Best food for baby during fever
Diet for Infants & Toddlers With Fever
When your baby or toddler is sick and has a fever, it can be physically taxing for your child as well as you. You can’t see your little one feeling miserable like that. While you can’t wave a magic want to make your child feel like herself again, there’s something you can do (apart from following the doctor’s order) to strengthen your little one’s immune system and to help him recover soon. One of the best ways to build up the strength to fight the infection is by putting your child on a diet that will bolster up the defences of the body. In this article, we will tell you what you can feed your child when he has a fever or when he is sick!
Feeding a Baby During Fever
One of the symptoms that accompanies a fever is the loss of appetite. Your baby is no different and will also refuse to eat in the manner she normally does. Try to get your baby to eat by offering foods that she likes, and ensure they are healthy and nutritious. Your baby might also want to be breastfed or have formula during this time. There is no reason to worry about this as breast milk will provide your baby with all the essential nutrients she needs during her illness. Remember to feed your baby food at regular intervals so her body has the energy to fight the illness, without forcing her to eat more than she wants to.
8 Foods for Babies With Fever (Age: 6-12 months)
Knowing what foods to feed is half the battle won when your baby has a fever. The food should be both well-balanced and energy-rich so it can shore up your baby’s defences in the face of the fever. Here are a few food items you can give your baby during fever.
1.
Dal KhichdiThis basic dish will help your baby regain strength as she fights the illness. It is rich in protein which is easy to digest and also high in energy. Prepare this dish with no spices and salt and do not add any strong flavours in order to make it more palatable to your baby. Keep it simple and serve it warm. Let your baby eat how much she can.
Keep it simple and serve it warm. Let your baby eat how much she can.
2. Soup
Giving your baby a bowl of warm soup is a great way to ensure that she gets the nutrition she needs while also keeping it light on her digestive system. It is easy to prepare and is packed with essential vitamins and minerals. Just boil a few chopped vegetables of your choice in some filtered water. You can either feed your baby only the broth or offer some of the boiled vegetables in mashed form.
3.
DaliyaYou can make this dish by cooking the washed daliya (broken wheat), in a pressure cooker with water. Remember to add a quantity of water that will give it the consistency of a porridge. Daliya is a good source of protein that will give your baby an energy boost. Add a pinch of turmeric, an excellent ingredient for boosting immunity.
4. Vegetable and Fruit Puree
One of the simplest things you can give your baby when she has a fever is pureed fruits and vegetables. You can choose which fruit or vegetable you want to give your baby according to her preferences. Apples, peas, and carrots in puree form are all good for your baby when she has a fever.
You can choose which fruit or vegetable you want to give your baby according to her preferences. Apples, peas, and carrots in puree form are all good for your baby when she has a fever.
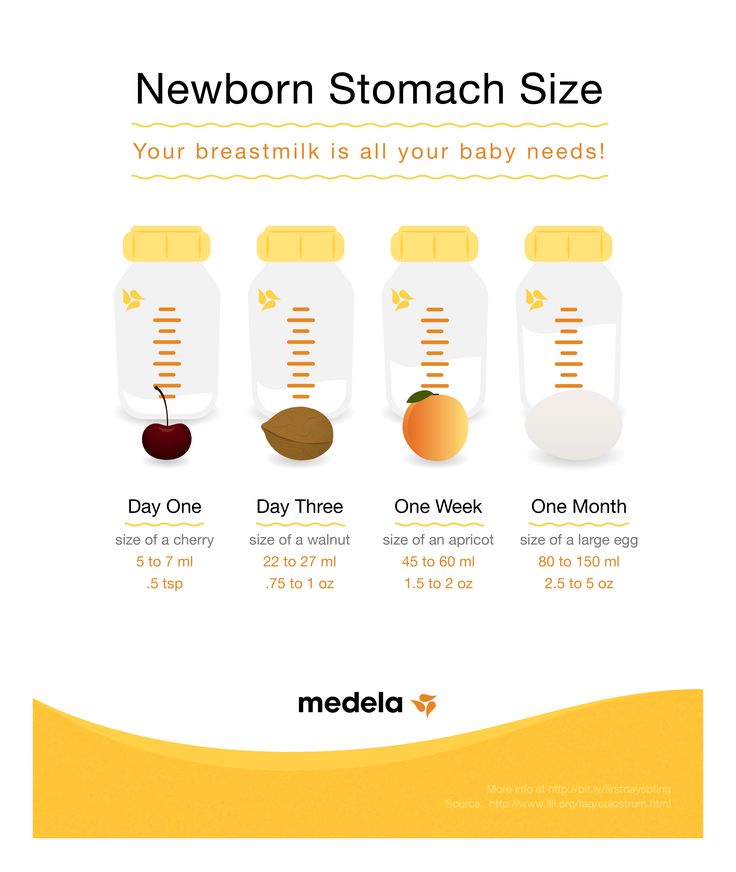
5. Breast Milk or Formula
Sometimes, your baby might want to go back to feeding entirely on breast milk or formula. As breast milk and formula are high in nutrition and also make sure that your baby stays hydrated during the fever, do not hesitate to offer some to her. Breast milk, in particular, contains antibodies that help build your baby’s immunity that help fight infection.
6. Popsicles
This is a unique way to get your baby to eat nutritious food – just ensure you make this yourself at home with ingredients that you know are safe. Juice a few fruits and put them in a popsicle mould. You can also add a few pieces of cut-up fruits into the mould. Freeze it for a few hours and let your baby enjoy this cold treat that is full of vitamins. Note: Please don’t give store-bought popsicles to your baby as they are high in sugar and contain artificial colours, which aren’t good.
Note: Please don’t give store-bought popsicles to your baby as they are high in sugar and contain artificial colours, which aren’t good.
7. Ginger Tea
This simple drink will boost your baby’s immunity. Ginger has been known to have high antioxidant properties. It also helps clear chest congestions. Boil some ginger in a cup of water for a few minutes. Strain it and let it cool till it is warm. Feed the beverage to your child.
8. Ajwain
Carom seeds are truly a superfood when it comes to treating illnesses. Soak some seeds overnight in a cup of water or just boil them in water for a few minutes and give your baby a couple of teaspoons every few hours.
5 Foods for Toddlers With Fever (Age: 1-3 years)
While fighting the fever can leave your toddler without her usual appetite, it is important that your child gets nutritious food packed with vitamins that will keep her hydrated. You might be wondering what foods to give a toddler with fever as they can be picky – here are a few things you must feed your child when she has a fever.
1. BRAT Diet
This stands for banana, rice, applesauce, and toast. You should be able to make these food items easily at home. Bananas can be offered just as is. For the applesauce, you will need to peel a few apples, slice them and boil in some water until it becomes syrupy. You can add in cinnamon and star anise for added nutrition and flavour. Remember to take the whole spices out of the applesauce before feeding it to your child.
2. CRAM Diet
This stands for cereal, rice, applesauce and milk. Depending on what your child likes, you can choose between the two diets in order to ensure that your child is getting every bit of nutrition she requires to get better.
3. Chicken Soup
Almost everyone will tell you the virtues of chicken soup during sickness. Chicken soup is beneficial for a fever-ridden baby as it is easy on the stomach and rich in proteins and other nutrients. Chicken soup with added vegetables will give your child a balanced meal with ample nutrition.
4. Baked/Steamed Food
Baking and steaming food will ensure that the nutrition of the food remains intact without the use of oil and butter, two things that can cause a strain on your child’s system. You can bake or steam a variety of food – vegetables like peas, carrots and sweet potatoes are ideal. If your child feels up to it, you can give her baked or steamed fish as well.
5. Turmeric Milk
A lot has been said and written about the health benefits of turmeric. While you can add turmeric to the food that you prepare for your child, it is also recommended that you add a pinch of turmeric in a glass of warm milk and give this drink to your child once a day. Turmeric has medicinal and anti-inflammatory properties that will boost your child’s immune system.
Tips for Feeding Your Child During Fever
- Break down the meals into small portions that you can feed your child at frequent and regular intervals.

- You can express breast milk and feed it to your baby with a spoon, especially if your baby is too weak to suckle.
- Exercise patience when feeding your child when she is sick. Offer food on a regular basis and try to give the food she enjoys.
