Baby throwing up food no fever
Why This Happens and What to Do
It can be difficult to tell the difference between vomit and spit-up. Both might look the same since your baby is currently on a steady of diet of milk or formula. The main difference is in how they come out.
Spit-up usually happens before or after a burp and is most common in babies under the age of 1 year. Spit-up will easily flow from your baby’s mouth — almost like white, milky drool.
Vomit typically comes out forcefully (whether you’re a baby or an adult). This is because vomiting happens when the muscles around the stomach are triggered by the brain’s “vomiting center” to squeeze it. This forces whatever is in the stomach to be hurled out.
In a baby’s case, vomit may look like milky spit-up but have more clear stomach juices mixed into it. It may also look like milk that has been fermented for a little while — this is called “cheesing.” Yes, it sounds gross. But the texture probably won’t bother you when you see it — you’ll be more concerned with baby’s well-being.
Your baby may also cough or make little retching noises before they vomit. This is likely the only warning you’ll have to grab a towel, bucket, burp cloth, sweater, your shoe — hey, anything.
Additionally, spit-up is normal and can happen at any time. Your baby will only vomit if there’s a digestive issue or they have another illness.
Feeding difficulty
Babies have to learn everything from scratch, including how to feed and keep the milk down. Along with spit-up, your baby may vomit occasionally after being fed. This is most common in the first month of life.
It happens because your baby’s tummy is still getting used to digesting food. They also have to learn to not gulp milk down too fast or overfeed.
Post-feeding vomiting typically stops after the first month. Give your baby more frequent, smaller feeds to help stop the vomit.
But let your pediatrician know if your baby vomits often or has very forceful vomits. In some cases, it might be a sign of something other than feeding difficulty.
Stomach flu
Also known as the tummy bug or “stomach flu,” gastroenteritis is a common cause of vomiting in babies and children. Your baby may have cycles of vomiting that come and go for about 24 hours.
Other symptoms in babies may last for 4 days or longer:
- watery, runny poop or mild diarrhea
- irritability or crying
- poor appetite
- stomach cramps and pain
The tummy bug can also cause a fever, but this is actually less common in babies.
Gastroenteritis usually looks a lot worse than it is (thank goodness!). It’s typically caused by a virus that goes away by itself in about a week.
In babies, severe gastroenteritis can lead to dehydration. Call your pediatrician immediately if your baby has any signs of dehydration:
- dry skin, mouth, or eyes
- unusual sleepiness
- no wet diapers for 8 to 12 hours
- weak cry
- crying without tears
Infant reflux
In some ways, babies really are like tiny adults. Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Vomiting from acid reflux happens when the muscles at the top of the stomach are too relaxed. This triggers baby vomiting shortly after feeding.
In most cases, the stomach muscles strengthen, and your baby’s vomiting goes away on its own. Meanwhile, you can help slow down the vomiting by:
- avoiding overfeeding
- giving smaller, more frequent feeds
- burping your baby often
- propping your baby up in an upright position for about 30 minutes after feeding
You can also thicken milk or formula with more formula or a bit of baby cereal. Caveat: Check with your pediatrician before you try this. It might not be suitable for all babies.
Cold and flu
Babies catch colds and flus easily because they have shiny new immune systems that are still developing. It doesn’t help if they’re in day care with other sniffling kiddos, or they’re around adults that can’t resist kissing their little faces. Your baby may have up to seven colds in their first year alone.
Your baby may have up to seven colds in their first year alone.
Cold and flu can cause different symptoms in babies. Along with a runny nose, your baby may also have vomiting without a fever.
Too much mucus in the nose (congestion) can lead to a nasal drip in the throat. This can trigger bouts of forceful coughing that sometimes cause vomiting in babies and children.
As in adults, colds and flu in babies are viral and go away after about a week. In some cases, sinus congestion may turn into an infection. Your baby will need antibiotics to treat any bacterial — not viral — infection.
Ear infection
Ear infections are another common illness in babies and children. This is because their ear tubes are horizontal rather than more vertical like in adults.
