Baby watery sick after feed
Reflux in babies - NHS
Reflux is when a baby brings up milk, or is sick, during or shortly after feeding. It's very common and usually gets better on its own.
Check if your baby has reflux
Reflux usually starts before a baby is 8 weeks old and gets better by the time they're 1.
Symptoms of reflux in babies include:
- bringing up milk or being sick during or shortly after feeding
- coughing or hiccupping when feeding
- being unsettled during feeding
- swallowing or gulping after burping or feeding
- crying and not settling
- not gaining weight as they're not keeping enough food down
Sometimes babies may have signs of reflux but will not bring up milk or be sick. This is known as silent reflux.
Things you can try to ease reflux in babies
Your baby does not usually need to see a doctor if they have reflux, as long as they're happy, healthy and gaining weight.
Do
-
ask a health visitor for advice and support
-
get advice about your baby's breastfeeding position or how to bottle feed your baby
-
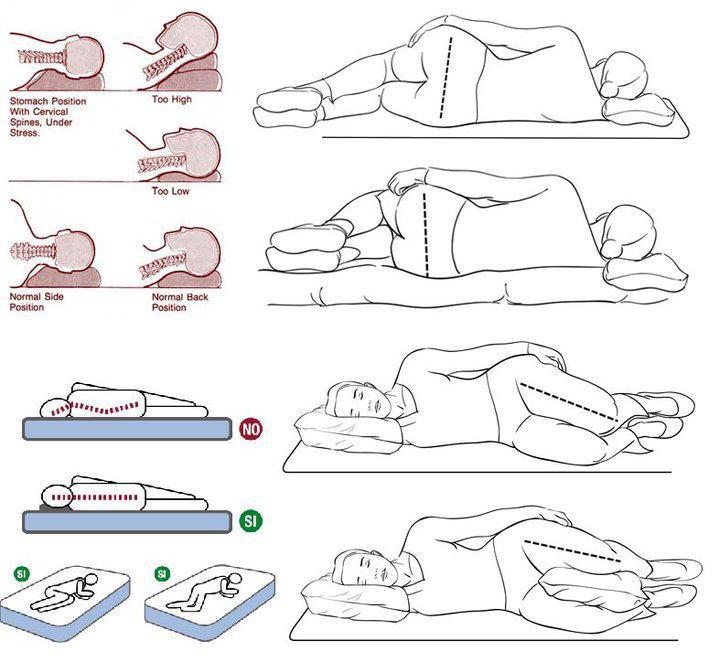
hold your baby upright during feeding and for as long as possible after feeding
-
burp your baby regularly during feeds
-
give formula-fed babies smaller feeds more often
-
make sure your baby sleeps flat on their back (they should not sleep on their side or front)
Non-urgent advice: See a GP if your baby:
- is not improving after trying things to ease reflux
- gets reflux for the first time after they're 6 months old
- is older than 1 and still has reflux
- is not gaining weight or is losing weight
Urgent advice: Ask for an urgent GP appointment or call 111 if your baby:
- has vomit that's green or yellow, or has blood in it
- is projectile vomiting (being sick with more force than usual)
- has blood in their poo
- has a swollen or tender tummy
- has a very high temperature or they feel hot or shivery
- keeps being sick and cannot keep fluid down
- has diarrhoea that lasts for over a week or has signs of dehydration
- will not stop crying and is very distressed
- is refusing to feed
Also call your GP or 111 if you have any other concerns about your baby.
Treatment for reflux in babies
A GP or specialist may sometimes recommend treatments for reflux.
If your baby is formula-fed, you may be given:
- a powder that's mixed with formula to thicken it
- a pre-thickened formula milk
If the thickening powder does not help or your baby is breastfed, a GP or specialist might recommend medicines that stop your baby's stomach producing as much acid.
Very rarely, surgery might be needed to strengthen the muscles to stop food or milk travelling back up. This is usually only after trying other things or if their reflux is severe.