- Keep your child upright when you are feeding her. Do not feed her when she is lying down, as it may cause her to choke.
- Do not force your child to eat.
- Offer fluids if your baby is vomiting.
When to Call a Doctor
If your baby is suffering from other symptoms aside from fever, it’s best to take her to the paediatrician immediately. Some of the symptoms to look out for are:
- Unexplained rashes
- Vomiting
- Diarrhoea
- Unusually sleepy, fussy, or ill
- Seizures
It is important that you give your child food that is nutritious and energy-giving when they are suffering from fever. Be patient and offer food in small quantities over frequent meals. If your child is not eating at all, then you must seek medical help as this lack of appetite could be indicative of something more serious than a fever.
If your child is not eating at all, then you must seek medical help as this lack of appetite could be indicative of something more serious than a fever.
Also Read: The Best Home Remedies for Fever in Children
Fever Food Chart for Babies and Toddlers
| | by Dr Hemapriya
Little children can get particularly fussy during fever, but they still need their nutrition. Get help from our Fever Food Chart for Babies and Toddlers.
Fever Food Chart for Babies and Toddlers
6 Months Fever Food Chart
7 Months Fever Food Chart
8 Months Fever Food Chart
9 Months Fever Food Chart
10 Months Fever Food Chart
11 Months Fever Food Chart
Fever Food Chart for Toddlers (Above One Year)
Tips for Feeding Your Child During Fever
Buy Healthy Nutritious Baby, Toddler food made by our own Doctor Mom !
We all get sick, and when we do, the first thing we want is our Moms! It’s the same with our children, and along with our presence, another important thing they need is nutrition. However, that is easier said than done, considering kids don’t have the appetite to eat anything when they’re sick. Some children may also feel nauseous, which makes it even more challenging to hold food down.
However, that is easier said than done, considering kids don’t have the appetite to eat anything when they’re sick. Some children may also feel nauseous, which makes it even more challenging to hold food down.
That’s why it’s important to choose foods carefully during a fever. The foods we choose should be able to fight the infection by boosting immunity, and it should also provide enough energy to get through this phase. Sufficient fluid intake is also important to prevent dehydration.
Considering all this, breast milk is one of the best foods to feed during a fever. It’s got enough calories and liquid, and it also contains antibodies that help your little one fight the fever. It also offers comfort at a time your baby needs it the most. Along with this, you can add some supplementary solids when your baby is over 6 months.
During a fever, babies can only eat a little, so it’s important to make that little count, in terms of calories and nutrients. Here are food charts for every age, covering all the meals of the day for 5 days. Hopefully by the end of this period, your little one should be up and have an appetite to eat all her favorite foods!
Hopefully by the end of this period, your little one should be up and have an appetite to eat all her favorite foods!
Important Note: Please remember that these food charts are only for guidance and not a substitute for medical advice. Breast milk is the best food for babies, so breast feed whenever your baby wants. The WHO recommends exclusive breastfeeding for babies under 6 months.
6 Months Fever Food Chart
7 Months Fever Food Chart
8 Months Fever Food Chart
9 Months Fever Food Chart
10 Months Fever Food Chart
11 Months Fever Food Chart
Fever Food Chart for Toddlers (Above One Year)
Tips for Feeding Your Child During Fever
- If your baby is too weak and tired to suck, express some breast milk and feed with a spoon
- Choose foods with more calorie content to avoid losing weight
- Keep the focus on protein, with foods like milk, dal and eggs or chicken
- Avoid oily, spicy and high fiber foods since they can be difficult to digest
- Cut down on butter, ghee and fried foods as well as soups with cream
- Offer only small quantities at a time, and offer them at more frequent and regular intervals
- Don’t force the child to eat, and stick to fluids in case of vomiting
- Maintain an upright position when feeding the child; don’t feed when lying down
- For toddlers, offer liquids like ginger tea or ajwain water throughout the day
Basically, just feed your baby whatever she likes, which may include fluids, soft solids and as much breast milk as she wants.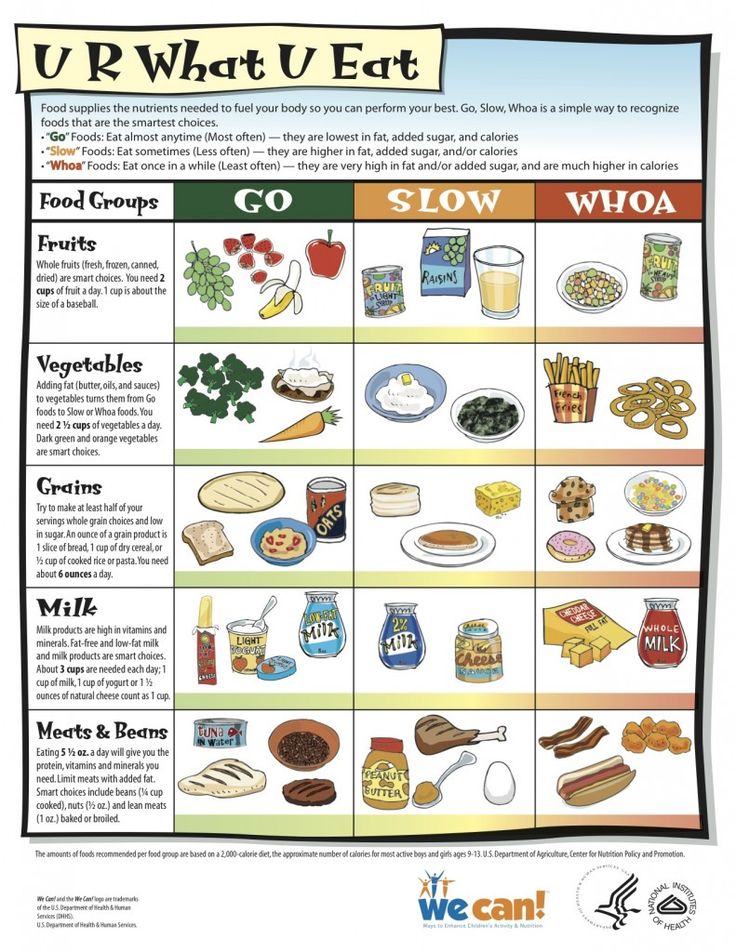 Most children recover their appetites once the fever passes, and they often eat more to makeup for what they lost during the fever. This is the body’s natural process, so there’s no need to worry too much. However, if the child is not eating at all, get medical help.
Most children recover their appetites once the fever passes, and they often eat more to makeup for what they lost during the fever. This is the body’s natural process, so there’s no need to worry too much. However, if the child is not eating at all, get medical help.
Buy Healthy Nutritious Baby, Toddler food made by our own Doctor Mom !
Shop now!REMINDER FOR PARENTS
Child has fever. What to do?
1 If your child's temperature suddenly rises (he was still healthy an hour ago), do not panic. As a rule, this is an acute respiratory disease, because it is ARI that makes up about 90% of childhood infections.
2. If the day before the child already had symptoms of infection (malaise, runny nose, sore throat, cough, voice change, moderate pain in the abdomen), then this is most likely a manifestation of the child's body's protective reaction to this infection .
