Baby solid food poop frequency
Your baby's poop - what's normal and what's not?
Bet you never thought you’d become someone that’s obsessed with poop, did ya?? Well, as a parent, this is just one of those things that we worry about and pay A LOT of attention to!
“Why’s my baby’s poop this colour?”
“My baby hasn’t pooped in days, is that normal?”
“My baby’s poop is really runny, is that diarrhea? How do I tell – it’s always liquid-like?”
These are just some of the questions I know swirl around in your head when you’re doing yet another diaper change. I know because I’ve been there!
And, while it may not be the most fun topic out there, it’s certainly an important one – so let’s go over everything you need to know about your baby’s poop!
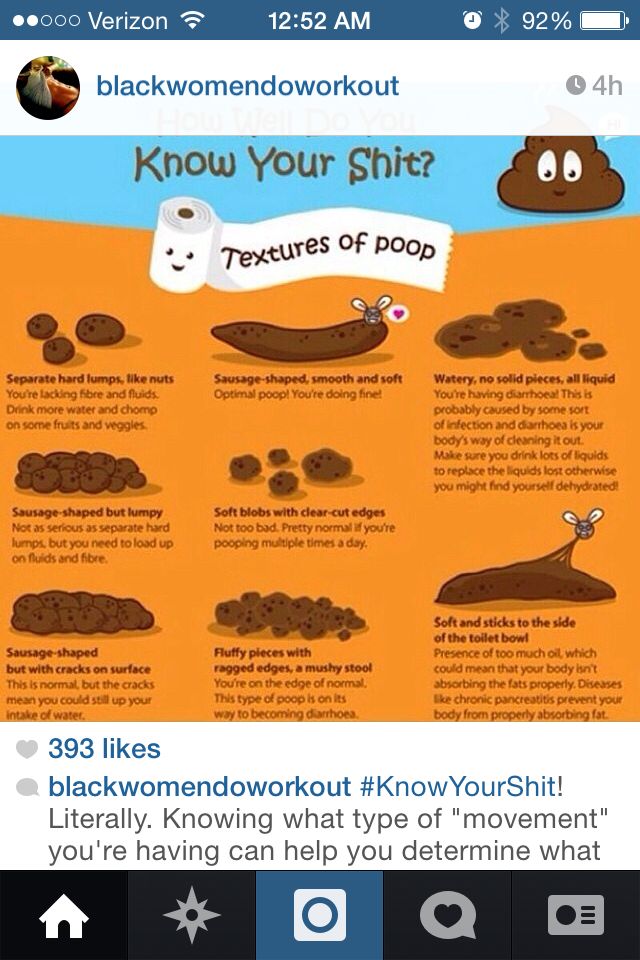
What does your baby’s poop tell us about their health?Since babies aren’t yet able to tell us how they’re feeling, we have to use certain indicators to collect information about their health and wellness – one of these is poop. We can use things such as the colour of your baby’s poop, the frequency, and the texture, to determine many different things. Including…
- Illness – sometimes your baby’s poop can be the first, or only, indicator of an illness, such as a gastrointestinal bug.
- Nutrition – certain colours can indicate issues with nutrient absorption, plus we can use the colours to tell us whether they’re taking in breastmilk/formula, and later on, if solids are being swallowed.
- Hydration – sometimes constipation can be a sign that more fluids are needed.
- Allergies/intolerances – there are certain signs to look out for that could indicate that your baby has an allergy or an intolerance to something they ate, and some of those signs show up in their diaper!
Knowing what is considered normal for your baby, based on what they’re consuming, is important so that you can determine when their poop is out of the ordinary, and then determine whether that change is to be expected, or warrants a call to their pediatrician.
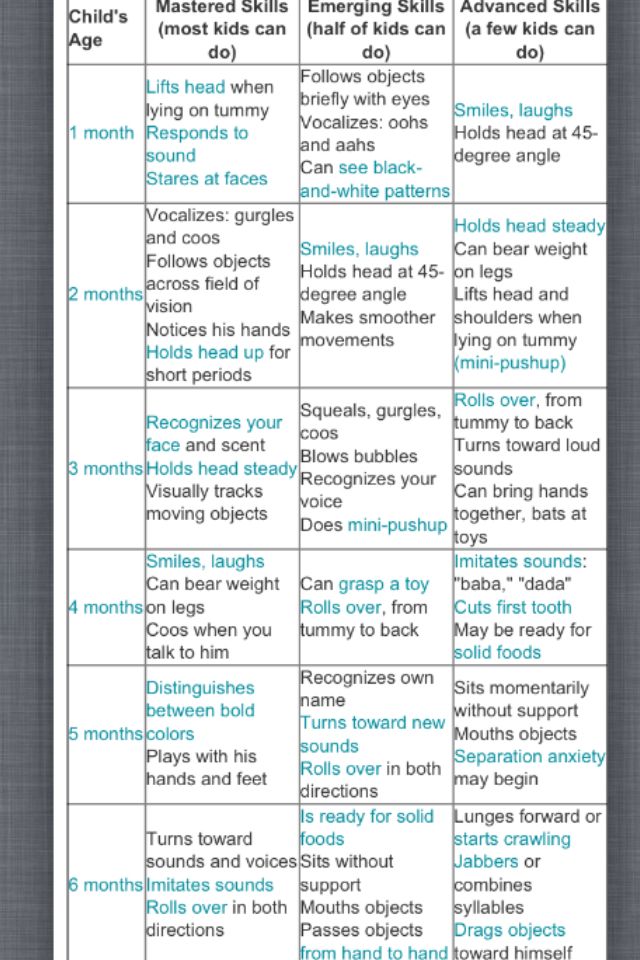
There are a lot of different factors that could affect your baby’s poop, namely age, diet, and illness. So it’s normal to expect that your baby’s poop is going to continue to change as they grow. A newborn’s poop is going to look drastically different from a 6 month old baby’s poop, which will look different from your baby’s poop at 1 year old, in large because as their diet changes, their poop changes. And diet typically changes with age. Let’s review some major changes that happen:
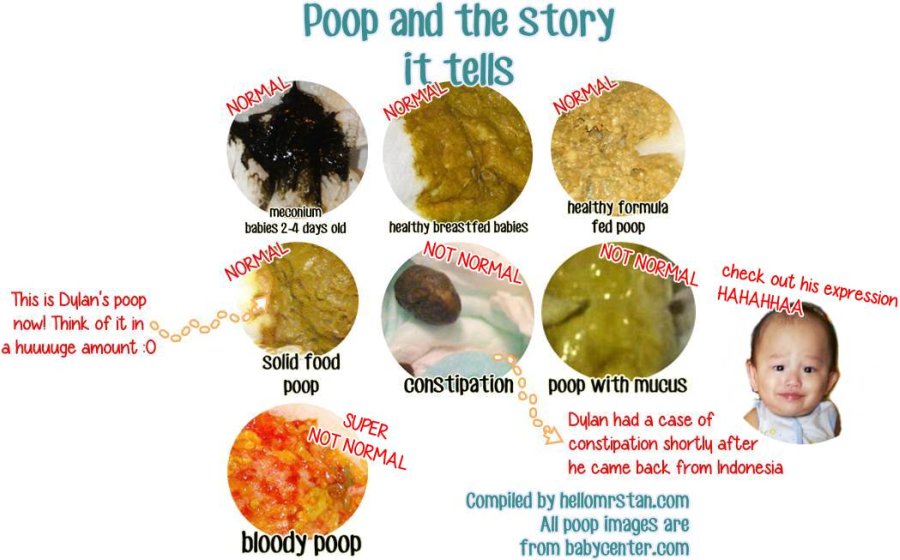
Newborn:Newborns have black, sticky, tar like poops that happen in the first 24 hours following birth. These poops are called meconium, and are basically a build up of ingested mucus, amniotic fluid, and other material from the womb. However, if they last longer than a few days, or go away and come back, you need to take your baby to their pediatrician ASAP. Black poops are not considered normal after the initial days following birth.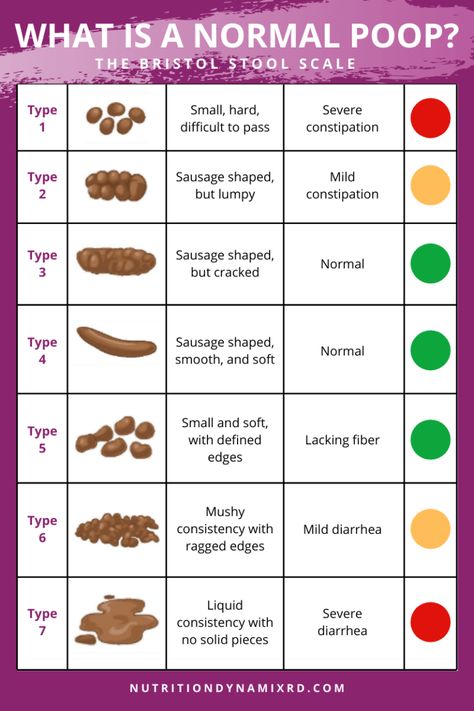
Typically, you’ll notice the meconium will change into what is referred to as “transitional poops”. These are a mixture of meconium and breastfed/formula fed poops that are expected once your baby begins to digest their milk feeds. These will continue to decrease in meconium, and change to what we expect breastfed/formula fed poops to look like, after a few days. We would expect babies to have 2 poops on day 2, and 3 poops on days 3-5. The colour will change from black, to green, to brown, and after a few more days, will change to adjust to whatever poops are characteristic of their main diet.
Breastfed baby’s poop:If your baby is being exclusively breastfed, after those first meconium poops, they’ll have poops that are clearly identifiable as breastfed baby poop.
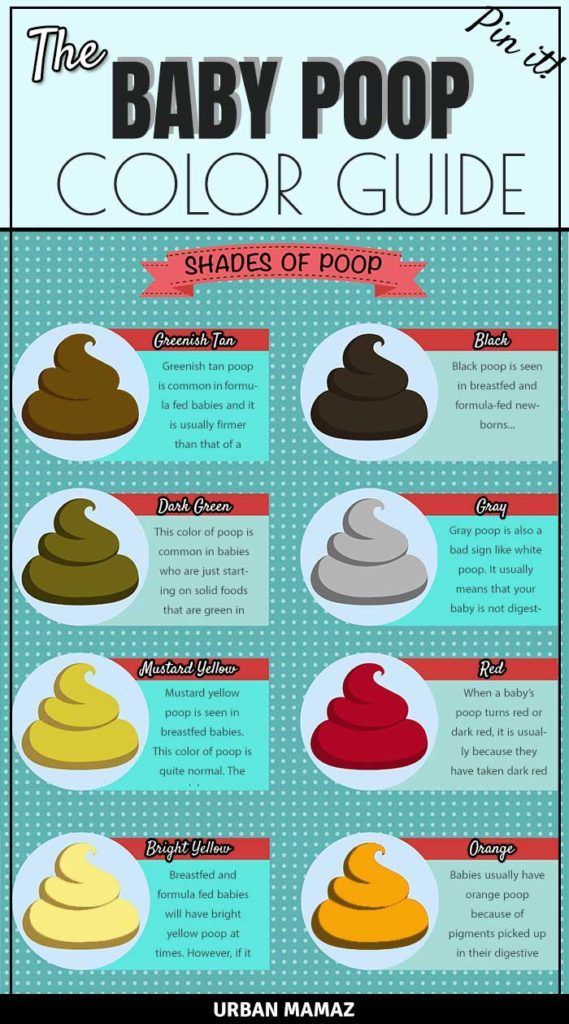
- Colour: Yellow – often bright or pale mustard coloured. Sometimes it can be bright green and frothy if babies are nursing for only short periods of time on each breast, and getting more foremilk than hindmilk.

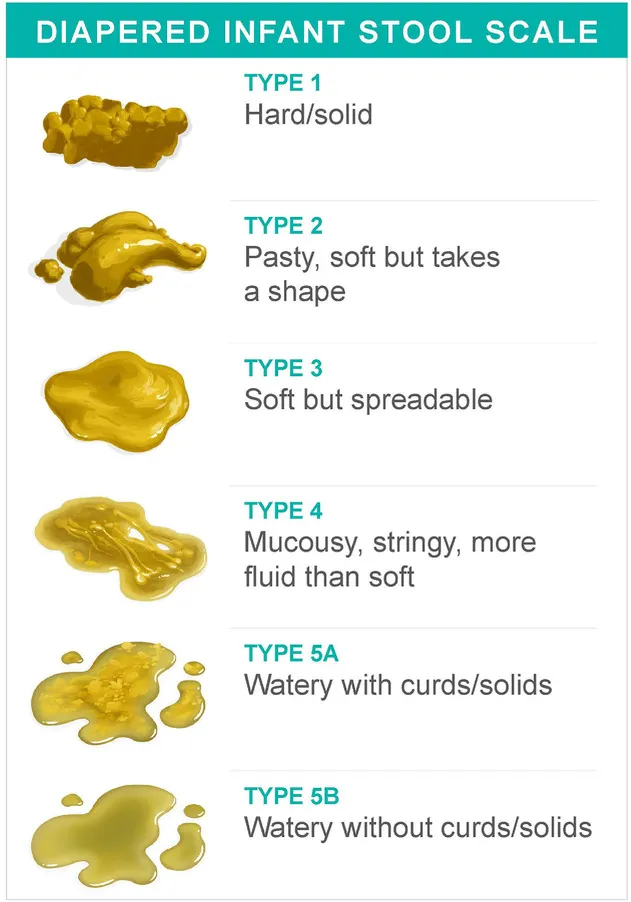
- Texture – Loose. They’ll be on the runnier side, but not like what would be considered diarrhea either. May contain seed-like or lumpy pieces – you’ll most likely notice tiny white spots or clumps within the yellow poop. This is normal.
- Frequency: Babies that are exclusively breastfed can go days without pooping, or they could poop with every single nursing session – both are considered normal.