Causes of reflux
Reflux usually happens because your baby's food pipe (oesophagus) has not fully developed, so milk can come back up easily.
Your baby's oesophagus will develop as they get older and the reflux should stop.
Page last reviewed: 13 December 2021
Next review due: 13 December 2024
Baby Spitting Up Clear Liquid? Causes and When to Call the Doctor
So clear liquid is part of the package deal. But what is it and why does it happen? Several things could be at play here: saliva, spit-up from breast milk or formula, mucus, or even a combination of these. Let’s take a closer look.
Spit-up
Babies under a year old spit up — for some it’s often and a lot. Usually, spit-up is simply part and parcel of their maturing digestive system.
Your baby may do you the kindness of burping before they spit up. So listen up and stay prepared with burp cloth in hand.
After a burp, you may see a lot of spit up or simply a white, milky drool. Sometimes the spit up or drool could be clear. Sometimes this is just partially digested formula or breast milk combined with saliva.![]()
Whether it is white or clear, a little spit-up or drool after a feed is normal.
Vomiting
Your baby has a ton of learning to do. Including learning not to gulp down milk too quickly, not to eat more than their tummy can hold in one sitting, and how to digest food.
During the first months, while they’re still learning, your baby may vomit. Here’s how you spot the difference between vomit and spit-up:
- Vomit shoots out when the muscles around the stomach contract forcefully to push out the contents.
- Vomit will probably have some clear stomach juices mixed into it. It may also look like curdled milk or miniature lumps of cottage cheese.
Unless the vomiting is happening frequently or accompanied by other symptoms, like a fever, it may just be part of the learning process. Yes, you’ll get used to this part of parenting too.
Teething
Your baby will probably cut their first teeth between 4 and 7 months old. While this milestone is a cause to celebrate, it may not be painless. Teething can sometimes cause discomfort and even pain.
Teething can sometimes cause discomfort and even pain.
Drooling plenty of clear saliva is your baby’s way of coping. Sometimes they may even spit up some excess drool.
You can help ease your baby’s discomfort by rubbing the sore gums with your finger or giving them a cool teething ring to bite on. You can also use bibs to help catch some excess saliva as it drips off their chin.
But there’s not much you can do to stop the excess drool, even if it makes them spit up — just know that it’s a temporary phase.
On the other hand, if the spit-up turns to vomit, it’s not just teething. You should consider whether your little one has other symptoms and consult with your doctor.
Illness
Babies and children get sick more often than adults because their immune system is developing. From about 6 months old, when the immunity you gave to your baby starts to fade, your little one will have to start building up their own immune system.
Heads up: This developing immune system means your baby may start to get colds. Since your baby hasn’t yet learned to blow their nose or cough up mucus, they’ll be swallowing a lot of the mucus, which might cause vomiting. This mucus can come up as a clear or cloudy liquid when they vomit.
Since your baby hasn’t yet learned to blow their nose or cough up mucus, they’ll be swallowing a lot of the mucus, which might cause vomiting. This mucus can come up as a clear or cloudy liquid when they vomit.
If your baby is vomiting and has fever and diarrhea, you may notice that the vomit is clear. This happens when nothing is left in the stomach to throw up except for clear stomach secretions.
Speak with your pediatrician if your baby exhibits these symptoms to be sure that your little one gets the appropriate care.
A fever of 100.4°F (38°C) or higher in a baby who’s under 2 or 3 months old also warrants a call to the doctor. You should also call your doctor if your older baby, between 3 and 6 months, has a fever of 101°F (38.3°C) or higher.
No matter their age, a fever that persists for more than 5 days warrants a call to the doctor and likely a visit.
Reflux
Your doctor will call it gastroesophageal reflux (GER). Reflux happens when your baby regurgitates food from their stomach and spits up. More than two-thirds of babies will have reflux that causes spitting up as often as a few times a day.