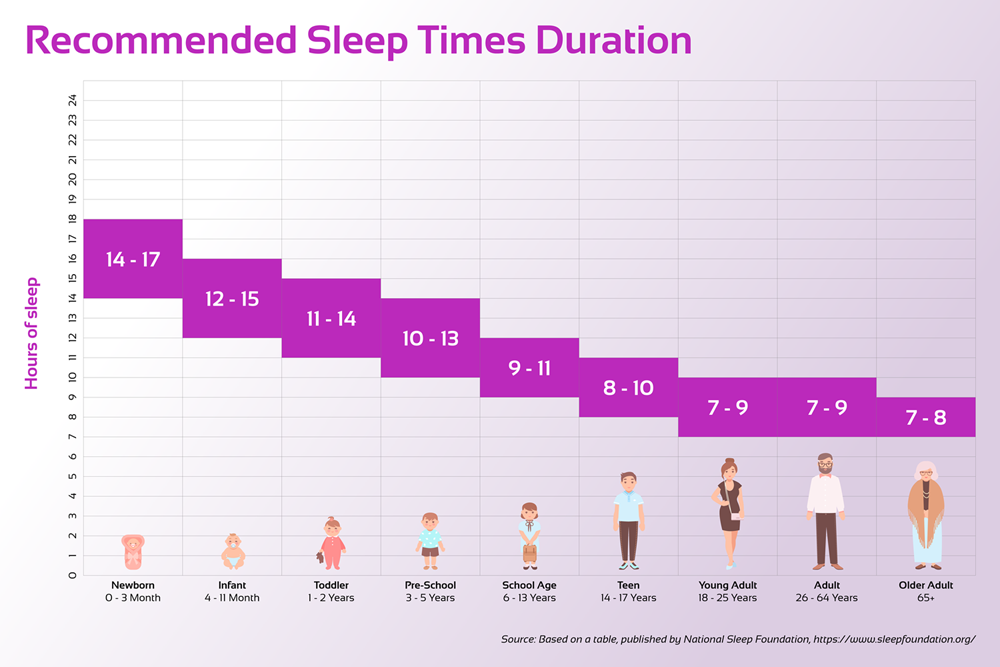
3. If the child tolerates elevated body temperature well up to 39-39.60, is older than 6 months, and does not have serious concomitant diseases, then do not rush to reduce it. Make sure your child has enough to drink for adequate perspiration (drinking temperature should be around body temperature for rapid absorption). The air in the room should be cool (18-200) to cool the upper respiratory tract, as well as the entire body of the child. Under no circumstances should babies be wrapped.
If the child tolerates elevated body temperature well up to 39-39.60, is older than 6 months, and does not have serious concomitant diseases, then do not rush to reduce it. Make sure your child has enough to drink for adequate perspiration (drinking temperature should be around body temperature for rapid absorption). The air in the room should be cool (18-200) to cool the upper respiratory tract, as well as the entire body of the child. Under no circumstances should babies be wrapped.
4. If the child does not tolerate fever or has a severe concomitant pathology, we begin to reduce the temperature, or rather, we strive to improve the child's well-being. For this, a decrease in temperature to the norm is not required (remember the protective role of elevated temperature). We use drugs ibuprofen and paracetamol (trade names may be different) approved for children in the Russian Federation in the form of syrups, drops, suppositories and tablets. The main thing is not to exceed the recommended daily dose of the drug. To improve well-being, the minimum dose of the drug indicated in the instructions may be sufficient. Typically, drug-resistant fevers are associated with the child's inability to sweat (drinks little or the child has a "pale" type of fever).
To improve well-being, the minimum dose of the drug indicated in the instructions may be sufficient. Typically, drug-resistant fevers are associated with the child's inability to sweat (drinks little or the child has a "pale" type of fever).
What should not be done when the temperature is high?
• Do not wrap up the child
• If he is pale and his extremities are cool ("pale" type of fever), do not use ice and cold water for cooling
• Do not use aspirin, analgin, etc., to reduce body temperature, drugs not approved for fever in children
How soon should the child be seen by a doctor?
If the child's health does not suffer (especially after the temperature drops), you can see a doctor the next day. The best option would be to go directly to the clinic at the place of residence, then the doctor will have the opportunity to timely conduct laboratory and instrumental examinations. Call an ambulance if your child has the following symptoms:
• Severe pallor, discoloration of the skin pattern, acute bluish-purple rash
• The child is very lethargic and refuses to drink, the child loses fluid with vomiting or loose stools
• The child has heavy groaning breathing, difficulty inhaling or exhaling
• A child under 3 years of age has no other symptoms of the disease, and the state of health suffers
• Severe pain in the abdomen, especially if they are accompanied by pallor and sweating
• The child has confusion, delirium, convulsions, headache with vomiting
• Fever of 400 and above, which cannot be reduced by 1-2 degrees after the use of antipyretics at the recommended dose and physical cooling methods
• The child's condition worsens, does not looking at a decrease in temperature
Fever in children: pediatric tactics
Article published on p. 88-94
88-94
An increase in body temperature is one of the most common reasons parents turn to a pediatrician. Fever as a symptom can accompany many diseases and conditions. Unfortunately, often an increase in body temperature is treated as a disease, and not as a symptom, carrying out therapeutic measures without taking into account the underlying disease. At the same time, fever is a nonspecific protective and adaptive reaction that occurs in response to exposure to various pathogenic stimuli and is associated with metabolic, endocrine, neurological, and immune changes in the body, which leads to a restructuring of thermoregulation processes.
Fluctuations in body temperature in a healthy child during the day are possible within 0.5–1.0 °C. Usually, when measured in the armpit, a body temperature of 37.0 ° C and above is considered elevated. However, in some cases, values up to 37.5 °C can be considered normal [1].
Numerous surveys show that more than 90% of parents are sure that fever can cause side effects, and about 20% are convinced that a fever of 39 °C and above is fraught with brain tissue damage [2, 3]. A similar opinion was noted even among experienced nurses in pediatric intensive care units [4, 5].
A similar opinion was noted even among experienced nurses in pediatric intensive care units [4, 5].
Since fever is a non-specific reaction of the body, the causes that cause it are very diverse. The most common fever occurs in infectious diseases. Fever of infectious origin develops in response to the effects of viruses, bacteria and their decay products. But at the same time, it plays an important role in protecting against infections. In animal models, an increase in mortality from infection with suppression of fever has been demonstrated [6].
Under the influence of moderate fever, the synthesis of interferons, proteins of the acute phase of inflammation, and leukopoiesis are enhanced [7]. Most microbes limit their ability to reproduce when the body temperature rises [8, 9]. Data have been obtained indicating that fever is associated with a better prognosis in severe bacterial infections [10]. In addition, antipyretic therapy reduces important markers of worsening disease, which may delay necessary diagnostic tests and changes in antimicrobial therapy.
However, an increase in temperature can play an adaptive role only when it rises to a certain limit. At high hyperthermia (40–41 °C), there is an activation of the intensity of metabolic processes. Despite the increased work of the respiratory and cardiovascular systems, with a rise in body temperature per degree above 37 ° C, the respiratory rate increases by 4 per 1 min, heart rate - by 10-20 per 1 min. At the same time, the increased delivery of oxygen may not meet the growing needs of tissues in it. This leads to the development of tissue hypoxia and disruption of the distribution of vascular tone. First of all, the functions of the central nervous system suffer. In this regard, with hyperthermia, the development of cerebral edema with inhibition of the functions of the central nervous system, the occurrence of febrile seizures, especially in young children with perinatal CNS damage, is possible [11]. In children with malnutrition, respiratory failure, adverse health effects can develop with a relatively moderate degree of body temperature increase (38. 5–39°C). In addition, fever is more dangerous for children of the first three months.
5–39°C). In addition, fever is more dangerous for children of the first three months.
In typical cases in acute infectious diseases, the most favorable form is a moderate increase in body temperature - up to 38–39.9 ° C, while its absence, subfebrile condition (37–37.9 ° C) or hyperpyrexia (41 ° C and above) indicate about reduced reactivity or about the severity of the disease. With a typical development of a febrile reaction, the evening body temperature (at 17–20 h) exceeds the morning one (at 4–6 h) within 1 ° C.
Information about the characteristics and dynamics of fever throughout the course of the disease is of great diagnostic value. With various diseases, febrile reactions can proceed in different ways, which is reflected in the forms of temperature curves.
Clinical variants of fever
First of all, it is necessary to assess the clinical signs of the correspondence of heat transfer processes to an increased level of heat production, since depending on the individual characteristics of the organism, fever, even with the same degree of increase in body temperature in children, can proceed in different ways. With an adequate reaction of the child to an increase in body temperature, heat transfer corresponds to increased heat production, which is clinically manifested by normal health, pink or moderately hyperemic skin color, moist and warm to the touch (“pink” fever). Tachycardia and increased respiration correspond to the level of body temperature, the recto-digital gradient does not exceed 5–6 °C. This variant of fever is considered to be prognostically favorable and often does not require the use of antipyretics [12].
