Best food for baby with reflux
Feeding A Baby With Reflux | Parenting Blog | Babocush Limited
It may seem like it was just yesterday when you brought home your little bundle of joy then just like that, it’s time to wean your baby off of milk and introduce solid foods. This process might feel overwhelming, especially if your child is still experiencing baby reflux.
What are the symptoms of baby reflux?
It is important to note the symptoms. Repeated crying, vomiting or spitting up, arching of the back or neck during or after feeds, recurrent ear infections, incapacity to sleep or frequent waking, irritability and lastly, frequent hiccups. Babies typically grow out of reflux within the first two years of their life. With that being said, there are still some foods that can aggravate reflux and others that can ease it.
If your baby suffers with reflux, you may feel more comfortable consulting your doctor before you wean your baby off milk and transition them onto solid foods. As a general rule of thumb, you should avoid giving your baby solid food before they’re four months old.
It’s important that you start the weaning process with purees and baby led weaning.The best foods to feed a baby with reflux are purees of vegetables, particularly root vegetables like potatoes, carrots, pumpkin, swede, parsnips and sweet potato. You can also feed your baby any non-acidic fruits. You should avoid citrus fruits like oranges, apples and grapes, tomatoes, peppers, courgettes, cucumbers and aubergines. In addition to that, you should also avoid any foods that have cow’s milk proteins as well as spicy foods.
How to introduce solid foods?
By the time your little one is 4 to 6 months old, you'll probably have your breastfeeding or formula drill down to an art. However, don’t get too comfortable - your baby will soon be ready for "real" food. When it comes to giving your baby solid food, there are a few tips you can follow that can make the process much easier…
Wean your baby slowly
As a general rule of thumb, you should wean your baby slowly and let them take the lead on how much food they need. Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Start with smooth foods
You should also start your baby on food that is completely smooth. The textures of different kinds of foods can be a trigger for your infant to spit it up. That is not to say you can never introduce different textures, just make sure that you do so slowly. You should also make sure that you sit your baby upright when feeding them.
Watch out for allergies
You can include any foods that are a part of your family’s diet during complementary feeding. As a precaution, you could introduce foods one at a time for three days at first and, if your baby has no issues, the next new food should be added.
This way, any problematic food would be easier to recognise in the unlikely event that an acute or delayed form of allergic reaction occurs. Once potential allergens, such as eggs and peanuts, have been introduced it is recommended that you continue to include them in your baby’s diet, ideally at least twice a week, to ensure that your baby remains tolerant to that particular food.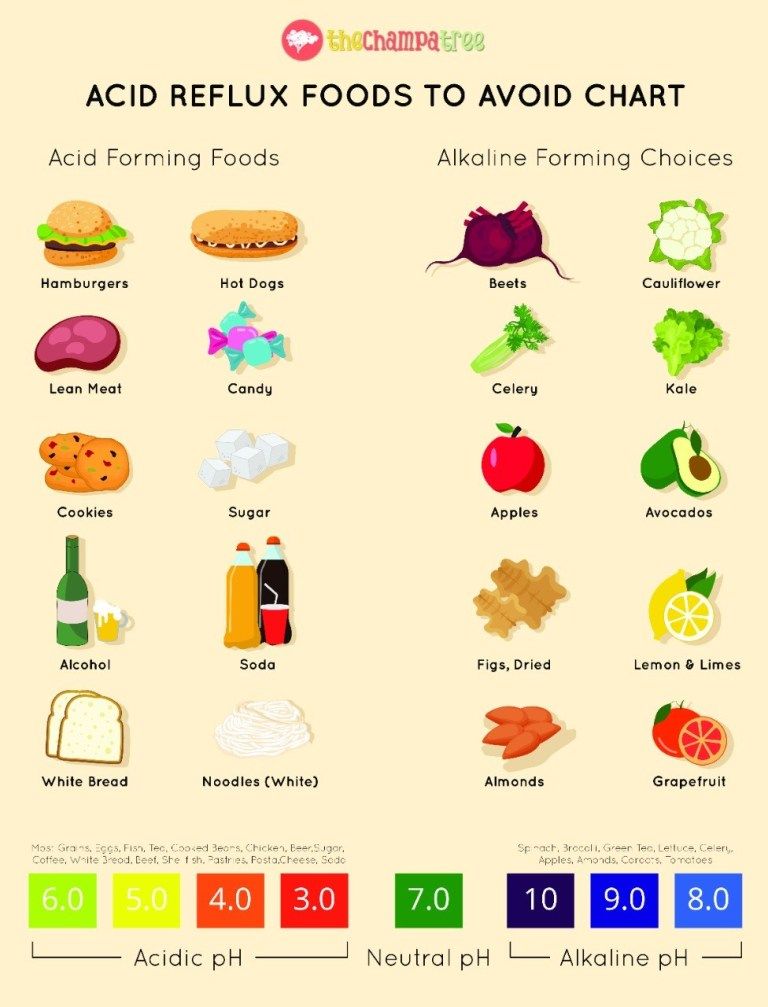
Spacing the time in between introducing new foods will give you the opportunity to discover the foods your baby likes and dislikes. Although your baby’s reflux can make introducing solid foods a challenge, it’s by no means impossible.