More than two-thirds of babies will have reflux that causes spitting up as often as a few times a day.
As long as your baby is happy and gaining weight, GER isn’t a cause for concern. Typically, it peaks at 4 months of age and by the time your baby is a year old, chances are it will probably be a bad memory.
In rare cases, GER can signal something more serious like an allergy, a blockage in the digestive system, or gastroesophageal reflux disease (GERD). Yes that D makes all the difference.
With GERD, your baby may vomit, refuse to eat, not gain weight, and let you know he’s unhappy by crying. Your doctor may advise you to feed your baby smaller meals more frequently and to change formula or to cut out dairy if you’re breastfeeding. Sometimes medication or surgery will be needed.
Pyloric stenosis
This rare condition is named after the pyloric sphincter muscle that sits at the outlet to the stomach and it affects well under 1 percent of infants in the United States (more boys than girls).
Babies with this condition have a pyloric sphincter muscle that is thickened and narrow (stenosis). The narrowed pyloric channel restricts food in the stomach from entering the small intestine.
The stomach reacts by contracting vigorously to force the food through, but because the channel is so narrow, the food is vomited up with tremendous force. This projectile vomiting can reach several feet away!
You’ll see clear fluid or curdled milk. As the channel narrows more and more, projectile vomiting becomes more frequent. Despite the vomiting, your baby still feels hungry and will want to eat again… and again.
If your little one is affected, you’ll start to notice this type of vomiting when your baby is 2 to 3 weeks old, but it can start as late as 6 weeks old. Without nourishment, your baby can become dehydrated, weak, and lose weight.
Although pyloric stenosis is a serious condition, it can be easily righted with surgery. If you suspect this is the issue you should call the doctor right away to discuss your baby’s symptoms.
When they’re spitting up lots of clear liquid you may think that your baby needs water to avoid dehydration. However, you shouldn’t give water to babies under 6 months of age.
Drinking plenty of water every day may be good for you, but it definitely isn’t good for your baby. That’s because babies have tiny tummies (about the size of a walnut in the first week) and their kidneys are still developing.
If you fill your baby’s tummy with water, their hunger mechanism is dulled, and they may not get the nutrients they need. In addition, if your baby’s water intake is too high, there’s a risk of water intoxication.
Sounds far-fetched? Not really when you consider the size of that tiny tummy. Too much water will lower the concentration of electrolytes such as sodium in the blood. So hold the water until your baby is about 6 months old and stick to formula or breast milk.
Your medical team is there to help you with concerns as your child grows. Don’t hesitate to contact them to discuss any issues.
While much of the mess around spit-ups can be easily handled (with a rag and some patience), if you see that your baby has fever, seems listless, is dehydrated, or doesn’t appear to be putting on weight, contact your doctor.
When you’re wiping away another spit-up, you may be tempted to throw in that towel. But hold on… one day soon your baby’s digestive system will be working smoothly and the two of you will be ready to move on to the next stage of child rearing.
Lactose insufficiency - articles from the specialists of the clinic "Mother and Child"
what it is
The main food of babies is milk (breast or formula). It contains many different nutrients (proteins, fats, carbohydrates), which, with the help of special digestive enzymes, are broken down into simple components and digested. But in young children, the gastrointestinal tract is still immature, there are few enzymes in it, others are not at all or they are not yet working at full capacity. When the baby grows up, there will be more enzymes, the digestive system will mature, but for now there may be various problems with it.
When the baby grows up, there will be more enzymes, the digestive system will mature, but for now there may be various problems with it.