If your little one has an ear infection, they might have nausea and vomiting without a fever. This happens because an ear infection can cause dizziness and loss of balance. Other symptoms of ear infections in babies include:
- pain in one or both ears
- tugging or scratching at or near the ears
- muffled hearing
- diarrhea
Most ear infections in babies and children go away without treatment.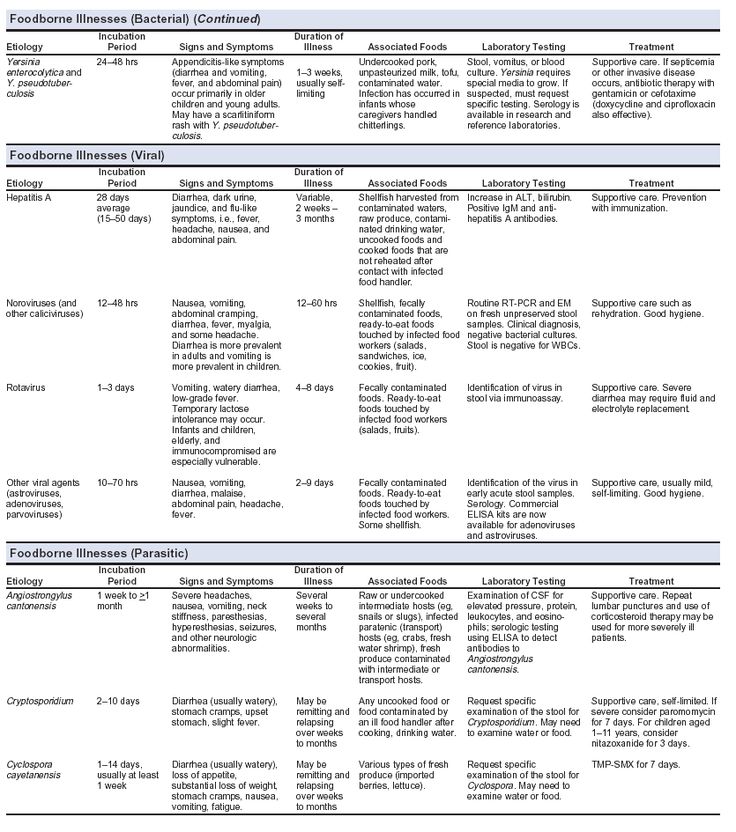 However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
Overheating
Before you swaddle your baby or put them in that adorable fluffy bunny suit, check the temperature outside and in your home.
While it’s true that the womb was warm and cozy, babies can overheat quickly in hot weather or in a very warm house or car. This is because their tiny bodies are less able to sweat out heat. Overheating might cause vomiting and dehydration.
Overheating can lead to heat exhaustion or in much more serious cases, heatstroke. Look for other symptoms like:
- pale, clammy skin
- irritability and crying
- sleepiness or floppiness
Immediately remove clothing and keep your baby out of the sun and away from heat. Try to breastfeed (or give your baby water if they’re 6 months or older). Get urgent medical attention if your baby doesn’t seem their usual self.
Motion sickness
Babies below the age of 2 years don’t commonly get motion or car sickness, but some babies may get sick after a car ride or being twirled around — especially if they’ve just eaten.
Motion sickness can make your baby dizzy and nauseous, leading to vomiting. It might be more likely to happen if your baby already has an upset tummy from bloating, gas, or constipation.
Strong smells and windy or bumpy roads can also make your baby dizzy. Nausea triggers more saliva, so you might notice more dribble before your baby vomits.
You can help prevent motion sickness by traveling when your baby is ready to sleep. (Great trick if your baby loves to sleep in the car!) A sleeping baby is less likely to feel queasy.
Keep their head well supported in the car seat so it doesn’t move around too much. Also, avoid going for a drive right after giving your baby a full feed — you want your baby to digest the milk, not wear it.
Milk intolerance
A rare kind of milk intolerance is called galactosemia. It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It can cause nausea and vomiting after drinking milk or any kind of dairy products. Galactosemia can also cause a skin rash or itching in both babies and adults.
If your baby is formula fed, check the ingredients for any dairy, including milk proteins.
Most newborns are screened at birth for this rare condition and other illnesses. This is usually done with a heel prick blood test or a urine test.
In the rare event that your baby has this, you’ll know it very early on. Make sure your baby completely avoids milk to help stop vomiting and other symptoms.
Pyloric stenosis
Pyloric stenosis is a rare condition that happens when the opening between the stomach and intestines is blocked or too narrow. It can lead to forceful vomiting after feeding.
If your baby has pyloric stenosis, they may be hungry all the time. Other symptoms include:
Other symptoms include:
- dehydration
- weight loss
- wave-like stomach contractions
- constipation
- fewer bowel movements
- fewer wet diapers
This rare condition can be treated with surgery. Tell your pediatrician immediately if your baby has any of the symptoms of pyloric stenosis.
