Baby twitching when feeding
Infantile Spasms: Symptoms, Causes & Treatment
Watching your baby's every movement typically brings parents so much joy. But when a baby shows signs and symptoms of a serious neurological condition such as infantile spasms (IS), that joy can quickly turn into concern.
Infantile spasms are little seizures with big consequences. Early recognition leads to better outcomes; waiting to seek treatment can increase your baby's risk of permanent brain injury.
What are infantile spasms?
Infantile spasms, first described with a group of symptoms known as West syndrome, is a form of epilepsy that occurs in 1 in 2,000 children. It typically begins between 2-12 months of age and peaks between 4-8 months of age.
What do infantile spasms look like?
While these seizures may last only a second or two, they often happen close together with each spasm occurring every 5-10 seconds in a series. During a spasm, the body stiffens suddenly, the back may arch, and the arms, legs, and head may bend forward. However, infantile spasms can sometimes be hard to notice—perhaps only the eyes roll up or there is a small tummy crunch. They are most common just after a baby wakes up and rarely occur during sleep.
Parents and childcare providers, or anyone wanting to educate a friend or relative about infantile spasms: watch this video, below. We see a baby experiencing a cluster of individual spasms. Each spasm is less than 1 second; the child exhibits a look of surprise, a brief stare, and elevation/extension of both arms. In between each spasm, the baby appears to be fine—very typical of infantile spasms.
Early diagnosis is key
It is very important that infantile spasms are diagnosed early. If you suspect your baby may be having infantile spasms, talk to your pediatrician right away. Your child may need to be seen by a
pediatric neurologist. If you can, try to video any episodes of your baby having a spasm and show this to your child's doctors.
Your child may need to be seen by a
pediatric neurologist. If you can, try to video any episodes of your baby having a spasm and show this to your child's doctors.
You may be told to go to the emergency room so a pediatric neurologist can examine your child. Your child may have to be admitted to the hospital to have a test called video-electroencephalogram (EEG) monitoring. Video-EEG is needed to verify specific brain-wave patterns during the spasms and to document specific patterns in between the spasms. Pediatric neurologists look for a distinct EEG pattern called hypsarrhythmia. The seizures' appearance and EEG are so distinct that the diagnosis of infantile spasms can be made with certainty in most cases. Determining the cause of the spasms may be more difficult.
Causes of infantile spasms
There are many causes of infantile spasms; almost any brain abnormality or brain injury can cause them. More than 50 genetic/metabolic diseases are associated with infantile spasms, and many patients have other disorders that cause developmental delays (e. g.,
cerebral palsy,
Down syndrome, tuberous sclerosis, etc.) prior to the onset of the spasms.
g.,
cerebral palsy,
Down syndrome, tuberous sclerosis, etc.) prior to the onset of the spasms.
Determining the cause of infantile spasms is very important, because it affects treatment and prognosis.
Treatment options
The American Academy of Neurology and the Child Neurology Society recommend adrenocorticotropic hormone (ACTH) as the first line of therapy for infantile spasms. This medication is given as a shot. The first doses are given in the hospital so your child can be closely watched for any side effects. Since your child will need to continue to get ACTH shots for about 6 weeks, you will be instructed on how to give your child the injections at home. The goals for this medication are to
In some cases, pediatric neurologists prescribe the seizure medication vigabatrin. Both drugs work well, but your child's doctor will talk with you about which medicine may be the better choice for your child.
What is the outlook for children with infantile spasms?
Even if the infantile spasms stop, many children develop other kinds of epilepsy and have
intellectual or other
developmental disabilities later in life. If the treatment is prompt and successful, the outlook is brighter. Normal development is possible for those who were developing on track before the spasms started.
If the treatment is prompt and successful, the outlook is brighter. Normal development is possible for those who were developing on track before the spasms started.
More Information
What is a Child Neurologist?
Seizures and Epilepsy in Children
Is Your Baby's Physical Development on Track?
Infantile Spasms: What Research Is Being Done? (National Institute of Neurological Disorders and Stroke)
Editor's Note: The article was published in recognition of Infantile Spasms Awareness Week to help parents, as well as physicians and other health care providers, learn more about this disease and its treatments. Check out www.isweek.org for more info.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Infantile Spasms: Causes, Symptoms & Treatment
Overview
What are infantile spasms?
Infantile spasms (also called epileptic spasms) are a form of epilepsy that happen to babies typically under 12 months old. Epilepsy is a group of neurological disorders characterized by abnormal electrical discharges in your brain.
Infantile spasms look like brief tensing or jerking spells that involve your baby’s abdomen (belly), head, neck, arms and/or legs. The spasms last for one to two seconds and usually happen one after another (in a series or cluster) every five to 10 seconds. Infantile spasms most commonly occur after your baby awakes from sleep.