All milk (women's, cow's, goat's, artificial mixtures) and dairy products contain the carbohydrate lactose, also called "milk sugar". In order for lactose to be absorbed, the lactase enzyme must break it down, but if the child has little or no lactase enzyme, then lactose is not broken down and remains in the intestine. As a result, there is always a large amount of milk sugar in the intestines, which begins to ferment, and where there is fermentation, conditionally pathogenic flora actively reproduces. What we feel during fermentation: intestinal motility increases (it rumbles), plus gas formation increases (the stomach swells). But in an adult, this is usually a one-time situation due to some inaccuracies in nutrition, and it quickly passes. But in babies, everything is different, especially since they lack the enzyme not once, but constantly. What it looks like: The milk sugar lactose retains water, hence loose stools. In the child’s stomach, “rumbles and boils”, colic begins, the stool becomes frothy, greens, mucus and even blood may appear in it. If at first the stool was liquid, then constipation appears, and all this changes in a circle: yesterday there was diarrhea, today and tomorrow there is no stool at all, the day after tomorrow it is liquid again. And the most unpleasant thing is endless colic and endless crying, there is no rest for both the parents themselves and the baby. Mom at some point notices that the baby is crying just after feeding, and then a variety of advice falls upon her. “Your milk is bad, better give the mixture,” says the beloved mother-in-law. “Only breasts and nothing else!” - advise breastfeeding gurus. As a result, the mother tries one thing or the other, but neither breast milk nor artificial mixture gives relief to the child. Colic, crying and problems with the stomach and stool continue. The parents are in a panic because they don't understand what is going on.
What it looks like: The milk sugar lactose retains water, hence loose stools. In the child’s stomach, “rumbles and boils”, colic begins, the stool becomes frothy, greens, mucus and even blood may appear in it. If at first the stool was liquid, then constipation appears, and all this changes in a circle: yesterday there was diarrhea, today and tomorrow there is no stool at all, the day after tomorrow it is liquid again. And the most unpleasant thing is endless colic and endless crying, there is no rest for both the parents themselves and the baby. Mom at some point notices that the baby is crying just after feeding, and then a variety of advice falls upon her. “Your milk is bad, better give the mixture,” says the beloved mother-in-law. “Only breasts and nothing else!” - advise breastfeeding gurus. As a result, the mother tries one thing or the other, but neither breast milk nor artificial mixture gives relief to the child. Colic, crying and problems with the stomach and stool continue. The parents are in a panic because they don't understand what is going on. In fact, this is a typical picture of bright lactase deficiency (LN), or insufficient production of the lactase enzyme.
In fact, this is a typical picture of bright lactase deficiency (LN), or insufficient production of the lactase enzyme.
various reasons
There are several types of lactase deficiency, and it is with them that confusion arises.
Congenital lactase deficiency is a genetic and very rare disease (one case in several thousand newborns), it is difficult to confuse it with something, since it is very difficult. The diagnosis is made in the maternity hospital or in the first days after birth, the child does not have lactase at all, he quickly loses weight, he is immediately started to be fed intravenously or through a tube. Some experts (but not doctors) on breastfeeding read once that congenital lactase deficiency is an extremely rare disease, and that’s all - they further began to assure young mothers: “In fact, LN is extremely rare, you don’t have it, you don’t need to listen to doctors ", etc. Yes, congenital LN is a rare disease, but the key word here is "congenital", and there are other types of lactase deficiency.
Transient lactase deficiency in infants . And this is exactly the condition that occurs very often. The baby was born, and so far he still has little lactase enzyme, plus little normal intestinal microflora. Hence the colic, and loose stools, and mucus, and greenery, and crying, and the nerves of the parents. After a while, the child's digestive system will fully mature, all enzymes will begin to work actively, the intestines will be populated with what is needed, and "lactase deficiency" will disappear. Therefore, such a LN is called "transient", that is, temporary, or passing. It passes for someone a month after birth, for someone longer - after six to seven months, and there are children in whom lactase deficiency completely disappears only by the year.
Secondary lactase deficiency. This condition appears if a person has had some kind of intestinal infection, and it does not matter whether it is an adult or a baby. For some time after the illness, the child does not tolerate milk (any), and then with proper nutrition and sometimes even without treatment, everything quickly passes.