Related Blogs:
- Why Do Babies Hiccup?
- How To Burp A Baby
Solid Foods To Help with Infant Reflux in Babies
Introducing solid foods to your baby can seem like a daunting challenge, but with some helpful guidance this task will be a lot easier—especially for those babies that struggle with infant reflux or Infant Gastroesophageal Reflux Disease (Pediatric GERD).
Currently, medical research indicates that roughly fifty percent of babies are born with some degree of infant reflux. Sadly, in many cases infant reflux is misdiagnosed as colic and as a result many months may pass without the simple diet modifications that will make your baby healthier and more comfortable.
Below are the symptoms of infant reflux that you should be aware of:
- frequent crying
- vomiting or spitting up
- arching of the back or neck during or after feeds
- frequent ear infections
- inability to sleep or frequent waking
- irritability
- frequent hiccups
A vast majority of children will grow out of infant reflux around age two. In fact a lot of parents and professionals notice positive changes when solid foods are finally introduced.
In fact a lot of parents and professionals notice positive changes when solid foods are finally introduced.
What Solid Foods are Good for Babies with Infant Reflux?
Having a comprehensive list of the solid foods that babies with reflux tolerate well would be a wonderful tool to have—unfortunately the reality is that every baby is different. How one baby reacts to certain foods will be different than another. But there are mainstay solid foods that can help infant reflux.
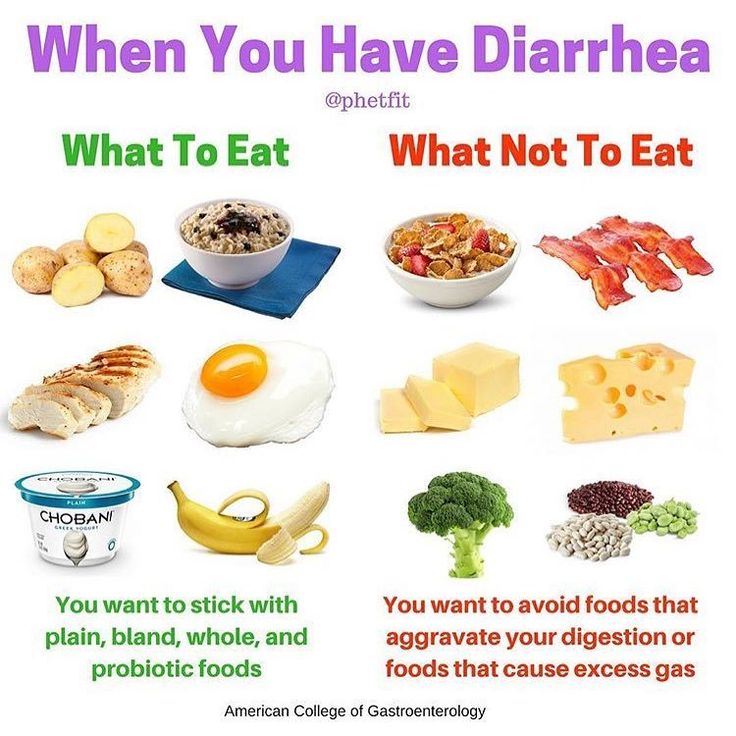
With your doctor’s permission, you can try introducing oatmeal instead of rice cereal or even pureed vegetables. For some babies with reflux, rice cereal contributes to excessive gas and even constipation.
On the fruit side, avocados, pears, and bananas tend to be good first foods for babies with reflux. All aid in digestion, are low in acidity, and provide great nutrients.
In ordinary cases, doctors recommend starting a baby on solid foods around six months of age. The pattern generally is as follows, first cereal, then vegetable, and lastly fruit.
The pattern generally is as follows, first cereal, then vegetable, and lastly fruit.
However, in the case of infant reflux a growing number of medical professionals recommend using cereal to thicken the formula or breastmilk before they are six months old to help keep down the milk.
While there is not a large amount of medical data that backs up the assertion that this method works, a number of doctors prefer parents try this trick before prescribing medication.
What Foods Make Infant Reflux Worse?
Many parents have found that when introducing solid foods to their baby with infant reflux that some fruits and juices like oranges, apples, and tomatoes make the reflux worse.
Let’s take a look at a list of foods that increases the amount of burping and therefore may worsen an infant’s reflux.
- Brussel sprouts
- broccoli
- corn
- cucumber
- cabbage
- cauliflower
- garlic
- onions
The above foods only increase the amount of burping, and may make reflux worse, but the foods below are common triggers of reflux flares and should be avoided when you have a baby with infant reflux:
- whole milk
- sausage
- bacon
- pineapple
- high fat foods
- carbonated drinks
- creamed vegetables
This is a common list of foods known to trigger reflux flares, but your baby may be triggered by something else. Pay attention to your baby’s diet and how they respond to it especially if your baby has infant reflux.
Pay attention to your baby’s diet and how they respond to it especially if your baby has infant reflux.
Is your baby struggling with reflux? What have you tried to find success in soothing your baby’s reflux symptoms? Tell us in the comments!
Proper nutrition for GERD - Clinic on Leninsky
The key to solving many problems with the gastrointestinal tract is proper nutrition. Gastroenterologist at the Clinic on Leninsky Katerina Chesskaya tells what you can and should eat for those who suffer from reflux disease.
What is GERD?
Gastroesophageal reflux disease (GERD) is a chronic relapsing disease in which there is a spontaneous, regularly repeated reflux of stomach contents into the esophagus. As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors. The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
GERD is usually manifested by belching and heartburn after eating or bending forward, and also at night. Another indication of the presence of GERD is pain behind the sternum, extending to the interscapular region, lower jaw, and the left half of the chest. There are also signs of GERD that are not directly related to the esophagus - a cough, shortness of breath, often occurring when lying down, hoarseness, dry throat, rapid satiety, and bloating. The cause of chronic inflammatory diseases of the nasopharynx (pharyngitis, laryngitis, sinusitis, tonsillitis) in 30% of cases is GERD. It has been proven that against the background of GERD there is a risk of developing obstructive pulmonary diseases, including bronchial asthma.
Proper nutrition for GERD
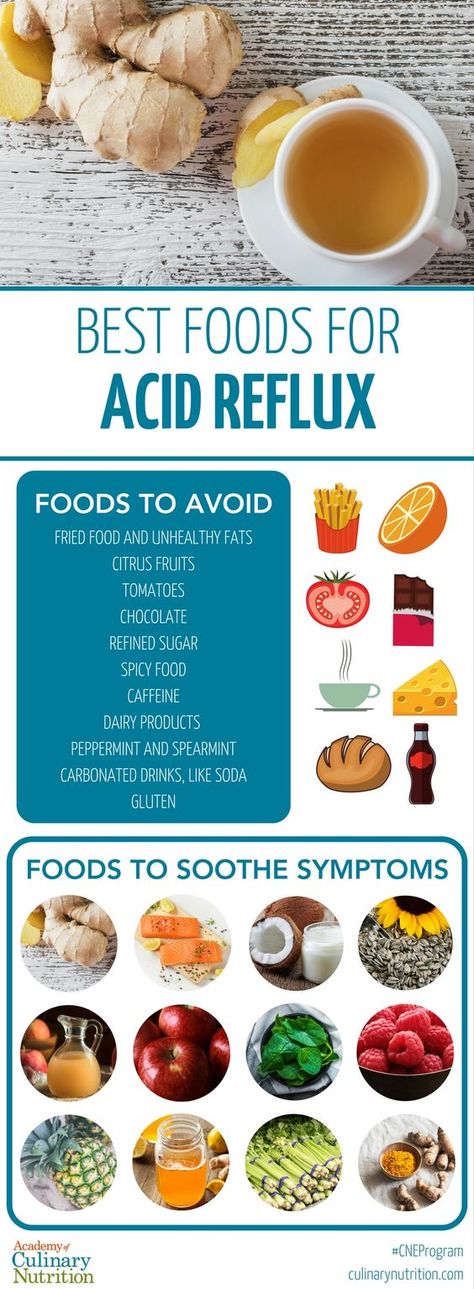
As in the case of many other diseases of the gastrointestinal tract, the main principle of the treatment of GERD is proper nutrition. There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
Here is a list of foods to consider when planning your menu for the day.
Delete:
1. Bread: fresh rye bread, tarts and pancakes.
2. Meat: stewed and fried meat dishes from fatty meat, poultry.
3. Fish: fatty fish, fried, smoked, salty dishes.
4. Vegetables: white cabbage, turnip, rutabaga, radish, sorrel, spinach, onion, cucumbers, salted, pickled and pickled vegetables, mushrooms.
5. Fruit: Raw, sour, unripe fruit, dried fruit puree.
6. Cereals: millet, pearl barley, barley and corn grits, legumes.
7. High acidity dairy products, spicy and salty cheeses.
8. Sweet: halva, chocolate, ice cream, cakes.
9. Drinks: sour, carbonated, fruit drinks, strong tea, coffee and alcohol.
Recommended:
1. Bread: from wheat flour of the first or highest grade, yesterday, dry, uncomfortable baking.
2. Meat: Beef, veal, chicken, rabbit, turkey, all in the form of cutlets, meatballs, soufflés, mashed potatoes and quenelles.
3. Fish: boiled river fish - zander, pike, perch, any low-fat varieties.
4. Vegetables: carrots, cauliflower, potatoes, beets, squash and squash.
5. Fruits: Sweet berries, ripe fruits. Preferably mashed or baked.
6. Cereals: oatmeal, semolina, buckwheat (mashed), rice porridge, on the water with the addition of milk, boiled vermicelli.
7. Dairy products: milk, lean cheese and low-fat sour cream. Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles.
8. Sweet: jam, marshmallows, honey, marshmallow, cream and milk puddings.
9. Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
It is also important to adhere to the diet:
— Fractional meals in small amounts and often up to 5-6 times a day.
- Do not lie down immediately after eating, the last meal is 2-3 hours before bedtime.
- Do not work in a slope, exclude the "gardener" pose.
- Do not wear tight belts and limit abdominal exercise.
- Obese people need to normalize body weight.
Remember that only a gastroenterologist can make a diagnosis of GERD (however, like any disease), to accurately determine the patient's condition. At the appointment, the doctor, together with the patient, will find the cause of the disease, outline a treatment plan and further supportive therapy in order to avoid relapses.
At the Clinic on Leninsky, an appointment is being made:
- pediatric gastroenterologist Natalya Medvedeva;
- gastroenterologist Ekaterina Chesskaya.
You can make an appointment with a gastroenterologist at the Clinic on Leninsky
by calling +7 (495) 668-09-86 .
Moscow, Leninsky prospect, building 67, building 2
Tel. .-Fri. 7:30–20:00 Sat-Sun 9:00–18:00
Diet for esophagitis of the esophagus | Sanatorium Gorny
Esophagitis is an inflammation of the esophageal mucosa due to weakness of the cardiac sphincter. A diet for esophagitis is a prerequisite for the complex treatment of the disease.
General rules. duration of the diet.
The main task of clinical nutrition in esophagitis of the esophagus is the complete exclusion of damage to the mucous membrane by mechanical and chemical factors.
With esophagitis, table number 1 is prescribed. In nutrition, you must adhere to a number of rules:
- the number of meals should be 5-6 times. portions are small. Such a tactic in nutrition with esophagitis allows the stomach to stretch unnecessarily and produce excess hydrochloric acid.
- Food should not be too hot or cold. The optimum temperature for food is 25-50 C.
- You can not eat "on the go". Eat slowly and chew your food thoroughly.
- Do not drink water immediately after eating. It is permissible to drink only 30-40 minutes after eating.
- Meals can be steamed, stewed, baked or boiled. You can't fry.
- Limit salt intake as much as possible.
In case of exacerbation of esophagitis, diet 1A should be followed for no more than 10 days. This diet is strict and if you stick to it, then the symptoms of the disease stop quickly enough. As soon as the discomfort and symptoms of exacerbation subside, you can go to table 1B. This table is more complete in terms of nutrients.
Notice! Acute esophagitis is a contraindication for spa treatment: it is better to go to a hospital.
If you have a chronic form, then you should regularly carry out preventive treatment .
Nutrition for chronic esophagitis:
In chronic esophagitis, table number 1 must be observed. From the diet it is necessary to remove all foods that can cause increased secretion of gastric juice or provoke increased gas formation.
Most of the food should be taken in the morning. You can not "eat up" at night, it is better to eat easily digestible foods, such as vegetable dishes or cereals.
List of approved products:
| Porridges and cereals | Buckwheat, rice, semolina, oatmeal |
| Dairy | Milk, non-acidic sour cream, low-fat dairy products, butter, unsalted cheese |
| Vegetables | Potatoes, zucchini, cauliflower, carrots, pumpkin, beets |
| Meat | Beef, veal, chicken, rabbit, turkey |
| by-products | Boiled tongue and liver |
| Fish | Low-fat varieties of river fish |
| Fruits | Bananas, apricots, pears, sweet apples, melons |
| Soft drinks | Weak tea, rosehip broth, compotes and kissels from sweet fruits and berries |
List of fully or partially restricted products:
| bread | Sweet pastries, fresh wheat and rye bread, pancakes, pancakes, fried pies |
| Vegetables | White cabbage, radish, radish, legumes, bell peppers, turnips, radishes, onions, garlic, sorrel, spinach |
| Groats | Millet, barley, corn, barley |
| Fruits and berries | All sour fruits: citrus fruits, currants, green apples |
| Meat | Goose, duck, pork, canned meat, lard, sausages, sausages, smoked meat, dried meat |
| Soft drinks | Strong tea, coffee, kvass, sparkling water, sweet fruit drinks |
Nutrition menu for esophagitis.
 Diet.
Diet. Nutrition for esophagitis should be based on the fact that food should not be digested for a long time. Dishes should be easily digestible, should not irritate the mucous membrane of the stomach and intestines. Products should envelop the gastric mucosa, and not irritate it.
Diet recipes for esophagitis:
Sample menu for one day:
Breakfast:
Oatmeal boiled in water with milk, red apple compote.
Second breakfast:
Steam omelet. Rosehip decoction
Lunch:
Chicken soup with vermicelli and vegetables. Pike perch fillet with boiled potatoes. Herb tea.
High tea:
Low fat yogurt. Cookie. Weak tea.
Dinner:
Vareniki with cottage cheese. Tea with milk.
Before going to bed you can drink a glass of warm milk.
Dietitian comments:
Therapeutic nutrition for esophagitis allows you to quickly get rid of unpleasant symptoms and normalize the work of the entire gastrointestinal tract.