With an adequate reaction of the child to an increase in body temperature, heat transfer corresponds to increased heat production, which is clinically manifested by normal health, pink or moderately hyperemic skin color, moist and warm to the touch (“pink” fever). Tachycardia and increased respiration correspond to the level of body temperature, the recto-digital gradient does not exceed 5–6 °C. This variant of fever is considered to be prognostically favorable and often does not require the use of antipyretics [12].
If the child’s reaction to an increase in body temperature is inadequate and heat transfer is significantly less than heat production, then clinically there is a pronounced violation of the child’s condition and well-being, chills, pale, “marble” skin, nail beds and lips with a cyanotic tint, cold feet and palms (“pale” fever). The leading pathogenetic link of "pale" fever is excessive hypercatecholaminemia, leading to the appearance of clinical signs of centralization of blood circulation: pallor, dryness, "marbling" of the skin, cold extremities, tachycardia, increased systolic blood pressure, increased difference between axillary and rectal temperatures (up to 1 ° C and higher). Persistent preservation of hyperthermia, excessive tachycardia, shortness of breath are observed, delirium, convulsions are possible, a rectal-digital gradient is more than 6 ° C. In some cases, fever is accompanied by muscle tremors, that is, chills or a feeling of chilliness. Chills are observed in bacteremia of various origins, sepsis, protracted septic endocarditis, bacterial pneumonia, and meningococcal meningitis [13]. Such a course of fever is prognostically unfavorable and is a direct indication for emergency care. These children usually require antipyretic drugs in combination with vasodilators and antihistamines (or antipsychotics).
Persistent preservation of hyperthermia, excessive tachycardia, shortness of breath are observed, delirium, convulsions are possible, a rectal-digital gradient is more than 6 ° C. In some cases, fever is accompanied by muscle tremors, that is, chills or a feeling of chilliness. Chills are observed in bacteremia of various origins, sepsis, protracted septic endocarditis, bacterial pneumonia, and meningococcal meningitis [13]. Such a course of fever is prognostically unfavorable and is a direct indication for emergency care. These children usually require antipyretic drugs in combination with vasodilators and antihistamines (or antipsychotics).
One of the clinical variants of the unfavorable course of fever in young children is a hyperthermic state (hyperthermic syndrome), in most cases caused by infectious inflammation, which is accompanied by toxicosis. The hyperthermic syndrome is associated with disturbances in thermoregulatory control and occurs without an increase in the hypothalamic set point.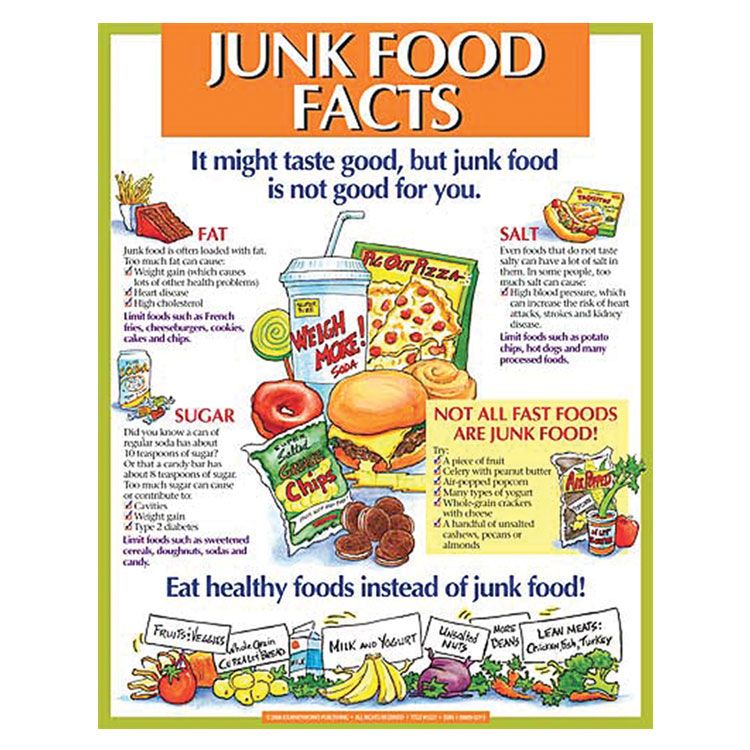 This condition is characterized by a persistent increase in body temperature in the absence of diurnal fluctuations characteristic of normal body temperature and fever, and a weak response to antipyretic drugs or its absence.
This condition is characterized by a persistent increase in body temperature in the absence of diurnal fluctuations characteristic of normal body temperature and fever, and a weak response to antipyretic drugs or its absence.
Hyperthermia may result from inadequate heat dissipation or excessive heat production without an adequate compensatory increase in heat output. For example, a young child who is left swaddled for a long time (or left in a car) may develop hyperthermia. In older children, hyperthermia may develop during intense exercise in a hot, humid environment.
In hyperthermic syndrome, there is a rapid and inadequate increase in body temperature, accompanied by impaired microcirculation, metabolic disorders, and progressively increasing dysfunction of vital organs and systems [14]. The risk of developing such conditions is especially high in young children, as well as those with a aggravated premorbid background. The younger the child's age, the more dangerous for him is a rapid and significant rise in body temperature due to the possible development of progressive metabolic disorders, cerebral edema, and impaired vital functions. If a child has serious diseases of the cardiovascular, respiratory systems, fever can lead to the development of their decompensation. In children with pathology of the central nervous system against the background of hyperthermia, the development of cerebral edema and convulsions with impaired functions of the respiratory and cardiovascular systems is possible.
If a child has serious diseases of the cardiovascular, respiratory systems, fever can lead to the development of their decompensation. In children with pathology of the central nervous system against the background of hyperthermia, the development of cerebral edema and convulsions with impaired functions of the respiratory and cardiovascular systems is possible.
Febrile convulsions are observed in 2-4% of children, more often at the age of 12-18 months. [fifteen]. Usually they occur with a rapid rise in temperature to 38-39 ° C and above at the very beginning of the disease. Repeated convulsions can develop in a child at other temperatures. Febrile convulsions in children are more often considered as a manifestation of CNS damage of various etiologies. The occurrence of febrile convulsions against the background of moderately febrile body temperature in children under one year and after 5 years, the absence of vegetative vascular reactions, the duration of convulsions for more than 10 minutes, the appearance of convulsions during sleep are an unfavorable factor in the course of the underlying disease, which requires a deep neurological examination.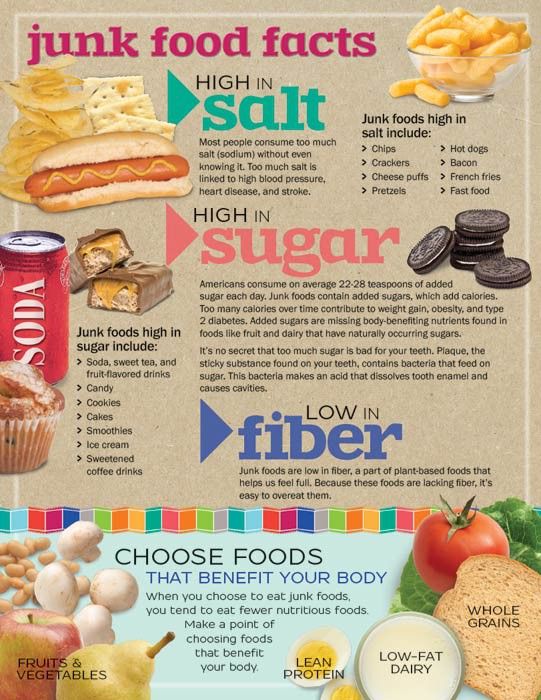 In infants with signs of rickets, a study of calcium levels is indicated to exclude spasmophilia.
In infants with signs of rickets, a study of calcium levels is indicated to exclude spasmophilia.
Thus, fever accompanies most diseases and is quite often a protective reaction. Therefore, reducing its level with the help of antipyretics is justified only in certain situations. Unfortunately, many parents (and doctors) consider fever the most dangerous manifestation of the disease and strive to normalize the temperature. According to our studies, more than 90% of children with acute respiratory viral infections receive antipyretics, including 72% of children with subfebrile temperature. Such tactics cannot be considered rational, since fever, as a component of the body's inflammatory response to infection, is largely protective.
Reducing the temperature during fever with the help of antipyretics does not affect its cause, they only transfer the setting of the “central thermostat” to a lower level . Moreover, antipyretics even prolong the period of virus shedding.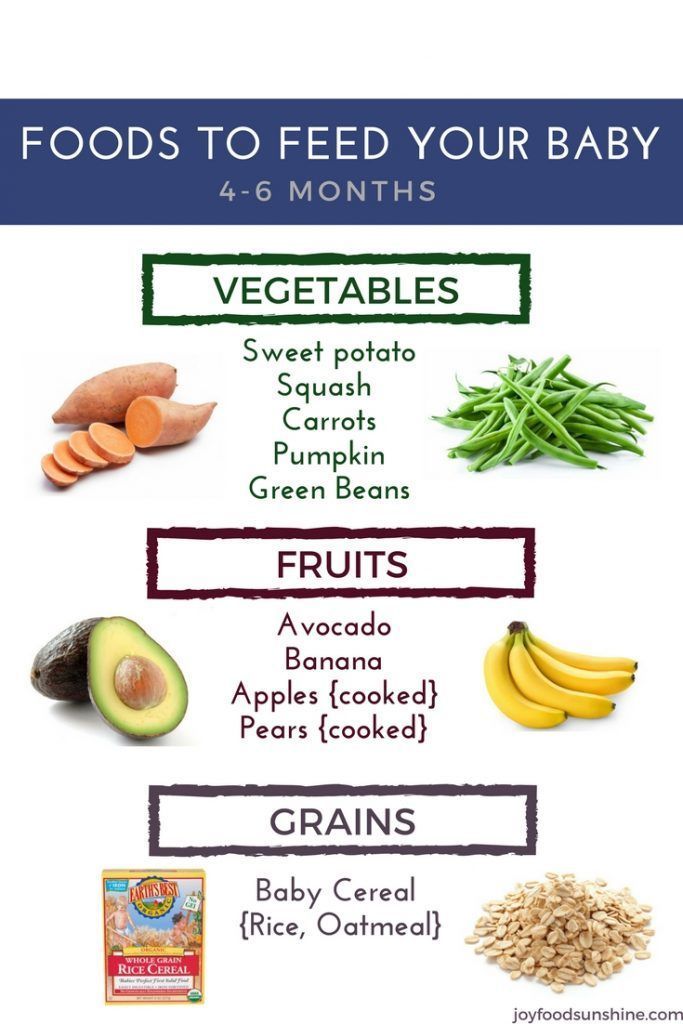 However, the increase in body temperature associated with hyperthermia must begin to be examined and treated immediately.
However, the increase in body temperature associated with hyperthermia must begin to be examined and treated immediately.
Body temperature must be reduced when it exceeds 38.5-39 ° C. But children under the age of 2 months, as well as those with perinatal encephalopathy, a history of convulsions and severe heart disease, need to constantly monitor their fever and prevent the temperature from rising above 38 ° C. Assign antipyretics in age doses. Children under 12 years of age are contraindicated in the use of acetylsalicylic acid in order to reduce temperature [16].
It should be noted that it is impossible to prescribe a regular (course) intake of an antipyretic drug! Its repeated dose can be used only after a new increase in temperature to the level indicated above. Antipyretics are not prescribed together with antibiotics, as this may mask the lack of effect of treatment and delay the change of antibiotic (with the exception of convulsions or impaired heat transfer). In children, the use of acetylsalicylic acid (aspirin) as an antipyretic is prohibited due to severe toxic effects and the development of Reye's syndrome. It is also forbidden to use analgin inside as an antipyretic because of the danger of agranulocytosis and persistent hypothermia.
In children, the use of acetylsalicylic acid (aspirin) as an antipyretic is prohibited due to severe toxic effects and the development of Reye's syndrome. It is also forbidden to use analgin inside as an antipyretic because of the danger of agranulocytosis and persistent hypothermia.
Before reducing body temperature, it is necessary to clearly understand what temperature fluctuations are acceptable in a healthy child (Table 1).
The standard area for measuring temperature in children in our country is the armpit. Abroad, it is customary to measure the body temperature of children under 5 years old in the rectum - then a fever is considered to be an increase of more than 38 ° C. At the same time, it must be remembered that body temperature measured in the armpit is 0.8–1 ° C, and oral temperature is 0.5–0.6 ° C lower than in the rectum. It should be remembered that within an hour after eating, intense physical effort, the body temperature may be subfebrile. The opinion that teething can cause fever is unfair, although on the day of the eruption of a milk tooth, body temperature can rise to subfebrile numbers in about half of the children.
Pharmacotherapy of fever
Pediatricians are always faced with the task of not only determining the cause of an increase in body temperature in a child, but also taking urgent measures to stop the fever. For this purpose, a wide variety of means are used, including physical and medical (antipyretics, steroids, etc.). However, in everyday practice, preference is given to drugs, primarily non-steroidal anti-inflammatory drugs (NSAIDs).
More than 100 years have passed since the synthesis of acetylsalicylic acid. Acetylsalicylic acid isolated in 1899, was the first drug that had not only antipyretic and analgesic, but also anti-inflammatory effect. And only in the second half of the 20th century, active anti-inflammatory drugs were discovered - various classes of weak acids, called non-steroidal anti-inflammatory drugs. In the clinic for the relief of fever, NSAIDs are most widely used, which inhibit the synthesis of prostaglandins from arachidonic acid.
Worldwide, more than 400 million people use NSAIDs every year. However, not all NSAIDs are equally effective and safe, therefore, in the treatment of febrile conditions in children, the choice of the drug is limited by its effectiveness and the presence of possible adverse side effects on the child. This is especially true because children with fevers are often treated at home and parents use antipyretics before the doctor arrives. The question arises: which drug to choose? At the same time, the drug must meet certain requirements for over-the-counter drugs: it must be effective, smoothly reduce the temperature, be safe, pleasant to the taste and have a prolonged action.
However, not all NSAIDs are equally effective and safe, therefore, in the treatment of febrile conditions in children, the choice of the drug is limited by its effectiveness and the presence of possible adverse side effects on the child. This is especially true because children with fevers are often treated at home and parents use antipyretics before the doctor arrives. The question arises: which drug to choose? At the same time, the drug must meet certain requirements for over-the-counter drugs: it must be effective, smoothly reduce the temperature, be safe, pleasant to the taste and have a prolonged action.
The mechanism of action of all antipyretics is to block the synthesis of prostaglandins along the cyclooxygenase pathway of inhibition of cyclooxygenase (COX) in the hypothalamus. It has been established that there are two COX isoenzymes. COX-2 is formed only during inflammatory processes under the influence of cytokines. During inflammation, the metabolism of arachidonic acid is significantly activated, the synthesis of prostaglandins, leukotrienes increases, biogenic amines, free radicals, NO, etc.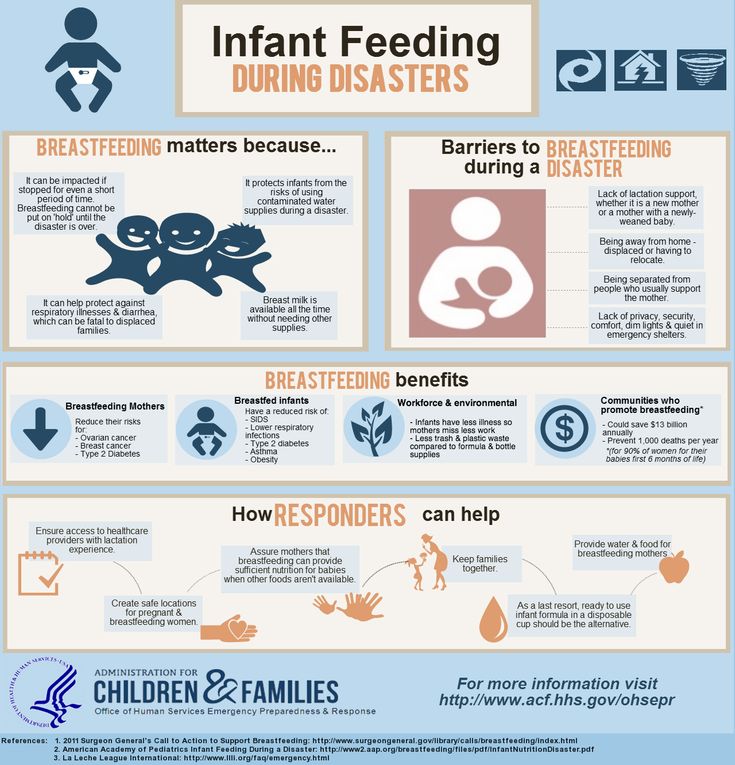 are released, which leads to the development of an early stage of inflammation. Blockade by analgesics-antipyretics COX-2 in the central nervous system allows you to achieve antipyretic and analgesic effect (central action), and a decrease in the content of prostaglandins at the site of inflammation - anti-inflammatory and, by reducing pain reception, analgesic action (peripheral action). At the same time, NSAIDs block the synthesis of prostaglandins that perform a protective function, therefore, against the background of the use of NSAIDs, severe side effects may develop: gastrointestinal bleeding, attacks of bronchial obstruction (aspirin bronchial asthma), acute renal failure, changes in bone marrow hematopoiesis up to a fatal agranulocytosis, Reye's syndrome and others [17, 18].