Lactase deficiency in adults. There are people in whom the lactase enzyme begins to be lacking only in adulthood, this happens for various reasons: for some, lactase ceases to be produced in the right amount after some kind of illness, for other people, the activity of this enzyme simply fades over time by itself. yourself. As a result, at some age, a person begins to tolerate milk and dairy products poorly, although before that everything was fine. The symptoms are the same as in babies: he drank milk and after that the stomach rumbles, boils, and the stool is liquid. Sooner or later, a person realizes that milk is not his product, and simply stops drinking it in its pure form.
what to do
If there is transient lactase deficiency, then what to do with it? First you need to understand if it exists at all. Why does the child have problems with the stomach, stool, why does he cry all the time? Is it neurology, common colic, errors in the mother's diet, an inappropriate mixture (if the baby is bottle-fed), improper breastfeeding technique, lactase deficiency, or a reaction to the weather? It can be difficult to figure it out right away, but if the tests show that there is lactase deficiency, then it is most likely in it. Now what to do next - treat it, wait for the enzymes to mature, or something else? Firstly, everything here will depend on how much the enzyme is lacking and, therefore, on how much LN worries the child and parents. Some children lack the enzyme quite a bit, so their colic is mild and children cry quite normally. Plus, the violation of the stool is also not very bright: there are a couple of times a slightly liquefied stool, but that's all. In other children, the lack of lactase is more pronounced, the child does not cry, but simply yells after each feeding, if at first he gained weight well, then after two months the increase is minimal, problems with stools begin in parallel (day - constipation, day - diarrhea), stool sometimes green, sometimes with mucus. Atopic dermatitis appears on the skin (the skin is the first to react to problems with the gastrointestinal tract). Parents have no rest day or night: the baby cries - he is fed - he cries again, they try to calm him down in other ways.
Now what to do next - treat it, wait for the enzymes to mature, or something else? Firstly, everything here will depend on how much the enzyme is lacking and, therefore, on how much LN worries the child and parents. Some children lack the enzyme quite a bit, so their colic is mild and children cry quite normally. Plus, the violation of the stool is also not very bright: there are a couple of times a slightly liquefied stool, but that's all. In other children, the lack of lactase is more pronounced, the child does not cry, but simply yells after each feeding, if at first he gained weight well, then after two months the increase is minimal, problems with stools begin in parallel (day - constipation, day - diarrhea), stool sometimes green, sometimes with mucus. Atopic dermatitis appears on the skin (the skin is the first to react to problems with the gastrointestinal tract). Parents have no rest day or night: the baby cries - he is fed - he cries again, they try to calm him down in other ways. But nothing helps. Mom and dad are in a panic, and no one has the strength anymore.
But nothing helps. Mom and dad are in a panic, and no one has the strength anymore.
If parents see that the child may have signs of lactase deficiency, that he needs help, first of all, you need to look for a good doctor. Only an experienced pediatrician will be able to figure out why the baby has colic or green stools, what the numbers in the tests say, and what is the norm for one baby and the pathology for another. And of course, it is not necessary to cancel breastfeeding and immediately prescribe lactose-free or low-lactose artificial mixtures (even as a supplement). By itself, milk sugar lactose is very necessary for a child, when lactose is broken down, its components (glucose and galactose) go to the development of the brain, retina, for the life of normal intestinal microflora. So do not completely eliminate this sugar, you need to help it break down. With a strongly pronounced LN, the missing enzyme is given before each feeding (it has long been learned to produce and it is sold in pharmacies), with a dim clinic, its dose can be reduced. And it is also possible that there is lactase deficiency (even according to tests), but it does not need to be treated, there are almost no symptoms.
And it is also possible that there is lactase deficiency (even according to tests), but it does not need to be treated, there are almost no symptoms.