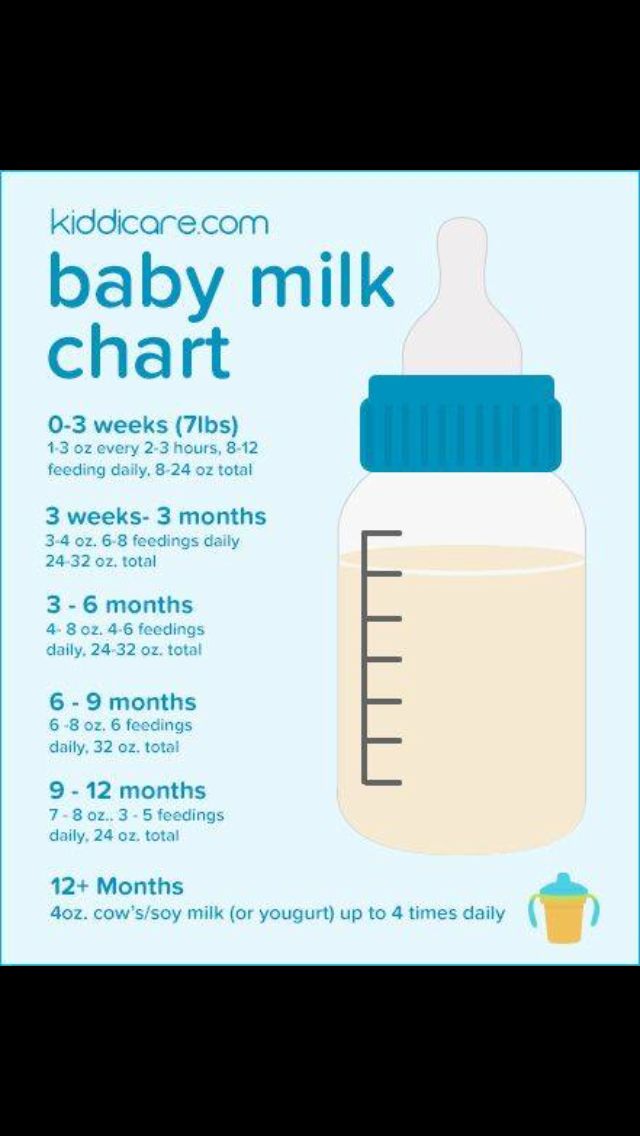
If you’re feeding your baby formula, their poops are going to look different than that of a breastfed baby. This is because formula is digested differently than breastmilk is, and it has different properties. So, if you’re exclusively formula feeding, your baby’s poops will take on the following characteristics listed below. It’s important to note that it may take 1-2 weeks after introducing formula exclusively for your baby’s diapers to change.
- Colour: Yellow-brown, green-tan, or brown.
 With formula there’s a bit more of a range as far as the colour of poops, but any of these colours are considered normal.
With formula there’s a bit more of a range as far as the colour of poops, but any of these colours are considered normal. - Texture: Thick and firm – typically it has a consistency similar to toothpaste, which is thicker than the poop of a breastfed baby.
- Frequency: Formula-fed babies don’t typically poop after each feed (as is common for some breastfed babies) because formula takes longer to process through the digestive tract. However, they should be going at least once per day, maybe even every other day. Anything less than that could be a sign of constipation. I’ll explain more about the other signs in a little bit, but this would warrant a call to their pediatrician.
Some babies are given both breastmilk and formula throughout the day, which is referred to as combination feeding. In these cases, your baby’s poop could vary and be seen as anything between the two types described above.
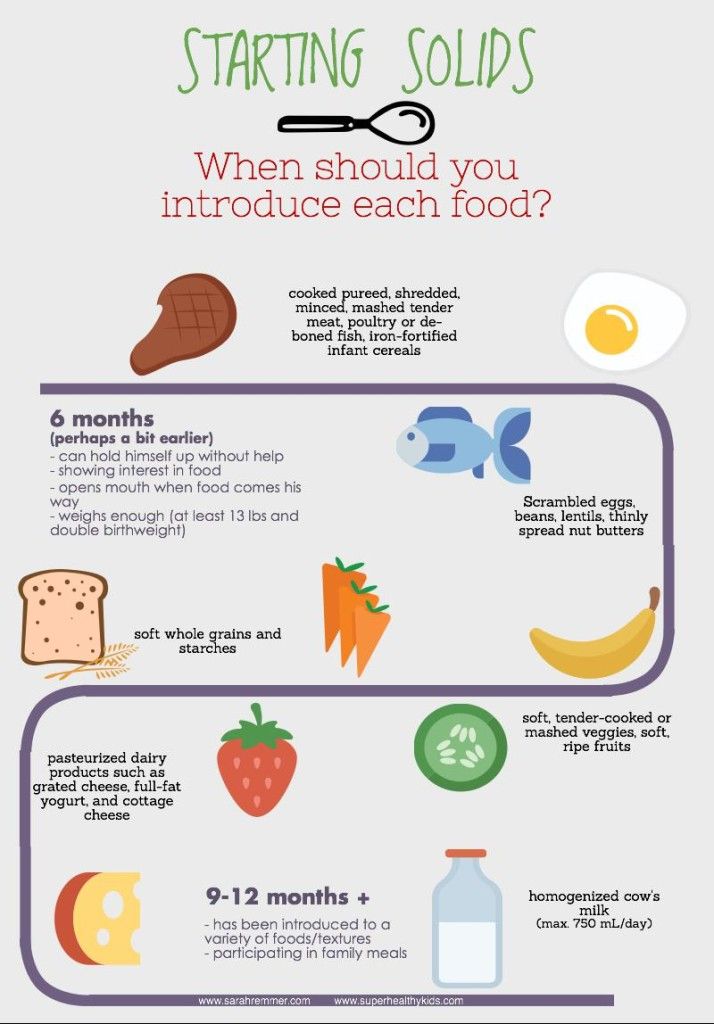
Once you begin feeding your baby solids, typically around the 6 month mark and once they’ve shown all the signs of readiness, your baby’s poop will change due to their new diet. After all, what goes in, must come out! However, I want to note that this doesn’t mean that your baby’s poop will begin to look like adult poop – their poop will continue to have certain characteristics that make it very clearly baby poop. Here are the main things to look for in normal poop.
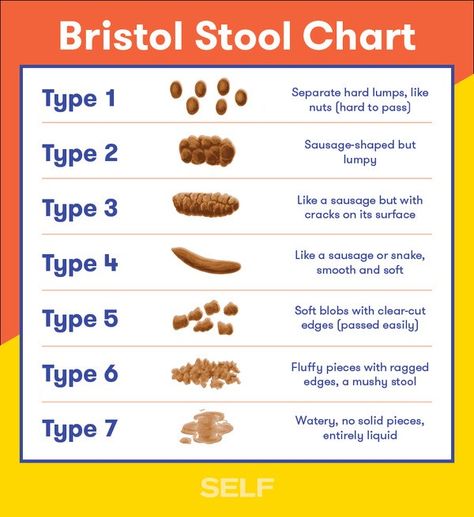
- Texture: If your baby was exclusively breastfed, you’re probably familiar with the more loose stools they were used to having (note: not diarrhea, but loose for sure). Once your baby starts solid foods, you’ll see a pretty significant change in stool texture – namely, they’ll get way firmer. This might not be as obvious if your baby was exclusively formula fed before, but generally, we want the texture of their poop to be like the texture of a cooked sweet potato – sort of pasty.

You might also notice bits of undigested food in your baby’s diaper. Is this a concern? No, it’s actually completely normal! See, your baby’s digestive tract is much shorter than an adult’s, and therefore there isn’t always enough time for their body to break down all of the food that they’re eating. This is especially true for foods higher in fibre, such as corn, carrots, blueberries, etc. It also can happen if your baby isn’t chewing their food a lot before swallowing, which is to be expected when they’re first starting out with solids. But hey, it’s a great indicator that they’ve actually ingested some food!
- Smell: Solid food produces smellier poop. Babies on a milk only diet usually have milder smelling poop, especially when it’s breastmilk only.
- Colour: Before starting solids, your baby’s poop colour was likely fairly consistent. A mustard colour if they were exclusively breastfed, a brownish colour if they were formula fed, and somewhere in between if they were…well…somewhere in between those two.
 Once your baby starts solids, you’ll see that it’s likely your baby’s poop will take on a broader variation in colour, and may even take on the colour of the latest coloured food they ate!Here are some examples of normal colour changes you might notice:
Once your baby starts solids, you’ll see that it’s likely your baby’s poop will take on a broader variation in colour, and may even take on the colour of the latest coloured food they ate!Here are some examples of normal colour changes you might notice:
Brown – this is kind of the standard colour, and happens naturally when they begin eating solids.
Dark green – common when starting solids that are green in colour, like spinach or peas. This can also happen if your baby is taking iron supplements, or eating a lot of iron rich foods (as is recommended for babies).
Blue – this sounds concerning but is a result of eating foods of this colour. One main culprit for producing this colour of poop is blueberries!
Orange – again, this could be from eating foods of this colour. Remember that baby’s digestive tracts are shorter, with less time to digest the food in its entirety, so it is easier to tell what they ate by looking at their poops. In babies that haven’t started solids, this can also happen because the poop absorbs pigments from the digestive tract, which is also considered normal.
Red – you may notice a deep red colour if they ate something of that colour recently, for example beets (I will say, from experience, it can look like a deep red, almost maroon colour!)
- Frequency: Once you go from an all liquid diet to introducing solids, you’re usually going to see the frequency of bowel movements go down. This is because solids bulk the stool up, there is usually less fluid being taken in, and sometimes it can take a while for a baby’s digestive system to adjust.
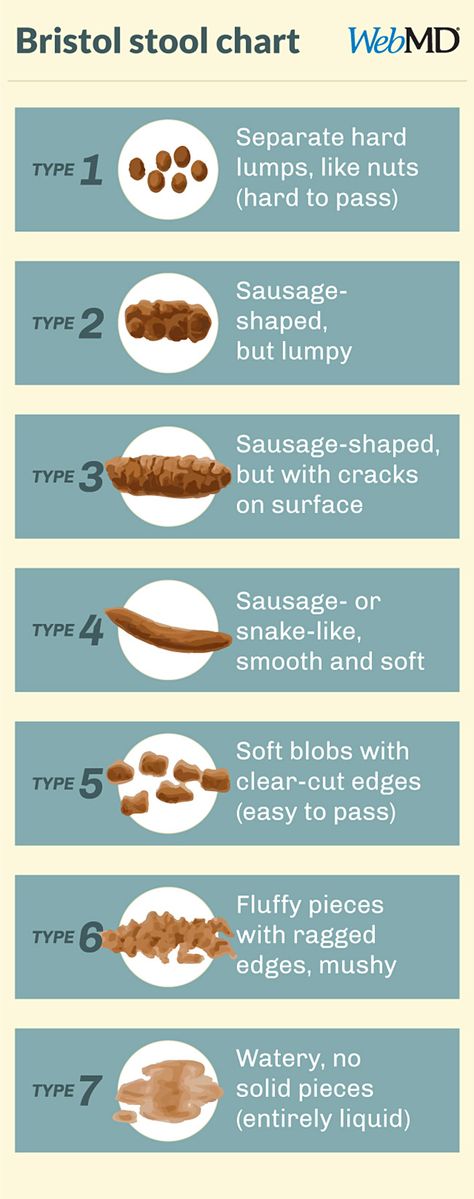
Diarrhea can happen when your baby is sick with a virus, bacteria, or perhaps taking antibiotics.
The key change in stools you’ll see is in the consistency – watery, loose and possibly mucousy – and the frequency – 3 or more of these watery, loose stools in a row.
I know your baby’s poop is naturally liquidy if they’re exclusively breastfed, and so it may seem difficult to distinguish diarrhea from their normal.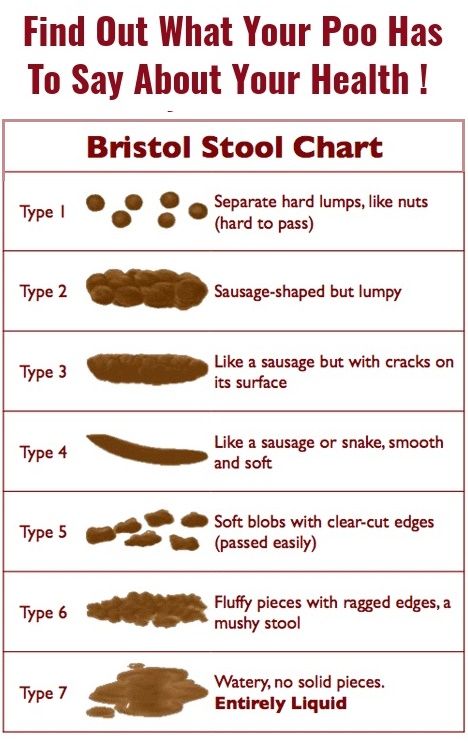 But that’s why we need to observe their normal, because I’m telling you, you’ll know diarrhea! I’ve changed a diaper that was best described as coloured water, it pooled in their diaper and the diaper couldn’t even soak all of it up fast enough, so when I opened it, there was a literal puddle (not a pleasant image I know!). It may not be that drastic, but a watery poop explosion up your baby’s back, is another good sign. Basically, my point is, that you’ll know, you’ll open the diaper and say: “Uh-oh, that’s not normal!”, and if you find yourself doing this, don’t second guess, your instinct is probably right!
But that’s why we need to observe their normal, because I’m telling you, you’ll know diarrhea! I’ve changed a diaper that was best described as coloured water, it pooled in their diaper and the diaper couldn’t even soak all of it up fast enough, so when I opened it, there was a literal puddle (not a pleasant image I know!). It may not be that drastic, but a watery poop explosion up your baby’s back, is another good sign. Basically, my point is, that you’ll know, you’ll open the diaper and say: “Uh-oh, that’s not normal!”, and if you find yourself doing this, don’t second guess, your instinct is probably right!
If your baby is experiencing diarrhea, it’s not necessarily an emergency, but your main goal is going to be to keep them hydrated! You need to ensure that they’re drinking enough formula/breastmilk. If they’re older and eating solids, try to serve foods with a high water content, such as watermelon, or cucumbers, along with encouraging them to drink water from an open cup with meals.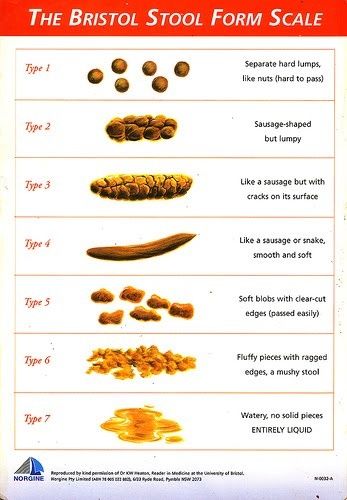
If your baby is also experiencing fever, irritability, or appears to be in pain, seek medical attention right away. Babies can dehydrate much faster than adults do, and it’s best to get them seen at the onset of these symptoms.
Also watch for other signs of dehydration, particularly if the diarrhea is ongoing and lasts for several days. The other signs you need to look for are:
- Decreased tears or crying without tears
- Lack of saliva
- Sunken eyes
- Sunken fontanel (soft spot on your baby’s head)
- Excessive fatigue
- Less playful than usual
Finally, if diarrhea is recurring, it can also be a sign of a food allergy (most likely cow’s milk allergy or lactose intolerance), so be sure to speak with your doctor if you suspect that.