Babies affected by infantile spasms often already have or later have developmental delays or developmental regression.
If your baby is experiencing spasms, it’s important to see their healthcare provider as soon as possible.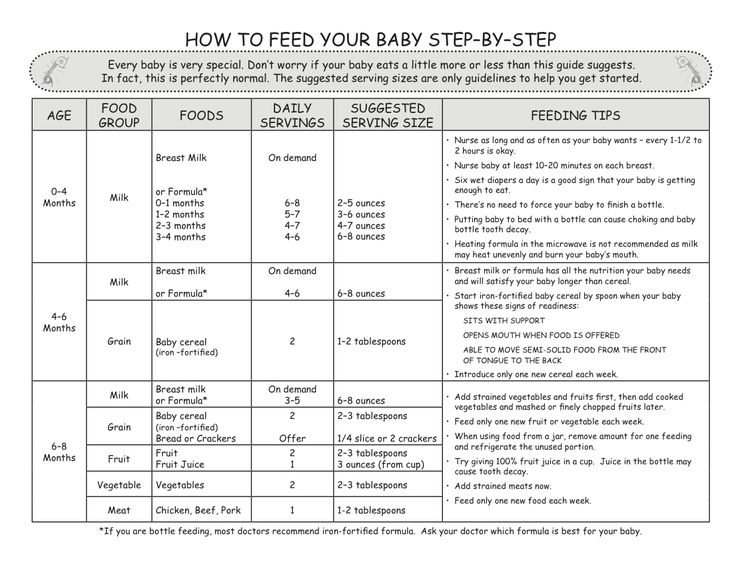 Early diagnosis and treatment are key.
Early diagnosis and treatment are key.
What’s the difference between infantile spasms and West syndrome?
West syndrome happens when your baby has a combination of symptoms, including:
- Infantile spasms.
- Abnormal brain wave patterns called hypsarrhythmia.
- Developmental delays or developmental regression.
While babies who’re affected by infantile spasms often have West syndrome, they can experience infantile spasms without having or later developing developmental delays.
What’s the difference between spasms and seizures?
Infantile spasms (also called epileptic spasms) are a type of seizure.
A seizure is a burst of uncontrolled electrical activity between brain cells that causes temporary abnormalities in muscle tone or movements, behaviors, sensations and/or states of awareness. Not all seizures are alike.
Spasms are typically shorter than what most people think of when they think of seizures — namely, a tonic-clonic (grand mal) seizure. Infantile spasms last around one to two seconds in a series; whereas other types of seizures can last from 30 seconds to two minutes.
Infantile spasms last around one to two seconds in a series; whereas other types of seizures can last from 30 seconds to two minutes.
What’s the difference between infantile spasms and the startle reflex?
While infantile spasms can look similar to a normal startle reflex in babies, they’re different.
The startle reflex (also called the Moro reflex) happens when a loud sound or sudden movement startles your baby. They typically throw their head back and extend their arms and legs with the palms of their hands facing upward. They may also cry and often pull their arms and legs back in.
This chart can help you tell the difference between infantile spasms and the startle reflex.
| Startle reflex | Infantile spasms | |
|---|---|---|
| Triggers | Loud noises, bright light or sudden movement. | Waking up from sleep is the most common trigger, but spasms can happen at any time during the day. |
| Frequency and timing | Happens once after a trigger and lasts a few seconds. | Often happen back-to-back or in clusters. Each spasm lasts for one to two seconds, but clusters can last for several minutes. |
| Age of occurrence | Most noticeable in newborns and slowly disappears by four to six months of age. | Often start occurring between the ages of three and 12 months and continue. |
At what age do infantile spasms start?
Healthcare providers diagnose infantile spasms in babies younger than 12 months of age in 90% of cases. The average age of diagnosis is between four and seven months of age.
When children who’re older than 12 months have spells resembling infantile spasms, they’re typically classified as epileptic spasms.
How common is this condition?
Infantile spasms affect approximately 1 in 2,000 to 4,000 babies.
Symptoms and Causes
What are the signs and symptoms of infantile spasms?
During an infantile spasm, your baby’s body will stiffen or tense up suddenly and only for a couple of seconds. They may also arch their back, and their arms, legs and/or head may bend forward. Infantile spasms often happen one after another in a cluster with five- to 10-second pauses in between spasms.
They may also arch their back, and their arms, legs and/or head may bend forward. Infantile spasms often happen one after another in a cluster with five- to 10-second pauses in between spasms.
After a spasm or series of spasms, your baby may appear upset or cry — but not always.
In some cases, infantile spasms are very subtle and difficult to notice. Subtle signs of an infantile spasm include:
- Eyes rolling up.
- Belly tensing up.
- Chin movements.
- Grimacing.
- Head nodding.
Spasms that are due to an abnormality in your baby’s brain often affect one side of their body more than the other or may result in pulling of their head or eyes to one side.
Infantile spasms are most common just after your baby wakes up and rarely happen while they’re sleeping.
Soon after your baby starts experiencing spasms, you’ll likely notice other changes in your baby, including:
- Loss of developmental milestones they had previously reached, such as rolling over, sitting, crawling and babbling.

- Loss of social interactions and smiling less.
- Increased fussiness or silence.
If you can, try to take videos of your child’s spasms so you can show them to their pediatrician. It’s very important that infantile spasms are diagnosed early. If you think your baby may be having infantile spasms, talk to their pediatrician as soon as possible.
How often do infantile spasms occur?
A baby can have as many as 100 spasms a day. Each baby is affected differently, so if you notice your baby having spasms — even if it’s once or twice a day — it’s important to talk to their pediatrician as soon as possible.
What causes infantile spasms?
There are several causes of infantile spasms. Scientists have listed over 200 different health conditions as possible causes of infantile spasms. But in about one-third of cases, healthcare providers can’t determine the cause.
An infantile spasm may happen due to an abnormality in a small portion of your child’s brain or may be due to a more generalized brain issue.
Possible causes of infantile spasms include:
- Brain injuries or infections: Almost any type of brain injury can cause infantile spasms. The most common causes include hypoxic ischemic encephalopathy (when your brain doesn’t get enough oxygen or blood flow for a period of time), meningitis and perinatal stroke (a stroke that happens to your baby anytime between the middle of pregnancy and the first month of their life).
- Issues with brain development: Several central nervous system (brain and spinal cord) malformations that occur while your baby is developing in the womb can cause infantile spasms. These can include focal cortical dysplasia, lissencephaly, holoprosencephaly and Aicardi syndrome. Abnormal blood vessels in your baby’s brain (arteriovenous malformations) can also cause infantile spasms.
- Gene mutations: Scientists are linking more and more gene mutations (changes) to infantile spasms. Some of these include trisomy 21 (Down syndrome), tuberous sclerosis, Miller-Dieker syndrome and CDKL5 deficiency disorder.
- Metabolic conditions: Inborn errors of metabolism (IEM) can cause infantile spasms. They’re genetic conditions that block metabolic pathways involved in the breakdown of nutrients you eat and the generation of energy. In rare cases, vitamin B6 deficiency also causes infantile spasms.
Diagnosis and Tests
How are infantile spasms diagnosed?
Your child’s healthcare provider will ask detailed questions about your child’s symptoms and medical history. They’ll also perform a physical exam.
Your child may have to see a pediatric neurologist or pediatric epileptologist. They’ll order a test called an electroencephalogram (EEG) to confirm the diagnosis of infantile spasms and other tests to find the cause.
Since there are hundreds of possible causes of infantile spasms, it can be more difficult for healthcare providers to identify the cause.
What tests will be done to diagnose infantile spasms?
Your child’s healthcare provider will order an electroencephalogram (EEG) to confirm the diagnosis of infantile spasms.
An EEG measures and records your child’s brain’s electrical signals. During an EEG, a technician places small metal disks (electrodes) on your child’s scalp. The electrodes attach to a machine that gives your baby’s healthcare provider information about your child’s brain activity. Ideally, the EEG will capture their brain’s activity while they’re having a spasm, as well as the time in between spasms. Healthcare providers look for a distinct EEG pattern called hypsarrhythmia. This pattern is very particular and makes it easy for healthcare providers to diagnose infantile spasms with certainty in most cases.
Tests your child’s healthcare provider may order to determine the cause of the infantile spasms include:
- Magnetic resonance imaging (MRI) brain scan: An MRI brain scan is a painless test that produces very clear images of the structures and tissues in your child’s brain. MRI uses a large magnet, radio waves and a computer to produce the detailed images.
 It doesn’t use X-rays (radiation). An MRI can help your child’s healthcare provider determine what’s causing their spasms.
It doesn’t use X-rays (radiation). An MRI can help your child’s healthcare provider determine what’s causing their spasms. - Genetic and metabolic tests: If your child’s MRI is normal, their healthcare provider will likely order other tests, such as genetic and metabolic tests, to try to determine the cause of the spasms. These tests typically require a sample of blood, urine (pee) or spinal fluid.
Management and Treatment
How are infantile spasms treated?
The main goals of treatment for infantile spasms are to stop or control the spasms and to treat the cause, if possible.
The main therapies to stop and/or manage spasms include:
- Adrenocorticotropic hormone (ACTH): ACTH is a hormone your pituitary gland releases that plays a large role in how your body responds to stress. The release of ACTH triggers your adrenal glands to produce cortisol, the “stress hormone.” ACTH for the treatment of spasms is a synthetic (man-made) form of the hormone that’s given as a shot (injection).
 Your child will receive the first doses in the hospital so their healthcare provider can closely monitor them for any side effects. As your child will continue needing ACTH shots for about six weeks, their healthcare provider will give you instructions on how to give your child the injections at home.
Your child will receive the first doses in the hospital so their healthcare provider can closely monitor them for any side effects. As your child will continue needing ACTH shots for about six weeks, their healthcare provider will give you instructions on how to give your child the injections at home. - Oral prednisolone: This medication is a synthetic form of a corticosteroid hormone made by your adrenal gland. It works well for the treatment of infantile spasms and can be used when there are problems with access to ACTH.
- Vigabatrin (Sabril®): This is an anti-seizure medication. It’s taken by mouth as a pill or liquid.
If your child doesn't respond to either hormone treatments or vigabatrin, further treatment options include:
- The ketogenic diet.
- Other anti-seizure medicine.
- Epilepsy surgery when there’s a focalized lesion that’s causing the infantile spasms.
Infantile spasms can be difficult to treat. Some children need a repeat course of treatment or a second treatment therapy. Throughout treatment, your child will need repeat EEG tests to check their brain activity to see if treatment is working.
Some children need a repeat course of treatment or a second treatment therapy. Throughout treatment, your child will need repeat EEG tests to check their brain activity to see if treatment is working.
If your baby’s healthcare provider can determine the cause of the spasms, they’ll need to treat the causes as well, if possible. This may include surgery or targeted therapy for an underlying genetic or metabolic condition.
Developmental delay and regression are common with infantile spasms. Your baby’s healthcare team will suggest therapies to help with development as much as possible.
What are the side effects of infantile spasms treatment?
Possible side effects of adrenocorticotropic hormone (ACTH) treatment for infantile spasms include:
- High blood pressure (hypertension).
- Weakened immune system (immunosuppression).
- Swelling (often in their face).
- Agitation and irritability.
- Stomach ulcers and/or intestinal ulcers.

- Passing of glucose through urine (pee).
Possible side effects of vigabatrin for treatment of infantile spasms include:
- Irreversible narrowing of their field of vision.
- Irritability.
Because of these side effects, your child’s healthcare provider will work with you to determine the best treatment option. They’ll also closely monitor your child to look for signs of these side effects.
Outlook / Prognosis
What is the prognosis (outlook) for infantile spasms?
The prognosis (outlook) for infantile spasms depends on several factors, including:
- The cause of infantile spasms.
- If the cause can be treated.
- How soon your child was diagnosed and treated.
- If your baby was reaching developmental milestones before the spasms started.
Up to 50% of children with infantile spasms have long-term developmental and neurological issues. Even if the spasms stop, many children develop other kinds of seizures and epilepsy.
If diagnosis and treatment are prompt and effective, the overall outlook is better. Normal development is possible for children who were reaching developmental milestones before their spasms started.
Living With
How do I take care of my child with infantile spasms?
To help your baby with infantile spasms, follow their healthcare provider’s instructions for:
- Giving any medications as prescribed.
- Getting developmental assessments and therapies.
- Going to all follow-up medical visits.
Infantile spasms can lead to cognitive (intellectual), neurologic and/or sensory issues. Most children with infantile spasms will have problems with their development and may need help with daily tasks throughout their lives.
Your child’s healthcare team can answer questions and offer support. They also might be able to recommend a local or online support group.
When should I see my child’s healthcare provider about infantile spasms?
If your child has been diagnosed with infantile spasms, they’ll need to see their healthcare team regularly to make sure their treatment is working. They’ll also need EEG tests throughout their treatment to monitor their brain activity.
They’ll also need EEG tests throughout their treatment to monitor their brain activity.
If you think your baby is having infantile spasms but hasn’t been diagnosed yet, it’s important to talk to their healthcare provider as soon as possible.
A note from Cleveland Clinic
Noticing that your baby isn’t behaving as they normally do or isn’t reaching development milestones can be concerning. You know your baby best. If you think they’re having spasms, which look like brief tensing or jerking spells, often in a series, talk to their healthcare provider as soon as possible. Try to take a video of their spasms if you can, so you can show their doctor. Early recognition of infantile spasms leads to better outcomes.
90,000 12 causes of concern for a child when breastfeeding. Why does a baby cry during breastfeeding In the first weeks after birth, a newborn and his mother only get used to each other, and much of the baby's behavior is unclear to the mother. Why, for example, does a child worry at the breast during feeding? There are many reasons for this, and we decided to describe them and offer ways to overcome difficulties. Let's start with the cause of the child's anxiety, which mothers call the first, but which really exists least of all. nine0004
Why, for example, does a child worry at the breast during feeding? There are many reasons for this, and we decided to describe them and offer ways to overcome difficulties. Let's start with the cause of the child's anxiety, which mothers call the first, but which really exists least of all. nine0004
Lack of milk
This is the first thing that comes to the mind of a nursing mother whose baby cries a lot, including at the breast. One of the biggest challenges with breastfeeding, oddly enough, is that breastfeeding moms don't know exactly how much milk their babies are getting or if they're getting enough.
If your child is overly restless, most outside well-wishers will likely point out to you that the baby is probably hungry. Since you are a mother, such remarks can make you feel guilty. After all, it is your responsibility to feed the child! How to dispel doubts and fears associated with a lack of milk? nine0005
- Watch your baby urinate and defecate.
 After the sixth day of life, you should receive at least six wet diapers and one dirty diaper per day. If so, then your baby is getting enough milk.
After the sixth day of life, you should receive at least six wet diapers and one dirty diaper per day. If so, then your baby is getting enough milk. - Frequent feedings are normal. In the first few weeks of life, a newborn usually needs 8-12 feedings per day. At the very beginning, you may at times have to keep it near your chest almost all the time. For several hours, he will demand it very often, and then fall asleep for four to five hours. As the baby learns to suckle more effectively, the number of feeds decreases. nine0016
- Keep track of your baby's weight. By two weeks, the baby should have regained the weight it was born with and gain at least 150 grams per week for the next two to three months.
If you are still worried that you are not getting enough milk, you may find it helpful to have a lactation consultant who will monitor, assess your baby's weight gain and suggest ways to increase your milk supply, if needed.
Swelling of the breast
Sometimes the child's restless behavior at the breast is caused by breast swelling. Excessive breast swelling most often occurs in the first weeks after childbirth. To reduce it, express some milk manually or with a quality breast pump to make the breast softer and easier for the baby to take it. Don't express too much milk, as this can cause you to produce too much milk later on, which will only make the swelling worse. Apply cold compresses to your breasts between feedings to reduce swelling and soreness. nine0005
Flat or indented nipples
Also, the baby may be nervous to latch onto the breast if the mother has flat or indented nipples. To stretch them, you can wear special pads between feedings. Turning on the pump for a few minutes before putting the baby to the breast will help elongate the nipples and also start the flow of milk so that the baby will immediately receive it and is more likely to continue sucking instead of dropping the breast and crying.
In some cases, a woman has to use pads that encourage sucking until her nipples become more prominent. This should happen after about two to four weeks of breastfeeding. If you are having trouble with flat or sunken nipples, seek help from a lactation consultant as soon as possible. nine0005
Incorrect attachment, awkward posture
Another cause of restless behavior at the chest is incorrect position . Both the mother and the baby may be uncomfortable, due to which the effect on the breast is not as it should be, and a sufficient flow of milk is disturbed. If your baby is very nervous, your best bet is to use the underarm position (when you hold the baby to your side, holding him tightly against your nearest breast) or the "cradle" position (when you hold the baby horizontally at your chest), as these positions allow you to control his head. nine0005
These postures allow you to guide the baby to the breast and hold him there. The baby's nose and chin should be pressed into the mother's chest. As a rule, he suckles better when his mother holds him tightly. If something makes you feel uncomfortable while feeding, contact a consultant. Perhaps this is the reason for your baby's anxiety.
As a rule, he suckles better when his mother holds him tightly. If something makes you feel uncomfortable while feeding, contact a consultant. Perhaps this is the reason for your baby's anxiety.
Gastroesophageal reflux
Almost all children have some degree of gastroesophageal reflux. This medical term refers to a condition in which the annular muscle (sphincter) that blocks the entrance to the stomach has not yet fully formed and does not always completely close the opening. Because of this, some milk, along with gastric juice, can flow back into the esophagus, causing a sensation that we call "heartburn." nine0005
As anyone who has ever experienced it knows, it is quite an unpleasant sensation. Just as an adult can relieve heartburn by sitting with a straight back, a child can also usually benefit from being held upright.
Sometimes reflux can occur during feeding. Its appearance can be prevented by holding the child more upright or periodically taking breaks so that the baby “stood” a little. As the child develops, so does the musculature, so that cases of reflux become rarer. nine0005
As the child develops, so does the musculature, so that cases of reflux become rarer. nine0005
Sometimes the problem is so severe that the child is unable to eat normally due to reflux. In such cases, you must consult a doctor.