But what cannot be done is to listen to non-specialists who deny either lactase deficiency itself or its treatment. They see the cause of all problems with the child's stomach and stool either in the wrong technique of breastfeeding, or partially admit that there is immaturity of the enzyme, but this is natural and will pass by itself. Yes, for some, LN is expressed easily and will pass quickly, but what about those parents whose child yells day and night, covered with a crust from atopic dermatitis and stopped gaining weight? Wait for the time to come and the enzymes to mature? Alas, with pronounced lactase deficiency (even if transient), enterocytes (intestinal cells) often suffer, so it is simply necessary to help such a child.
If you see that your baby has signs of lactase deficiency, look for a doctor who is committed to maintaining breastfeeding and has extensive experience. He will definitely help to find out why the baby is crying, why he has a stomach ache or has problems with stool. And then the life of the parents and the child will return to normal.
He will definitely help to find out why the baby is crying, why he has a stomach ache or has problems with stool. And then the life of the parents and the child will return to normal.
"Transient" (temporary) lactase deficiency in someone passes a month after birth, in someone longer - after six to seven months, and there are children in whom lactase deficiency completely disappears only by the age of one
If the tests show that there is a lactase deficiency, then the matter is most likely in it.
Milk sugar lactose is very necessary for a child: when lactose is broken down, its components (glucose and galactose) go to the development of the brain, retina, for the life of normal intestinal microflora
Parent's note
1. In infants, transient (temporary) lactase deficiency is most common.
2. Symptoms of lactase deficiency usually appear some time after birth. These are colic, frequent crying, increased gas formation, stool - either constipation or diarrhea (over time it becomes frothy, greens, mucus and even blood may appear in it).
3. The simplest study that can reveal lactase deficiency is the analysis of feces for carbohydrates.
4. It is usually not necessary to cancel breastfeeding or partially replace it with lactose-free or low-lactose formulas. You can give the missing enzyme from the outside.
Diarrhea in infants - what causes it and how to treat it
- Alla Anatolyevna, please tell us what diarrhea (diarrhea) is in babies.
- Diarrhea is a disease, a functional disorder of the gastrointestinal tract, which is accompanied by loose stools. There is a Bristol stool scale, according to which diarrhea is considered to be liquid or semi-liquid with hard lumps. Diarrhea is not typical for healthy children.
- What are the symptoms of this problem and how can a mother tell diarrhea from normal stool?
- Diarrhea in young children is quite rare. However, according to the statistics of the World Health Organization, a functional disorder of the gastrointestinal tract, accompanied by diarrhea, is in second place among the causes of death in children of the first year of life.
- Loose stools in babies are normal.
A child of the first or second month of life has a more liquid stool than an adult. If a baby has an egg-yolk-like stool and empties his intestines after each feeding, but gains weight well, eats and sleeps, is cheerful and does not cry, then this should not cause concern to the mother.
Important! Diarrhea is not just loose stools. If a child does not gain weight in the first months of life and has frequent watery, frothy or loose stools with mucus or blood, this is a reason to immediately contact your pediatrician.
- Alla Anatolyevna, what can cause diarrhea in a baby?
- For a child of the first months of life, the main cause of diarrhea is food intolerance, for a child of the second half of life and the second year of life - an intestinal infection of a viral nature. But why the baby has diarrhea, in each case, the doctor must decide.
A food allergy in an infant occurs to the food he receives, most often to cow's milk protein. Causes of allergies in infants:
- in a child exclusively breastfed - the use of dairy products by a nursing mother;
- in a formula-fed child - a reaction to cow's milk formula protein;
- in a mixed-fed child - more allergic to formula milk, to a lesser extent allergic to mother's milk.
Infection of the baby with intestinal infections occurs through dirty hands and toys (when the child starts to crawl, pick up objects from the floor with his hands, play outside).
Signs of an intestinal infection in a child:
- refusal to eat;
- decreased appetite;
- temperature increase;
- vomiting.
- What does the color of the stool in a breastfed and bottle-fed baby say - what are the norms and dangerous situations?
