Baby turns blue while feeding
Blue Clues: Common Causes of Neonatal Cyanosis
You go down the hall to see a term infant who is now 2 weeks old. The triage nurse said the baby looks fine to her and the vitals are normal for age, including the oxygen saturation, which is 98% on room air. The mother is quite concerned, however. She says that with feeding she’s noticed that the baby turned blue around the lips today. She noticed this several times and thought she’d bring the child in to be evaluated. The infant is feeding well and behaving normally for age. She’s an avid bottle feeder and is gaining weight. She doesn’t sweat during feeds or seem to tire out. She has not yet had her first well-baby check, but was examined in the newborn nursery and there were no concerns.
You examine the infant and she looks fine. But what about the peri-oral cyanosis during feeds, should you be worried about it?
You know that some congenital heart disease is sneaky – the infant won’t always have a heart murmur in the neonatal period. Parents may not always notice cyanosis at rest, but may appreciate it with increased activity, such as vigorous crying or feeding. You decide to place the child on a pulse oximeter and observe a feeding.
ADVERTISEMENT
There’s no problem getting the baby to feed. She latches onto the nipple like a barracuda. As she is vigorously sucking away, the mother points out to you a slight bluish discoloration around the lips. It’s there all right, but the pulse oximeter remains in the upper 90’s. Furthermore, you notice (and point out to the mother), that the lips and tongue remain pink, not blue.
So what’s going on? Babies have a venous plexus around the mouth that can engorge with blood during feeds, producing a faint blue appearance. This can be differentiated from true, central cyanosis, as the lips and tongue remain pink. It is completely normal and benign and all that’s needed here is reassurance.
Another benign cyanosis phenomenon in neonates: the ever-famous acrocyanosis, or blue hands and/or feet that occur in newborns when they are cold and that disappears with warming. You can get a falsely low pulse oximeter reading if you wrap it around a cold blue toe. Sometimes all that is needed to resolve “hypoxia” is to move the pulse ox probe from a cold toe to a warm finger.
You can get a falsely low pulse oximeter reading if you wrap it around a cold blue toe. Sometimes all that is needed to resolve “hypoxia” is to move the pulse ox probe from a cold toe to a warm finger.
ADVERTISEMENT
Case 2
You know you’re in for trouble by the look on the charge nurse’s face. He’s just put an infant in room 3 and wants you to come see it “right now.” As you motor down the hall he tells you that the baby is just 4 days old, is breathing fast and is blue. Oxygen sats range from the upper 70’s to the low 80s.
You get to the room and see an alert infant who is looking at you while working on a pacifier. The child appears dusky all over. The respiratory rate is 76. The child has minimal retractions but no flaring. He is not grunting. As you are sizing this up the nurse puts the child on 100% oxygen and is starting a line.
Ok, tachypneic and blue at 4 days of age. The two most likely causes of this condition are lung disease or congenital heart disease. So which is it? As if reading your mind, the nurse tells you he didn’t hear a murmur.
So which is it? As if reading your mind, the nurse tells you he didn’t hear a murmur.
No heart murmur, does that mean it’s a pulmonary problem? Not necessarily. You examine the infant and confirm that the nurse is right about the heart exam. There is no heart murmur. The lungs sound clear. The capillary refill is 3 seconds peripherally and the pulses are present, but weak.
ADVERTISEMENT
This infant has cyanotic congenital heart disease. In many cases, such as transposition of the great arteries and pulmonary atresia, there is no murmur. Infants with cyanotic congenital heart disease can be pink early on but dependent on flow through the patent ductus arteriosis to allow oxygenated blood into the systemic circulation. As the ductus begins to close, they can develop hypoxemia and/or shock. One key to recognizing this scenario is that these babies don’t appear to be working as hard to breath as do babies with lung disease. Another key observation is the response to 100% oxygen. Infants with pulmonary disease will usually raise their PO2 above 100 mm Hg on 100% inspired oxygen. The PO2 will remain well below that despite 100% oxygen in infants with cyanotic heart disease. An EKG may or may not be helpful. A CXR in pneumonia is typically going to show busy lung fields, suggesting infiltrates, whereas the blue baby who has inadequate pulmonary blood flow will have clear lungs or diminished pulmonary markings.