Intussusception
Intussusception is a rare intestinal condition. It affects 1 in every 1,200 babies and most commonly happens at the age of 3 months or older. Intussusception can cause vomiting without a fever.
This condition happens when the intestines are damaged by a virus or other health conditions. The damaged intestine slips — “telescopes” — into another part of the intestine.
Along with vomiting, a baby may have severe stomach cramps that last for about 15 minutes. The pain can cause some babies to curl their knees up to their chest.
Other symptoms of this intestinal condition include:
- fatigue and tiredness
- nausea
- blood or mucus in bowel movements
If your baby has intussusception, treatment can push the intestine back into place. This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
See your baby’s pediatrician if your baby has vomiting for longer than 12 hours. Babies can get dehydrated quickly if they’re vomiting.
Get immediate medical attention if your baby is vomiting and has other symptoms and signs like:
- diarrhea
- pain or discomfort
- constant or forceful coughing
- hasn’t had a wet diaper for 3 to 6 hours
- refusing to feed
- dry lips or tongue
- few or no tears when crying
- extra tired or sleepy
- weakness or floppy
- won’t smile
- swollen or bloated stomach
- blood in diarrhea
Baby vomiting without a fever can happen because of several common illnesses. Your baby will likely have one or more of these several times in the first year. Most of these causes go away on their own, and your little one will stop vomiting without any treatment.
But too much vomiting can lead to dehydration. Check for signs of dehydration and call your pediatrician if you’re not sure.
Some causes of baby vomiting are more serious, but these are rare. Your baby will need medical care for these health conditions. Know the signs and remember to keep the doctor’s number saved in your phone — and take a deep breath. You and baby got this.
Why Is My Child Throwing Up With No Fever? Nausea and Vomiting, Age 11 and Younger
Written by WebMD Editorial Contributors
In this Article
- Stomach Flu
- Food Allergy
- Food Poisoning
- Intestinal Obstruction
- Concussion
- Medications
- Motion Sickness
- Migraines
- Stress
Throwing up is no fun for kids. But it can worry you, too. A kid who’s vomiting but doesn’t have a fever could be dealing with any number of things. Knowing what else to look for can help you narrow down the reasons for your child’s upset stomach --and get their the treatment they need.
Stomach Flu
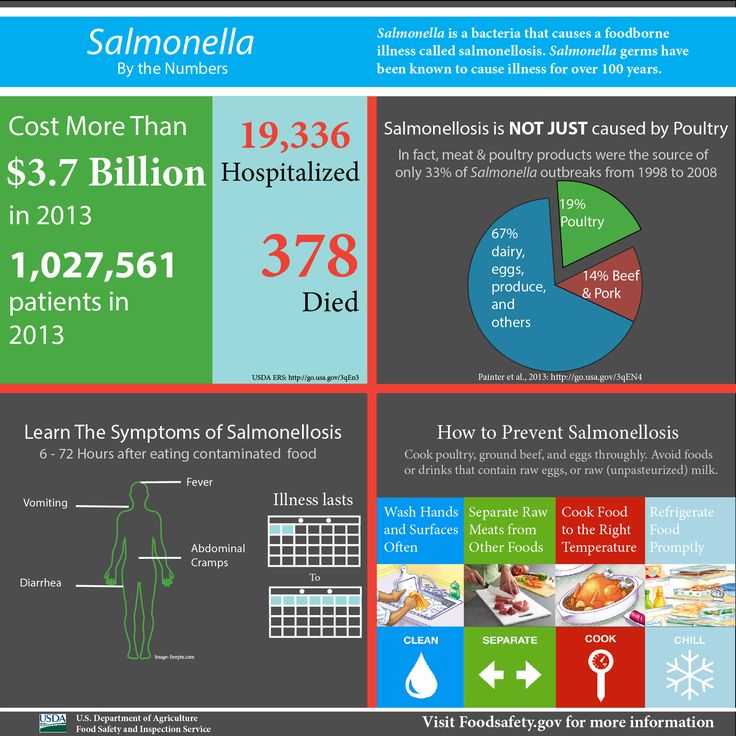
This isn’t the same as influenza (the flu). It’s the term people use when they’re talking about an illness called gastroenteritis. Most of the time, gastroenteritis is caused by a virus like rotavirus or norovirus. But you can also get it from bacteria like E. coli or salmonella. Although norovirus can sometimes cause a low-grade fever, you can also have it with no fever at all.
Norovirus is contagious like all viruses. If your child has it, they got it in one of three ways:
- They came into contact with someone who has it.
- They ate food that had the virus in it.
- They touched a surface with the virus on it, then touched their mouth or nose before washing their hands.
Symptoms start 12–48 hours after your child gets the virus. Along with throwing up, they’ll probably also have diarrhea, nausea, and stomach cramps.
Most kids get better within 1 to 3 days, but symptoms may last 7-10 days longer.
Food Allergy
Sometimes throwing up is a sign your child is allergic to food they’ve eaten. Throwing up may be their only symptom, but there could also be others, like trouble breathing, hives, repetitive cough, wheezing, or trouble swallowing. Nine out of 10 allergic reactions are linked to the following foods:
Throwing up may be their only symptom, but there could also be others, like trouble breathing, hives, repetitive cough, wheezing, or trouble swallowing. Nine out of 10 allergic reactions are linked to the following foods:
- Peanuts
- Tree nuts (almonds or walnuts, for example)
- Fish
- Shellfish (shrimp, for example)
- Eggs
- Milk
- Wheat
- Soy
Very young babies who try milk, soy, certain grains, and some other solid foods for the first time are at risk for something called “food protein-induced enterocolitis syndrome” (FPIES). It shows up 2 to 6 hours after they eat and makes them throw up many times. They may also have bloody diarrhea or stools flecked with blood. Take your child to the doctor right away if you suspect they have FPIES.
Food Poisoning
Anytime germs hitch a ride on food your kids eat, there’s a chance they could get a food-borne illness (food poisoning). Some of the bacteria that usually hide in food are:
- Salmonella
- Listeria
- Campylobacter
- E.
 coli
coli
You can get food poisoning from almost any food, especially if it hasn’t been cooked or stored correctly. The most common culprits are:
- Meat
- Poultry
- Eggs
- Shellfish
- Unwashed vegetables, like lettuce
Your child might start throwing up within a couple of hours of eating contaminated food. Sometimes it can take a day or two for symptoms to show up. Usually, your child will also have nausea, watery diarrhea, and stomach pain.
It’s possible for food poisoning to cause fever, but it’s common for it to cause throwing up with no fever, too. Symptoms can last anywhere from a couple of hours to several days.
Intestinal Obstruction
In newborns, it can be hard to tell whether they're throwing up or spitting up. Vomit usually comes out with more force than spit-up. Spit-up also tends to be linked to feeding and usually occurs shortly afterwards. Your doctor can help you figure out which one you’re dealing with.
Forceful throwing up in babies is rare, but when it happens, it can be a sign of a blockage in your baby’s intestines. It’s also possible that your little one could have what doctors call “pyloric stenosis.” That means their stomach is too narrow for food to pass through. Both of these are serious problems you should see a doctor about right away.
Concussion
Kids hit their heads a lot -- especially when they’re learning to walk or if they play sports. Anytime your child gets a head injury, it’s important to watch for signs of a concussion. Throwing up is one of these signs. Others include:
- Losing consciousness
- Headache
- Blurred vision
- Trouble walking
- Confusion
- Slurred speech
- Trouble waking up
Throwing up and other symptoms may not show up until 24 to 72 hours after your child hits their head.
Seek medical attention immediately if vomiting occurs after your child sustains a head injury.
Medications
If your child takes certain medications on an empty stomach, it can make them throw up. Sometimes, vomiting is a sign you’ve given your child too much of certain medications. The most common meds that cause this are:
Sometimes, vomiting is a sign you’ve given your child too much of certain medications. The most common meds that cause this are:
- Codeine
- Erythromycin
- Some birth control pills
- Some asthma medications, like theophylline
- Iron
- Acetaminophen
- Ibuprofen
Motion Sickness
When your child’s brain gets mixed signals about how they're moving, it can make them feel sick enough to vomit. For example, some kids might feel sick just watching a movie -- their eyes see motion, but their body doesn’t feel motion. Carsickness is common in kids who are too small to see out the car window.
Motion sickness usually starts with a tummy ache or a queasy feeling. Some kids may also sweat, lose their appetite, and not want to eat. Eventually, throwing up starts. It’s a genetic condition. Your child is more likely to have motion sickness if one of their parents did.