are released, which leads to the development of an early stage of inflammation. Blockade by analgesics-antipyretics COX-2 in the central nervous system allows you to achieve antipyretic and analgesic effect (central action), and a decrease in the content of prostaglandins at the site of inflammation - anti-inflammatory and, by reducing pain reception, analgesic action (peripheral action). At the same time, NSAIDs block the synthesis of prostaglandins that perform a protective function, therefore, against the background of the use of NSAIDs, severe side effects may develop: gastrointestinal bleeding, attacks of bronchial obstruction (aspirin bronchial asthma), acute renal failure, changes in bone marrow hematopoiesis up to a fatal agranulocytosis, Reye's syndrome and others [17, 18].
Therefore, not all NSAIDs are equal in terms of safety and efficacy. Thus, according to WHO materials, metamizole sodium (analgin) has been withdrawn from the pharmaceutical market in more than 30 countries or its use is sharply limited and strictly controlled.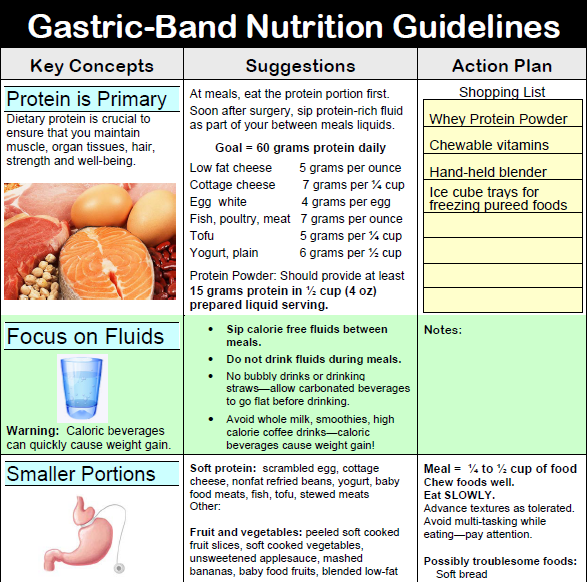 This decision was largely based on data from the International Agranulocytosis and Aplastic Anemia Study IAAAS, conducted in 8 medical centers in seven countries from 1980 to 1986 and showed a high risk of developing agranulocytosis when taking analgin. However, in urgent situations, such as hyperthermic syndrome, parenteral use of analgin and metamizole-containing drugs is also acceptable in children.
This decision was largely based on data from the International Agranulocytosis and Aplastic Anemia Study IAAAS, conducted in 8 medical centers in seven countries from 1980 to 1986 and showed a high risk of developing agranulocytosis when taking analgin. However, in urgent situations, such as hyperthermic syndrome, parenteral use of analgin and metamizole-containing drugs is also acceptable in children.
The use of nimesulide is unacceptable due to its hepatotoxicity [19–21]. Today, nimesulide and its generics are not recommended as antipyretics for children under 12 years of age. Phenacetin is also excluded from the list of antipyretics due to toxicity. The latter, unfortunately, is part of the cefecon suppositories, and amidopyrine is cefecon-M. It is dangerous to use these suppositories in the treatment of children.
The recommended rate of temperature decrease is 1–1.5 °C in 30–60 minutes. The duration of the use of antipyretics is no more than 3 days.
Diet. Any febrile child should be given additional fluids to prevent dehydration, which occurs easily in children due to increased breathing and increased sweating. For children older than a year, additional liquid is given in the form of berry and fruit fruit drinks, decoctions, juices. Dietary restrictions are determined by the nature of the disease, premorbid background, but even with a sharply reduced appetite, easily digestible carbohydrates are advisable. Avoid spicy foods, hard-to-digest foods, canned foods. Food should be chemically, mechanically and thermally gentle.
Any febrile child should be given additional fluids to prevent dehydration, which occurs easily in children due to increased breathing and increased sweating. For children older than a year, additional liquid is given in the form of berry and fruit fruit drinks, decoctions, juices. Dietary restrictions are determined by the nature of the disease, premorbid background, but even with a sharply reduced appetite, easily digestible carbohydrates are advisable. Avoid spicy foods, hard-to-digest foods, canned foods. Food should be chemically, mechanically and thermally gentle.
Physical methods of cooling increase the release of heat from the surface of the body, and they are usually used at body temperatures above 39 ° C - sponging with a sponge moistened with water at a temperature of 30-32 ° C for 5 minutes every half hour (4-5 times). Physical methods of cooling are not used if the child has signs of microcirculation disorders (fever of the "pale" type). With great care, physical methods of cooling should be used for febrile convulsions against the background of hyperthermia.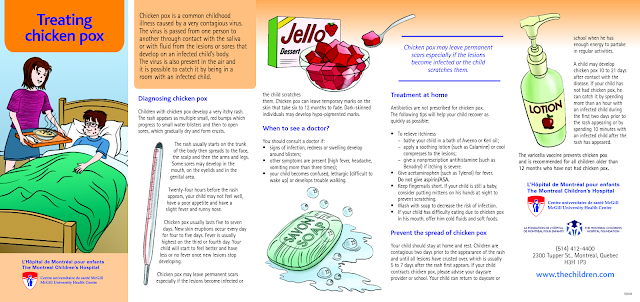 Although convulsions are provoked by high temperature, cold baths, rubbing with alcohol, the use of fans, enemas, gastric lavage with cold water and other similar procedures are contraindicated, as they can provoke the development of a convulsive syndrome in a child. Physical cooling of the head helps to a greater extent.
Although convulsions are provoked by high temperature, cold baths, rubbing with alcohol, the use of fans, enemas, gastric lavage with cold water and other similar procedures are contraindicated, as they can provoke the development of a convulsive syndrome in a child. Physical cooling of the head helps to a greater extent.
In children at risk, especially young children, antipyretic therapy should be started.
Guidelines for the selection of antipyretics in children
Antipyretics are most commonly used in children compared to other drugs, so they are chosen primarily for safety rather than efficacy. Currently, only ibuprofen and paracetamol fully meet the criteria for high efficacy and safety. They are officially recommended by the World Health Organization and national programs as antipyretics in pediatric practice [17, 18, 22].
Ibuprofen, synthesized in 1962, is rightfully considered the leader in the relief of fever in children. Ibuprofen (Nurofen, Nurofen suspension for children, ibufen, etc. ) has a pronounced antipyretic, analgesic and anti-inflammatory effect. Ibuprofen blocks COX both in the CNS and in the focus of inflammation (peripheral mechanism), which determines not only its antipyretic, but also a significant anti-inflammatory effect [23, 24].
) has a pronounced antipyretic, analgesic and anti-inflammatory effect. Ibuprofen blocks COX both in the CNS and in the focus of inflammation (peripheral mechanism), which determines not only its antipyretic, but also a significant anti-inflammatory effect [23, 24].