Infants with pulmonary disease will usually raise their PO2 above 100 mm Hg on 100% inspired oxygen. The PO2 will remain well below that despite 100% oxygen in infants with cyanotic heart disease. An EKG may or may not be helpful. A CXR in pneumonia is typically going to show busy lung fields, suggesting infiltrates, whereas the blue baby who has inadequate pulmonary blood flow will have clear lungs or diminished pulmonary markings.
What to do? Manage the ABCs like you always do but get this infant on a prostaglandin E drip while you wait for the Cardiologist.
Case 3
The nurse alerts you to a baby that needs “your immediate attention.” The infant is 3 weeks old and was noted by the mother to be blue today.
You walk in and see an infant that does not appear to be in distress. He is alert and vigorous but has a definite bluish hue. The vitals are unremarkable and the pulse oximeter reading is in the normal range. A quick assessment shows a normal heart and lung exam and great peripheral perfusion. You place the infant on 100% oxygen and the cyanosis doesn’t change at all. Ok, this kid looks too good to have pulmonary or cardiac disease, why is he blue? And what’s with the pulse ox?
You place the infant on 100% oxygen and the cyanosis doesn’t change at all. Ok, this kid looks too good to have pulmonary or cardiac disease, why is he blue? And what’s with the pulse ox?
You get a rapid history from the worried mother. The baby was full term and has been healthy so far, feeding well and gaining weight. The 2-week well-baby check raised no concerns. The baby was first noted to be a bit off color yesterday but the mother thought it might just be a trick of the lighting. He seemed to behave normally. This morning he definitely seemed blue to mom so she rushed him here. He’s had no fevers, no respiratory symptoms, no diarrhea or vomiting. In fact, if it weren’t for his color she wouldn’t be here.
So what’s going on? Does the pulse ox help? Is it even working? After all, it’s reading in the normal range and this kid is blue. Thinking this through, you remember that the pulse oximeter is designed to measure the oxygen saturation of hemoglobin that is available to bind oxygen. Abnormal hemoglobin that is not available to be saturated with oxygen may not be measured. So a child with an abnormal form of hemoglobin may be blue while the pulse oximeter reading is in the normal range.
Abnormal hemoglobin that is not available to be saturated with oxygen may not be measured. So a child with an abnormal form of hemoglobin may be blue while the pulse oximeter reading is in the normal range.
So what hemoglobin is a possible candidate? One form of hemoglobin that can produce cyanosis in babies is methemoglobin. Methemoglobin results from a higher-than-usual proportion of heme iron in the ferric rather than ferrous state. There’s a congenital form of this, but the majority of cases are due to toxin exposure. Severe diarrhea and acidosis can cause this as well, but this baby hasn’t had any of that. No, toxin exposure is the most likely. There’s a list of possible toxins that cause this. One, you remember, is nitrates that are sometimes found in well water. Young infants are particularly susceptible to this as the enzyme systems that keep their heme iron in its proper state are not yet mature. You ask mom about well water and hit pay-dirt: The family just moved into a house with a well and the mother has been using the well water to mix the baby’s formula.
Fortunately, this baby doesn’t look too bad. You send some blood to the lab to get the methemoglobin level measured. You notice that the blood is somewhat chocolate-colored in appearance. Sure enough, the lab calls back to confirm your suspicion. The child’s methemoglobin level is 25%, enough to cause cyanosis but not enough to cause problems. When the methemoglobin level is less than 30% and symptoms are mild, removal of the toxin is all that’s needed, normal red cell metabolism will take care of the problem in a few hours. Levels higher than 30% will produce increasingly severe symptoms, from dyspnea and tachycardia to lethargy, obtundation and even death. Infants with significant symptoms should receive 1-2 mg/kg methylene blue, which can be repeated in one hour if symptoms remain. Infants with high levels and severe symptoms that fail to respond to methylene blue may require exchange transfusion or hyperbaric oxygen therapy.
These are just some of the many causes of cyanosis in newborns. Think abnormal hemoglobin saturation, abnormal hemoglobin, or poor circulation as the three main pathways to blue. Make sure it’s true, central cyanosis before you get too worked up about it. Response to oxygen administration can be very helpful in sorting things out.
Think abnormal hemoglobin saturation, abnormal hemoglobin, or poor circulation as the three main pathways to blue. Make sure it’s true, central cyanosis before you get too worked up about it. Response to oxygen administration can be very helpful in sorting things out.
Blue baby syndrome: Causes, symptoms, and treatments
Blue baby syndrome, also known as infant methemoglobinemia, is a condition where a baby’s skin turns blue. This occurs due to a decreased amount of hemoglobin in the baby’s blood.
Hemoglobin is a blood protein that is responsible for carrying oxygen around the body and delivering it to the different cells and tissues.
When the blood is unable to carry oxygen around the body, the baby turns blue (cyanotic).
Blue baby syndrome is rare in industrialized countries, but it does occasionally occur in rural areas. Babies born in developing countries with poor water supply continue to be at risk for the condition.
Share on PinterestBlue baby syndrome is not common in industrialized countries.
The most common cause of blue baby syndrome is water contaminated with nitrates.
After a baby drinks formula made with nitrate-rich water, the body converts the nitrates into nitrites. These nitrites bind to the hemoglobin in the body, forming methemoglobin, which is unable to carry oxygen.
Nitrates are most common in drinking water in farming communities that use well water. This contamination is due to the use of fertilizers and manure.
Infants younger than 3 months are at highest risk for blue baby syndrome, but it can also occur in other populations.
People at risk for methemoglobinemia include adults with:
- a genetic predisposition
- ulcers or gastritis
- kidney failure requiring dialysis
Other conditions that can cause a baby to appear blue include:
- Tetralogy of Fallot (TOF): TOF is a serious congenital heart condition causing four structural abnormalities in the heart that lead to a lack of oxygen in the blood.
 This condition can cause a baby to look blue, though it usually occurs at birth.
This condition can cause a baby to look blue, though it usually occurs at birth. - Other congenital heart abnormalities: Any congenital heart abnormality that affects the amount of oxygen in a baby’s blood can cause their skin to turn blue.
- Methemoglobinemia: This is due to exposure to inhaled nitric oxide, or certain anesthetics and antibiotics.
The most common symptom of blue baby syndrome is a blue discoloration of the skin around the mouth, hands, and feet. This is also known as cyanosis and is a sign that the child or person is not getting enough oxygen.
Other potential symptoms of blue baby syndrome include:
- difficulty breathing
- vomiting
- diarrhea
- lethargy
- increased salivation
- loss of consciousness
- seizures
In severe cases, blue baby syndrome can even cause death.
Share on PinterestA doctor may request a blood test to diagnose blue baby syndrome.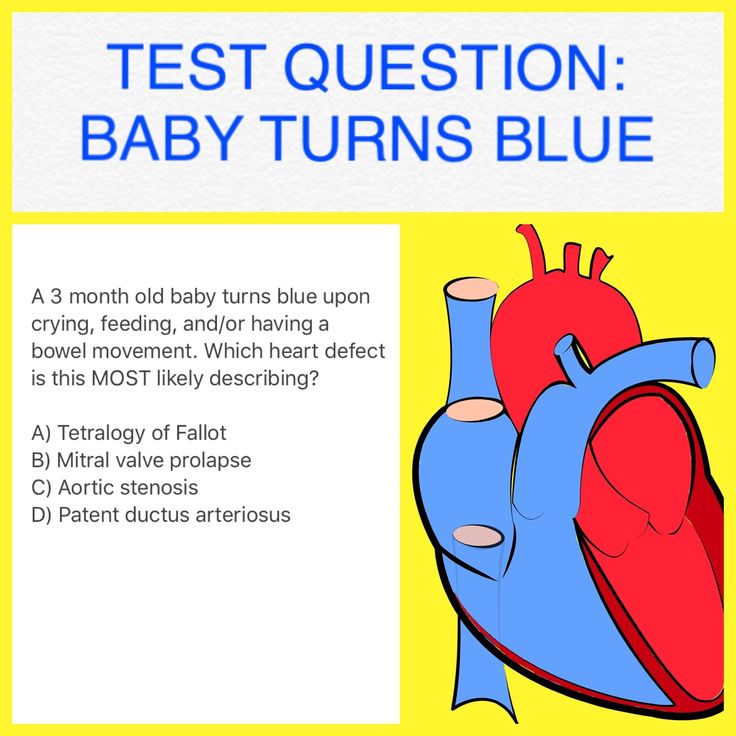
A doctor may suspect that an infant has blue baby syndrome during a regular checkup. Parents or caregivers who notice a bluish discoloration should schedule an appointment with a doctor.