ConstipationConstipation is not simply a reduction in the amount of dirty diapers. The more important factors to look at to see if your baby is constipated is if they have…
- Extremely hard and difficult to pass poop
- Poop that appears pebble-like and is in small pellets or marbles
- Poop that is a thicker consistency than toothpaste (specifically for younger infants)
- Pain when pooping
Note: a red face while pooping is not a sign of constipation in young infants. They simply haven’t learned how to activate the correct muscles to push their poop out, and as they get closer to 1 year old, you’ll notice this won’t happen as often, if at all.
They simply haven’t learned how to activate the correct muscles to push their poop out, and as they get closer to 1 year old, you’ll notice this won’t happen as often, if at all.
Constipation can happen when your baby is dehydrated and isn’t taking in enough fluids, or isn’t getting in enough of the right types of fiber, or has an imbalance in gut bacteria. You can learn more about my strategies for managing constipation here. And if you’re unsure about what types of food to serve your baby, and how to safely introduce solids and finger foods – my Baby Led Feeding course is for you!
When to seek helpHere’s the thing, poop is going to vary with each baby, and you are going to notice changes in consistency, frequency, and colour fairly frequently, especially as their diet changes with introducing solids. The key to remember is that their poop should be soft, your baby should be gaining weight and eating well, but frequency will vary with each child.
However, there are certain times when I want you to seek help from your pediatrician right away. If you notice…
If you notice…
Generally, we don’t want to see red in your baby’s diaper as this indicates bleeding of some sort, somewhere along the digestive tract. Bright red blood in the diaper typically indicates some bleeding somewhere closer to the end of the tract. It could be an infection, an anal fissure from excessive pushing due to constipation, a milk allergy, or sometimes flecks of red appear in a breastfed baby’s diaper if their mom has cracked, bleeding nipples. And once a baby begins solids, it may happen from ingesting certain red-coloured foods. However, we really want to err on the side of caution with red poop. So if you cannot say with 100% certainty that your baby’s poop has a red tinge due to eating a lot of beets, it’s best to call their doctor and discuss it. They may have you wait to see if the next poop is the same colour, or they may want to check it out right away. Dark red and black poops indicate a very serious problem – specifically internal bleeding, as this is digested blood. So, if the poop is at all borderline, as in you’re having a difficult time deciding if it’s the colour of beets or a dark red/black colour, it’s absolutely best to get your baby checked out, just in case.
So, if the poop is at all borderline, as in you’re having a difficult time deciding if it’s the colour of beets or a dark red/black colour, it’s absolutely best to get your baby checked out, just in case.
These colours can happen, and they may have a chalky texture as well. White indicates that there is an issue with your baby’s liver, and basically there isn’t enough bile being produced to properly digest food. It needs to be addressed immediately. Gray could also indicate an issue with the liver in that food isn’t being digested properly, or it could also mean that your baby’s body isn’t absorbing the nutrients in their food. Again, it needs to be addressed right away.
MucusAlthough some mucus can be normal, consistently having mucusy poop can also be a sign of an allergy or an infection, so again, if you’re unsure of the cause, it’s best to speak with your baby’s doctor.
Dramatic changes after introducing solidsIf you notice any drastic changes after introducing solids to your baby, either with regards to consistency, frequency, pain, etc.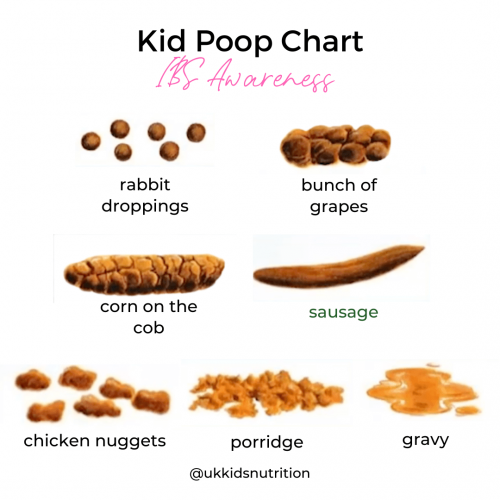 speak with your baby’s pediatrician. This can indicate a possible food allergy and should be addressed before offering that food again.
speak with your baby’s pediatrician. This can indicate a possible food allergy and should be addressed before offering that food again.
If your baby’s poops continue to be runny and liquid-like leading up to their first birthday (not diarrhea), be sure to discuss this with your baby’s pediatrician. By this age, their diet should consist of mainly solid foods, and therefore, their poops will reflect that and should have a thicker consistency than when they were on a liquid diet of breastmilk or formula.
I know that was a lot of info about poop, so I hope you were able to stick with me, because this is really an important topic. Taking notice of your baby’s normal, when it comes to so many things, is crucial in being able to recognize and react when something happens that’s outside of their normal. Poop is no exception.
If you’re feeling stressed about all the information you need to process and retain regarding starting solids with your baby, I have a solution! My Baby Led Feeding course is the most comprehensive online course on feeding out there, and provides you with step-by-step guidance into this new world of serving solids and finger foods to your baby.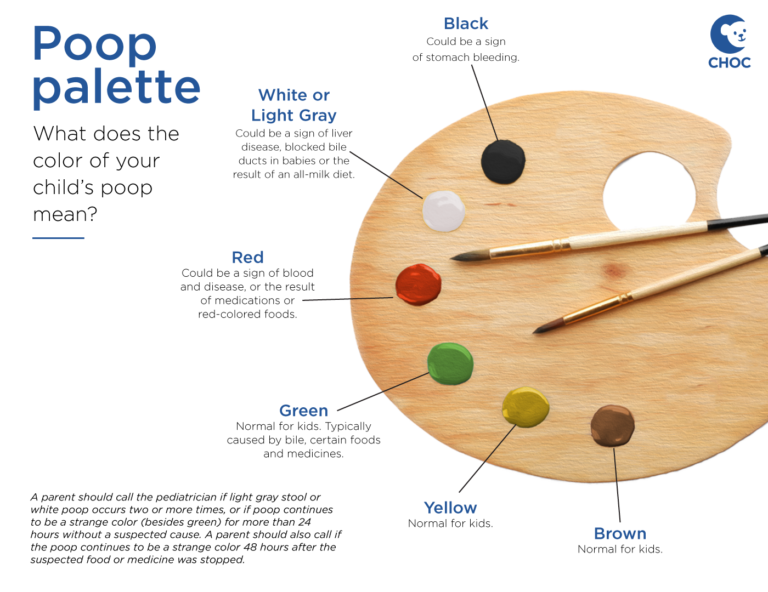 Plus, you have access to it for a lifetime! Check back in whenever you need a question answered or a refresher on a specific topic, and never feel like you need to search the depths of the internet to find a trusted answer. Enroll today!
Plus, you have access to it for a lifetime! Check back in whenever you need a question answered or a refresher on a specific topic, and never feel like you need to search the depths of the internet to find a trusted answer. Enroll today!
How Your Baby's Poop Changes After Starting Solids
Home / baby-solid-foods-complications / How Your Baby’s Poop Changes After Starting Solids
by Emily DeJeu in baby-solid-foods-complications, baby-solid-foods-reactions —
Starting solids is a big step for your baby — he’s learning a whole new way of eating, after all! All those new foods affect his every aspect of his digestion, including what ends up in his diapers.
That’s right — we’re talking poop today!
Starting Solids? The Poop Changes!Before you start your baby on solid foods, it’s best to prepare yourself in advance for the fact that starting solids will probably affect your baby’s poop.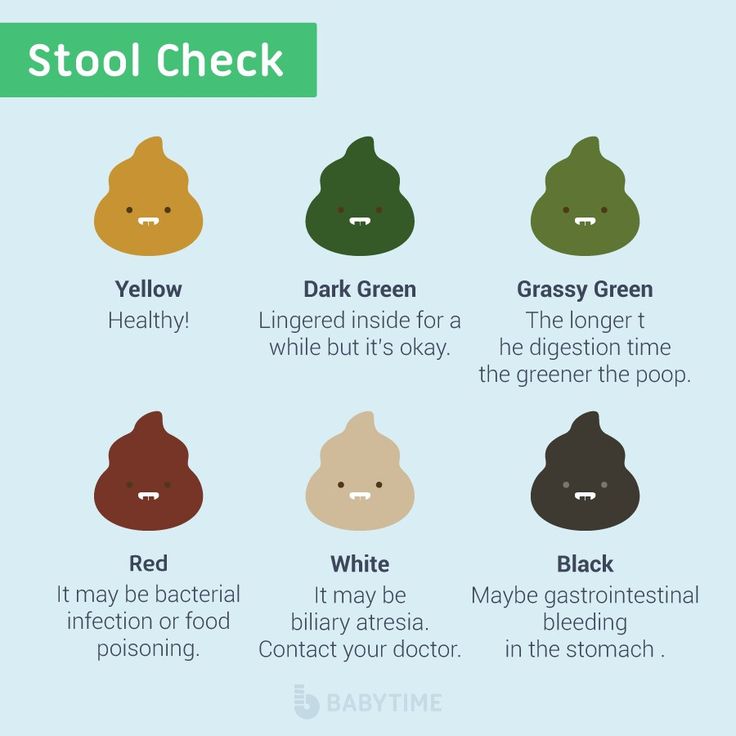 The poop will smell worse. The poop may be brightly colored. The poop may appear many times a day. Or, the poop may stop coming altogether.
The poop will smell worse. The poop may be brightly colored. The poop may appear many times a day. Or, the poop may stop coming altogether.
We repeat — the poop changes.
6 Ways Your Baby’s Poop May Change After Starting Solids- The poop will smell even worse.
Now, poop never smells great. There’s a reason you won’t find any poop-scented perfumes on the market! But up until the time you start your baby on solids (and this is especially true if baby has been exclusively breastfeeding), the poop probably didn’t stink to high heaven.
Once you start your baby on solids, though, that’s going to change. Solid food produces smellier poop, and as your baby eats more and more solid food, the poop will only get stinkier. There’s no way around it. Just plan on doing lots of mouth-breathing during diaper changes. 😉
- The poop may be colorful.
Before starting solids, your baby’s poop was probably a consistent yellowish-brown color.
 Nice and predictable. After starting solids, though, that’ll likely change. Feed your baby plenty of tasty spinach for lunch, and you may very well see green poop at bedtime. Offer a big bowl of yummy steamed carrots for dinner, and you might wake up to a diaper full of bright orange poop the next morning.
Nice and predictable. After starting solids, though, that’ll likely change. Feed your baby plenty of tasty spinach for lunch, and you may very well see green poop at bedtime. Offer a big bowl of yummy steamed carrots for dinner, and you might wake up to a diaper full of bright orange poop the next morning.This is nothing to be worried about; brightly-colored poop is normal at this stage. Your baby’s digestive system is still fairly immature and is learning how to process solid foods; as she grows, her poop will change to a more normal color, regardless of what she eats.
- The poop may get firmer.
If your baby’s been on formula, this one may not apply. But if your baby’s been breastfeeding up to this point, you may discover that after starting solids, his poop is firmer and more “shaped”. Breastfed babies typically have runny, liquid-y poop; once they start solids, however, it becomes firmer, more like paste.
- The “poop” may look a lot like undigested food.
This isn’t an issue when you’re feeding your baby smooth purees, but once you start adding some chopped table food into the mix, look out!
I remember taking my oldest son, when he was just 9 months old, to a dinner buffet. I loaded up a little plate with all kinds of vegetables and felt so proud when my son gobbled them up. The next morning, however, I was a little shocked — the contents of his diaper looked almost exactly like the contents of his plate the night before. The poop didn’t look like like poop at all — it looked like food!
Turns out I didn’t need to be worried; again, this is just a sign that my son’s digestive system was figuring out how to handle pieces of table food. Over time, as he ate more and more chopped table food, his poop returned to normal.
- The poop may start appearing more often.
By the time you’re ready to start your baby on solid foods, it’s likely that he’s pooping pretty normally (as in once or twice a day).
 In fact, if he’s being breastfeed exclusively, he may be going a few days in between bowel movements. That’s considered very normal for breastfed babies. And how nice for you, right? Poop-free diapers are so much easier to change. 🙂
In fact, if he’s being breastfeed exclusively, he may be going a few days in between bowel movements. That’s considered very normal for breastfed babies. And how nice for you, right? Poop-free diapers are so much easier to change. 🙂But once you start your baby on solid foods, that may come to an end. For some babies, starting solids means pooping more frequently. We can chalk this up (again) to their immature little digestive systems. As your baby’s systems figure out how to process solid food more efficiently, you’ll find that he returns to more normal amounts of pooping (thank goodness!)
Note: Diarrhea can be a sign of a food allergy or sensitivity. If you suspect that your baby’s frequent pooping is actually diarrhea, talk to a healthcare provider about possible food allergies and sensitivities.
- The poop may disappear altogether.
Some babies poop WAY more after starting solids. Other babies, though, have the opposite problem: constipation.
 Constipation often occurs when you offer your baby lots of “binding” foods, like bananas and rice.
Constipation often occurs when you offer your baby lots of “binding” foods, like bananas and rice.For more information on the signs and symptoms of constipation, as well as ways to alleviate constipation naturally, check out our post on “How to Handle Your Baby’s Constipation.”
What if you could find everything you needed to know about starting your baby on solid foods – when it’s best to start solids, how to introduce solids, complications, food allergies, etc. – in one easy-reference guide? Now you can! Your Baby’s Start To Solid Foods: A Comprehensive Guide will walk you through every step of starting solids. Plus, your e-Book package includes several bonus materials, designed to maximize your success in starting solids. You’ll get a thorough guide to treating constipation, a dietitian’s advice on how to avoid 5 common solid-foods mistakes, and a weekly meal plan for your baby’s first year. Grab your e-Book today, and ensure your baby has the healthiest possible start to solid foods!
Grab your e-Book today, and ensure your baby has the healthiest possible start to solid foods!
The Baby Sleep Site® is a participant in the Amazon Services LLC Associates Program and other product affiliate programs. If you click on a product link and make a purchase, The Baby Sleep Site® may (but not always) receive a small commission from the company selling the product, but will not affect your purchase price. We only recommend products that we believe are quality products and are good for our readers.
Need Baby and Toddler Sleep Help? We Have the Resources You Need!If you are tired of wading through stacks of baby sleep books that just aren't working, if you are beyond exhausted and just can't solve your child's sleep problems on your own...then personalized sleep consulting is for you. We have been around since 2008 and invite you to tap into our MANY years of experience.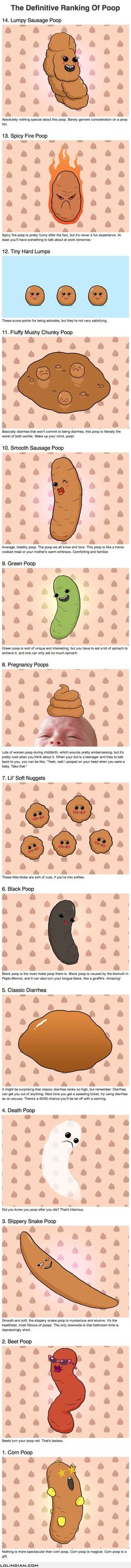 Our team of expert consultants will create a Personalized Sleep Plan® just for your family and then support you through every step of implementing your plan. We encourage you to consider our personalized, one-on-one baby and toddler sleep consultation packages if you want to see real, meaningful results now. Your consultation package also includes ample follow-up help, designed to help you troubleshoot problems and tweak your plan as needed.
Our team of expert consultants will create a Personalized Sleep Plan® just for your family and then support you through every step of implementing your plan. We encourage you to consider our personalized, one-on-one baby and toddler sleep consultation packages if you want to see real, meaningful results now. Your consultation package also includes ample follow-up help, designed to help you troubleshoot problems and tweak your plan as needed.
Learn More About Services
For those persistent nighttime struggles, check out The 3 Step System to Help Your Baby Sleep. Using the same unique approach and practical tools for success, this e-book helps you and your baby sleep through the night.
Learn More About The 3-Step System
If you’re looking for ways to get your baby or toddler into a healthy sleeping routine during the day, explore Mastering Naps and Schedules, a comprehensive guide to napping routines, nap transitions, and all the other important “how-tos” of good baby sleep.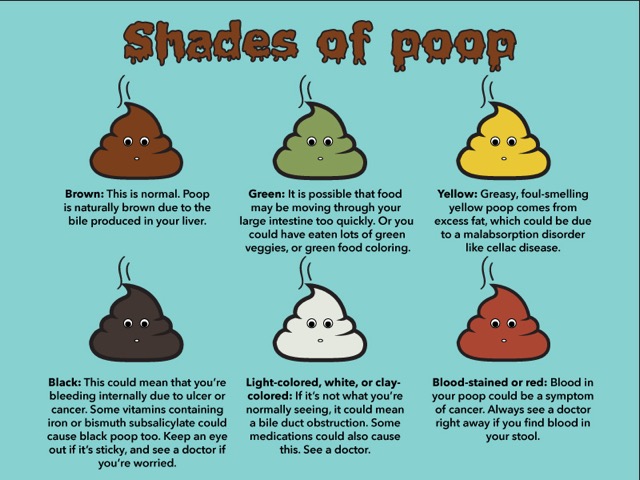 With over 45 sample sleep schedules and worksheets, Mastering Naps and Schedules is a hands-on tool ideal for any parenting style.
With over 45 sample sleep schedules and worksheets, Mastering Naps and Schedules is a hands-on tool ideal for any parenting style.
Learn More About Mastering Naps
For those persistent toddler sleep struggles, check out The 5 Step System to Help Your Toddler Sleep. Using the same unique approach and practical tools for success, this e-book helps you and your toddler sleep through the night and enjoy a better daytime schedule.
Learn More About The 5-Step System
Join our VIP Members Area packed with exclusive content and resources: e-Books, assessments, detailed case studies, expert advice, and more. As a VIP member, you'll also enjoy a weekly chat with an expert sleep consultant.
Learn More About VIP Membership
In over 10 years, we have over 10,000 comments on our blog.
At this time, we’ve turned the comment sections off.
We would, of course, love to hear from you! For help with your specific sleep problems, please learn more about our DIY resources or our sleep consultation services. Or, consider emailing us for a fast and helpful response!
Diarrhea in a child causes, effects and methods of treatment of diarrhea
Diarrhea is an increase and change in the consistency of the stool.
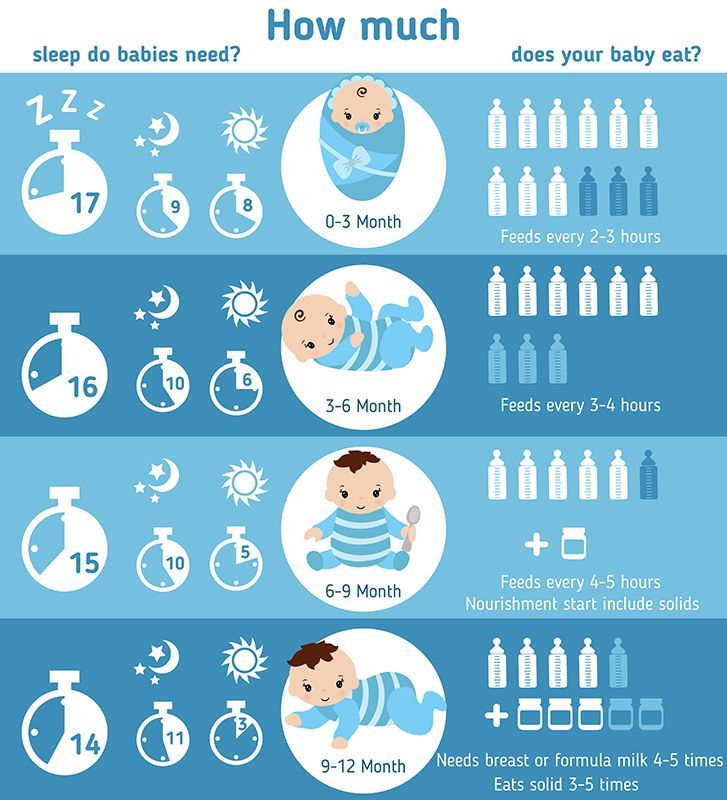
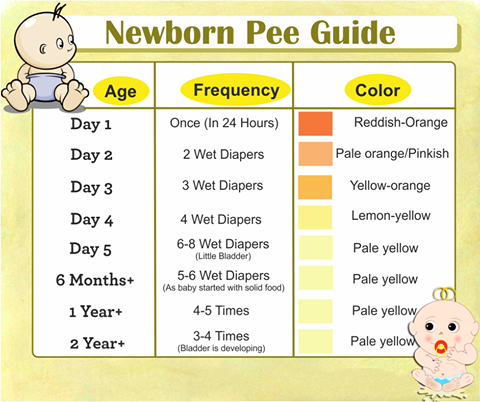
The frequency and nature of the stool varies depending on the age of the child, the type of feeding (breast milk, mixed, artificial) and the individual characteristics of the child (Table 1).
Therefore, during the first six months (before the introduction of complementary foods), the baby's stools with breast milk are usually homogeneous, thick, yellowish, up to 5-7 times a day. This is fine. The frequency increases to 10 or more times and the stool is completely absorbed into the diaper - a symptom of diarrhea.
The introduction of mixed and complementary foods reduces the frequency of stools, increases its density, changes color and smell.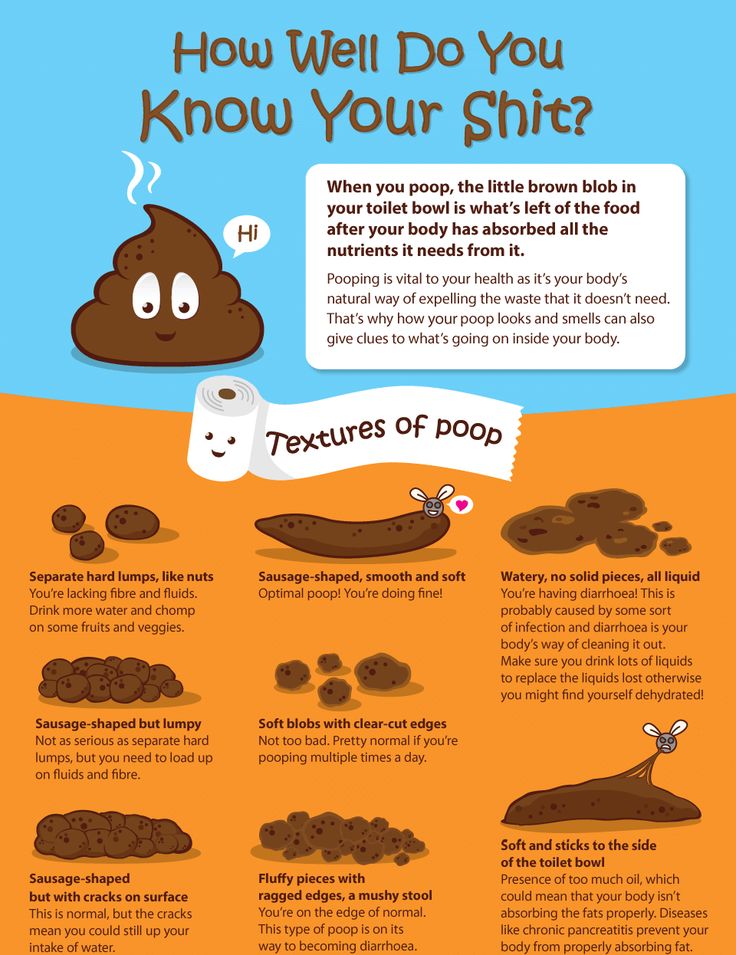 Wet or watery stools 3 or more times a day is a sign of diarrhea.
Wet or watery stools 3 or more times a day is a sign of diarrhea.
ears. 1. Number of stools in infants
Number of flights per week
Number of flights per day (average)
6 to 12 months
4 years and older
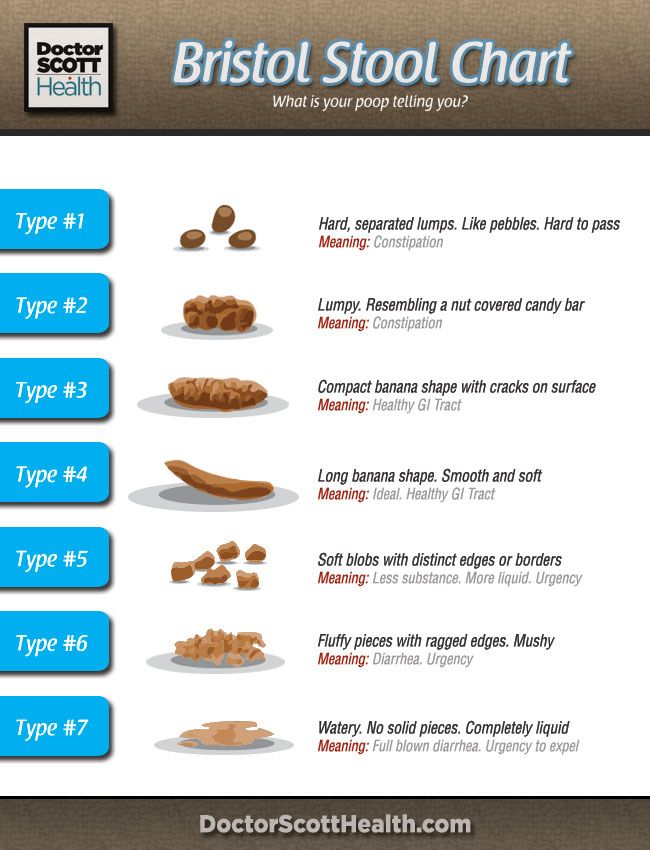
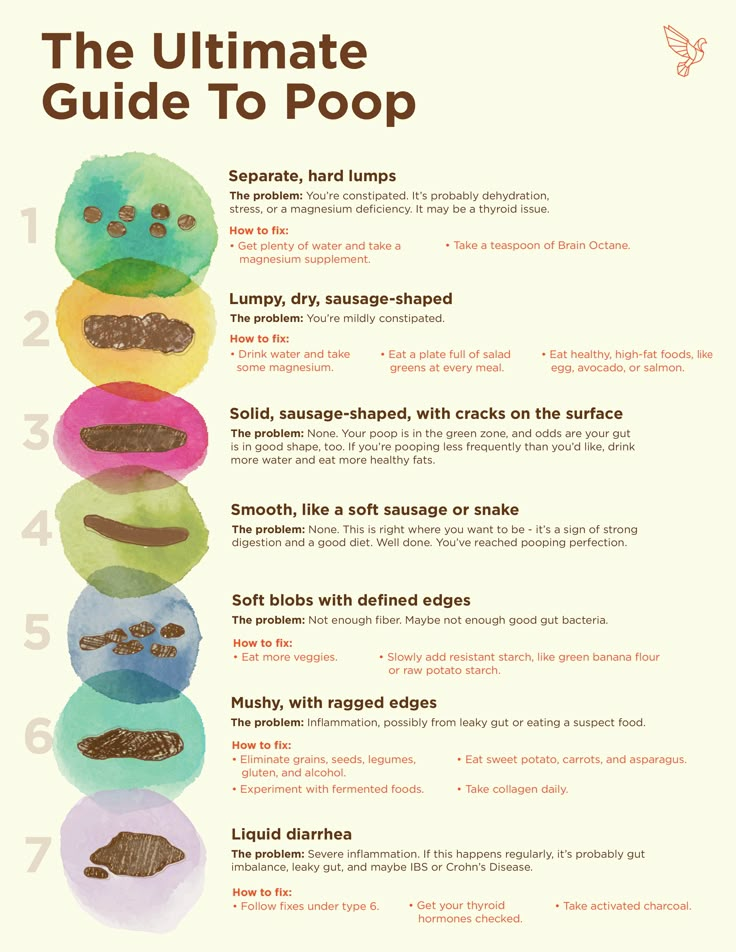
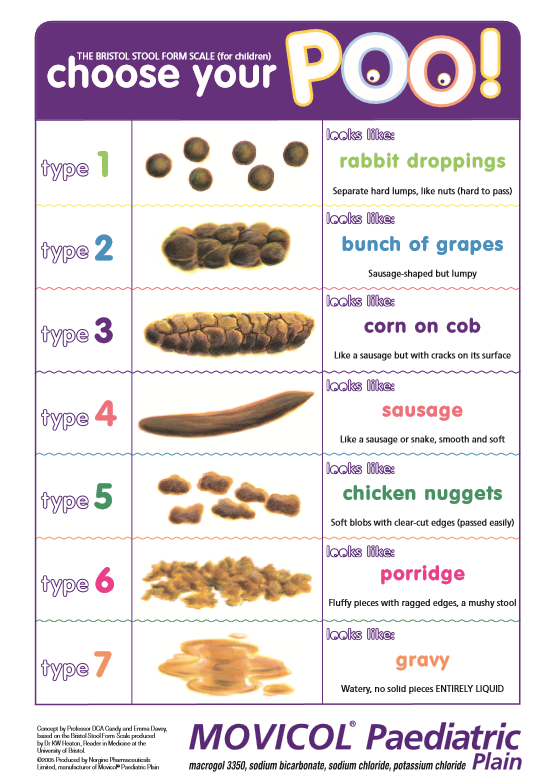
Bristol stool scale 5-7, stool type is a symptom diarrhea and indicates an increase in the rate of gastrointestinal transit of the esophagus.
What can cause diarrhea in babies?
There are two main causes: infectious and non-infectious.
Viruses, bacteria, fungi and protozoa can cause infectious diarrhea.
Food allergies (FMA), food intolerance (lactose), antibiotics, pancreatic disease, and congenital diseases can cause non-infectious diarrhea.
Why is diarrhea dangerous?
Acute watery diarrhea is accompanied by massive fluid and electrolyte losses. As a result, this leads to the development of dehydration. His symptoms are shown in Table 2.
ears. 2. Dehydration scale
general condition
eyeball
mucous membrane
grinder
The degree of dehydration is calculated by summing the frequency.
mild dehydration
alarms
- vomiting
- (Temperature rise)
- bloody stools, vomiting
- Gekibutori
- lethargy
- serious illness
- Violation of spatial perception
Adverse consequences (complications)
- hysteria
- disturbance of consciousness
- onset of acidosis
- so often
What should I do if my baby has diarrhea?
Non-drug treatment consists of three points.
- Water and electrolyte recovery
- dietary supplement
- Proven Efficacy Probiotics
Usually a dry powder for making mortar.
The diet aims to reduce the load on the digestive system. This is especially true of milk sugar (lactose) and milk protein. Therefore, products containing animal milk (cow, goat, mare, etc.) should be (temporarily) excluded.
Continue breastfeeding. In consultation with the pediatrician, lactase enzyme preparations can be used to reduce the risk of developing lactase deficiency.
It is advisable to replace the usual mixture with a lactose-free one, for example, Nutrilak Premium is lactose-free, but not completely, but partially (from 1/3 to 1/2 of the main amount). According to the doctor's prescription, a complete transition to the therapeutic mixture in the acute phase is possible.
The use of lactose-free and lactose-free CMP Deep Hydrolyzed Peptides MCT or Nutrilac Premium Soy Blend is justified in the presence of symptoms of allergy to cow's milk proteins.
Contains probiotics Lactobacillus rhamnosus (LGG)® and Saccharomyces blardi.
These two microbes alone are particularly effective against infections and diarrhea associated with antibiotics. Young people can only use it at the beginning. This is especially helpful if your baby food is rich in probiotics. Therefore, there is no need to take it separately after calculating the time, frequency and cost, saving time.
Highlights
In case of prolonged (more than 2 weeks) and recurrent diarrhea, a specialist should be consulted to exclude genetic or chronic diseases of the gastrointestinal tract.
recovery
Enteritis can have a serious effect on the child's gastrointestinal tract, so suddenly return to normal nutrition or stop taking lactase without doctor's permission just because the stool is normal, NG.
When preparing food, eat grains (cereals, pasta) and meat first. Vegetables and fruits are preferably subjected to heat treatment. It is better to exclude or replace dairy products with acidic ones - they contain nico-probiotics and their metabolites, which have a positive effect on the digestive tract. For children under 1 year of age, traditional milk milk can be partially or completely replaced with the exclusive Nutrilac Premium milk. This helps to facilitate the process of digestion, normalize stools and maintain microbial balance.
Prevention measures
Antibiotic travelers' diarrhea and stool imbalance are easier to prevent than to treat.
Studies have shown that taking L. rhamnosus (LGG)® significantly reduces the risk of diarrhea after leaving the house or taking antibiotics.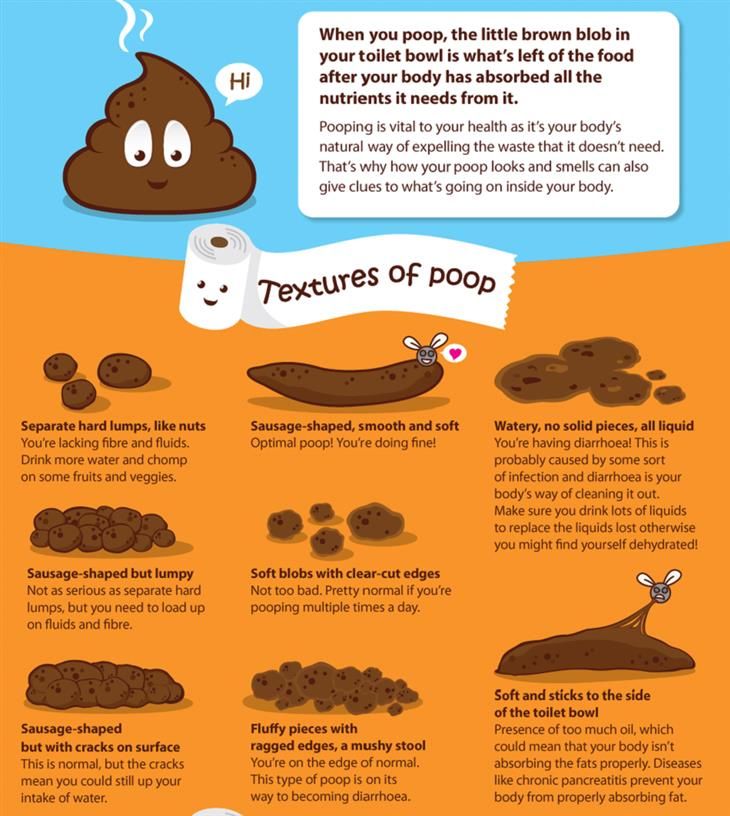 There are nutritional supplements for adults and probiotics for children.
There are nutritional supplements for adults and probiotics for children.
Editor, medical expert - Khartyunyan Mariam Khartyunovna.
Viewed 692 times 306 times
Last updated: May 25, 2022
Average reading time: 10 minutes
Small amounts of mucus always present during bowel movements8 - usually produced in the inner lining of the colon1 However, mucus-rich compartments, especially when associated with diarrhea in children, usually indicate pathology 2. Parents may notice membranes, flakes, lumps, and sometimes hard lumps or tubes on the surface of the stool8.
This should be a reminder to parents. About diseases in which mucous diarrhea develops and what parents need to do in this case, read the article.
Causes
Diarrhea with mucus is a symptom of damage to the digestive system. Excessive secretion of mucus is characteristic of a disease of the colon (colitis). This is due to the fact that the walls of the colon contain much more beautiful cells responsible for the secretion of mucus 1 .
The causes of mucous diarrhea in children can be divided into two categories: infectious and non-infectious.
due to infection
Intestinal infection lasts 1-3 weeks 2. Infectious diseases include viruses, bacteria and pathogenic fungi that penetrate the intestinal mucosa and cause diarrhea. toxic to the body. Parasites can cause allergies and maintain persistent inflammation in the digestive tract9.
Diarrhea is classified according to the mechanism of occurrence as follows.
- excrement. The cause of productive diarrhea is enteritis, primarily a viral lesion of the wall of the small intestine. Under such conditions, the stool becomes watery and watery14.
- Invasive diarrhea Invasive involves damage to the colon by pathogenic bacteria such as Salmonella, Shigella and Escherichia. It penetrates the intestinal wall and causes active inflammation, i.e. colitis leading to diarrhea with mucus 14 .
The large intestine is normally responsible for the formation of stools, and when its function is impaired, mucous and loose stools occur.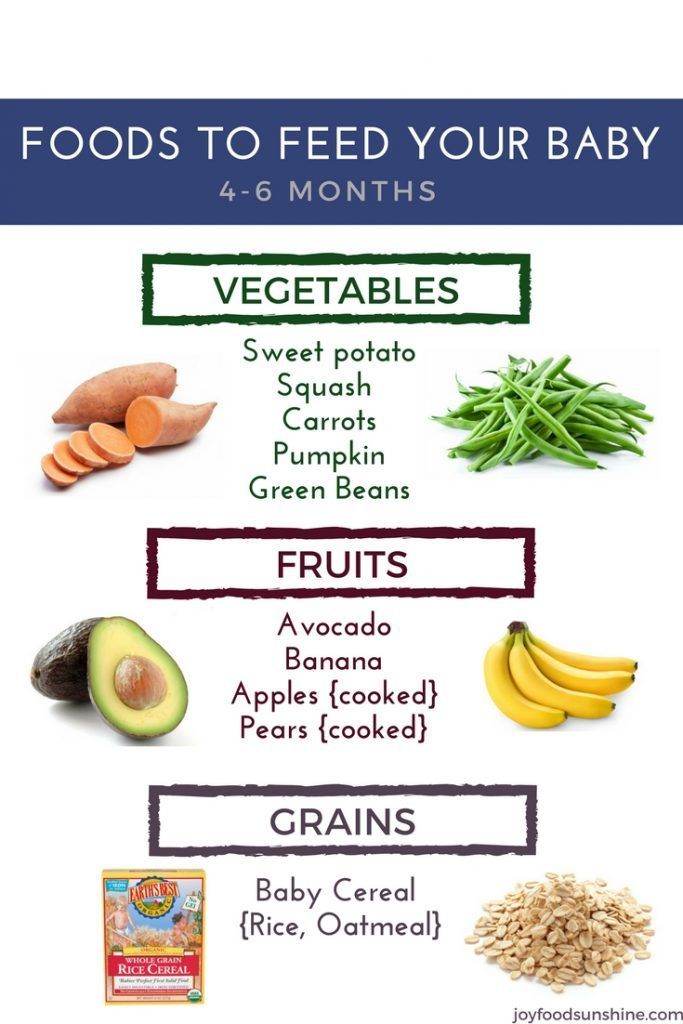
non-infectious causes
Chronic non-infectious diarrhea lasting more than 3 months 2 .
Mucopurulent diarrhea in children is often the result of an allergic reaction2,11. For young children, the main food allergens are cow and goat milk proteins. The list of allergens is expanding as new foods become available, and students and teens often already have allergies to foods containing eggs and gluten 10 . An unbalanced diet, frequent meals or very low meals can trigger the development of food allergies.
Liquid, wet stool with mucus and blood is observed in: 2.
- Ulcerative colitis is a disease in which the mucosa and submucosa of the large intestine are actively damaged, resulting in the formation of ulcers. It is based on the disruption of the body's immune response, which leads to chronic inflammation 16 .
- Crohn's disease is a pathological condition that occurs for a long time with repeated exacerbations. Unlike ulcerative colitis, this disease can affect all parts of the digestive system.
 In children and adolescents, the disease begins in the colon. In this case, chronic inflammation affects all layers of the intestinal wall 16,17.
In children and adolescents, the disease begins in the colon. In this case, chronic inflammation affects all layers of the intestinal wall 16,17. - Juvenile polyposis is the formation of multiple polyps in the small and large intestine, where mucus-producing epithelial glands are active 5 .
irritable bowel syndrome
Another cause of diarrhea in children and adolescents is irritable bowel syndrome. It is caused by dysfunction of the digestive system. In this case, the child usually has mucous diarrhea with grains of indigestible food.
Symptoms often appear in the morning, immediately after breakfast, for example on the way to school. This phenomenon is called "morning attack syndrome". In this case, during puberty, stools first form, but then the stool becomes mushy or moist. After a bowel movement, the child feels better and, as a rule, diarrhea does not recur during the day.
Antibiotic-associated diarrhea in children
Separately, it is customary to single out "antibiotic-associated diarrhea" - a violation of the stool that occurs during and several months after taking antibiotics 2 . Along with taking medications, the composition of the intestinal flora is disturbed, bacterial anomalies occur. Behind this is the fact that Clostridium actively multiply and pseudomembranous colitis develops. As a result, children develop recurrent and distressing diarrhea with mucus and blood6,15.
Along with taking medications, the composition of the intestinal flora is disturbed, bacterial anomalies occur. Behind this is the fact that Clostridium actively multiply and pseudomembranous colitis develops. As a result, children develop recurrent and distressing diarrhea with mucus and blood6,15.
Symptoms of diarrhea with mucus
Diarrhea is not an independent disease, but a separate symptom. In this case, it is important for parents to pay attention to the frequency, volume and consistency of the child's stool.
Children over one year old usually have no more than one or two bowel movements per day. The stool is usually dark brown, formed and hard. No visible impurities. Diarrhea results in loose stools and sometimes no solid food at all 13 .
Diarrhea with green mucus is often associated with bacterial infection 3 . When the colon is affected, stools usually pass repeatedly, but not in large quantities. In addition to mucus, it may also contain blood and pus2,7.
Food allergies may present with abdominal pain, frequent wet stools, and vitreous mucus. Persistent wet stools raises the suspicion of a more serious problem, especially a non-infectious one.
In intestinal infections, diarrhea is accompanied by pain in the abdomen (usually quite severe pain and cramps). Going to the toilet is painful, sometimes with false urge to defecate - effort 3.
If the stool is liquid, mucous and is accompanied by other symptoms, special parental attention is required 7 .
- Vomiting of indigestible food and bile, sometimes with blood.
- Fever - fever
- Tremor and weakness.
- Rarely urge to urinate.
- Flatulence - bloating.
- body pain, muscle pain
- A rash may appear on the skin.
- Anorexia.
- You may feel drowsy or, conversely, your emotions may be over the top.
- black chair
Severe diarrhea can cause dehydration in children, causing them to complain of thirst.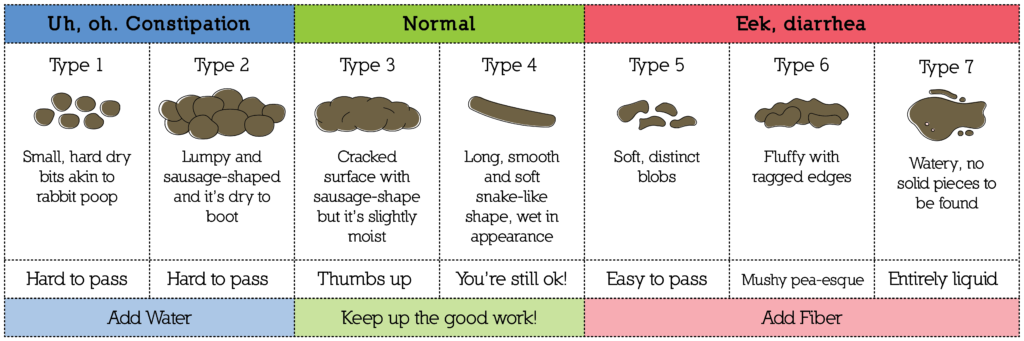 Diarrhea-related malabsorption of nutrients leads to weight loss in children 7 .
Diarrhea-related malabsorption of nutrients leads to weight loss in children 7 .
Recurrent episodes of diarrhea with mucus accompanied by other warning signs should be referred to a pediatrician 7 . The doctor will make the correct diagnosis and prescribe the appropriate treatment.
How is the child examined?
In most cases, diarrhea with mucus does not require special examination 7 . The doctor will understand the condition of the child, examine him and, based on this, recommend treatment. To distinguish between infectious and non-infectious causes of mucous diarrhea, pediatricians prescribe laboratory and instrumental studies4,7.
Telling your doctor about your child's eating habits, recent medications, allergies, etc. is essential for a proper diagnosis. 2.
Treatment
Diarrhea in children should be monitored by a qualified specialist such as a pediatrician or pediatric gastroenterologist. Only a doctor can correctly assess the severity of the patient's condition and prescribe adequate treatment.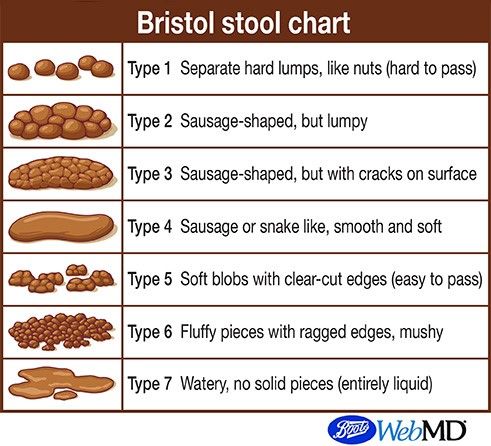
If the flow is light, give plenty of fluids to quickly replace the lack of fluid. If severe dehydration develops, hospitalization and intravenous saline may be required3,7.
dietary supplement
It is important to monitor your child's nutrition in order to quickly restore bowel function. Older children should eat 15-20% less food if the diarrhea is not severe and there are no signs of poisoning. It is best to cook the ingredients well and mash the food before serving. From 3-5 days you can return to the previous diet. Moderate diarrhea for the first few days with a 20-30% reduction in food intake and a gradual return to normal eating over 4-6 days 14 .
You should avoid eating foods that make diarrhea worse. Foods containing soft fibers should be added to the menu 14.
Diet for diarrhea with mucus in children 14
foods to avoid
medical care
Treatment should be comprehensive in order to remove the cause of mucous diarrhea. In addition to the main treatment, antidiarrheal medicine is used 7.
In addition to the main treatment, antidiarrheal medicine is used 7.
Imodium® can be used as a symptomatic treatment for children from 6 years of age. The active ingredient in this drug is loperamide, which delays peristalsis and reduces the amount of stool 12. Imodium® is recommended for acute and chronic diarrhea that develops in the background of allergies, changes in food intake and medications. Imodium may be used as an adjunct to combination treatment of infectious diarrhea.
Imodium® does not work directly on frequent or rotating flights. This drug only relieves the symptoms, which improves the condition of the child. Imodium® has contraindications, so you need to consult your doctor before using it. Use for children under the age of 6 and 12 years is contraindicated.
Diarrhea with baby mucus is a troublesome symptom. This symptom often indicates a serious condition of the digestive system. Therefore, it is important for parents to consult a doctor in a timely manner.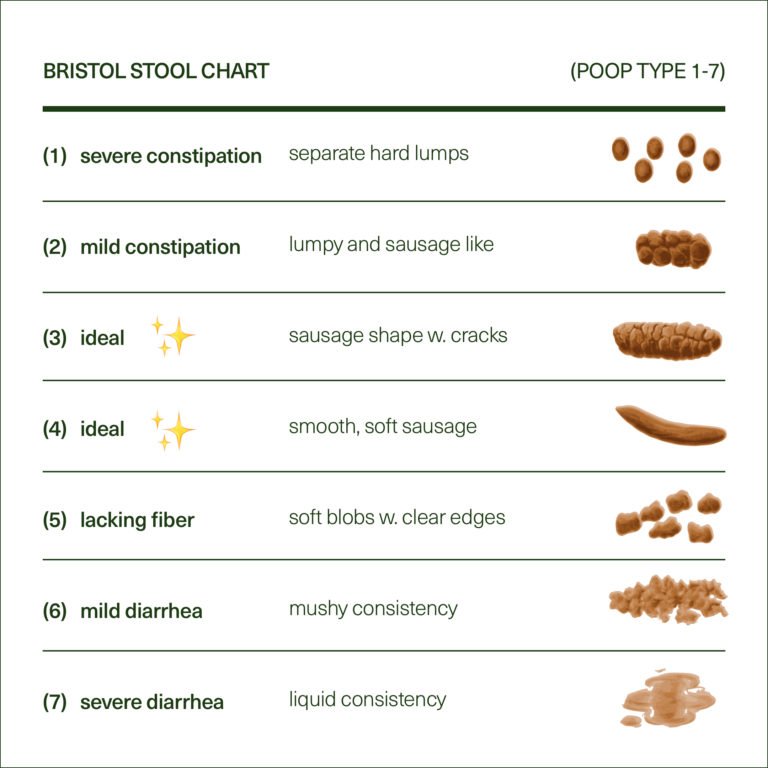 Specialists can find out the cause of free flights and choose the appropriate treatment.
Specialists can find out the cause of free flights and choose the appropriate treatment.
The information described in this article is merely a reference and does not replace expert medical advice. Please consult a qualified specialist for diagnosis and treatment.
Diarrhea, nausea and vomiting are symptoms of acute gastroenteritis, which are inflammation of the stomach and intestines. This can usually happen suddenly, with fever, mild abdominal pain, general malaise and weakness. Some people call it poisonous, blamed old salads and raw eggs, and believe others had "enteritis". In most cases, the cause of this disease is unknown, but the method of treatment for this disease remains the same.
Is poisoning and enteritis the same?
In general, this is true. Of course, doctors say poisoning is to consume obviously dangerous toxic substances in the body, such as mushrooms, which should not be eaten. Infectious diseases are mainly involved in microorganisms such as viruses and bacteria. It causes most of the acute gastroenteritis. In other words, both the "poisoned person" and the "infected person" actually have an intestinal infection.
It causes most of the acute gastroenteritis. In other words, both the "poisoned person" and the "infected person" actually have an intestinal infection.
Why do you have enteritis?
Some bacteria and viruses enter the body through contaminated water and food. For example, eggs, raw meat, and dairy products can contain salmonella and E. coli, while shellfish and lettuce can contain norovirus. In many cases, the danger is not the bacterium itself, but the toxin poison. For example, homemade canned toxins may contain botulinum toxins, and cream and pie may contain intestinal toxins in staphylococci. High temperatures do not harm all bacteria and cannot neutralize toxins.
In particular, if you do not wash your hands after going to the toilet, use shared utensils and towels, go to swimming pools and public places during the acute phase, you will directly get an intestinal infection from patients. You can. Rotavirus is often infected this way.
Is it dangerous?
Most intestinal infections are mild and resolve in 1-3 days. However, vomiting and loose stools cause the body to lose a lot of water and electrolytes. This can damage vital organs and even lead to death.
However, vomiting and loose stools cause the body to lose a lot of water and electrolytes. This can damage vital organs and even lead to death.
Dehydration can be dangerous, so it's important to recognize the signs early. These are:
In severe cases, there is a narrowing of the eyeballs and vestibule (in children under 1 year old), shedding of tears when crying, drowsiness, clouding of consciousness.
how to treat
Mild enteritis can be treated at home, but if in doubt, seek medical attention immediately.
The main task of treatment is the timely replacement of fluid and salt losses. Drink at least 50 ml of water per kg of body weight within 4 hours of the onset of illness. In this case, it is better to give the child frequent small sips to prevent vomiting. Thereafter, 10 ml/kg or more should be administered for each diarrhea and 2 ml/kg or more for each vomiting. For example, a child weighing 15 kg should drink 750 ml of fluid a few hours after the illness, then 150 ml each time with loose stools and 30 ml or more with each vomiting.
It is better to use a special solution sold in a pharmacy. Unlike other drinks, it contains a good balance of water and electrolytes. True, recent studies have shown that with mild gastroenteritis, drinks familiar to children (compote, diluted apple juice) can help.
But what about cola?
Cola is not suitable for the treatment of acute gastroenteritis. It contains some sodium and potassium, but contains a lot of caffeine and glucose, which will only aggravate diarrhea. The pH of cola is higher than the pH of gastric juice, so the myth that cola is acidic and therefore antiseptic is a myth. Perhaps in third countries, where intestinal infections are on the rise and access to clean drinking water is limited, people believed in the healing properties of cola. In this case, cola is actually an effective measure to counteract dehydration. But I find it frankly dubious to recommend using one particular brand instead of all sugary soft drinks. The official European guidelines for the management of children with diarrhea and vomiting warn against the use of sugary carbonated drinks (as well as concentrated juices) in infant formulas.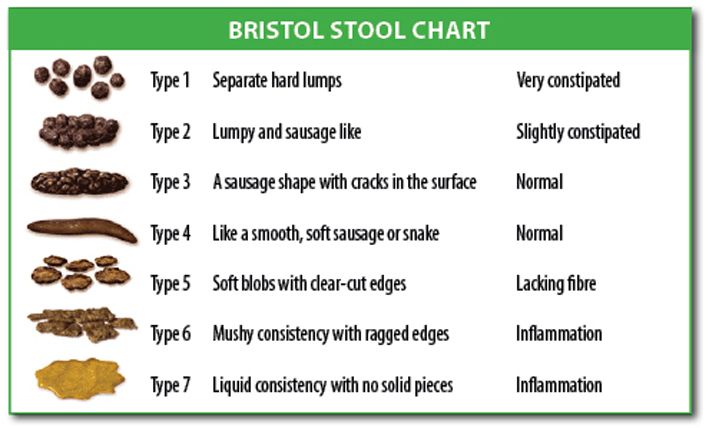
Is it okay to feed a baby with diarrhoea?
I need this. Your baby should be breastfed more often and, if formula-fed, formula-fed. Cereals, rice, potatoes, bread, lean meats, apples, bananas, sugar-free vegetables, and yogurt are good choices for older children. Fatty foods are difficult to digest and should be avoided.
But what about antibiotics?
Intestinal infections are often caused by viruses, so they do not use antibiotics. However, "bacterial" diarrhea does not necessarily require antibiotics. It is ineffective or, even worse, can cause serious harm. Therefore, the fact that blood is found in the stool (characteristic of bacterial inflammation in the large intestine) does not mean why you yourself start antibiotics. If you talk to a doctor, it will be carefully examined and it will probably order a "intestinal group" stool test so that you can clarify the specific pathogen and determine if antibiotics are needed.。
Drink and feed...
 is that all treatment?
is that all treatment? In general, this is true. Recently, the effects of probiotics, feeders and zinc (children within 6 months) have been actively discussed. Researchers have more questions about the effects of probiotics, but snowballing and zinc preparations seem to be able to shorten the period of diarrhea by about one day. The use of antidepressants for childhood intestinal infections is prohibited. Enzymes are not shown and the effectiveness of the immunosuppressive agent has not been proven. Therefore, treatment should give appropriate watering and food intake, monitor the disease, and if you have alarming symptoms, you should immediately consult a doctor.
Diarrhea is an abnormal defecation symptom with frequent loose stools (more than three times a day). This may be due to intestinal infections, poisoning, surgical pathology, and mental factors. Experienced doctors at the Moscow SM-Doctor clinic will find out the cause of children's diarrhea (frequency) and prescribe a full treatment.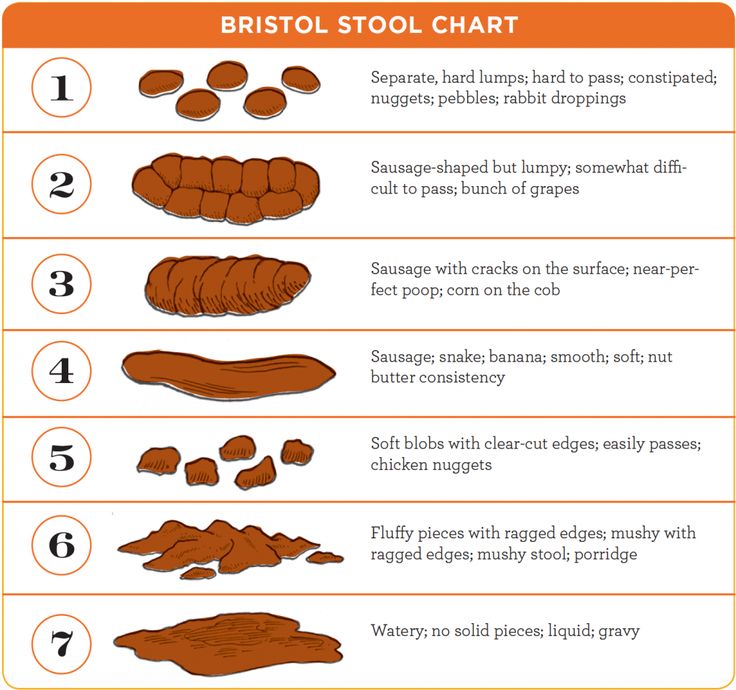
About the disease
Diarrhea is not an independent disease. This is a symptom caused by the intestines, damaged toxins, bacteria, viruses, etc. found by normal functions and increased bowel movements.
It is important to note that this symptom can be a serious health hazard for children, especially young children (under 3 years of age). Because water stools are common, large amounts of water, trace elements, and macronutrients are lost from the child's body. In such a defect, the pathological change in the function of the brain, heart and kidneys of the child progresses very quickly.
Classification of diarrhea in children
There is no widely recognized classification of the type of disease. Doctors distinguish between acute diarrhea (within 14 days) and chronic diarrhea that lasts more than two weeks. In addition, diarrhea for children is the type depending on the cause.
- Subject.
- Toxicity?
- Toxic, toxicity, allergy, etc.
Symptoms of diarrhea in children
Diarrhea is a symptom caused by an organic, functional or infectious disease of the digestive tract. This feature is that the free stool is distributed more than three times a day. Depending on the underlying cause, childhood diarrhea may accompany the following clinical symptoms.
- Change the character of the chair
- Abdominal pain (can always be painful or tight).
- Fever is a typical symptom that occurs when bacteria enter the gastrointestinal tract.
- Blue white leather
- Serious weakness of the whole body. In case of dehydration, children become lethargic, do not want to play, and sometimes get out of bed.
- Reduced quality of sleep
- Anorexia, weight loss (in case of acute diarrhea weight loss loses a lot of water).
If the bowel is infected with bacteria, the appearance of the stool is characteristic and may help identify the underlying disease.
The severity of the clinical picture depends on the degree of damage to the gastrointestinal tract, the individual characteristics of the child's body, the aggressiveness of the pathogen. If you find these symptoms, you should seek immediate medical attention to reduce your risk of serious complications and start appropriate treatment.
Causes of diarrhea in children
The etiology of childhood diarrhea is insufficient irritation of the intestinal mucosa, accompanied by excessive secretion of mucus, reduced absorption of nutrients, a rapid increase in the strength and frequency of peristaltic movements of the corresponding part of the gastrointestinal tract. Possible causes of acute diarrhea.
- Food poisoning - consumption of poor-quality products can cause acute gastrointestinal illness, accompanied by vomiting, as well as diarrhea.
- Bacterial or viral invasion - when food or water contaminated with pathogenic microorganisms is consumed, gastroenteritis develops with damage to the entire digestive system.
- Toxins in the body. The use of drugs and chemicals causes toxic damage to the lining of the stomach and intestines, leading to diarrhea.
Chronic diarrhea in children is most often caused by disorders of the internal organs directly related to digestion. The traditional causes of this clinical picture are exacerbations of pancreatitis, autoimmune bowel disease, ulcerative colitis, irritable bowel syndrome, lactose and gluten intolerance.
Diagnosis of diarrhea
SM-Doctor is a modern medical center staffed by highly qualified doctors. Using modern diagnostic methods and a comprehensive assessment of the health status of each baby, our specialists can quickly and objectively determine the cause of diarrhea.
Diagnosing the cause of acute diarrhea is not important. Based on the patient's complaints, anamnesis data, examination of feces, etc., an experienced doctor can make a preliminary diagnosis already at the first visit. Therefore, the doctor will prescribe a microscopic examination and bacteriological analysis of the patient's feces.
Diagnosis of chronic diarrhea can be difficult. In this case, doctors use the following methods to identify the underlying cause of the symptoms:
- - This is an x-ray study that allows you to understand the state of the entire gastrointestinal tract. - Endoscopic method: a method in which a thin catheter with a camera is inserted into the cavity of the large intestine of a child.
- A set of specific laboratory tests designed to detect autoantibodies to the virus or autoantibodies to the intestinal mucosa.
If necessary, the child should be referred to specialized specialists to exclude or confirm the presence of other visceral and systemic diseases.
Treatment of diarrhea in children
The choice of treatment for acute and chronic diarrhea in children depends on the cause and type of diarrhea.
The essence of the treatment is the correction of water and electrolyte balance. During the acute phase, infants should be given plenty of fluids (sometimes with saline) to prevent dehydration. After determining the cause of diarrhea, doctors prescribe psychotropic drugs.
After determining the cause of diarrhea, doctors prescribe psychotropic drugs.
The following groups of drugs can be used for this purpose.
- Antibiotics to kill pathogens.
- Control pain with antispasmodics.
- An enzyme prescribed when pancreatic dysfunction is recognized and digestion is stable.
- Benefits used to combine toxins and the daily needs of pathogens.
- Probiotics is a drug group that influences the return of intestinal flora that has been damaged by bacteria, viruses and toxins.
In case of a surgical disease condition, surgery may be required to remove it. Delia is a problem that should be diagnosed as soon as possible and treated.
Prevention of diarrhea
Prevention of diarrhea mainly to prevent infectious diseases that may occur in the gastrointestinal tract. Therefore it is recommended.
- Long-term mothers for child care
- Do not feed the donkey for less than 6 months.
- Feeling of consumption feeling of feeding (ban on fast food) after the start.
- Use only fresh ingredients.
- SM-Fetor experts have successfully treated children who suffer from diarrhea from all causes for many years. We guarantee the highest quality services with advanced technology and the latest abilities related to early digestive diseases. If you have worrisome symptoms, consult an expert
Diarrhea is a symptom that parents with children are often afraid of. On the other hand, the depletion of toxins in the body in this way is an important defense mechanism. On the other hand, the child begins to immediately lose water, and this situation can develop life dehydration. Therefore, if diarrhea occurs, it is important to restore moisture and reduce pathological symptoms as soon as possible, and it is important to consult a doctor.
Doctor's opinion
Should I protect my diet with diarrhea?
Q&A
of course! (Laughs, as far as possible, everything that can worsen the symptoms, such as berries, fruits and dairy products, should be excluded.
 Eating a small amount (according to a doctor's prescription) is a small amount.。
Eating a small amount (according to a doctor's prescription) is a small amount.。 Do I need antibiotics for diarrhea?
The cause can only be identified by a doctor's diagnosis with only infectious diseases.
Uchaikin V.F., Balikin V.F., Siam Shiwa O.V. A guide to infectious diseases for children. M. Geotar-Media 2021.
References
- Pediatric disease: Manual / Edition Moscow: Geotar-Media, 2007.
- Moscow
Pediatric Clinic M. Ulitsa 1905.
Food poisoning is an acute infectious toxic condition. Occurs when using poor quality pathogens, harmful substances and poisonous things. The main symptoms are diarrhea, vomiting, fever, dehydration and severe addiction. The goal of treatment is to quickly ward off poisoning, compensate for the lack of body fluids, and prevent complications.
Drinking poisoning is caused by poison and poisoning. I got sick after taking bad food, water, plants, chemicals and medicines.
Classification
There are two types of food poisoning for children.
Infectious disease. The causative substances are microorganisms and their toxic beings.
- N E-WINE. Plants, animals obtained by toxic substances and harmful impurities.
- During the asymptomatic periods of food poisoning and incubation, toxins entered the body before the first symptoms appeared. The period depends on the individual difference, age, amount of poison and absorption rate. This stage is most suitable for treatment, because the poison has not yet entered the bloodstream.
The toxin stage begins with the first symptom of poisoning and continues until the bacteria and toxins in the body have been completely eliminated. At this time, all the symptoms of poisoning appear. To effectively carry out treatment, it is necessary to identify toxins and promote excretion processes.
The last stage of rest restores clear functions of the digestive system, the excretion system and the immune system.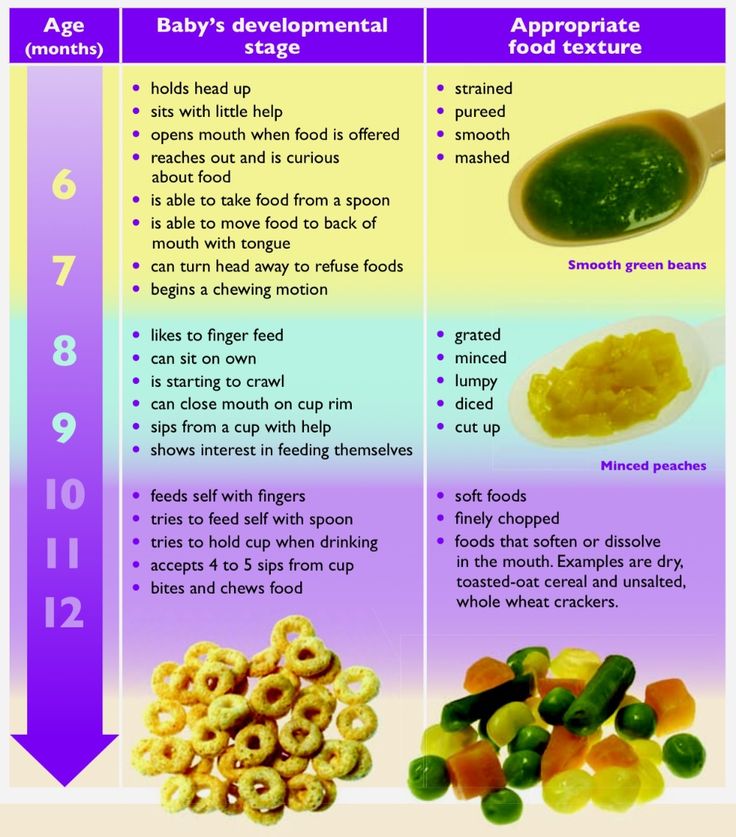
Food poisoning is one of the most common problems in pediatrics. In the case of children, dependent symptoms are less likely than adults. This is based on the characteristics of the child's body, such as reduced gastric acidity, lack of intestinal flora, rapid absorption of poisoning, and toxins are distributed throughout the body.
Causes
The main pathogens of childhood food poisoning are Staphylococci, Protes, Creb Sierra, intestinal toxic Escherichia and Crostidium bacteria. The pathogen invades the body only from food, grows in it and releases toxins.
Causes that the quality of food is broken.
Non-surgical rules of hygiene
- Food for people with intestinal infections and purulent diseases (tonsillitis, ragitis, pancreatitis, mastitis, chain viginitis).
- Pollution of soil and plants and animal faeces.
- Rotten foods may show off taste, odor and unusual viscosity, but in many cases the organs, organs, are in the normal range.
- Inappropriate poisoning results from accidental use of berries, plants and mushrooms. If you use toxic sterilizers and agricultural products contaminated with insecticides, you may be poisoned.
In the case of children, it seems that food poisoning often occurs after the use of inseparable water, missing milk and dairy products.
Dangerous products as follows.
Which products are classified as potentially hazardous?
I use eggs.
Eggs; eggs; -Sets using fresh cream.
- seafood.
- Sausage, sausage, sausage, sausage with fish and cream, sausage with fish meat.
- Can be preserved with meat and vegetables
- Mushrooms.
- Food poisoning is often diagnosed from summer to autumn. Currently, microbial pathogens can spread.
- Despite the variety of treatment, the clinical symptoms are almost the same. The incubation period may take an average of 2 to 6 hours, over 30 minutes, or may take a day or more.
 Signs of poisoning appear with gastroenteritis, poisoning and dehydration.
Signs of poisoning appear with gastroenteritis, poisoning and dehydration.
Poisoning always begins with i-nausea, multiple vomiting from particle-like particles. The child complains of abdominal pain, stools are watery, mucous membranes, green impurities and live blood. Intestinal secretions occur about 5 to 10 times a day.
Symptoms of food poisoning in a child
At the same time as the behavioral disorder, it rises to 38-39 degrees. Signs of poisoning appear immediately: refusal of food, head and muscle pain. When dehydration symptoms appear, symptoms such as drying pale, dryness of the face, decreased urination, and drying of the mucous membranes. In infants, the fonnelnel is lowered. Convulsions are common in food poisoning and the acidosis progresses.
In many cases, symptoms of poisoning gradually disappear after 2-3 days, but weakness and abdominal pain may last for several weeks.
Severe food poisoning is common in infants whose immunity is declining. The risk of complications associated with drug poisoning is also increased by premature babies, minorities, and recurrent biological disorders.
The risk of complications associated with drug poisoning is also increased by premature babies, minorities, and recurrent biological disorders.
If the child is poisoned by poisonous and poisonous fruits, there is damage to the central nervous system.
Suppression of reaction
Euphoria; euphoria;
- Phantom -
- Language and visual disturbance
- Convulsions; convulsions; hallucinations; hallucinations, hallucinations, hallucinations, convulsions.
- When toxins affect the circulatory system, the heart rate increases, slow or blood pressure decreases.
- Mushroom poisoning is very dangerous for children. After using the throat by the pale monkey, indomitable vomiting and dung diarrhea of cholera, including blood impurities, begin. Other symptoms include intestinal pain, respiratory distress, and seizures. Toxins adversely affect the liver and develop hepatitis. He dies and due to acute liver failure at 90% of cases.

Signs of Galik flyer poisoning a-included saliva, shortness of breath, violent vomiting, convulsions, bronchial convulsions, hallucinations, glancing, strangers, etc. However, the mortality rate does not exceed 1%.
Botulinum poisoning occurs when you eat bad canned food. This toxin affects the nervous system and appears in the form of paralysis and parks. Poisoning of children can cause acute respiratory failure and heart rate. The first symptoms appear after 4-6 hours. I am worried about epidemic pain, nausea, vomiting and diarrhea. Sometimes there may be problems with visual acuity. When the respiratory system is damaged, breathing begins, the skin near the triangle of the face turns blue, and arrhythmia occurs.
Action required immediately. First Aid Rules
Mushrooms, berries and medicines cause vomiting.
First aid for child poisoning
Stomach washes and purifies water to flush out toxins in the intestines. Babies cannot do this on their own, as they may vomit from their breath. Instead, you can do a cleansing enema. The amount of water for cleansing the stomach is 16 ml / kg for 3-6 years, and 7 years - up to 14 ml / kg.
Instead, you can do a cleansing enema. The amount of water for cleansing the stomach is 16 ml / kg for 3-6 years, and 7 years - up to 14 ml / kg.
- Tenkovy intestinal absorption is a drug that collects toxins in the intestinal cavity and excretes it with the help of stool.
- Let's drink more. You must drink it often, but frequently. Drinking weak saline, weak tea and mineral water can be drunk without gas.
- Call a doctor.
- Timely first aid leads to the prevention of addiction to poisoning.
- With addiction children are impossible.
Give foods that are effective for painkillers, medications, vomiting, and diarrhea.
Place a warm and cold cloth over the abdomen.
- It promotes vomiting in soda and nets the stomach with potassium permanganate.
- Give milk and dairy products.
- Pediatricians and infectious diseases can diagnose food poisoning in children. The inspection begins with the Gabbages collection and patient consultation.

- A specific diagnostic test is ordered to identify the pathogen. Generic substances o-fecal stool, vomiting, cleansing gastric water, contaminated food residues. Blood bacteria are prescribed for a general infection. Auxiliary lift method, PCR, ELISA. You may need to see a neurologist, digestive, or surgeon.
Diagnosis of food poisoning in a child
It is obligatory to carry out a differential diagnosis and exclude acute gastritis, cholecystitis, pancreatitis, iodosis, acute enteritis, appendicitis, meningitis. Blood tests are done to rule out viral or bacterial infections and stool tests to check for unusual bacterial infections.
Treatment of poisoning in children begins with the elimination of signs of dehydration. Administer oral and parenteral hydration therapy.
enzyme?
How to treat
Snow Rativa
- Prebiotic that restores the balance of intestinal flora.
- Severe toxic infections require antibiotics.

- For freshwater frog poisoning, emergency bleeding is performed to cleanse the blood of toxins.
- Children should not be fed for 12-24 hours after poisoning. After the cessation of vomiting, a moderate diet is prescribed. Breastfed babies under one year of age should avoid certain foods.
How to feed a child after poisoning.
Diet in case of poisoning in a child
Moist porridge - rice, buckwheat, boiled in a mixture of equal parts of water and milk.
A few days later: Vegetable puree, baby cottage cheese or kefir, plain yogurt.
- Meat soufflé, fish soufflé, etc. are gradually being introduced into the menu.
- Prohibited foods are pastries, whole milk, black bread and freshly baked white bread. Do not give pasta, chocolate, ice cream, ice chips, sugary sodas, wheat or barley porridge. From vegetables, cucumbers, tomatoes, cabbage are contraindicated.
- The duration of the diet is 14 days.
- Complications arise due to severe poisoning, lack of adequate and timely treatment.

- dysbacteriosis
- renal failure, liver failure
- Disorders in the work of the nervous system, immune system.
chronic gastrointestinal disease
Poisoning in children of mild and moderate severity ends in complete recovery.
Possible consequences of food poisoning in a child
Store the product correctly and respect the temperature and other storage conditions.
- According to the rules of heat treatment, children should never eat raw fish or low-quality fried meat.
- Do not swallow water when swimming in an aquarium.
- Wash your hands, vegetables and fruits frequently.
- Keep medicines and chemicals out of the reach of children.
Prognosis and prevention
Tell children about poisonous mushrooms, poisonous berries, poisonous plants and the dangers of their use.
- Those who work in the orphanage's kitchen should have regular medical check-ups.
 Employees with signs of pustular skin diseases, respiratory diseases or intestinal infections are not allowed in the catering department.
Employees with signs of pustular skin diseases, respiratory diseases or intestinal infections are not allowed in the catering department. - Food poisoning in children is a dangerous condition, so seek immediate medical attention without self-diagnosis. Call our office and tell us about your symptoms, the patient's condition and possible causes of poisoning. The Miracle Doctor center manager will write to the Doctor shortly.
- Why is acute poisoning dangerous for children?
- Fever, vomiting more than 3-5 times, diarrhea in children are reasons for an immediate call for an ambulance.
- Poisoning of children, regardless of age, leads to a breakdown of the immune system. Dehydration is very dangerous for babies. Children under 4 years of age who vomit profusely and have loose stools for several hours may experience a critical period of dehydration.
- If my baby is vomiting a lot, how should I feed him?
Even if vomiting is severe and stable, children must drink.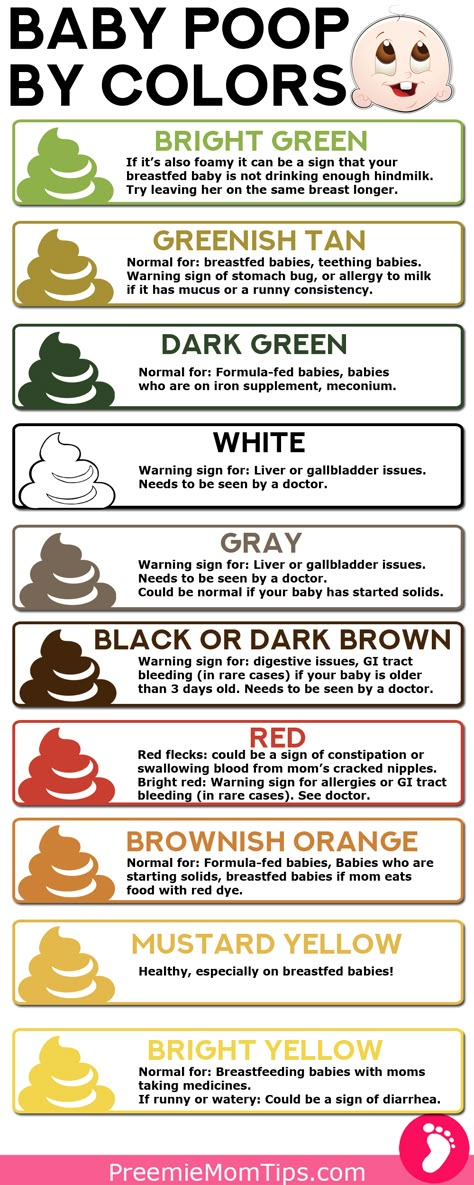 Dehydration is very dangerous for a child's body. Children should be divided into a small teaspoon and drink. Every 5 minutes, the water should not be cold, so as not to cause cramps and vomiting. The optimum temperature is a few degrees above body temperature.
Dehydration is very dangerous for a child's body. Children should be divided into a small teaspoon and drink. Every 5 minutes, the water should not be cold, so as not to cause cramps and vomiting. The optimum temperature is a few degrees above body temperature.
Food poisoning treatment in Moscow
Shutterstock_1065379265.jpg
Q&A
疝 pain 4.jpg
New terraca lactose.jpg0003
Peptide_ststst.jpg
Allergy 4.JPG
Diarrhea with baby mucus
Normal stools of newborns and children up to the first six months of life
The contents of a diaper excite every young mother. Any change or change in the frequency of bowel movements causes her to panic and forces her to look for diseases in the child. We understand how the gastrointestinal tract works in infants and what the baby's stool should be like.
Peculiarities of digestion in an infant
Despite the long intrauterine development, many systems and organs of a newborn child cannot fully perform their functions.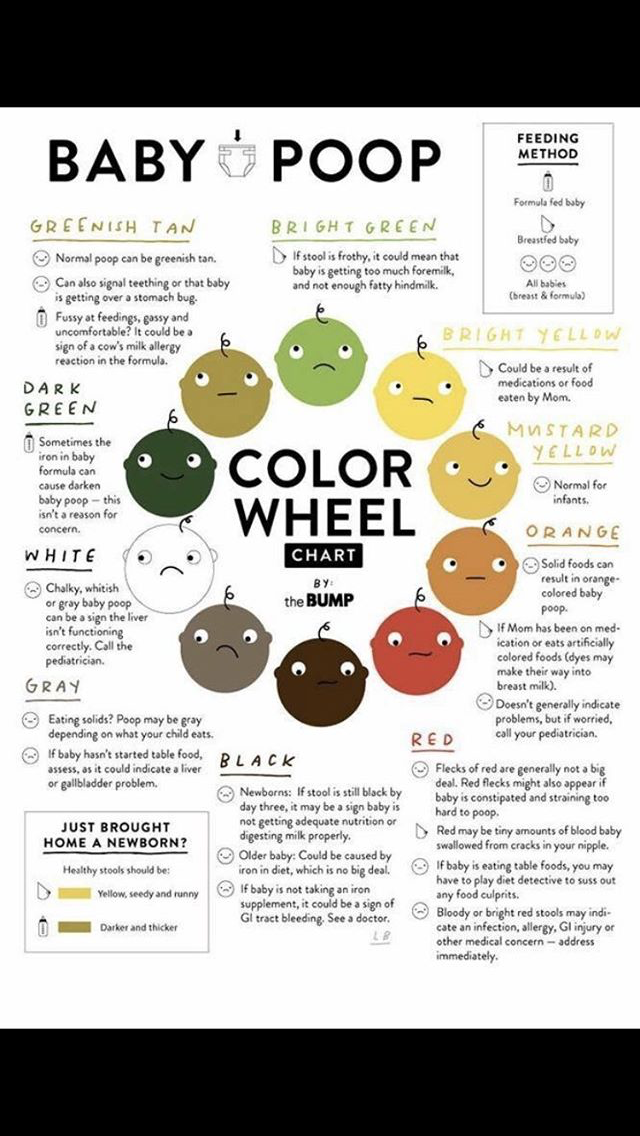 The gastrointestinal tract is no exception. Babies don't have teeth to chew solid food, and their liver and pancreas don't produce enough enzymes.
The gastrointestinal tract is no exception. Babies don't have teeth to chew solid food, and their liver and pancreas don't produce enough enzymes.
In addition, the baby is born with a sterile intestine. Its settlement with beneficial microflora occurs in the first weeks of life, and full development can last up to a year. Children of the first half of the year eat only breast milk or a milk mixture adapted for their intestines. Feeding whole milk or fermented milk products is dangerous to his health.
The baby's stool is also different. In the first days of life, a newborn baby passes meconium - the original feces are usually dark green or black. Then it gradually changes color, smell and texture. What exactly it will be depends on the type of feeding and the characteristics of the child himself.
Stool norm in newborns and children up to a year
Normal stool indicators depend on how the mother feeds the child, whether he has congenital gastrointestinal diseases, allergies or intolerances. The frequency of stool in a newborn and children in the first half of life also depends on this.
The frequency of stool in a newborn and children in the first half of life also depends on this.
| Type of | Description |
| Chair in newborns while breastfeeding | In the first six months, the stool is mushy, soft, blotches and inclusions may occur. The first months does not smell strongly, then the smell changes. May be completely absent for several days. |
| Chair in infants with artificial feeding | The chair is regular from one to 6 times a day. Often associated with feeding (a bowel movement occurs before or during it). Thicker, pasty, smells stronger than breastfed babies |
With mixed feeding, the frequency and appearance of the stool depends on the proportion in which the child receives breast milk and an adapted mixture.
At first, the baby can defecate after each feed. Over time, stool frequency decreases and volume increases. This can be scary for new parents. Our doctors remotely and at any time of the day will answer all questions about the health of the child and help determine when stool changes indicate pathology.
Over time, stool frequency decreases and volume increases. This can be scary for new parents. Our doctors remotely and at any time of the day will answer all questions about the health of the child and help determine when stool changes indicate pathology.
Newborn stool color
The second parameter, after the frequency, to which mothers pay the closest attention, is the color of the child's stool. Normally it is yellow or orange. It can be plain or with white patches. This color is typical for fresh stools when the baby has just gone to the toilet.
When exposed to air, the feces oxidize and become greenish in color. This is not a pathology. This color of the stool does not require treatment or medical attention. However, a sharp change in color, consistency or frequency of bowel movements, the appearance of foam, blood and streaks in the feces can indicate digestive problems - lactase deficiency, constipation, allergies, dysbacteriosis.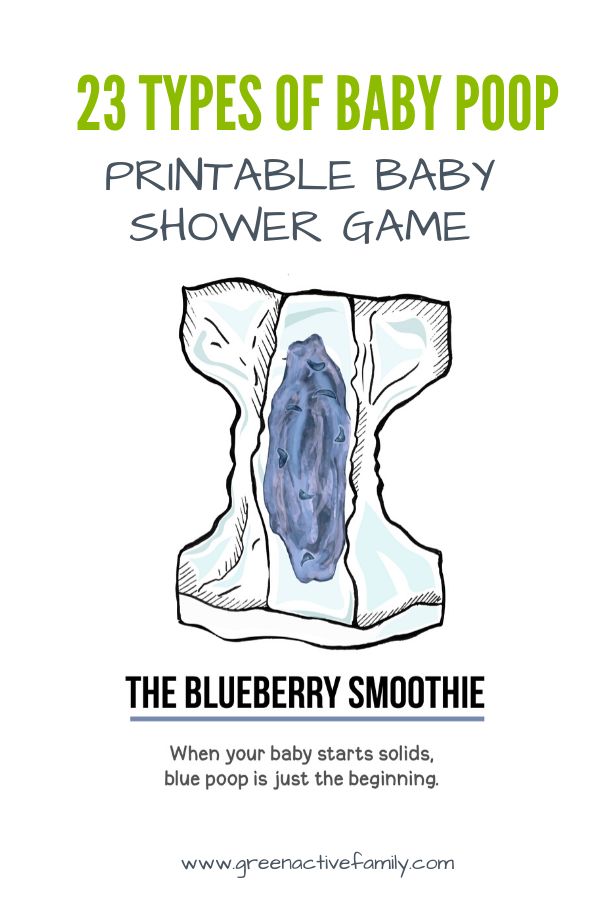
What problems does stool disorder indicate?
It is believed that the feces of a newborn should depart daily and not cause him any inconvenience. However, in children who are fully breastfed, stools may be completely absent up to 6 days. If after that the baby defecates without problems, and the feces themselves remain soft, this is considered a variant of the norm.
However, in some cases, a violation or change in bowel movements can indicate problems with digestion. The main ones are:
- constipation;
- diarrhea;
- allergy;
- intolerance to certain products;
- lactase deficiency;
- bleeding in the gastrointestinal tract;
- cracks.
The main symptoms to look out for include the following:
- the child becomes restless and capricious;
- he draws his legs to his stomach;
- the chair becomes rare and dense;
- the stool becomes too liquid and frequent;
- mucus, blood streaks, black blotches appear in the feces;
- stool immediately green;
- he smells bad;
- foam is visible in the feces.
These symptoms should be reported to the health visitor or pediatrician during the preventive visit. If blood is found in the diaper, you should immediately call an ambulance and hospitalize the child.
Changes in stool may indicate problems with the gastrointestinal tract in a child. It can be difficult for young parents to distinguish the norm from the pathology, so if you have any concerns, you should consult a pediatrician. Our doctors will answer all your questions about your baby's health, help you find the problem and tell you what to do in case of illness.
How to help your baby with stool problems
To help the baby, you need to understand why there are problems with the stool. To do this, the pediatrician will offer to undergo diagnostics - take blood tests, check feces, sign up for an ultrasound scan, colonoscopy or gastroscopy. The latter in young children are performed under general anesthesia and require temporary hospitalization.
After making a diagnosis, the doctor will suggest treatment and related activities:
- If an allergy is suspected, a nursing mother will be offered to follow a hypoallergenic diet. If the baby is bottle-fed, they will offer to change the mixture.
- Also, the doctor will give recommendations on the diet of the child. Breastfeed your baby freely, but less than once every two hours. Formula-fed babies can tolerate long intervals.
- In case of allergies, the child may be recommended to take antihistamines and sorbents.
- With confirmed lactase deficiency, the child is either transferred to a lactose-free mixture, or it is recommended to give special enzymes before feeding.
- If constipation, diarrhea and dysbacteriosis are suspected, the child may be prescribed drugs to improve the stool or special mixtures with lacto- and bifidobacteria.
- If an infection is suspected, against which diarrhea began, the baby may be prescribed antibiotics and antiviral agents.
If congenital pathologies of the development of the gastrointestinal tract are detected during the examination, the doctor takes appropriate therapeutic and preventive measures. Which ones and for how long depends on the type of disease and its degree.
Important! Abdominal problems are often associated with increased gas or colic. In this case, it is recommended to massage the abdomen, put a warm heating pad on it, or put the bare tummy against the mother's stomach.
FAQ
How many times a day should a newborn have a stool?
+
In the first days of life, the child passes meconium. After that, the chair can be after each feeding. In a month-old baby, the frequency of stools is removed and varies from 1 to 6 times a day. In children who are fully breastfed, it can recede up to 6 days.
What does feces look like in newborns?
+
Newborn babies have black or dark green stools. Over time, it brightens, becomes yellow-orange. It may contain white blotches and heterogeneities.
Over time, it brightens, becomes yellow-orange. It may contain white blotches and heterogeneities.
What are the problems with the chair?
+
The problems are indicated by the absence of stool against the background of the child’s anxiety and a change in the consistency of feces, too frequent stools, bad smell, foam, green color of feces immediately after a bowel movement, the appearance of streaks and inclusions of red and black or mucus in it.
What to do if the child does not poop?
+
If the child behaves normally (does not cry, does not act up and does not tighten his legs), and after the stool is pasty and easily leaves, then nothing needs to be done. If the child is worried and cannot poop, you need to see a doctor. He will conduct examinations and prescribe treatment.
Expert opinion
A change in the stool of a newborn, its complete absence or too frequent bowel movements can indicate digestive problems, allergies, and congenital diseases of the gastrointestinal tract.