Migraines
About 10% of school-age children deal with migraines. These headaches can happen in kids as young as 18 months old. They cause head pain, but it’s also common for a migraine to make your child throw up. In addition, your child may have:
These headaches can happen in kids as young as 18 months old. They cause head pain, but it’s also common for a migraine to make your child throw up. In addition, your child may have:
- Dizziness
- Nausea
- Sensitivity to touch, sound, and odors
Experts aren’t clear what causes migraines. It could be caused by something your child is around a lot. It’s also genetic: If one parent has migraines, your child has a 50% chance of getting them. If both their parents have migraines, their chance of getting them goes up to 75%.
if your child has a headache, fever, and vomiting, consult their doctor.
Stress
It’s true -- some kids throw up when they’re stressed. It may be because some other health problem, such as an ear infection, is bothering them. Or your child might throw up after crying for a long time. A good way to tell if the throwing up is stress-related is if it happens only once or twice and they don't have any other symptoms like stomach pain or diarrhea.
Children's Health Guide
- The Basics
- Childhood Symptoms
- Common Problems
- Chronic Conditions
Regurgitation and vomiting in children
Regurgitation syndrome is one of the most common reasons for parents of young children to visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i. e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc. nine0003
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes. nine0003
The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes. nine0003
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life. nine0003
This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life. nine0003
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
nine0003
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical. nine0003
Experienced pediatricians and surgeons are on duty around the clock at the EMC Children's Clinic, providing emergency and planned care to children of all ages, starting from the first days of life.
If surgical treatment is required, the method of choice in our clinic is minimally invasive endoscopic surgery, which in most cases allows the child to go home on the day of the operation. The operation is accompanied by an experienced anesthesiologist, who individually selects modern and safe anesthesia for each child. Postoperative wards are equipped with high-tech equipment, where round-the-clock monitoring systems are installed, and a separate nurse continuously monitors the condition of small patients. nine0003
In the comfortable hospital of the EMC Children's Clinic, parents can stay with their child all the time, round-the-clock visits are open for relatives and friends, which ensures maximum comfort for the child and parents.
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes: nine0003
The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes: nine0003
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body. nine0003
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile. nine0003
In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile. nine0003
What explains physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation.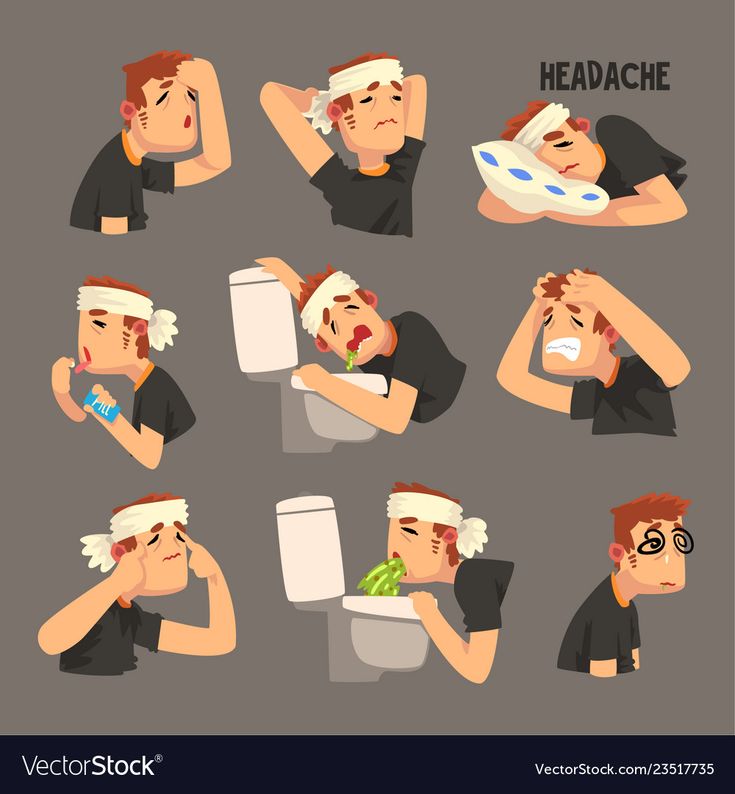 These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation. nine0003
These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation. nine0003
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled. nine0003
-
Swallowing air during feeding (aerophagia). A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk.
 Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. nine0003
Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. nine0003 -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up. nine0003
Abnormal regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
nine0042 -
increased intracranial pressure.

Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year. nine0003
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
nine0042
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air.
 Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again. nine0003
Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again. nine0003 -
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency. nine0003
-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.