The doctor will begin the diagnosis by taking a thorough medical history by asking about any symptoms, feeding patterns, and the conditions at home. They will then perform a physical exam, looking at the discolored areas discoloration and listening to the heart and lungs.
Additional diagnostic tests may include:
- blood tests
- chest X-rays to look at the lungs and heart
- echocardiogram to look at the heart and how well it functions
- oxygen saturation to determine how much oxygen is in the blood
- cardiac catheterization to directly look at the blood vessels and structures inside the heart
In addition to testing the baby, it is possible to get the tap water tested to measure the nitrate levels.
In general, water with nitrate levels below 10miligrams per liter (mg/L) is considered safe. If a water sample has nitrate levels above 10mg/L, do not give it to an infant.
If a water sample has nitrate levels above 10mg/L, do not give it to an infant.
Treatment will vary depending on what is causing the baby to turn blue. If congenital heart disease is causing the discoloration, surgery may be required to correct the abnormalities.
A surgeon will usually operate before the baby turns 1 year old, ideally at around 6 months of age, or even a little earlier. Successful surgery means that the baby will start to get more oxygen and will no longer look blue.
If high nitrate levels in the water are causing blue baby syndrome, the doctor will likely need to consult with the local poison control center or toxicologist to help figure out the best way to treat the condition.
Avoiding the source of nitrate contamination, such as well water or tap water, is essential for all children with this condition.
Doctors may monitor children with a mild form of blue baby syndrome to make sure that they do not develop any further health problems as a result of the condition.
Children with a more severe form of the condition may need a medication called methylene blue, which a doctor will give as an injection.
Blue baby syndrome is a rare condition that occurs when infants drink formula that has been made with water contaminated by high levels of nitrates.
For this reason, it is essential to avoid giving infants water from a well until they turn at least 1 year of age. Medication and monitoring the baby can usually prevent any complications. Left untreated, however, blue baby syndrome can be life-threatening.
Most children with blue baby syndrome go on to live a normal and healthy life without lasting health complications.
How to get rid of sleep apnea while feeding a baby?
Home→Articles → Patients→Topical topics→Apnea while feeding a baby: how to make the baby breathe normally?
Apnea is the most common breathing control problem in infants. There are many reasons for this state of affairs. Most often, the nervous system or pathological diseases are not sufficiently formed.
New mothers often complain that the baby stops breathing during feeding. Moreover, when breastfeeding, this happens much less often than when feeding from a bottle. When the baby eats with "greed", begins to choke, the breath disappears, then he turns blue, clears his throat in a moment and continues to eat.
The simplest thing pediatricians advise is bottle feeding in a position close to vertical. The head should be slightly tilted forward. In this position, the chances of choking are much less. Also:
- The bottle can be taken out periodically to let the baby catch his breath.
- To avoid problems with breathing, it is recommended to feed in a crib on your side.
What causes such apnea, the treatment of which also requires a serious approach? Doctors in most cases attribute this to prematurity. The shorter the gestation period, the more frequent the occurrence of apnea during feeding. In addition, more children with low weight suffer from this disease.
Apnea during feeding of a premature baby
There are many reasons for such apnea. Premature babies, as a rule, have an immature respiratory center, which means that the mechanism that regulates breathing is imperfect. As for the feeding reflexes, we are talking about swallowing, sucking, they are also not quite active. Their activities are poorly coordinated.
In addition, in premature babies, the work of the muscle fibers of the soft palate, as well as nearby tissues, is disrupted. They sag when feeding on the back and apnea is clearly manifested. When feeding on the side, the baby suffers less from breathing problems, or there are no problems at all.
This is important!
Statistics show that babies born before 29 weeks can suffer from apnea during feeding in 80% of cases, half of babies born at 30-31 weeks and 10% of babies born after 32 weeks .
The baby may choke on milk with strong pressure. If the baby is breastfed, you can first express a little milk, and if he is bottle-fed, reducing the hole in the nipple helps.
What should a mother do if her baby has an apnea attack? First, stop feeding and try to "stir up" the child. If at the same time breathing is not restored, then you need to do artificial respiration.
In severe cases, go to chest compressions. For such young children, it is done by means of the thumbs, placing the rest of the fingers on the back of the child. Pushes should be carried out often, after every 5 pushes, mouth-to-mouth breathing should be done.
Remember that feeding apnea requires systematic medical prevention of seizures. To do this, oxygen is given to a premature baby before and after feeding. And, of course, in case of apnea in infants, it is always worth consulting a doctor once again.
You might be interested
Local irritation of the skin from the mask, especially in the back of the nose
Choosing orthopedic pillows for sleeping: which ones are better?
You can forget about snoring forever! What do experts advise?
The main types of oxygen concentrators
Blue nasolabial triangle - causes, threats, what to do?
Blue nasolabial triangle.
Very often, parents turn to a pediatrician with complaints of blue around the lips or, as it would be more correct to say, cyanosis of the nasolabial triangle. What is it and is it worth worrying about this issue, we will now consider with you.
The nasolabial triangle is an area on the face bounded by the nasolabial folds on the sides, the nose above and the lips below. Cyanosis can be caused by physiological (i.e., occur in absolutely healthy babies) and pathological (with various diseases) conditions of the body.
Physiological states .
In the region of the nasolabial triangle, the blood supply is highly developed: both arterial and venous vessels are present. And the skin of infants and young children is very thin and delicate, so the vascular plexuses seem to “shine through” through it and it seems bluish.
Crying baby . Sometimes mothers note that cyanosis appears when crying or crying for a long time. This is due to the peculiarity of the pulmonary system in newborns. At this time, the level of oxygen in the body decreases (its amount can drop to 92%), and the capillaries expand from tension and therefore are clearly visible through thin skin. In medicine, this phenomenon is called pulmonary cyanosis, and does not pose any threat to health. It disappears when the baby calms down. As the child grows older and the lung function improves, this symptom disappears.
This is due to the peculiarity of the pulmonary system in newborns. At this time, the level of oxygen in the body decreases (its amount can drop to 92%), and the capillaries expand from tension and therefore are clearly visible through thin skin. In medicine, this phenomenon is called pulmonary cyanosis, and does not pose any threat to health. It disappears when the baby calms down. As the child grows older and the lung function improves, this symptom disappears.
Feeding. Breast sucking is a big load for the baby, in which capillaries appear and become noticeable at the surface of the skin. After feeding, the blue immediately disappears.
Low air temperature . When the baby is cold, some parts of the body, including the nasolabial triangle, may turn blue. This is due to the imperfect heat exchange system of the child's body. As soon as the baby warms up, the skin will take on a natural color. The same thing happens while walking. If you notice a blue nasolabial triangle, it's time to leave the street, because this may be the first sign of a child's hypothermia.
If you notice a blue nasolabial triangle, it's time to leave the street, because this may be the first sign of a child's hypothermia.
We examined with you the physiological conditions of cyanosis of the nasolabial triangle in children, not associated with the manifestation of any diseases. What pathological conditions can lead to the appearance of this symptom?
Pathological conditions.
Respiratory diseases. Respiratory diseases that can lead to cyanosis of the nasolabial triangle include SARS, pneumonia, bronchial asthma, obstructive or allergic bronchitis, that is, those that lead to impaired air exchange. Of course, along with cyanosis, other symptoms of these diseases should also be present (fever, nasal discharge, prolonged dry cough). In this case, you cannot do without consulting a pediatrician, who, in turn, can refer you to other narrow specialists.
Foreign objects. This is another common cause of cyanosis of the nasolabial triangle.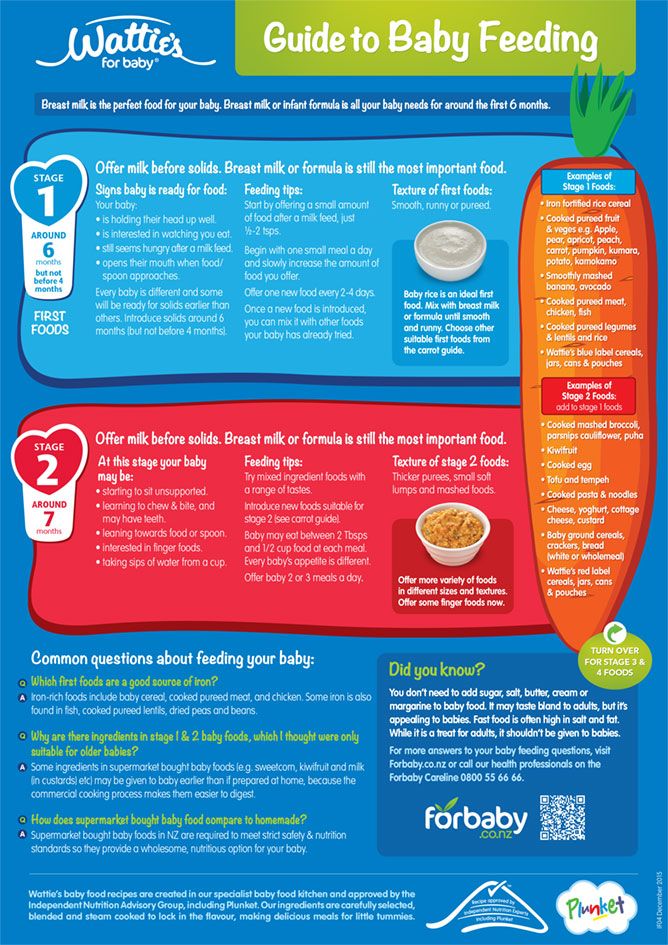 Young children are very curious. Taste buds are best developed in them, and therefore they learn the whole world through their mouths. Everything they are interested in is in the mouth - one careless breath and a tiny object enters the respiratory tract. The child begins to cough strongly, greedily grab air with his mouth. It is necessary to provide first aid and call an ambulance.
Young children are very curious. Taste buds are best developed in them, and therefore they learn the whole world through their mouths. Everything they are interested in is in the mouth - one careless breath and a tiny object enters the respiratory tract. The child begins to cough strongly, greedily grab air with his mouth. It is necessary to provide first aid and call an ambulance.
First aid for foreign bodies in the respiratory tract : Turn the child face down and with force, but not excessive, tap on the back. It is better to carry out manipulations over a sofa or chair so that the baby does not fall to the floor, accidentally slipping out of your hands.
The second option. Sit in a chair or chair. Place the baby on the left knee face down. Your left hand should be on his chest and hold his neck. With your right hand, carry out strong pushes with the edge of the palm between the shoulder blades towards the mouth. Additionally, induce vomiting in the child by pressing your fingers on the root of the tongue. Follow all the steps until the ambulance arrives.
Follow all the steps until the ambulance arrives.
Neurological pathology. Very often, cyanosis can be observed in children who experienced hypoxia or asphyxia at the time of birth (for example, when entangled with the umbilical cord), and were also born prematurely. We see the blue nasolabial triangle in babies with increased intracranial pressure, with immaturity of brain structures. In any case, a consultation with a neurologist is necessary.
Congenital heart defects . Cyanosis of the nasolabial triangle in a child is one of the first signs of congenital heart disease and heart failure. To clarify the diagnosis and timely treatment, it is necessary to conduct EchoCG (ultrasound of the heart), ECG and consult a cardiologist.
Problems with the development of the respiratory system. Malformations of the broncho-pulmonary system (tracheal stenosis, bronchial hypoplasia, etc.) can also lead to cyanosis of the nasolabial triangle. Such conditions require urgent treatment.
Such conditions require urgent treatment.
Poisoning by drugs or chemicals. Poisoning causes tissue hypoxia, which is manifested by a violation of the absorption of oxygen by cells, hence the cyanosis of the nasolabial triangle. Also, cyanosis will be observed in children in whose presence their parents smoke, as a consequence of nicotine intoxication.
If the doctor, having examined the baby, did not find any pathologies and recognized the cyanosis of the nasolabial triangle as the norm, the following measures should be taken so that the blue disappears as soon as possible.
Be sure to walk with your child outdoors every day. Long walks will not only harden the baby's body, but also saturate it with oxygen. And if there is no lack of it, then the nasolabial triangle will not turn blue.
Don't let your baby cry for a long time. This is harmful not only for physical health, but also for the emotional comfort of the child. Crying is a form of appeal to the mother that is accessible to the baby.