- Bile pigments are responsible for the color of the stool, which are produced by the liver, accumulate in the gallbladder and are released during nutrition, helping digestion. They stain the baby's stool yellow, green, or olive. Therefore, if the child feels well and gains weight well, and the stool has a greenish-yellow tint, this is the norm for up to a year.
They stain the baby's stool yellow, green, or olive. Therefore, if the child feels well and gains weight well, and the stool has a greenish-yellow tint, this is the norm for up to a year.
- Yellow diarrhea in a baby
If a child of 4, 5 or 6 months has yellow stools and a fever, the stools become more frequent and become watery and plentiful, appetite has decreased - these are signs of an intestinal infection.
- Infant has diarrhea with mucus
Mucus in the stool is a product of the goblet cells of the intestine that secrete mucus. Mucus in the stool in a child is a sign of inflammatory colitis of the colon (an indicator of a food allergy or the final stage of an intestinal infection). Mucus in the stool should not be.
- Diarrhea without fever in a child - what can this mean and what should a mother do?
- Do not ignore diarrhea without fever in the baby. This may be a manifestation of pathological conditions. Such as:
Such as:
- Food allergy - its cause will be determined by the doctor, who will also tell you what to do for mom.
- Antibiotic-associated diarrhea - in children, it occurs during the treatment of an infectious disease, which is associated with the activity of clostridia and their toxins, which is accompanied by diarrhea with blood. Such a serious condition requires a visit to the doctor.
- Gluten intolerance - prolonged diarrhea in celiac disease does not respond to traditional treatment and does not resemble the course of an intestinal infection. The assumption of the presence of such a disease requires additional examination, observation, and at least a consultation with a competent pediatrician and pediatric gastroenterologist.
- Alla Anatolyevna, can diarrhea begin when teething?
- During the teething period, there may be a violation of the stool, but it is not related to the fact that the baby is teething. Teething is a normal, physiological process that occurs in all children. Diarrhea is not a norm, but a pathological disorder of the gastrointestinal tract (GIT), which is accompanied by loose stools.
Teething is a normal, physiological process that occurs in all children. Diarrhea is not a norm, but a pathological disorder of the gastrointestinal tract (GIT), which is accompanied by loose stools.
- Diarrhea for complementary foods - what is considered the norm, and what is a problem in such a situation?
- The first complementary foods are introduced to a healthy child in the second half of life. Starting from 6 months, the mother will gradually introduce vegetable purees, cereals, fruit purees and other complementary foods into the baby's menu.
The introduction of complementary foods in a child may be accompanied by a violation of the nature of the stool. But I wouldn't say it's diarrhea. The color of the stool may change in response to the color of the complementary foods, do not worry or worry.
It is necessary to worry and consult a doctor if atopic dermatitis worsens during the introduction of complementary foods, mucus appears in the stool, and skin rashes appear. It is important to determine the cause of the exacerbation (food allergy, intestinal infection, or simply a reaction to complementary foods). Mom needs to remove complementary foods for one or two days, observe the child, and then decide with the doctor what tactics of behavior to choose.
It is important to determine the cause of the exacerbation (food allergy, intestinal infection, or simply a reaction to complementary foods). Mom needs to remove complementary foods for one or two days, observe the child, and then decide with the doctor what tactics of behavior to choose.
- What medical tests should be done for diarrhea?
- If the child is not gaining weight well, he has diarrhea, stool disorders (mucus, blood in the stool), the doctor should examine him and prescribe studies (and then evaluate their results).
What test should be taken for diarrhea in a child
- Test for dysbacteriosis. But it is worth remembering that there is no such diagnosis as dysbacteriosis, and it makes no sense to treat a child from conditionally pathogenic microorganisms that are in his intestines.
- Coprogram - examination of feces under a microscope. With its help, the doctor draws conclusions about the organoleptic, biochemical and bacterioscopic properties of the stool.

- Intestinal culture - test for intestinal viruses (noroviruses, rotaviruses, bocaviruses) to exclude intestinal infection.