Increased flatulence
All newborns have flatulence . When a child begins to eat, he starts reflex gas production, which is necessary for the waste generated during nutrition to be removed from the body more quickly. This prevents constipation.
Since breast milk is very easy to digest, it takes very little time for this food to pass through the baby's gastrointestinal tract. You can often hear characteristic sounds while the baby is still suckling. Although all children have gas, some tolerate it better than others. The time of day can also influence this. Apparently, the problem of flatulence becomes more noticeable at the end of the day. Traditionally, this time is considered the most hectic. The child seems to not want to let go of the breast at all, and this, in turn, can aggravate flatulence. This problem disappears on its own as the baby develops. nine0005
This problem disappears on its own as the baby develops. nine0005
How to calm a crying baby
Many of the methods that promote calming are somehow related to the imitation of intrauterine conditions. Make sure that the air temperature is comfortable - not too hot and not too cool. Change diapers promptly. The baby can feel peace if he is held tightly to him or rocked. Swaddling or monotonous sounds - music or the buzzing of electrical appliances - may turn out to be effective. You can carry your baby in a sling, thereby providing him with comfort and getting the opportunity to do some business at the same time. nine0028 You can involve one of the family members in calming the child - for example, a father, grandmother or grandfather; in this case, the baby will not feel the smell of breast milk coming from the mother, which can excite him. In addition, this will give the mother the opportunity to devote some time to herself.
Physiological lactase deficiency
At the beginning of feeding, mother's milk is more saturated with milk sugar - lactose. It's called "front". After 10-15 minutes of feeding with the same breast, she begins to produce "hind" milk. It is richer in fats, which neutralize lactose and thereby reduce gas formation. If the baby is getting too much foremilk and not getting enough hindmilk, an excess of lactose and a lack of the lactase enzyme, which increases flatulence.
It's called "front". After 10-15 minutes of feeding with the same breast, she begins to produce "hind" milk. It is richer in fats, which neutralize lactose and thereby reduce gas formation. If the baby is getting too much foremilk and not getting enough hindmilk, an excess of lactose and a lack of the lactase enzyme, which increases flatulence.
Try to have your baby suckle from one breast for at least 12-15 minutes to get the hind milk. When the baby grows up and sucks more efficiently, it will get to him in a shorter period of time after the start of feeding. Hindmilk has a calming effect and helps restless babies fall asleep. Most newborns naturally fall asleep at the end of a feed due to the calming action of hindmilk. nine0005
The baby chokes on milk
While the baby is just learning to breastfeed, the so-called milk ejection reflex can be too powerful for him and lead to him choking. Because of this, the baby can drop the breast and start to get nervous. Press firmly on the breast for about a minute to stop the too rapid flow of milk, and then put the baby back on the breast. Try expressing some milk before feeding and see if you can trigger the ejection reflex before the baby takes the breast. Feed your baby in the underarm position. As the baby gets older, it will be able to cope with the consequences of the milk ejection reflex in any position for feeding without any problems. nine0005
Press firmly on the breast for about a minute to stop the too rapid flow of milk, and then put the baby back on the breast. Try expressing some milk before feeding and see if you can trigger the ejection reflex before the baby takes the breast. Feed your baby in the underarm position. As the baby gets older, it will be able to cope with the consequences of the milk ejection reflex in any position for feeding without any problems. nine0005
Smell
In rare cases, the baby becomes nervous and throws up the breast because of the soaps or creams you put on the breasts or nipples . If you start using some new remedy, and the child becomes more nervous, wash it off and start feeding again.
Thrush
The baby may develop a yeast infection in the mouth or on the nipples - the so-called thrush. You will see white spots in the child's mouth.
Your nipples may become bright red or itchy and burn after feeding. During feeding, the baby may be more restless than usual.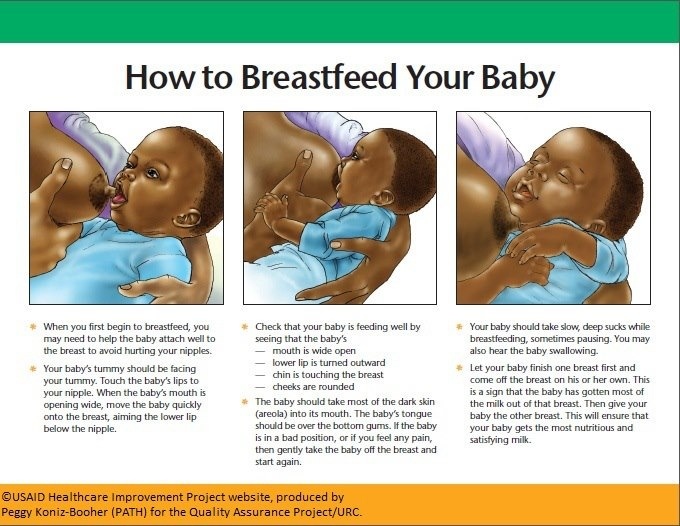
See a doctor. If he confirms that you have a fungal infection, both you and the child will have to undergo treatment.
Too noisy and too bright
In some children, excessive anxiety is associated with overstimulation. They can behave more calmly during feeding if it takes place in a darkened and quiet room. nine0005
Wants to calm down with the breast
Before 12 weeks, babies have little ability to soothe themselves and often reach for the breast just for comfort. They begin to suck to calm down, not experiencing at this moment the need for food. For parents, this need of the baby should be on a par with all the other vital things that you provide to the child.
The main causes of restless behavior of the newborn disappear after the first six weeks. Some problems may exist for a little longer, but they are usually resolved by three months. nine0005
During this period, you must definitely take care of yourself. Eat well. Drink plenty of fluids and exercise outdoors. Try a variety of relaxation techniques—yoga, meditation, massage, or a warm bath—to help you get through the tough times.
Try a variety of relaxation techniques—yoga, meditation, massage, or a warm bath—to help you get through the tough times.
Share your feelings with the child's father and other family members, and have them take turns comforting, lulling, and rocking the child.
Set small goals for yourself, like reading one chapter from a book or going for a walk for 15 minutes. nine0028 Group classes for young mothers are very useful, because there you will find out that other mothers and their children, like you and your child, go through exactly the same period of adjustment.
The main thing you need to remember is that this is a very short period in your own life and the life of your baby. Try to hug and cuddle your child as often as possible to help him get through a difficult time for him. Together you will succeed.
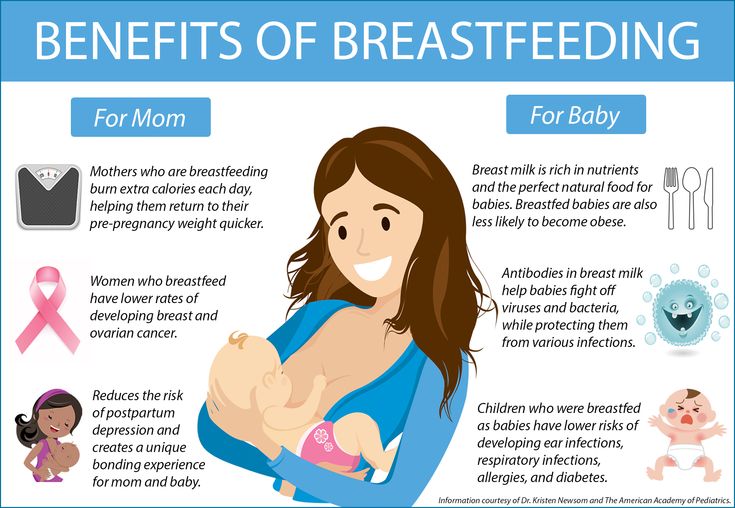
12 reasons why breastfeeding is not just about milk
Breastfeeding is the right choice for expectant mothers and their babies.
Increasingly, at appointments, pediatricians on the day of a healthy child are faced with the problems of breastfeeding in new mothers. This problem is very relevant, because at the moment in the world there is a "boom" of breastfeeding, and that's fine.
This problem is very relevant, because at the moment in the world there is a "boom" of breastfeeding, and that's fine.
It is important to remember that the best food for a baby is and will always be the mother's breast milk in the first year of life.
Breastfeeding is a natural process that replaces pregnancy and childbirth. A newborn and his mother equally need breastfeeding. nine0005
12 reasons why breastfeeding is not just about milk.
1. Calm down. Babies have a need to suck. Even when the baby is full, the baby can still continue to breastfeed. Even if you are scared by the thought that your baby is “hanging on his chest” too much and for you this means that he is not full, then this is not so. The child has one of the most pronounced reflexes in the first weeks of life - the sucking reflex. And best of all, he satisfies him naturally, and not through pacifiers or bottles. nine0005
2. Analgesic effect. Attachment to the chest helps to remove pain from cutting teeth, ear pain and other similar phenomena.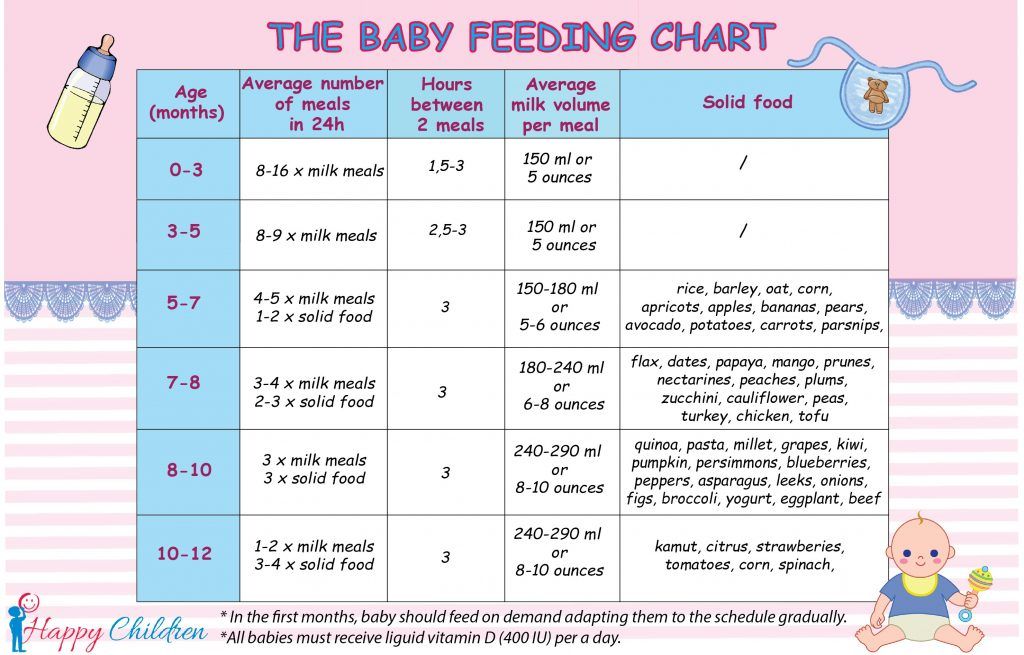 Note that this is not always the case. If your child is restless on the chest, draws his legs during feeding, is naughty, hits his ears, then it is best to contact a specialist to examine the child.
Note that this is not always the case. If your child is restless on the chest, draws his legs during feeding, is naughty, hits his ears, then it is best to contact a specialist to examine the child.
3. Quenching thirst. Breast milk contains a lot of water, so the baby can take it if he wants to drink, but not eat.
It is important not to supplement your breastfeeding baby! If your personal physician or consultant claims otherwise, you should consider another candidate. Supplementation with water takes place to be bottle-fed. Don't force your child to drink water if he doesn't want to. nine0005
4. Natural medicine. If a child is sick, he may ask for a breast more often, because his body dictates to him so. Babies are less likely to get sick while breastfed. Most often, parents do not experience respiratory diseases in the first year of a child's life.
5. Relaxation. When the baby is overworked or frightened, the chest will help to relax and calm him down. First of all, here plays the role of contact between mother and child. The baby has no one dearer and closer than the mother, and this will continue for the first years, until the child socializes and feels himself in society. Mom is like a whole world for him, and when a child feels warmth and mother's touch, he feels completely safe. At the time of breastfeeding, this is especially pronounced. nine0005
The baby has no one dearer and closer than the mother, and this will continue for the first years, until the child socializes and feels himself in society. Mom is like a whole world for him, and when a child feels warmth and mother's touch, he feels completely safe. At the time of breastfeeding, this is especially pronounced. nine0005
6. Sleeping pills. An interesting fact: at night, the level of melatonin, a natural sleeping pill for an infant, rises in breast milk. Perhaps that is why most babies fall asleep on their breasts with ease. And at the same time they continue to suck
7. Breast milk is easily digested. There is no danger of overfeeding the baby, you can breastfeed whenever you ask. When feeding with a mixture, you should always monitor the amount eaten per day.
8. Sucking regulates milk production. Every time a baby is breastfed, it shows the mother's body how much milk she needs. It is important not to skip breastfeeding on demand so that milk is produced in sufficient quantities. The same applies to the quality and composition of milk. nine0005
The same applies to the quality and composition of milk. nine0005
9. Attachment. When a baby suckles, the mother's body releases the hormone oxytocin, also known as the love hormone. And the truth is, every time you feed a child, you fall in love with each other even more.
10. Everything is free! Why buy bottles, breast pumps, bags...? Breast milk is both healthy and free. No bottles and nipples, it's better to once again spend money on really necessary or pleasant things for the baby, or for yourself)
11. Breast milk from the breast is always at the ideal temperature. No need to freeze, defrost, heat…
13. You can get enough sleep while breastfeeding☺ Believe it or not, many breastfeeding moms say they get enough sleep even though no one helps them with nighttime feeds. And the reason is that they don't have to get out of bed to cook and heat the formula. Breastfeeding mothers, and especially those who practice co-sleeping, breastfeed the baby that has not yet fully woken up, which allows both of them to fall asleep sooner.