As a result, the phagocytic production of mediators of the acute phase, including IL-1 (endogenous pyrogen), decreases. Ibuprofen has a dual analgesic effect - peripheral and central. The analgesic effect is already manifested at a dose of 5 mg / kg and is more pronounced than that of paracetamol. This allows you to effectively use ibuprofen for mild to moderate sore throat, pain with tonsillitis, acute otitis media, toothache. The antipyretic effect of ibuprofen at a dose of 7.5 mg/kg is higher than that of paracetamol at a dose of 10 mg/kg and acetylsalicylic acid at a dose of 10 mg/kg. This is manifested by a large decrease in temperature after 4 hours, which was also observed in a larger number of children [25, 26].
Paracetamol (acetaminophen, tylenol) has antipyretic, analgesic and slight anti-inflammatory effects, tk. blocks COX and prostaglandin synthesis mainly in the central nervous system, in the hypothalamus, without having a peripheral effect. It does not relieve intense pain or pain of visceral origin associated with spasm of smooth muscles.
Ibuprofen can be prescribed to children from the age of three months. Recommended single doses of ibuprofen are 5–10 mg/kg. Repeated use of ibuprofen is possible not earlier than after 4–5 hours, but not more than 4 times a day [27, 28].
In 1990, the first original ibuprofen called Nurofen ® and Nurofen ® Suspension specially designed for children appeared on the European market. Before Nurofen ® Suspension for Children was launched on the international market, a study of side effects of the drug was conducted (Lesko S., Mitchell A., 1995), during which more than 80,000 children were examined. The results indicate that the good safety profile of the drug allows it to be widely used in pediatric practice. In addition, comparisons of ibuprofen with paracetamol show significant benefits. Thus, when using ibuprofen at a dose of 10 mg/kg, in comparison with a similar dose of paracetamol, a more effective temperature reduction is achieved and a longer (up to 8 hours) antipyretic effect is noted [17, 21]. In addition, paracetamol does not significantly affect the course of the disease itself, since it does not have an anti-inflammatory effect. It should be noted that Nurofen for children has good taste and is well tolerated by children of all ages. There are no side effects from the digestive organs, the development of allergic reactions, the intensification or provocation of bronchospasm when using Nurofen.
The results indicate that the good safety profile of the drug allows it to be widely used in pediatric practice. In addition, comparisons of ibuprofen with paracetamol show significant benefits. Thus, when using ibuprofen at a dose of 10 mg/kg, in comparison with a similar dose of paracetamol, a more effective temperature reduction is achieved and a longer (up to 8 hours) antipyretic effect is noted [17, 21]. In addition, paracetamol does not significantly affect the course of the disease itself, since it does not have an anti-inflammatory effect. It should be noted that Nurofen for children has good taste and is well tolerated by children of all ages. There are no side effects from the digestive organs, the development of allergic reactions, the intensification or provocation of bronchospasm when using Nurofen.
However, it is known that children on the background of fever and intoxication often refuse not only food, but also oral medication. In these cases, as well as when it is impossible to take drugs inside - with nausea, vomiting, swallowing disorders, in children with regurgitation syndrome or in the postoperative period - it is advisable to use rectal suppositories. In addition, in rectal suppositories, the drug is mixed with a low-melting substance that is highly soluble in the rectum, which allows the active principle of the drug to be rapidly absorbed. This method of drug delivery also determines the greater accuracy of drug dosing. Very often, suppositories are used in combination therapy: during the day, the patient receives tablets or suspension, and at night - suppositories, which creates the best therapeutic effect. Therefore, the emergence of a new over-the-counter form of ibuprofen - Nurofen for children rectal suppositories significantly expanded the possibility of using ibuprofen in children [29]. Nurofen for children rectal suppositories is allowed for non-prescription use from 3 months of life in a single dose of 5-10 mg/kg of body weight, if necessary - 3 times a day (no more than 30 mg per 1 kg of body weight of a child per day).
In addition, in rectal suppositories, the drug is mixed with a low-melting substance that is highly soluble in the rectum, which allows the active principle of the drug to be rapidly absorbed. This method of drug delivery also determines the greater accuracy of drug dosing. Very often, suppositories are used in combination therapy: during the day, the patient receives tablets or suspension, and at night - suppositories, which creates the best therapeutic effect. Therefore, the emergence of a new over-the-counter form of ibuprofen - Nurofen for children rectal suppositories significantly expanded the possibility of using ibuprofen in children [29]. Nurofen for children rectal suppositories is allowed for non-prescription use from 3 months of life in a single dose of 5-10 mg/kg of body weight, if necessary - 3 times a day (no more than 30 mg per 1 kg of body weight of a child per day).
E.E. Lokshina et al. [29] conducted a multicenter open controlled study to assess the clinical efficacy, tolerability and safety of Nurofen for children rectal suppositories in the treatment of hyperthermic conditions in children with acute respiratory infections. The results of the use of Nurofen for children rectal suppositories in the relief of fever in patients aged 3 months to 2 years with manifestations of acute respiratory disease (acute nasopharyngitis, laryngitis, laryngotracheitis, tracheobronchitis, bronchitis) were compared with data on the use of paracetamol rectal suppositories for the same purpose.
The results of the use of Nurofen for children rectal suppositories in the relief of fever in patients aged 3 months to 2 years with manifestations of acute respiratory disease (acute nasopharyngitis, laryngitis, laryngotracheitis, tracheobronchitis, bronchitis) were compared with data on the use of paracetamol rectal suppositories for the same purpose.
Assessing the effectiveness of the use of antipyretic drugs in the observed groups, the authors state that ibuprofen is more effective than paracetamol during the first 6 hours after use: a persistent decrease in temperature during the first 6 hours of the disease was observed in 44% of children who received Nurofen, and in 27.5% treated with paracetamol [29]. Intoxication and pain syndrome stopped almost twice as fast in the group of children who received Nurofen rectal suppositories for children. Also, in children of this group, a significant reduction in the duration of fever was observed. When using the drug Nurofen for children, rectal suppositories were twice less likely to require the use of parenteral antipyretics.
Thus, due to the high efficiency and safety of Nurofen for children, rectal suppositories are recommended for the treatment of fever and pain, including teething, in young children, both in a hospital and emergency room, and on an outpatient basis.
In children with "pale" fever with hyperthermic syndrome, that is, pronounced clinical signs of centralization of blood circulation with microcirculation disorders, the use of NSAIDs to reduce body temperature is either ineffective or insufficiently effective. Such children are prescribed drugs from the group of phenothiazines (pipolphen, diprazine, propazine) at a dose of 0.25 mg / kg (single dose), sometimes in combination with droperidol (0.05–0.1 ml of a 0.1% solution per 1 kg of body weight). body per injection), every 6-8 hours. These drugs reduce the excitability of the central nervous system, dilate peripheral vessels, thus eliminating microcirculation disorders and increasing sweat output. They are used intravenously or intramuscularly. As a first appointment for children with clinical signs of centralization of blood circulation, a combination of drugs such as papaverine and dibazol can also be used (for young children - 0.2 ml / year of life per administration, for older children - 0.1 ml / year of life per administration, with frequency of administration no more than 3-4 times a day). Often, in these conditions, vasodilators are prescribed - nicotinic acid at a dose of 1 mg / kg per reception simultaneously with NSAIDs. The inefficiency of the double dose of drugs may be an indication for the intramuscular administration of pipolfen and droperidol at the above doses. Steroid hormones have a powerful antipyretic effect (prednisolone 1-2 mg / kg / day divided into 2-3 doses).
They are used intravenously or intramuscularly. As a first appointment for children with clinical signs of centralization of blood circulation, a combination of drugs such as papaverine and dibazol can also be used (for young children - 0.2 ml / year of life per administration, for older children - 0.1 ml / year of life per administration, with frequency of administration no more than 3-4 times a day). Often, in these conditions, vasodilators are prescribed - nicotinic acid at a dose of 1 mg / kg per reception simultaneously with NSAIDs. The inefficiency of the double dose of drugs may be an indication for the intramuscular administration of pipolfen and droperidol at the above doses. Steroid hormones have a powerful antipyretic effect (prednisolone 1-2 mg / kg / day divided into 2-3 doses).
With the phenomena of toxicosis and dehydration, the relief of hyperthermia is impossible without adequate replenishment of the fluid balance. The volume of enteral and infusion fluid therapy depends in each individual case on losses, needs, degree of dehydration and intoxication.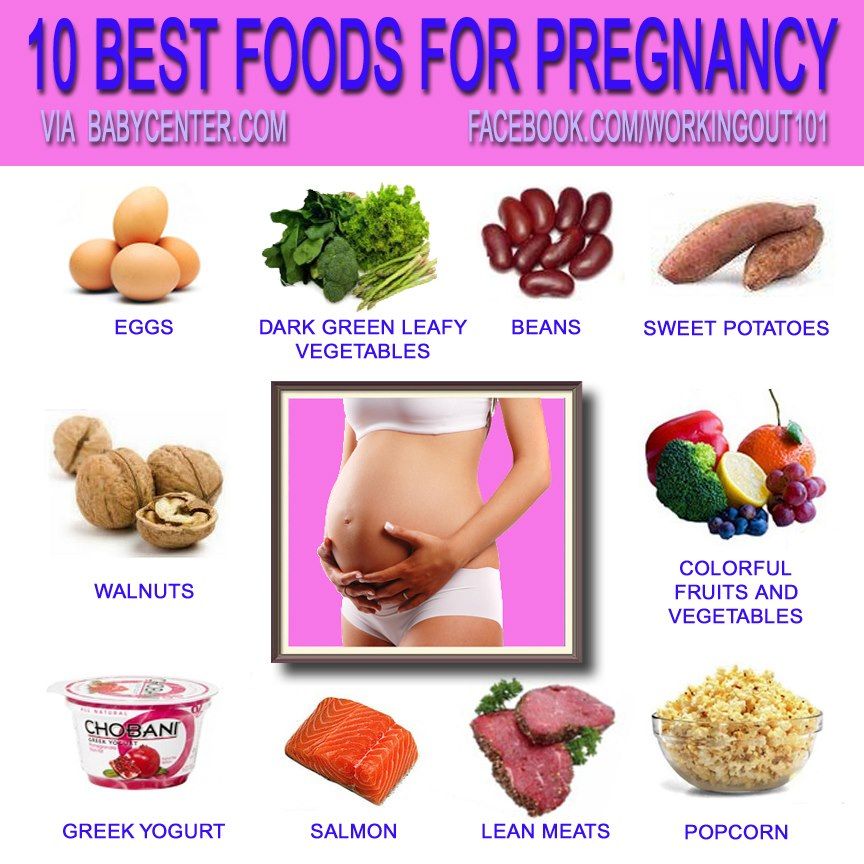
Post-vaccination reactions - the expected conditions specified in the instructions for use of vaccines. They are quite common, they should not be confused with complications of vaccination, the development of which is most often unpredictable and reflects the individual reaction of the child or a violation of the vaccination technique. A well-known post-vaccination reaction in children is hyperthermia after immunization. In addition, hyperemia, swelling, pain of moderate intensity at the injection site may appear at the injection site, which is also sometimes accompanied by fever, malaise and headache. Hyperthermia and local reactions after immunization are considered as indications for the appointment of ibuprofen [33]. Since post-vaccination reactions are predictable, it is appropriate to recommend ibuprofen or paracetamol to the child for prophylaxis during DTP vaccination within 1-2 days after vaccination.
Thus, antipyretic therapy in children should be prescribed strictly individually, taking into account clinical and anamnestic data. When prescribing any antipyretic, it is necessary to clearly determine the dose, avoid the use of combined preparations containing more than one antipyretic, understand the role of dehydration in vomiting, decreased fluid intake, and diarrhea. The course use of antipyretics without specifying the causes of fever is unacceptable. The drugs of choice for fever of infectious and inflammatory origin in children are ibuprofen and paracetamol (especially in young children).
When prescribing any antipyretic, it is necessary to clearly determine the dose, avoid the use of combined preparations containing more than one antipyretic, understand the role of dehydration in vomiting, decreased fluid intake, and diarrhea. The course use of antipyretics without specifying the causes of fever is unacceptable. The drugs of choice for fever of infectious and inflammatory origin in children are ibuprofen and paracetamol (especially in young children).
Bibliography
1. Goncharik I.I. Fever. - Minsk: Higher School, 1999. - 175 p.; Tatochenko V.K. Child with fever // Attending physician. - 2005. - No. 1. - S. 16–20.
2. Schmitt B.D. Fever phobia: Misconceptions of parents about fever // Am. J. Dis. child. - 1980. - 134. - 76.
3. Crocetti M., Moghbeli N., Serwint J. Fever phobia revisited: have parental misconceptions about fever changed in 20 years? // Pediatrics. - 2001. - 107. - 1241-6.
4. Kramer M. S., Naimark L., Leduc D.G. Parental fever phobia and its correlated // Pediatrics. - 1985. - 75. - 1110-3.
S., Naimark L., Leduc D.G. Parental fever phobia and its correlated // Pediatrics. - 1985. - 75. - 1110-3.
5. Poirier M.P., Davis P.H., Gonzalezdel Rey J.A., Monroe K.W. Pediatric emergency nurses’ perspectives on fever in children // Pediatr. Emerg. care. - 2000. - 16. - 9–12.
6. Bernheim H.A., Kluger M.J. Fever: Effect of drug-induced antipyresis on survival // Science. - 1976. - 193. - 237.
7. Lorin M.I. The Febrile Child: Clinical Management of Fever and Other Types of Pyrexia. — Wiley; New York, 1982.
8. Mayoral C.E., Marino R.V., Rosenfeld W., Greensher J. Alternating antipyretics: is this an alternative? // Pediatrics. - 2000. - 105. - 1009-12.
9. Jiang Q., Cross A.S., Singh I.S. et al. Febrile core temperature is essential for optimal host defense in bacterial peritonitis // Infect. Immun. - 2000. - 68. - 1265-70.
10. Kluger M.J., Kozak W., Conn C.A. et al. Role of fever in disease // Ann. NY Acad. sci. - 1998. - 856. - 224–33.
11. Goncharik I.I. Fever. - Minsk: Higher School, 1999. - 175 p.; Tsybulkin E.K. Fever: Threatening conditions in children. - St. Petersburg: Special Literature, 1994. - S. 153–157.
12. Balagangadhar R. Totapally M.D. Fever, "fever-phobia" and hyperthermia. What should a pediatrician know? // International Pediatrics. - 2005. - 20(2). - R. 95-103.
13. Hegglin R. Differential diagnosis of internal diseases: TRANS. with him. - M., 1997. - 121-126.
14. Korovina N.A., Zakharova I.N., Zaplatnikov A.L. Acute fever in children // RMJ. - 2005. - No. 17. - S. 1165-1170.
15. Tatochenko V.K. A child with a fever // Attending physician.—2005.—No. 1.—S. 16–20.
16. http://medstandart.net/browse/1273
17. V. P. Vetrov and V. V. Dlin. et al. Rational use of antipyretics in children: A guide for physicians. - M., 2002. - 23 p.
18. Korovina N.A., Zaplatnkov A.L. et al. Fever in children. Rational choice of antipyretic drugs: A guide for physicians. - M., 2000, - 67 p.
- M., 2000, - 67 p.
19. Red book 2000. Report of the Committee on Infectious diseases / Ed. by L.K. Pickering. — American Academy of Pediatrics. Elk Grove Village. Ill. 2000.
20. Tatochenko V.K. Rational use of antipyretics in children // Russian Medical Journal. - 2000. - No. 3. - S. 40–42.
21. Federal Guidelines for Physicians on the Use of Medicines (formulary system). - Issue. III. — M.: GEOTAR Medicine, 2002. — 462 p.
22. The management of fever in young children with acute respiratory infections in developing countries/WHO/ARI/93.90/, Geneva 1993.
23. Marushko Yu.V., Chef G.G. Nevidkladna pediatrics. - Kiev: FO-P Storozhuk O.V., 2011. - 352 p.
24. Kyllönen. Perioperative pharmacokinetics of ibuprofen en anti omersafter rectal administration /Kyllönen M., Olkkola K.T., Seppälä T., Ryhänen P. // Paediatr. Anaesth. - 2005. - Vol. 15 suppl. 7. - P. 566-573.
25. Beaver W.T. Review of the analgesic efficacy of ibuprofen / W.