- Complete blood count with leukoformula — to determine the tactics of prescribing antibiotics in severe cases (in the treatment of intestinal infection).
- Ultrasound of the abdominal cavity - a comprehensive ultrasound examination to determine the causes of disorders of the gastrointestinal tract in a child.
- Should my mother have any tests and when?
- Nursing mothers are often asked to prescribe an analysis for staphylococcus aureus and allergies. If the child is sick, then there is no special point in examining the mother. Staphylococci are opportunistic microbes that live on the skin and in the ducts of the mammary glands of healthy women. They can cause disease under certain conditions.
In 30% of cases, breast milk of healthy women contains staphylococci. Treatment is not required.
Treatment is not required.
There are also no indications for the analysis of breast milk for sterility, because mother's milk should not be sterile. Breast milk contains a microbiota that is specific to this mother and which she will inhabit the baby's intestines.
- Consequences of diarrhea - how to deal with them?
Diarrhea causes a child's body to lose fluid and electrolytes. This leads to dehydration and loss of 10% or more of body weight. This condition can be dangerous, especially for small children and young children. Treatment is carried out in a hospital (infusion therapy or dehydration with a dropper).
In addition, hospital treatment and observation in a hospital environment require serious complications of intestinal infections. If the baby pees little or there is no urination, this can be an alarming sign of hemorrhagic syndrome in infants, which is accompanied by kidney failure.
The indirect consequences of an intestinal infection sometimes include diaper rash (the stool contains digestive enzymes that irritate the skin during diarrhea).
Important! Signs of diarrhea in infants that require an appointment with a doctor during the day:
- Loose stools and no weight gain.
- The appearance of blood in the stool.
- Combination of diarrhea and vomiting.
- Discolored white chair.
- Remedies for diarrhea for children under 1 year old - what does the doctor prescribe, and what can mom use on her own?
- How to treat diarrhea in infants or loose stools in a one-year-old child always depends on the condition of the baby and the opinion of his doctor.
Intestinal infection disappears (1-3 days), stool and appetite are restored, the temperature subsides most often against the background of symptomatic treatment without additional therapeutic measures. The doctor may recommend a diet without milk, coarse fiber, sugar. Enzymes can be prescribed (they are added to food and help digestion), enterosorbents (taken without food and absorb toxic decay products of viruses) or biologics (displace pathogenic viruses from the microbiota and colonize the intestines with good strains).
If we talk about food allergies and diarrhea in infants during breastfeeding, then a dairy-free diet can be recommended to the mother. If diarrhea in a baby occurs during artificial feeding, a special therapeutic milk mixture is selected for the baby. When a child receives nutrition that suits him within a month, he should have a clear positive trend (weight gain, a significant improvement in well-being).
— How to alleviate the condition of a child with diarrhea?
- 10 years ago, for the treatment of diarrhea with an intestinal infection, a water-tea break was prescribed - the child was not fed anything and was given only drink during the day. Now it is believed that such pauses are not needed and the little patient suffers more from hunger than from the manifestation of an intestinal infection.
It is necessary to feed a child with diarrhea in small portions and more fractionally (reduce the interval between meals and reduce the volume of one feeding). No need to give water or supplement the baby. In case of dehydration with children's diarrhea, tea, mineral water, jelly, dried fruit compote are indicated.
No need to give water or supplement the baby. In case of dehydration with children's diarrhea, tea, mineral water, jelly, dried fruit compote are indicated.
A child's stool is an indicator of his health. So do not rush to throw away the diaper and pay attention to its contents. If you suspect diarrhea in a baby, be sure to discuss the situation with a pediatrician, especially if you have a child in the first months of life. Diarrhea is a pathology and a common symptom of an intestinal infection or food allergy in a child under one year old. Mom's care and attention, doctor's advice and appropriate treatment are all that a child needs to cope with diarrhea, be healthy and happy.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist.