any help him to stay awake.
 Some babies may be more wakeful in a rugby hold or in an upright position such as a straddle hold compared with a traditional cradle hold. Some may be more active in reclining positions while some may fall into a deep sleep. You can see the different positions to try in Breastfeeding Positions for Newborns.
Some babies may be more wakeful in a rugby hold or in an upright position such as a straddle hold compared with a traditional cradle hold. Some may be more active in reclining positions while some may fall into a deep sleep. You can see the different positions to try in Breastfeeding Positions for Newborns. - Dimming the lights. Bright lights can make a baby want to shut their eyes which encourages sleep, try soft lighting instead.
- Quiet time. Try to create a peaceful atmosphere so baby does not get overstimulated. Passing a baby around family members and constant loud noise can cause some babies to “withdraw” and go to sleep to escape.
- Avoid a dummy. A dummy can encourage a baby to sleep longer. Sucking releases hormones to pacify or calm baby back to sleep and can therefore lead to missed feeding opportunities. See Pacifier, Dummy or Soother, Yes or No?
How do I keep my baby awake during feedings?
Getting baby latched and drinking well at the start of a feed is not always the end of the story. Once the initial let-down subsides, a sleepy baby is quite likely to fall asleep again before he has finished the feed. The following ideas can help your sleepy baby to feed effectively:
Once the initial let-down subsides, a sleepy baby is quite likely to fall asleep again before he has finished the feed. The following ideas can help your sleepy baby to feed effectively:
Skin-to-skin. Undressing your baby and placing them skin-to-skin on your chest maximises their feeding reflexes and helps stimulate feeding cues.
Position and latch. If your baby is not latched and positioned well it will be difficult for them to get milk (and breastfeeding may hurt!). Check positioning in Breastfeeding Positions for Newborns and see Latching Tips and Why Does Breastfeeding Hurt? Try different positions, upright positions may help your baby stay awake to breastfeed longer.
Breast compressions. Putting gentle pressure on the breast with a free hand while baby suckles can help to keep milk flowing at a faster pace and so keep a baby feeding longer. See What is Breast Compression?
Keep switching sides. As soon as sucking slows on the first breast offer the other breast before baby falls asleep. By switching and repeating you can help to keep baby awake and feeding actively for longer.
By switching and repeating you can help to keep baby awake and feeding actively for longer.
Look for active feeding. Watch your baby carefully. Is he actively moving his jaw to suck and can you hear swallowing or see the pause in his suck as he swallows? Watch for the baby who is frequently flutter sucking or comfort nursing but not swallowing anything. If your baby isn’t getting enough milk he will probably fall asleep hungry and your milk supply will continue to drop.
Express and top up if needed. If baby is still falling asleep before he has had enough to eat, pumping and topping him up with expressed breast milk will help his energy levels for feeding longer at the next feed. The more breast milk your baby gets the sooner he will be more wakeful and better able to breastfeed effectively. And pumping will protect your supply, only by frequent emptying of the breasts will they know to make more milk.
Get support. Mothers across the world have traditionally taken several weeks to nest with their newborn baby and get breastfeeding established. Finding support with preparing meals or looking after older children can be invaluable. Your sleepy baby will benefit from your focussed attention to get breastfeeding established. And if your otherwise healthy baby continues to be sleepy or is not feeding very well seek the help of a breastfeeding specialist e.g. an IBCLC lactation consultant.
Finding support with preparing meals or looking after older children can be invaluable. Your sleepy baby will benefit from your focussed attention to get breastfeeding established. And if your otherwise healthy baby continues to be sleepy or is not feeding very well seek the help of a breastfeeding specialist e.g. an IBCLC lactation consultant.
How can I tell if my baby is feeding well?
Our sister article How Often Should a Newborn Feed? explains:
Excerpt from
How Often Should a Newborn Feed? Breastfeeding Support, 2019
When a baby is feeding actively, even if they look like they are asleep, the baby’s jaw will move as they suck and they will swallow regularly e.g. in a pattern of one or two sucks per swallow for 10-15 minutes or more at a time from one or both breasts. The length of time a baby is attached to the breast is not as important as how effectively that baby is feeding. Even if a baby is latched on for an hour, if he isn’t feeding actively with plenty of swallows of milk he might not be getting enough milk.

It is important to be aware that just being attached to the breast and making mouth movements alone doesn’t guarantee that a baby is drinking well. Although a baby can feed well in their sleep sometimes, other times they can be dreaming about sucking but not swallowing, sometimes for hours at a time. It’s helpful to be able to tell the difference between active feeding and flutter sucking and comfort nursing. The way the baby is attached to the breast is important too—see Latching Tips.
Even if a baby is latched on for an hour, if she isn’t feeding actively with swallows of milk she might not be getting enough milkIs my baby getting enough milk?
There are lots of ways to determine whether a baby is getting enough breast milk without seeing the volume that has been drunk e.g. looking for active feeding, plenty of dirty nappies and weighing baby regularly. See Is My Baby Getting Enough Milk? and Breastfed Baby Poop for more reading. How Often Should a Newborn Feed? has a guide to the volumes of breast milk a newborn baby might need at each feed.
What if my baby is too sleepy to breastfeed?
If, despite trying the ideas above, your baby is still not waking up to breastfeed, or is latching but not actively getting enough milk, supplements of expressed breast milk will keep them well fed. Topping your baby up every two to three hours will give him more energy to wake up to breastfeed at the next feed. A baby is much more likely to be able to breastfeed effectively if they are gaining weight. Expressing your milk as often as baby ought to be feeding (at least eight times a day) will stimulate the breasts to make more milk and provide the perfect supplement for your baby. If you can’t express any breast milk to keep your baby well fed, and if donor milk is not available, your baby may need infant formula until you can get more help with your milk supply.
- Check in with your health professional if your baby is consistently too sleepy to breastfeed to make sure they are not poorly or getting dehydrated.
- Hand expressing or pumping your milk will protect your milk supply and provide a breast milk supplement to keep your baby fed until they can breastfeed. See Hand Expressing, How to Increase Milk Supply When Pumping and How Long Does Breast Milk Last?
- Supplementing a sleepy baby. A sleepy baby can be given small amounts of expressed breast milk (or formula if needed) by teaspoon, syringe or bottle. If your baby is alert and awake but not ready to latch on, another option is to offer a cup feed. Although a bottle teat could introduce a bottle preference or teat confusion it can be helpful for a very sleepy baby who needs larger volumes. Following the ideas in Tips to Bottle Feed your Breastfed Baby and Best Bottle for a Breastfed Baby can help minimise any problems.
If a baby is too sleepy to breastfeed properly a supplemental nursing system is probably not going to be helpful at this stage as it relies on a baby sucking actively.
- Check in with a breastfeeding specialist for tailored suggestions to help your baby breastfeed well and maximise your milk supply.
Poor weight gain
A sleepy baby who is not feeding well is at risk of not gaining enough weight or losing weight. This situation can be prevented or quickly reversed by expressing your milk to both protect your milk supply and to keep your baby well fed until you can get more urgent help with breastfeeding. With more milk inside him, your baby will have more energy to stay awake and breastfeed. See Baby Not Gaining Weight, Supplementing an Underweight Baby and How Often Should a Newborn Feed? for much more information.
Try different positions, upright positions may help your baby stay awake to breastfeed longerBabies do sleep a lot but they will normally wake every two to three hours to feed. If a baby is not waking to breastfeed and is constantly sleeping longer than two to three hours, reminding them to breastfeed can both keep your baby well fed and healthy and also protect your milk supply. Hand expressing or pumping your breast milk to provide a supplement for a sleepy baby may sometimes be needed for a while. There is no advantage to keep weighing a sleepy baby every few days and watching their weight stay the same (or go down) hoping it will pick up eventually. Getting help with breastfeeding as soon as possible will be much more effective in protecting your milk supply and getting breastfeeding on track.
Footnotes & References
-
Normal Sleep Development, Baby Sleep Info Source (BASIS), 2019
-
Mohrbacher, Breastfeeding Answers Made Simple, 2010 p 86
-
ABM Clinical Protocol #5: Peripartum Breastfeeding Management for the Healthy Mother and Infant at Term, ABM Revision 2013
-
Franco et al, Influence of swaddling on sleep and arousal characteristics of healthy infants.
 Pediatrics, 2005
Pediatrics, 2005 -
ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Revised 2017
Sleepy Baby – Why And What To Do
Nobody likes to disturb a sleeping baby, but sometimes a baby can be too sleepy for their own good. At times like this they may need you to take action.
Your newborn baby needs to nurse actively for one or both breast at each feed. Offer the second breast after they seem to have finished at the first, although they may not want both sides at every feed.
What makes a baby sleepy?
Recovering from birth: In the first few days, some babies are sleepy or uninterested in feeding. It’s especially true for small babies, after a difficult labour or birth, or if you received drugs for pain relief during labour.
Jaundice or an infection may make a baby sleepy. Newborn jaundice is normal but frequent breastfeeding helps prevent it becoming a problem.
Not enough milk: Your baby may sleep to conserve energy if they are not getting enough food. They may also sleep longer that is good for them if they are apart from you.
Is my baby too sleepy?
To gain weight and stimulate your milk production, expect your newborn to:
- Breastfeed effectively at least 8–12 times in 24 hours
- Feed actively from one or both breasts at each feed, swallowing regularly.
- Nurse at least every 2–3 hours from the start of one feed to the next, with one longer sleep of 4–5 hours.
- Have periods where they breastfeed on and off for several hours, usually in the evening.
- Gain weight from day 4 and regain birth weight by about two weeks.
Look at our page Beginning Breastfeeding for more information. If your baby is too sleepy to do all these things they may need your active help to ensure they are nursing effectively and getting enough milk.
Is my baby getting enough milk?
A baby may lose up to 7% of their birth weight during the first few days. From around day 3-4, expect them to start gaining, and to regain their birth weight by 10-14 days. Many breastfed babies gain around 200-235g (7-8oz) as week for the first 2-3 months. If you baby consistently gains less, or they haven’t regained their birthweight by 14 days, seek skilled help to assess whether they are getting enough milk. What comes out is a sign of what has gone in, so counting dirty nappies can be a useful guide between weighing sessions. For more information to help you know if your baby is getting enough milk in the first few days, you could read our article here about signs of effective feeding in the early days. And then after the first few days, this article will help you decide if your baby is getting enough milk.
From around day 3-4, expect them to start gaining, and to regain their birth weight by 10-14 days. Many breastfed babies gain around 200-235g (7-8oz) as week for the first 2-3 months. If you baby consistently gains less, or they haven’t regained their birthweight by 14 days, seek skilled help to assess whether they are getting enough milk. What comes out is a sign of what has gone in, so counting dirty nappies can be a useful guide between weighing sessions. For more information to help you know if your baby is getting enough milk in the first few days, you could read our article here about signs of effective feeding in the early days. And then after the first few days, this article will help you decide if your baby is getting enough milk.
| Age | Dirty nappies per 24 hours |
|---|---|
| 1-2 Day | 1 or 2 greenish-black tarry meconium poos |
| 3-5 days | At least 3 green transitional poos |
| 5+ days | At least 3-5 yellow, loose unformed poos the size of a 2p coin or larger |
Remind your baby to nurse
If your baby is too sleepy or groggy to rouse themselves every few hours, you will need to wake them to feed to ensure they get enough milk. This will be easier if your baby is in a light sleep cycle: watch for rapid eye movements under their closed eyelids, arm and leg movements, sucking activity and changes in their facial expression.
This will be easier if your baby is in a light sleep cycle: watch for rapid eye movements under their closed eyelids, arm and leg movements, sucking activity and changes in their facial expression.
- Aim for your baby to feed at least 10 times in 24 hours, including at least once at night
- Encourage active nursing on the first breast, watching and listening for signs of swallowing.
- Use breast compression (see below) to keep your baby nursing actively.
- Offer the other side in the same way. You can switch back and forth several times if it helps your baby stay awake and feed.
- Encourage cluster nursing whenever your baby is more alert.
- Give expressed milk if they aren’t feeding well.
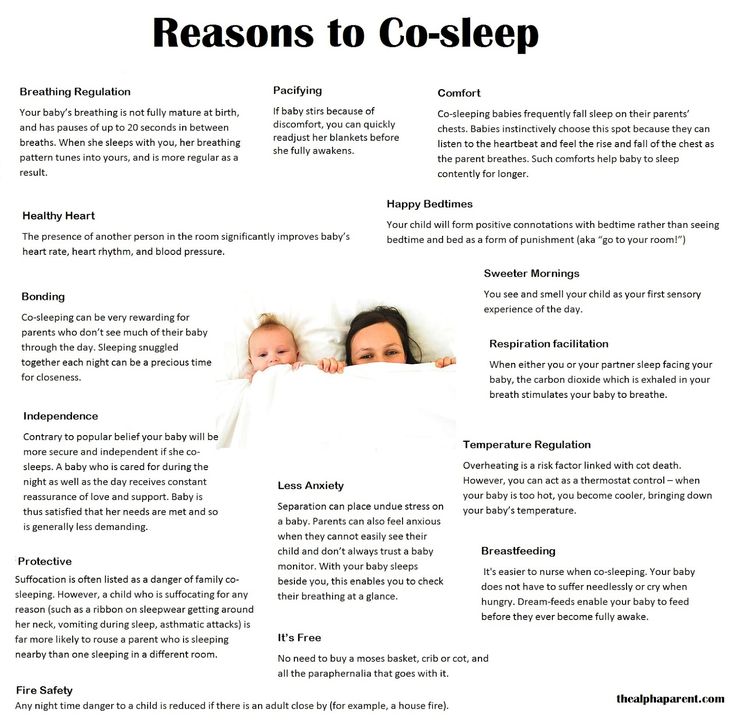
- Keep them close by—day and night—so they don’t sleep too long and you don’t miss their feeding cues.
Also try
- Dimming the lights and keeping your surroundings quiet and peaceful.
- Keeping the room temperature at around 18°C or undressing your baby a little if the room is warm.
 Being too hot can make a baby sleepy.
Being too hot can make a baby sleepy. - Unwrapping any blankets.
Newborn feeding cues
Signs of interest in feeding include:
- Mouth movements; smacking or licking his lips
- Sucking on lips, tongue, hands, fingers, toes, toys or clothing
- Rooting, head bobbing or nuzzling against whoever is holding them
- Fidgting and squirming a lot
- Fussing
- Crying – a late sign of hunger.
Do offer feed generously. A newborn won’t find it easy to feed well, if they have to wait and reached late hunger signs.
Helping your sleepy baby
Positioning and attachment
Getting a deep, comfortable latch is crucial. If your baby is not latched on well at the breast, they will have to work harder to get your milk. They may tire easily and fall asleep. Sometimes just a small adjustment to the way your baby comes to the breast can make a huge difference. An LLL Leader can provide individual suggestions tailored to your circumstances. If your breasts are engorged, gently hand express a little milk and/or ease swelling back with your fingertips to make it easier for your baby to latch on deeply and prevent you getting sore. See our longer article about Positioning and Attachment for more help on how to help your baby latch well, feed effectively and be comfortable for you.
If your breasts are engorged, gently hand express a little milk and/or ease swelling back with your fingertips to make it easier for your baby to latch on deeply and prevent you getting sore. See our longer article about Positioning and Attachment for more help on how to help your baby latch well, feed effectively and be comfortable for you.
Copyright Suzanne Tobin
Seek skilled help early on if you are finding breastfeeding difficult or uncomfortable.
Laid back breastfeeding
Try letting your baby lie on your body with their chest and tummy against you as you recline at about 45 degrees. If they can snuggle up close to your chest for periods of time, even when sleepy or during light sleep, they will often instinctively seek the breast and attach deeply and comfotably even during light sleep. This can be done skin-to-skin or with you and your baby lightly clothed. Watch for signs your baby is stirring and gently encourage feeding. Spending time relaxing like this can make a real difference to how well your baby feeds and how much milk you make. Our page on Comfortable Breastfeeding has more ideas.
Spending time relaxing like this can make a real difference to how well your baby feeds and how much milk you make. Our page on Comfortable Breastfeeding has more ideas.
Breast compression
If your baby starts to doze at the breast, this technique will help him breastfeed actively and take more milk.
- Cup your breast with your hand, near your chest wall, thumb opposite fingers in a C shape. Keep your hand well back from the nipple area.
- Wait while your baby breastfeeds actively, with their jaw moving all the way to his ear. When they stop swallowing, compress your breast firmly. They probably start swallowing again. Hold it squeezed until they stop nursing actively, then release your hand.
- Rotate your hand around your breast and repeat step 2 on different areas of the breast as needed. Go gently—this should not hurt.
Try switching breasts at least two or three times during each feed—when your baby comes off the first breast on their own or when breast compression no longer keeps them breastfeeding actively.
Express milk for your baby
Until your baby gets the hang of feeding you may need to do some work for your baby. If they aren’t latching at all, or is not feeding well and gaining weight, then expressing your milk will help establish milk production. The earlier you start, the sooner you’ll produce plenty of milk. Hand expression is often easiest at first but when your milk comes in combining hand expression with pumping can be most effective.
Giving expressed milk
First, encourage your baby to nurse at both breasts. Watch for swallowing and use breast compression an switch nursing until they stop drinking and start to doze.
Next, give your baby expressed milk until they have had enough. (For more on how to give additional milk, our article here). Giving your baby your expressed milk after breastfeeding can help them overcome sleepiness and feed more effectively next time.
Then, once your baby has settled, express from both breasts switching back and forth and using compressions and hand expression to get the available milk. Store this milk in the fridge ready for the next feed.
Store this milk in the fridge ready for the next feed.
Aim to complete this process within about an hour.
Avoid bottles and dummies
You can give small amounts of expressed milk using a spoon, flexible feeding cup or syringe. If you decid to use bottles for larger amounts, you can give the bottle in a way that helps protect breastfeeding. For more information on ways to give your baby milk and bottles see our article on Bottles and other tools. An alternative is to use a nursing supplement: this acts like a straw to deliver extra milk through a tube along your breast as your baby nurses, avoiding the need for bottles. Our article Nursing Supplementers explains more.
Don’t give up too soon
If your baby doesn’t respond quickly to your efforts to get him to breastfeed more often and more effectively, don’t give up. Keep your baby fed, Keep your supply protected and Keep your baby close. You may find our article on Getting breastfeeding back on track after a tricky start helpful.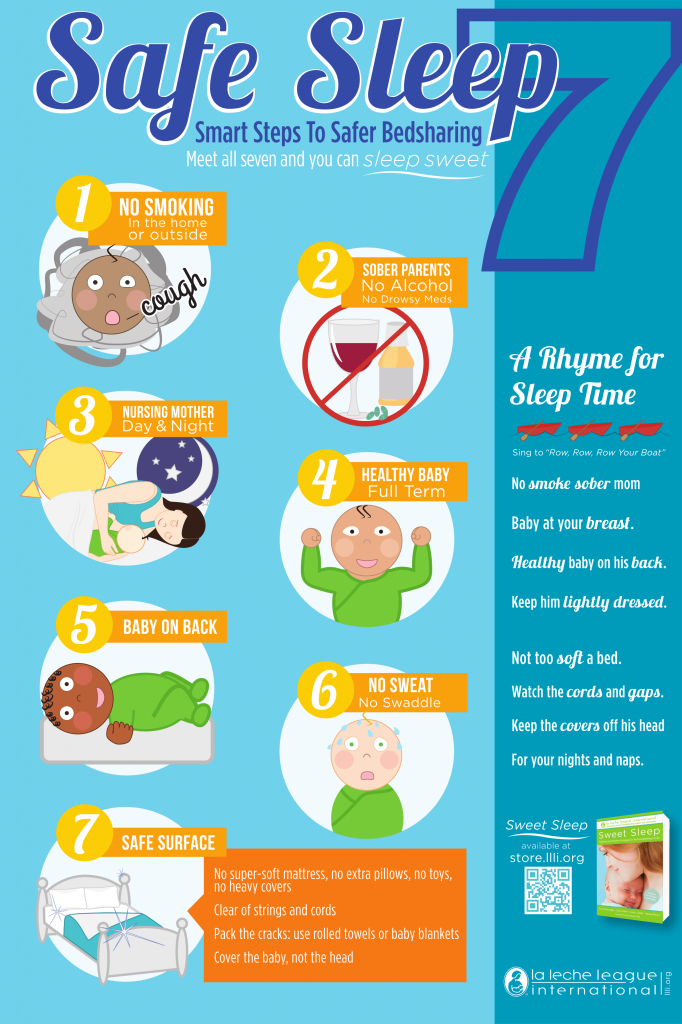 Check with your doctor to eliminate any medical reasons and contact your local LLL Leader to find one-to-one breastfeeding help. You can find support and encouragement from breastfeeding mothers in your local LLL Group too.
Check with your doctor to eliminate any medical reasons and contact your local LLL Leader to find one-to-one breastfeeding help. You can find support and encouragement from breastfeeding mothers in your local LLL Group too.
Written by mothers of LLLGB. Photos courtesy of Ellen Mateer and Suzanne Tobin.
Further Reading
Comfortable Breastfeeding
Positioning and attachment
Engorged Breasts – Avoiding & Treating
Hand Expression of Breastmilk
Is my baby getting enough milk?
My Baby Needs More Milk
Nursing supplementers
Jaundice in Healthy Newborns
Getting back on track after a tricky start – the Three Keeps
My baby won’t breastfeed
Bottles and other tools
Other websites
Biological Nurturing™: www.biologicalnurturing.com/video/bn3clip.html
Natural Breastfeeding Position video, Nancy Mohrbacher:
Benefits of skin-to-skin contact: www.kangaroomothercare.com
Books
The Womanly Art Of Breastfeeding. LLLI, London: Pinter & Martin, 2010
LLLI, London: Pinter & Martin, 2010
This information is available to buy in printed form from our shop.
Copyright LLLGB 2020
Updated June 2022
Children from 0 to 5 years old. When should you urgently take your child to the doctor?
We are all very worried when a child gets sick; including the fear that he will certainly be sent to the hospital. And the children's hospital, as you know, is like this: you get in with one, you leave with another. That is why mothers often refuse hospitalization or postpone a visit to the doctor, hoping that the disease will recede on its own, others prefer online consultations on forums and advice from grandmothers and girlfriends.
Fortunately for all mothers, in most cases, modern medicine makes it possible to diagnose and provide the necessary assistance very quickly, resorting to hospitalization only as a last resort. Something like in the famous series with Hugh Laurie - and MRI, and all the necessary tests, and CT scans, and, most importantly, competent pediatricians and highly specialized specialists. Unfortunately, not all polyclinics have such a set, but in one place in Moscow they definitely have it - in the department of emergency pediatrics of the Federal State Autonomous Institution "NMIC for Children's Health" of the Ministry of Health of Russia, where doctors usually need no more than 2 hours to establish an accurate diagnosis, taking all the necessary analyzes and quickly receive their results, stabilize the child and send him home if there is no threat to life and indications for emergency hospitalization.
Unfortunately, not all polyclinics have such a set, but in one place in Moscow they definitely have it - in the department of emergency pediatrics of the Federal State Autonomous Institution "NMIC for Children's Health" of the Ministry of Health of Russia, where doctors usually need no more than 2 hours to establish an accurate diagnosis, taking all the necessary analyzes and quickly receive their results, stabilize the child and send him home if there is no threat to life and indications for emergency hospitalization.
If you understand that your child needs a prompt consultation with a specialist, but for some reason you postpone the visit to the doctor, if you are afraid that the child will be immediately sent to the hospital ward “to clarify the diagnosis”, or he will not be given due Attention, just come to the pediatric emergency department of the Federal State Autonomous Institution "NMIC of Children's Health" of the Ministry of Health of Russia. Here they immediately do all the necessary research and provide the child with assistance as efficiently and quickly as possible. Every year, more than 3,000 children receive care in the department, and only 2% of them are hospitalized by doctors in a round-the-clock hospital. The rest are sent home after all the necessary procedures with appropriate recommendations, or will be observed for several days in a day hospital. The department accepts children without an appointment, works on CHI, VHI and on a commercial basis.
Every year, more than 3,000 children receive care in the department, and only 2% of them are hospitalized by doctors in a round-the-clock hospital. The rest are sent home after all the necessary procedures with appropriate recommendations, or will be observed for several days in a day hospital. The department accepts children without an appointment, works on CHI, VHI and on a commercial basis.
If your child is between 0 and 5 years old, do not neglect visits to the doctor because your child is at risk. It is this age that accounts for most of the serious diseases that are well studied by medicine, are well treated, but require prompt medical intervention. Tatyana Vladimirovna Kulichenko, Head of the Department of Emergency Pediatrics, FGAU "NMIC of Children's Health" of the Ministry of Health of Russia, Doctor of Medical Sciences, pediatrician of the highest category, WHO expert, spoke about the cases in which it is worth immediately contacting specialists for young children (we are talking about children first 5 years of life).
High temperature (fever)
First, it is important to define what a fever is from a doctor's point of view. Fever is an increase in body temperature greater than 38°C if measured rectally (preferred as this is the most reliable way to determine body temperature in any person) and greater than 37.5°C if measured axillary depression.
Not every fever is a very bad sign, but with children under three years old it is better to play it safe and see a doctor as soon as possible. There are no legislative "terms of patience"; there is no need to wait three days, as pediatricians usually say: all the most severe infections develop very quickly and can be threatening from the first hours of the illness. The sooner you contact a specialist, the better. Examination of the child, instrumental and laboratory studies will help to understand the cause of the fever and quickly stabilize the child's condition.
If a mere fever seems not enough reason for you to see a doctor, then pay attention to the symptoms of intoxication:
- The child refuses to drink (not to eat, namely to drink).

- There is lethargy and drowsiness, it is difficult to establish eye contact with the child (some pediatricians say about such patients "the child looks into himself").
If a child develops a rash on the skin along with an increase in body temperature, then you should go to the doctor immediately.
Cough
Cough is a fairly common symptom in children. Precisely because it seems to be a common, “understandable” sign of illness, parents often miss the moment of timely visit to the doctor. Cough can be caused not only by problems with the organs of the respiratory system. It can signal a malfunction in the cardiovascular or digestive systems. It can even be caused by a sulfur plug in the ear. Until you eliminate the cause, the symptom will not disappear!
Take your child to the doctor immediately if:
- The child is less than 6 months old (whether or not he has a fever or other symptoms).
- The child has a nocturnal cough.
- The child has a cough to the point of vomiting.
- Cough does not go away for more than 3 weeks.
- Barking cough, often accompanied by hoarseness and noisy breathing.
Difficulty breathing
Any difficulty in breathing can be a life-threatening symptom, especially in infants. How to understand that breathing is difficult in an infant: when inhaled, retraction is visible along the edge of the costal arch (the child, as it were, strongly draws in the stomach when breathing). Difficulty in breathing in older children can be noticed if there is no fluency of speech: the child cannot speak in long sentences (as a rule, these are obstructive bronchitis or asthmatic conditions).
Take your child to the doctor immediately if you notice signs of difficulty breathing, especially if the breath is grunting, groaning or you hear wheezing or whistling when breathing even from a distance.
Vomiting, diarrhea (diarrhea, loose stools)
These symptoms are often associated with simple and well-known conditions that are caused by extremely unpleasant, but in modern conditions, with proper treatment, non-life-threatening intestinal infections. But if the child is not fed with special solutions for rehydration, if the volume of fluid losses is not replenished correctly, then vomiting and liquefied stools are dangerous because they lead to rapid dehydration and electrolyte disturbances due to loss of water and salts.
But if the child is not fed with special solutions for rehydration, if the volume of fluid losses is not replenished correctly, then vomiting and liquefied stools are dangerous because they lead to rapid dehydration and electrolyte disturbances due to loss of water and salts.
It happens that loose stools are not a serious problem if it happened, for example, once. If you observe it more often 3 times a day, this is a reason to sound the alarm, especially if you notice the first signs of dehydration:
- Decreased frequency and volume of urination. If your child has not peed for 5 hours, see a doctor immediately!
- Dryness of the skin and mucous membranes: there were fewer tears, saliva, the skin became dry and unusually flabby.
- Thirst.
When to take the child to the doctor immediately:
- The child refuses to drink (does not want to drink despite being very dehydrated).
- The child stops urinating (break more than 5 hours).

- The child is lethargic, capricious, not interested in toys (even if there is no temperature).
- "Sink" eyes or fontanel (this is rare, but it is a formidable symptom).
- There is blood in the stool (even if there is no diarrhea).
Skin rashes
Skin rashes are not always normal. If the rash is accompanied by fever, this is always a reason for urgent medical attention. There are children diagnosed with skin diseases (for example, atopic dermatitis or psoriasis), in which case the parents are usually already trained on how to behave when the rash increases or the skin process worsens. Then you need to go to the doctor if the measures taken previously recommended to you turn out to be ineffective - and you will most likely go to an allergist or dermatologist, i.e. to a specialist you know. But if the rash appeared for the first time, if the rashes are not associated with understandable provoking factors, this is an occasion to consult a doctor. Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
Pain
Pain is always a symptom of anxiety, which the human body signals about danger. An intense and growing pain symptom is always a reason to consult a specialist. Remember that if a child is "teething" - this may be the cause of the child's capriciousness and irritability, but in the vast majority of cases it does not cause a temperature rise above 37.5 * C or severe pain. Therefore, you should not write off the symptoms that have appeared on teething.
How to understand that a child is in pain:
- The child cries, does not calm down.
- Unmotivated excitability.
- Anxiety (the child cannot find peace, a comfortable position).
Head injuries and loss of consciousness
Very often, parents go to the doctor only when the injury leaves traces (hematoma, swelling). If the child fell from a certain height (even if you did not see what exactly he hit), or he hit his head, do not be too lazy to immediately go to a specialist. Not every head injury can pass without a trace, and, most importantly, you may not see the internal damage that occurred during the injury.
If the child fell from a certain height (even if you did not see what exactly he hit), or he hit his head, do not be too lazy to immediately go to a specialist. Not every head injury can pass without a trace, and, most importantly, you may not see the internal damage that occurred during the injury.
An episode of loss of consciousness, "slackness" or convulsions is always a cause for immediate medical attention.
You can read more about the department of emergency pediatrics of the National Medical Research Center for Children's Health on the official website >>>
Increased fatigue in children | Private children's clinic "Children's Doctor" in Yekaterinburg
When a cheerful and reasonable child suddenly becomes lethargic, apathetic, capricious and irritable, when even his favorite games cease to please him, and he has to make incredible efforts to complete the simplest task, you should be wary. Doctors call this condition "asthenic syndrome". And to put it simply, it's about chronic fatigue.
Yes, it is familiar not only to adults. Even children experience a breakdown, especially at school age. This is understandable: the curriculum has changed dramatically in recent years. Requirements for students have increased, and homework has become noticeably more. Let's add visiting sections, circles, tutors to the student's loads, and now he is already falling down. These changes are clearly manifested in winter, when the third, longest quarter of the school year begins. Experts are sure: during this period, children simply need the support of their parents and even doctors.
- Inattention, bad mood and unwillingness to do something is not always laziness, - tells the neurologist of the medical clinic "Children's Doctor" Anastasia Nikolaevna Dron . - If we are dealing with chronic fatigue syndrome, we must understand that it is based on deeper problems. It can be provoked by: excessive activity, common infection (ARVI), anemia, diabetes and hypoglycemia (low blood sugar), and others. This suggests that under the mask of asthenia, sometimes serious diseases are hidden. That is why it is so important to solve this problem together with a doctor who can establish an accurate diagnosis and determine the cause of increased fatigue.
This suggests that under the mask of asthenia, sometimes serious diseases are hidden. That is why it is so important to solve this problem together with a doctor who can establish an accurate diagnosis and determine the cause of increased fatigue.
WILL REST HELP?
It seems that the rest will correct the situation, and if you give the child a day or two to sit back, then everything will work out. However, experts are sure that this is not an option. The student, on the contrary, gets out of the working rhythm even more, and when he again plunges into the educational process, he experiences great stress. Doctors advise to start "with a simple" - to normalize the diet and sleep.
- Asthenic syndrome significantly reduces the quality of life of a child, leads to learning difficulties, complicates communication with peers, and intra-family relationships too, - continues Anastasia Nikolaevna . - In this state, he is not happy with himself, and suffers greatly from his behavior and reactions to events. It is necessary to solve this problem comprehensively. First of all, parents need to optimize the mode of study and rest for their children. It is desirable that they fall asleep and wake up at about the same time, while it is important that they have a full night's sleep, lasting at least eight to nine hours. It is better to do homework with breaks, periodically change the type of activity, arrange breaks more often. In addition, we must not forget that regular exercise is an important part of the prevention and treatment of asthenia in children. And, of course, you should limit your child's stay in front of a computer, tablet, phone, TV to 30 minutes a day. An important aspect is a balanced diet, balanced in proteins, fats and carbohydrates, intake of vitamins and minerals.
It is necessary to solve this problem comprehensively. First of all, parents need to optimize the mode of study and rest for their children. It is desirable that they fall asleep and wake up at about the same time, while it is important that they have a full night's sleep, lasting at least eight to nine hours. It is better to do homework with breaks, periodically change the type of activity, arrange breaks more often. In addition, we must not forget that regular exercise is an important part of the prevention and treatment of asthenia in children. And, of course, you should limit your child's stay in front of a computer, tablet, phone, TV to 30 minutes a day. An important aspect is a balanced diet, balanced in proteins, fats and carbohydrates, intake of vitamins and minerals.
WHAT CAN A DOCTOR HELP?
If you are doing everything right, but there is no improvement, you need to seek help from a specialist. As a rule, neurologists successfully deal with the problem of increased fatigue in children. Remember: fatigue is not just a whim of a child. Asthenia is a pathological condition, it indicates that something is wrong in the body.
Remember: fatigue is not just a whim of a child. Asthenia is a pathological condition, it indicates that something is wrong in the body.
- Laboratory diagnostics allows us to clarify the diagnosis, because a lot can be understood from a blood test: whether there is some kind of inflammatory process in the body or not, whether the child has hidden infections, such as herpes and cytomegalovirus, whether the thyroid gland is working normally, and so on, - explains the neurologist Dron Anastasia Nikolaevna - This is important to do, because often violations of some organs and systems are hidden under the mask of fatigue. And if this is confirmed, then we refer the patient to an additional consultation with a cardiologist, endocrinologist, immunologist, ophthalmologist, psychologist and other specialists. If not, then we prescribe drug therapy, which is aimed at improving the metabolism in nerve cells, stimulating thought processes, reducing the level of anxiety, irritability and impulsivity.