Best way to feed a newborn baby
Feeding Your Newborn (for Parents)
How you feed your newborn is the first nutrition decision you make for your child. These guidelines on breastfeeding and bottle feeding can help you know what's right for you and your baby.
Breast or Bottle?
The American Academy of Pediatrics (AAP) recommends that babies be breastfed exclusively for about the first 6 months. After they start on solid foods, babies should breastfeed through the first year of life and even beyond, if desired.
But breastfeeding isn't possible or preferable for all new moms. Deciding to breastfeed or bottle feed a baby is usually based on the mother's comfort level with breastfeeding and her lifestyle. In some cases, breastfeeding may not be recommended for a mom and her baby. If you have any questions about whether to breastfeed or formula feed, talk to your pediatrician.
Remember, your baby's nutritional and emotional needs will be met whether you choose to breastfeed or formula feed.
Benefits of Breastfeeding
Breastfeeding your newborn has many benefits. Perhaps most important, breast milk is the perfect food for a baby's digestive system. It has the nutrients that a newborn needs, and it’s easily digested. Commercial formulas try to imitate breast milk, and come close, but can't match it exactly.
Breast milk has
antibodiesthat help protect babies from many infections, including diarrhea and ear and lung infections. Breastfed babies are less likely to develop medical problems such as diabetes, high cholesterol, asthma, and allergies. Breastfeeding also might make a child less likely to become overweight.
Breastfeeding is great for moms too. It burns calories, so can help nursing moms lose the weight gained during pregnancy. Breastfeeding also may offer protection from breast cancer and ovarian cancer.
Some moms find breastfeeding easier and quicker than formula feeding — it needs no preparation, and you don't run out of breast milk in the middle of the night.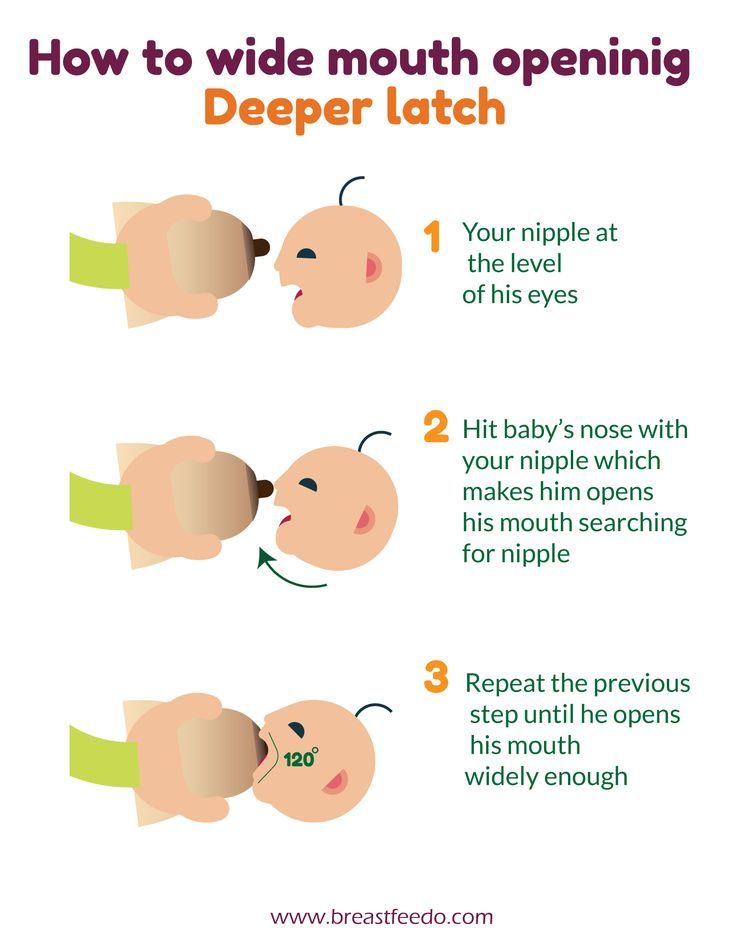 Also, breastfeeding costs little. Nursing mothers do need to eat more and may want to buy nursing bras and pads, a breast pump, or other equipment. But these expenses are generally less than the cost of formula.
Also, breastfeeding costs little. Nursing mothers do need to eat more and may want to buy nursing bras and pads, a breast pump, or other equipment. But these expenses are generally less than the cost of formula.
Breastfeeding meets a variety of emotional needs for both moms and babies. The skin-to-skin contact can enhance the emotional connection, and providing complete nourishment can help new moms feel confident in their ability to care for their newborn.
Limitations of Breastfeeding
With all the good things known about breastfeeding, why doesn't every mother choose to breastfeed?
Breastfeeding requires a big commitment from a mother. Some new moms feel tied down by the demands of a nursing newborn. Because breast milk is easily digested, breastfed babies tend to eat more often than babies who are fed formula. This means moms can be in demand as often as every 2 or 3 hours in the first few weeks. This can be tiring, but it's not long before babies feed less often and sleep longer at night.
Some new mothers need to get back to work outside the home or separate from their babies from time to time for other reasons. Some opt for formula feeding so other caregivers can give the baby a bottle. Mothers who want to continue breastfeeding can use a breast pump to collect breast milk to be given in a bottle, so their babies still get its benefits even when mom isn't there to breastfeed.
Fathers and other family members may want to share in feeding the baby. When mom is breastfeeding, dad or siblings may want to stay close by. Helping mom get comfortable, or providing a burp cloth when needed, will let them be part of the experience.
When breastfeeding is going well, other family members can help by giving the baby pumped breast milk in a bottle when mom needs a break.
Some moms may feel embarrassed or worried about breastfeeding. These feelings usually end after a successful breastfeeding process is set. It can help to get advice from those who've gone through the experience.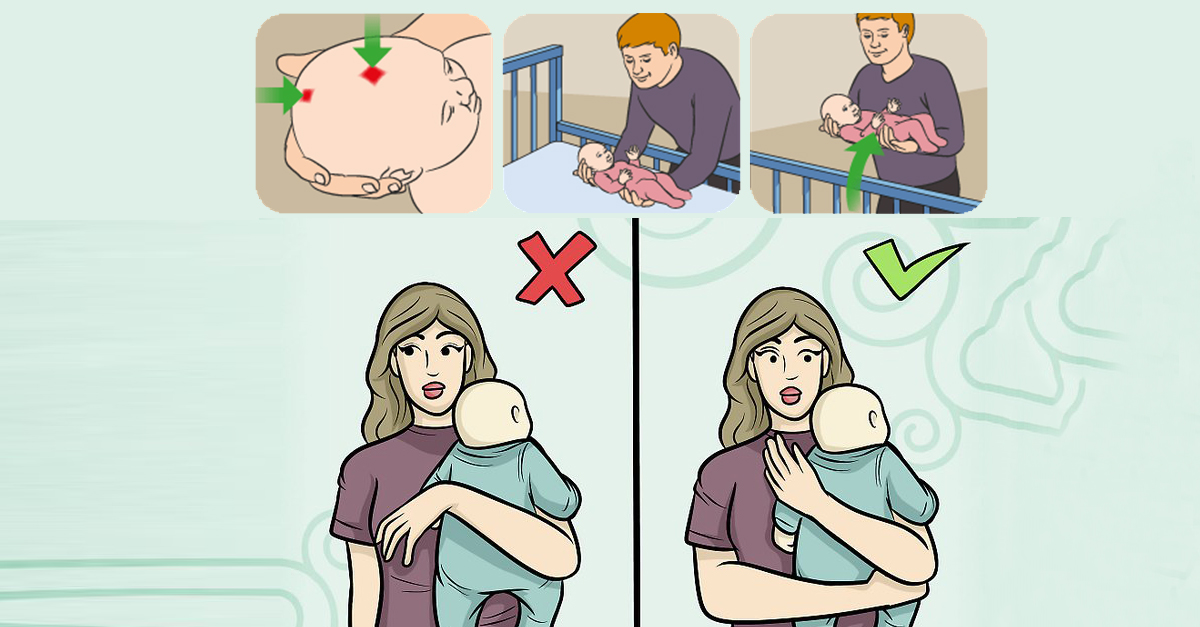 Most hospitals and birthing centers offer in-depth instruction on breastfeeding to new moms. Your pediatrician, nurse practitioner, or nurse can answer questions or put you in touch with a lactation consultant or a breastfeeding support group.
Most hospitals and birthing centers offer in-depth instruction on breastfeeding to new moms. Your pediatrician, nurse practitioner, or nurse can answer questions or put you in touch with a lactation consultant or a breastfeeding support group.
In some cases, a mother's health may affect her ability to breastfeed. Moms getting chemotherapy for cancer and those who have HIV should not breastfeed, for example.
If you have a medical condition or take any medicines regularly, talk with your doctor about whether it's OK to breastfeed. If you have to stop nursing temporarily, continue to pump breast milk to maintain milk production. If you or your baby are sick, continue to breastfeed if you can. Talk to the doctor if you have any concerns.
In some situations, it may not possible to breastfeed, such as when a baby is very sick or born early. Mothers should talk with their baby's doctor about expressing and storing milk. Often, a baby who can't breastfeed can get breast milk through a feeding tube or bottle.
Some moms who have inverted nipples may have trouble breastfeeding, but a lactation consultant usually can help them overcome this. Likewise, women who have had plastic surgery on their breasts should be able to successfully breastfeed. Talk with your doctor if you have any concerns.
Hold off on pacifiers or bottles until your baby has gotten used to and is good at breastfeeding. Lactation professionals recommend waiting until a baby is about 3–4 weeks old before offering artificial nipples of any kind (including pacifiers).
Benefits of Formula Feeding
Commercially prepared infant formula is a nutritious alternative to breast milk. Bottle feeding can offer more freedom and flexibility for moms, and make it easier to know how much the baby is getting.
Because babies digest formula more slowly than breast milk, a baby who is getting formula may need fewer feedings than one who breastfeeds. Formula feeding also can make it easier to feed the baby in public, and lets the father and other family members help feed the baby, which can enhance bonding.
Limitations of Formula Feeding
Just as breastfeeding has its unique demands, so does bottle feeding. Bottle feeding takes organization and preparation, especially if you want to take your baby out. Store-bought formula can be pretty expensive, but do not try to make your own formula at home.
It's important to make sure that you have enough formula on hand, and bottles that are clean and ready to be used.
Here are a few guidelines for formula feeding:
- Carefully follow directions on the label when preparing formula. Do not add more water than directed.
- Bottles left out of the refrigerator longer than 1 hour and any formula left in the bottle that a baby doesn't finish should be discarded.
- Prepared bottles of formula can be stored in the refrigerator up to 24 hours and carefully warmed just before feeding. You don't have to warm formula, but most babies prefer it.
- A bottle of formula can be warmed by holding it in running warm water or setting it in a pan of warm water.
 A bottle of formula (or breast milk) should never be warmed in a microwave. The bottle can heat unevenly and leave "hot spots" that can burn a baby's mouth.
A bottle of formula (or breast milk) should never be warmed in a microwave. The bottle can heat unevenly and leave "hot spots" that can burn a baby's mouth.
How Often Do Newborns Eat?
Your newborn will nurse about 8 to 12 times per day during the first weeks of life. In the beginning, mothers may want to try nursing 10–15 minutes on each breast, then adjust the time as needed.
Breastfeeding should be on demand (when your baby is hungry), which is generally every 1–3 hours. As newborns get older, they'll nurse less often and have longer stretches between feedings. Newborn babies who are getting formula will likely take about 2–3 ounces every 2–4 hours. Newborns should not go more than about 4–5 hours without feeding.
Signs that babies are hungry include:
- moving their heads from side to side
- opening their mouths
- sticking out their tongues
- placing their hands and fists to their mouths
- puckering their lips as if to suck
- nuzzling against their mothers' breasts
- crying
A feeding schedule is not necessary — you and your baby will get into a routine. Babies know (and will let their parents know) when they're hungry and when they've had enough. Watch for signs that your baby is full (slowing down, spitting out the bottle or unlatching from breast, closing the mouth, turning away from the breast or bottle) and stop the feeding when these signs appear.
Babies know (and will let their parents know) when they're hungry and when they've had enough. Watch for signs that your baby is full (slowing down, spitting out the bottle or unlatching from breast, closing the mouth, turning away from the breast or bottle) and stop the feeding when these signs appear.
As babies grow, they begin to eat more at each feeding and can go longer between feedings. There may be other times when your infant seems hungrier than usual. Continue to nurse or feed on demand. Nursing mothers need not worry — breastfeeding stimulates milk production, and your supply of breast milk will adjust to your baby's demand for it.
Is My Newborn Getting Enough to Eat?
New parents often worry about whether their babies are getting enough to eat.
Babies are getting enough to eat if they:
- seem satisfied
- have about 6–8 wet diapers a day
- have regular bowel movements (poops)
- sleep well
- are alert when awake
- are gaining weight
A baby who is fussing, crying, seems hungry, does not appear satisfied after feeding, and has fewer wet diapers may not be getting enough to eat. If you're concerned that your baby isn't getting enough to eat, call your doctor.
If you're concerned that your baby isn't getting enough to eat, call your doctor.
Most infants "spit up" a small amount after eating or during burping, but a baby should not vomit after feeding. Vomiting after every feeding might be a sign of an allergy, digestive problem, or other problem that needs medical care. If you have concerns that your baby is spitting up too much, call your doctor.
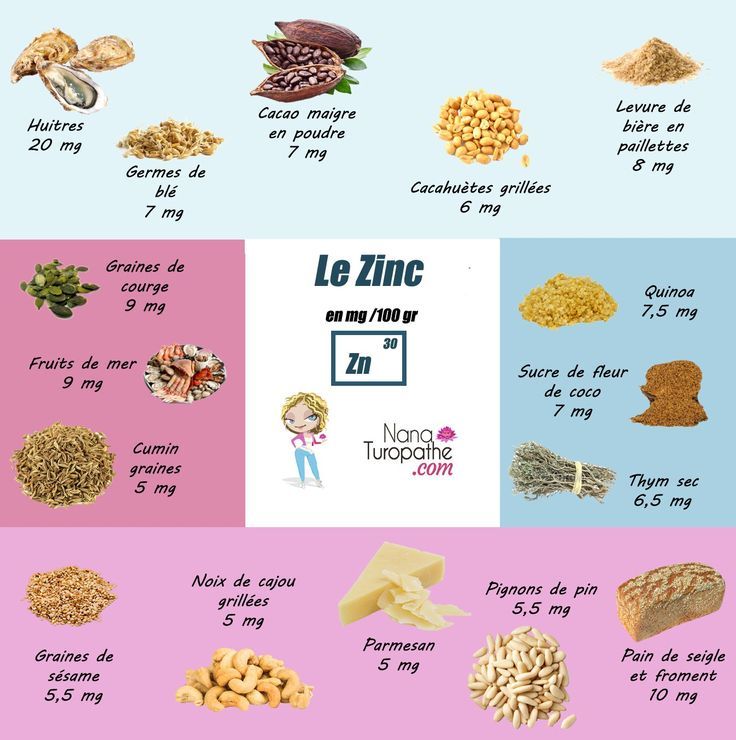
Should Newborns Get Nutritional Supplements?
Breast milk has the right combination of vitamins and easily absorbed iron for newborns. A healthy infant being nursed by a healthy mother doesn't need extra vitamins or nutritional supplements, with the exception of vitamin D. Breastfed babies should begin vitamin D supplements within the first few days of life, continuing until they get enough vitamin D-fortified formula or milk (after 1 year of age).
Breastfeeding mothers who follow vegetarian diets that do not include animal products need vitamin B12 supplements.
Iron-fortified formula has the right blend of vitamins and minerals for a baby, so supplements usually aren't needed. Infants drinking less than 1 liter, or about a quart, of formula a day may need a vitamin D supplement.
Infants drinking less than 1 liter, or about a quart, of formula a day may need a vitamin D supplement.
Water, juice, and other foods usually aren't necessary during a baby's first 6 months. Breast milk and formula provide everything babies need nutritionally until they start eating solid foods. Talk to your doctor if you have any questions about feeding your newborn.
Reviewed by: Mary L. Gavin, MD
Date reviewed: February 2021
12 Expert Baby Feeding Tips For A Healthy, Happy Newborn
In the middle of juggling diapers, onesies, and nap schedules, one of your biggest concerns when you have a new baby is nutrition. It’s completely understandable — you want your little one to grow and develop as they should.
The experts at Mustela are here to give you some tips on baby feeding so you can rest a little bit easier! Whether you’re breastfeeding or formula-feeding, you’ll find tips that apply to you and learn a couple of ways to take care of yourself as well.
12 Expert Baby Feeding Tips
1) Skip The Water And Juice
For the first several months of your baby’s life, don’t give them anything other than breastmilk or formula. That means no water and no juice.
As boring as this might sound, it’s all that your baby needs to grow and develop! Once your little one is around six months old, you can begin giving them small amounts of water or juice, but breastmilk or formula should still be their main beverage.
2) Find A Comfortable Breastfeeding Position
Babies eat frequently, meaning breastfeeding moms will spend a lot of time nursing their little ones! If that’s you, find the right breastfeeding position so you can be as comfortable as possible.
There’s no one right position — try various breastfeeding positions (like the cradle hold, crossover hold, or laid-back position) to see what works best for you and your baby. Don’t forget to use pillows as needed to support yourself.
It’s also important to alternate breasts throughout the day to ensure adequate milk supply in each breast. You can try switching breasts during your feeding or alternate between each feeding (just make a note to help you remember which breast to try for the next feed!).
You can try switching breasts during your feeding or alternate between each feeding (just make a note to help you remember which breast to try for the next feed!).
Once you and your little one are in the right position, it’ll be easier for your baby to latch on correctly, which is important for more than one reason! That brings us to our next tip.
3) Help Your Baby Latch On Correctly
Making sure your baby latches on correctly helps them feed well and get enough milk. It can also save you from sore or cracked nipples.
While we hope our little ones will latch correctly by themselves, it doesn’t always go according to plan and might require a little bit of practice (and a lot of patience!).
Your baby might need a little guidance from you to get started. Touch their upper lip with your nipple so they open their mouth big and wide. Then bring their head to your breast (not your breast to their head) and put their chin to your breast first, followed by their mouth.
When your baby is latched correctly, you should feel comfortable and not experience any pain in your breasts or nipples. It’s not unusual to feel a stretching or tugging sensation at first, but if this continues, try readjusting your baby.
If baby is sucking deeply, you’re able to hear them swallowing, and their chin is pressed gently to your breast, you can be sure they’re correctly latched. Their bottom lip should be turned out over your nipple (not tucked in), and they should have the whole nipple in their mouth.
Your breasts should also feel softer after your little one has finished feeding, meaning your milk has been drained properly.
If you have to take your baby off for any reason, break the suction by gently pushing down on your skin near their mouth or inserting your finger into the corner of their mouth.
4) Take Care Of Your Physical Health
Motherhood can take a toll on you, and breastfeeding is not always a walk in the park! It’s crucial that you practice self-care during this time, and there are plenty of ways to do it.
The first step to caring for yourself applies whether you’re breastfeeding or bottle-feeding — stay hydrated! Keep a bottle of water with you whenever possible and try not to let yourself get thirsty, as this can mean you’re starting to become dehydrated.
In addition to staying hydrated, ensure you’re eating throughout the day (a difficult task when you’re so focused on your little one!) and try to get enough sleep.
It’s also important to take care of your skin by tending to your breasts. A little TLC will go a long way toward helping you feel good and care for your little one.
Look after your nipples (this is especially important if you have soreness or cracking!) by applying Mustela’s Nursing Comfort Balm.
This soothing nipple cream will ease discomfort and moisturize sensitized nipples. Plus, it’s environmentally friendly, made of 100% naturally derived ingredients, and safe for both you and your baby during prenatal and postpartum pregnancy.
Also, try Mustela’s Bust Firming Serum to nourish and hydrate your breasts, neck, and neckline. Safe to use while breastfeeding, this serum will tone your skin and give it a firmer look and feel!
Safe to use while breastfeeding, this serum will tone your skin and give it a firmer look and feel!
5) Don’t Wait For Your Baby To Cry
Babies cry for several reasons, including wanting to eat! But crying is a late hunger cue — it’s a sign that they’re too hungry. If you wait until your little one cries to give them a bottle or nurse them, you may have a more difficult time calming them down.
Instead, be on the lookout for earlier signs of hunger, like rooting (opening their mouth and moving their head side-to-side), sucking on their fingers, or smacking their lips. That’s your cue to warm the bottle or settle in to nurse.
6) Monitor Diapers And Weight Gain
Your baby can’t yet verbalize if they’re full or not, so how can you know if they’re eating enough? Look for wet and dirty diapers as well as weight gain.
Wet And Dirty Diapers
For the first couple of days, your tiny baby won’t have many dirty diapers, but by the time they’re four or five days old, they should dirty a diaper two or three times per day.
The same principle applies to wet diapers. The first day or two, your little one may wet only two diapers, but that will increase over the next few days. By five days old, they’ll typically wet six or more diapers every day.
Around this time, your little one’s stools will change from the dark green-colored meconium that lines their intestines in the womb to the typical baby poo color, which is more of a mustard yellow.
Get into good diaper-changing habits from the beginning. Don’t leave your little one in a dirty diaper, clean their bottom with Cleansing Wipes, and care for their delicate skin with Mustela’s Liniment and Diaper Cream with Olive Oil and Aloe, both made with natural ingredients.
Weight Gain
When it comes to your baby’s weight, don’t be surprised if they lose a bit right at first. Babies usually drop several ounces over the first couple of weeks, but after that, they should gain five to eight ounces per week for the first several months.
Your pediatrician will check your baby’s weight when you go for a visit. If you have any concerns or questions about your little one’s weight gain or eating habits, don’t be afraid to ask.
If you have any concerns or questions about your little one’s weight gain or eating habits, don’t be afraid to ask.
7) Feed Your Baby Frequently
It might seem like all you do is feed your baby, change their diapers, and try to get a few precious minutes of sleep when you can. There’s a reason you feel that way — babies eat frequently during their first few months!
While their little tummy can only hold a teaspoon or so of liquid in their early days, their stomach will slowly stretch as they grow to allow for more food intake.
Although breast-fed babies tend to eat more often than bottle-fed babies due to breastmilk being quicker to digest, all newborns should eat between eight and 12 times in a day (24 hours) — at least every four hours. They may even eat as often as every one and a half or two hours!
But after the first month, the number and frequency of feedings will decrease as your baby grows older. Your little one will also become more efficient with feedings, so you may notice that the duration decreases from up to 20 minutes per breast to around 10 minutes per breast.
If you notice your baby is suddenly hungrier than usual, they may be going through a growth spurt! You can expect to experience a sudden increase in feeding frequency every two months or so up until your baby is six months old.
How can you know when your little one is all done with a feeding? Your baby should stop nursing when they’re ready and will be relaxed and content.
To be sure they’re finished, give them a little break and a burp, then offer the breast or bottle again.
8) Prepare The Right Amount Of Formula
While you’re still getting the hang of this parenthood thing, it can be difficult to know how much formula to prepare for a feeding.
Prepare too little and you’ll be trying to get a bottle ready with one hand while your baby cries. Prepare too much and you may have to throw out what you don’t use.
We recommend making two to three ounces of formula each time you feed your little one at first. As your baby grows, they’ll eat less frequently and need more formula at each feeding.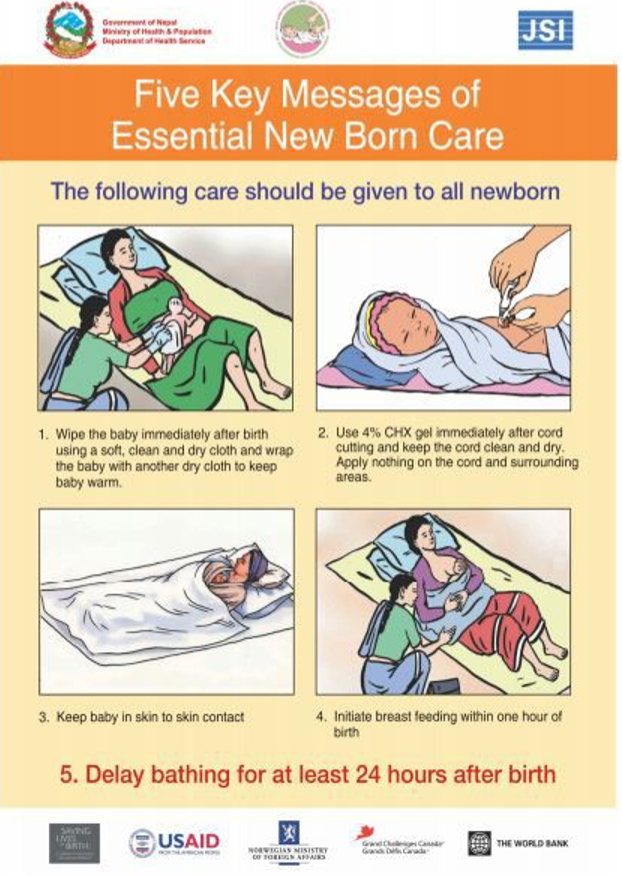 Increase the amount of formula you make over time so that your baby is full and content after a feeding.
Increase the amount of formula you make over time so that your baby is full and content after a feeding.
9) Don’t Introduce Solid Foods Too Early
Breast milk (or formula) is the best source of nutrients for your baby, and doctors recommend breastfeeding for at least the first six months of their life — up to one year if you can!
Regardless of how long you breastfeed, when your baby is around six months old, you can introduce solid foods. You’ll know they’re ready if they’re picking things up with their fingers, able to sit and hold their head up well, and don’t push food out of their mouth with their tongue.
Just remember: even once you’ve started offering solids to your baby, breastmilk or formula is still an essential part of their diet!
10) Stock Your Diaper Bag With Baby Feeding Essentials
Knowing that your baby will need to eat frequently, stock your diaper bag so that you have what you need when you’re out-and-about or traveling with your little one. Don’t get caught empty-handed!
Don’t get caught empty-handed!
Make sure you have a nursing cover, bottles, formula, bibs, and the like. That’s in addition to the other diaper bag essentials, like No Rinse Cleansing Water for easy clean-ups and a multi-purpose ointment like Cicastela Moisture Recovery Cream.
And don’t forget Mustela’s Bebe On The Go travel-friendly set for quick and easy hydration and clean-ups no matter where you are!
11) Burp Your Little One Regularly
Babies can easily swallow excess air while they’re feeding, which can lead to gas that needs to be burped out. But when it comes to burping your baby, it can take a few tries to find a position that works!
A common burping position is holding baby upright against your chest with their chin resting on your shoulder. Drape a burping cloth over your shoulder to catch any excess milk your little one might spit up, and then give them gentle pats on the back with a cupped hand.
If this position doesn’t offer your baby relief, sit them upright on your lap instead. Otherwise, your baby might be more comfortable laying belly down on your lap with a slightly raised head. Try gently rubbing your baby’s back in either of these positions to provide relief.
Otherwise, your baby might be more comfortable laying belly down on your lap with a slightly raised head. Try gently rubbing your baby’s back in either of these positions to provide relief.
While it’s important to burp your baby after each feeding session, it’s also a good idea to stop feeding a couple of times during to see if they need to burp.
If you’re breastfeeding, try burping your little one in-between switching breasts. If you’re bottle-feeding your baby, attempt to burp them after every two to three ounces of fluid.
Your little one should settle after being fed and burped. If you notice that they’re regularly unsettled after being burped, consult your pediatrician to ensure there are no underlying issues, such as acid reflux, that might be bothering your baby.
12) Keep Up Your Milk Supply
Like we mentioned earlier, you’ll know your little one is getting enough milk by their weight gain and amount of dirty diapers. But if your baby is struggling? Could it be due to low milk supply?
There are many potential causes of low milk supply, including medical conditions such as diabetes, excess stress, certain medications, delayed start to breastfeeding, and not breastfeeding often enough.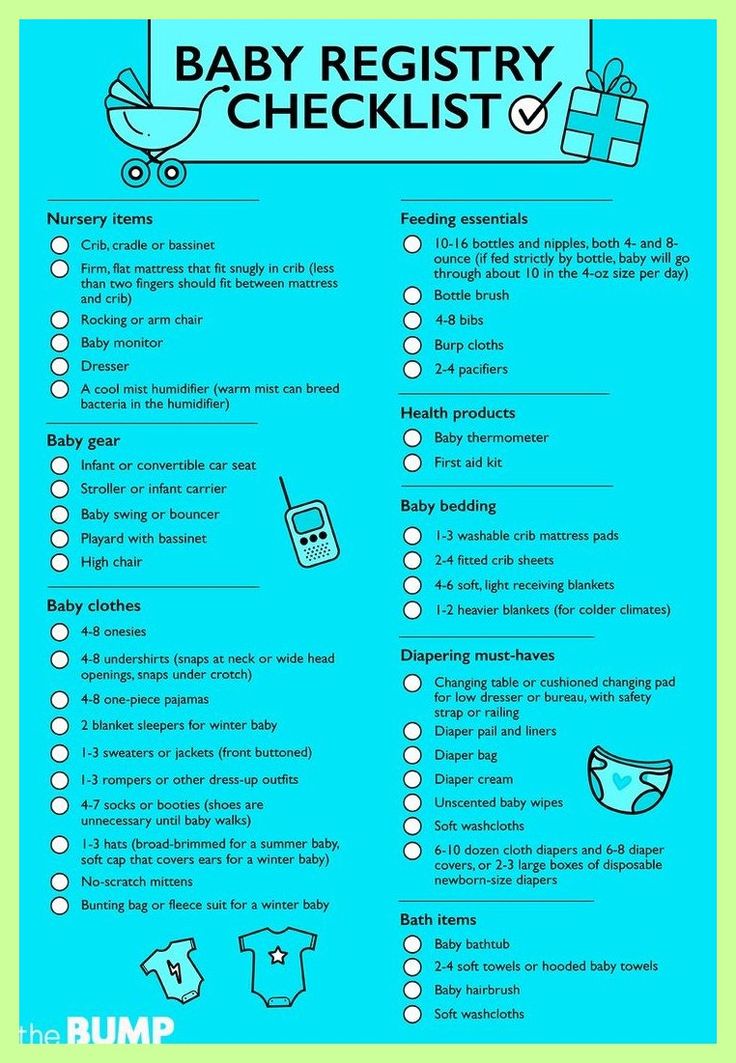
You can make small, simple changes to try to increase your milk supply. By breastfeeding as soon as possible (preferably within an hour of your little one’s birth), you’re setting yourself up for feeding success.
Increasing baby’s feeds to include snacks between main meals is another way to improve your supply, as is alternating between each breast during feeds. Using a breast pump may also help to stimulate your milk supply.
And, as always, ensuring you’re well-hydrated, eating a well-balanced diet, reducing stress by making time for yourself, and making sure you’re getting plenty of sleep are all key to maintaining a healthy milk supply for your little one.
If you’ve tried the tips mentioned above and you’re still experiencing difficulties with breastfeeding and low milk supply, talk to your doctor or lactation consultant to see if there are medications or additional techniques to implement.
Common Feeding Issues And How To Solve Them
Cluster Feeding
In the early days of breastfeeding when you and your little one are still trying to find your groove, you might find that your baby begins to cluster feed. This is when your baby takes short feeds in quick succession, often eating multiple times over just a few hours.
This is when your baby takes short feeds in quick succession, often eating multiple times over just a few hours.
While it’s normal to experience cluster feeding, it can be a difficult adjustment for new mothers. When you’re in the throes of cluster feeding, it can feel like there’s no end in sight. But don’t fret — it won’t last forever!
The best thing you can do to ride the wave of cluster feeding is to remember it’s completely normal and that you haven’t done anything wrong to cause it. Be gentle with yourself by practicing simple self-care and rest when you can.
Cluster feeding is only a concern if it becomes excessive. If the cluster feeding lasts more than a few days, consult your doctor to be sure your little one is happy, healthy, and gaining weight as they should.
Blocked Milk Ducts
If you’ve experienced blocked milk ducts, you know just how painful they can be! You might notice a small lump in your breast or a painful white spot on your nipple as the first sign of clogged ducts.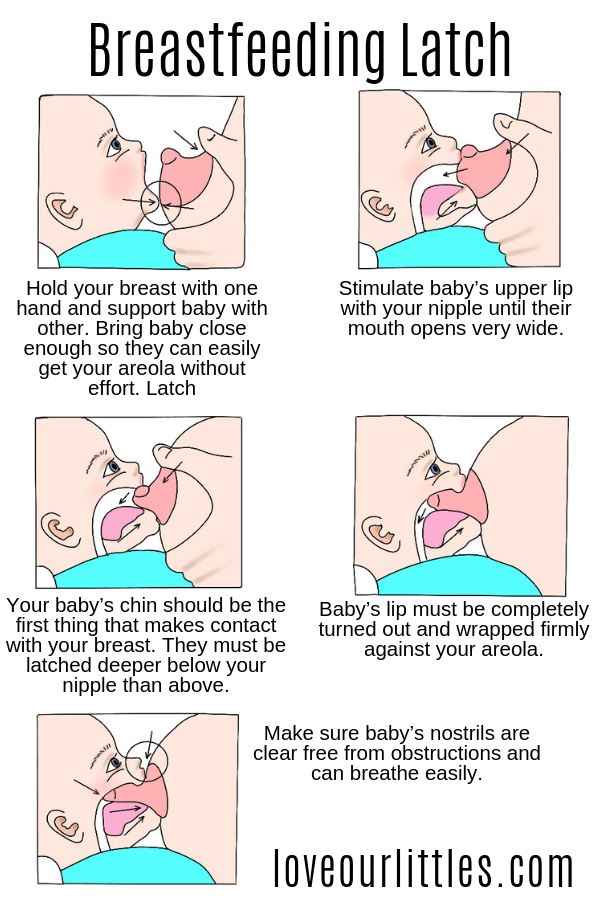
There are a few ways to clear a clogged milk duct. Start by having a hot shower and massaging your breast to break up the lump. Alternatively, try holding a warm compress to your breast before massaging.
Continue feeding your baby through the breast with the clogged duct if you can, as it can help to provide relief by unclogging the duct.
After your little one has finished feeding, try using a breast pump to drain excess milk and prevent potential clogs.
Mastitis
Mastitis is a painful condition of inflammation in the breast that can lead to infection. It usually begins with a simple clogged milk duct and is often accompanied by additional uncomfortable symptoms, such as a fever, fatigue, aching, swelling of the breast, and redness.
Like clogged milk ducts, mastitis can be caused by incorrect breastfeeding techniques and not fully draining your breasts after feeding sessions. It can also be caused by clogged ducts that aren’t treated swiftly enough.
It’s important to seek treatment for mastitis as soon as you begin to notice symptoms. Your doctor will likely prescribe antibiotics to help clear the infection — these are completely safe to take during breastfeeding.
Try to continue breastfeeding despite the mastitis to prevent further clogged ducts or abscesses from forming. Reducing feeds during this time can worsen the condition and prolong your recovery time, so try to keep your routine as much as possible to promote healing.
Nurture Your Newborn And Care For Yourself
Caring for a newborn can feel overwhelming, but keeping them well-fed doesn’t have to be complicated and is a great opportunity to bond with your little one.
With our baby feeding tips, regularly scheduled visits to the pediatrician, and lots of love and TLC, your baby will be full, healthy, and happy.
Don’t forget to care for yourself in the meantime so you can give the best possible care to your little one. Keep Mustela’s Bust Firming Serum and Nursing Comfort Balm on hand so you can continue nursing your tiny one as long as you want!
Breastfeeding for beginners | Philips Avent
search support iconSearch Keywords
because it will take a long time during the first few months of a child's life. In this article, we will discuss all of its main aspects, from the basic principles of breastfeeding to the best tips for effective newborn feeding.
In this article, we will discuss all of its main aspects, from the basic principles of breastfeeding to the best tips for effective newborn feeding.
As always, if you have any questions or concerns, seek the opinion of another specialist.
Basic principles of breastfeeding
Although every baby is different, newborns usually eat every two to three hours, for a total of 8 to 12 times a day. In the first one or two days after birth, babies usually drink 25-50 ml of milk per feeding. This volume will gradually increase to 50-75 ml when the baby is about two weeks old.
More information on how much a newborn should eat can be found here.
How long does one feeding last?
Again, every baby is different, so there is no set time frame for every newborn. But in general, breastfeeding a newborn takes five minutes to one hour. This time depends on the size, age of the baby and the frequency and duration of feeding the newborn.
How to start breastfeeding?
In the very first minutes of a child's life, his mother should put the baby on her chest and ensure body contact. This time is called the "golden hour": it is at this hour that a connection is established between mother and child and the newborn's natural instinct to seek the breast manifests itself. As soon as the child begins to show signs of hunger, you need to give him a breast.
Mothers who are just learning to breastfeed their newborns should remember that comfort is key. There is no better way to ensure breastfeeding success than by creating a comfortable and relaxing environment for the mother. For starters, mom can sit comfortably on the couch, on the bed, or in a chair with pillows to support her back while feeding. Breastfeeding moms can get creative with breastfeeding and choose specific lighting, soothing music, or anything else that helps them relax.
Bring your baby to your breast, not the other way around.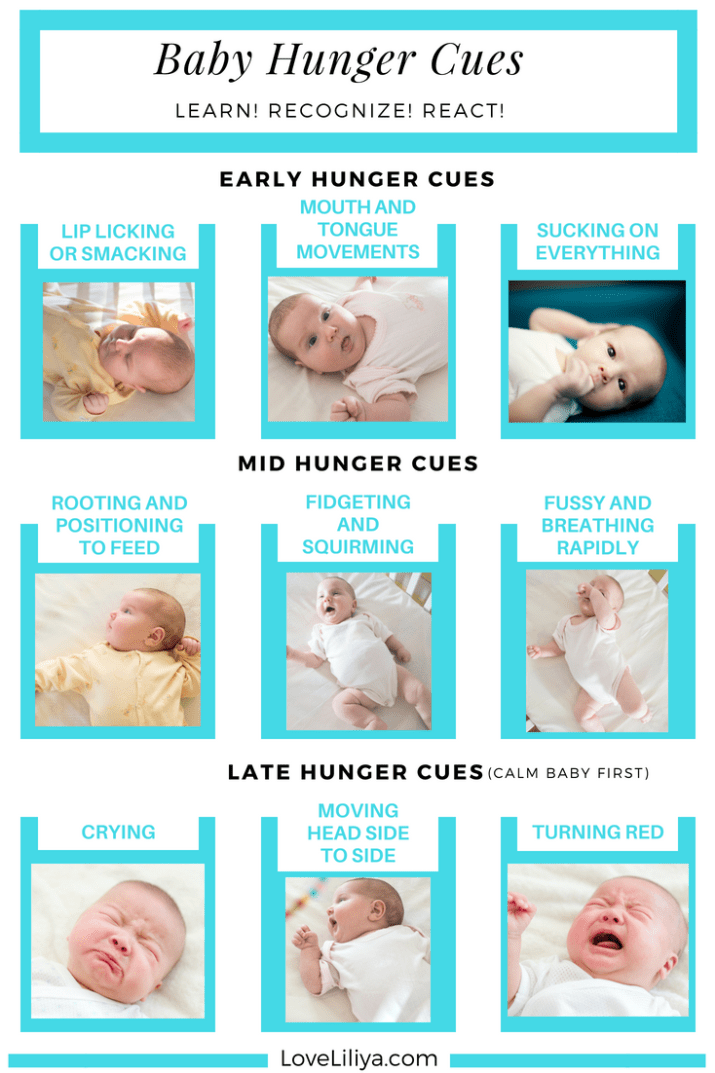 If you want to make breastfeeding a newborn easier, then do not lean towards the baby, but bring it to your chest. The baby's mouth should be opposite the nipple, the neck should be straight, and the shoulders and hips should be in line. Mom can also lightly touch her nipple to her baby's nose and mouth to encourage him to latch on.
If you want to make breastfeeding a newborn easier, then do not lean towards the baby, but bring it to your chest. The baby's mouth should be opposite the nipple, the neck should be straight, and the shoulders and hips should be in line. Mom can also lightly touch her nipple to her baby's nose and mouth to encourage him to latch on.
Support your chest. Holding the newborn with one hand, the mother can place the other hand directly under the breast to support it. When learning to breastfeed, some mothers prefer to leave one hand free; in this case, a rolled towel can be used.
Breastfeeding can be done in different positions; experiment with them to find the one that works best for you and your baby. We list the most common breastfeeding techniques below:
- Cradle. In this position, the baby lies on the mother's hand from the side of the breast, which he sucks. The baby's head lies on the mother's elbow during feeding.
- Cross cradle.
 With a cross cradle, the mother holds the baby with the hand opposite to the mammary gland that the baby sucks. With the other hand, mom can support her breasts.
With a cross cradle, the mother holds the baby with the hand opposite to the mammary gland that the baby sucks. With the other hand, mom can support her breasts.
- Underhand or Football. In this position, the mother holds the child next to her, putting her back on her arm. With the other hand, she supports the baby's head, facing the mammary gland, with which she feeds the baby.
- Lying on your side. In this position, the mother lies on her side, and the child lies next to her, facing her chest. Mom can support the child under the back with the hand that is on top, or put a folded towel under the back of the child.
Newborn Breastfeeding Tips
After looking at breastfeeding techniques, here are some tips for new mothers:
A good grip is important for both mother and baby. With a good grip, the baby will suck out milk correctly, and the mother's nipples will not hurt. To achieve a good latch, the mother needs to find a position that makes it easier for the newborn to latch onto the breast, and to do this, she should experiment with different positions. If a mother is having difficulty feeding, she should contact a lactation consultant.
If a mother is having difficulty feeding, she should contact a lactation consultant.
2. Maintain milk supply. Sometimes a nursing mother cannot be constantly with her child during feedings. In such cases, it is very important to maintain milk production. An excellent solution for maintaining milk production when mother and baby are not together is pumping milk.
Take a look at this double breast pump: it reduces pumping time and features a massage petal attachment to gently stimulate milk flow.
3. Breastfeeding everywhere. One of the many benefits of breast milk is that mom always has it with her. But some moms feel awkward at first when they have to breastfeed their baby in public. For such mothers, we recommend that you first practice breastfeeding your newborn in front of a mirror and choose clothes that allow you to cover your breasts during feeding. A shawl or scarf can help with this - with them, the mother will feel more comfortable when feeding the baby outside the home.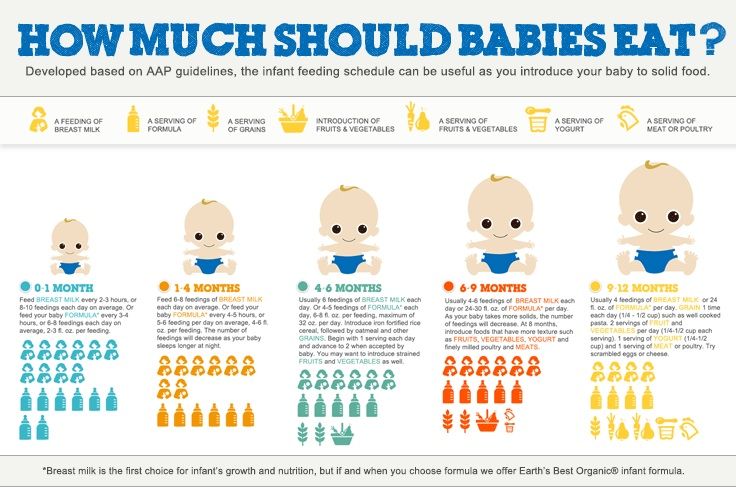
And to keep clothes dry and clean while breastfeeding, we recommend that mums use these disposable bra pads with a porous and breathable structure: they do not leak and let air through.
Be prepared for difficulties. It is important for moms not to panic or get upset when faced with a common breastfeeding problem, such as insufficient milk production, breast engorgement, clogged milk ducts, mastitis, or sore nipples. To feel calm and confident during all stages of breastfeeding a baby, mothers need a circle of support: family members, friends, and healthcare professionals. The main thing is to stay calm, but if a mother is concerned about any aspect of breast health, she should definitely see a doctor. Learn more about breastfeeding difficulties and how to overcome them.
Articles & tips from Philips Avent
Baby+ app
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
How to apply the baby while breastfeeding
Desired position
First of all, you need to correctly position the baby at the chest. Take him in your arms so that he is turned to his mother with his whole body, the child's face should be close to the chest, his mouth is wide open. In case of an incorrect position, the baby's body is deviated from the mother's, the chin does not touch the chest, the lips are extended forward. This is an important point, because if the baby starts sucking the breast incorrectly, he will not receive enough milk, the baby will begin to throw and grab the breast again, and sometimes even refuse it.
In case of an incorrect position, the baby's body is deviated from the mother's, the chin does not touch the chest, the lips are extended forward. This is an important point, because if the baby starts sucking the breast incorrectly, he will not receive enough milk, the baby will begin to throw and grab the breast again, and sometimes even refuse it.
Correct grip
Now you need to correctly insert the breast into the baby's mouth. In general, every healthy newborn has reflexes that help him eat. But the baby does not have a reflex that would help him keep his mother's breast in his mouth, and the baby cannot properly grasp the nipple himself. Therefore, the child needs help - put the breast into the crumbs' mouth so that it captures not only the nipple, but also the areola. If the baby grabs only the nipple, then the pressure on the ducts of the mammary gland will be weak and the milk will flow poorly from the breast. In addition, if a child suckles only the nipple, his skin is often damaged and cracks appear on the nipple. Sometimes, in order to give a breast to a child, a mother pinches the nipple and areola with her fingers and tries to push them into the baby's mouth. You don’t need to do this, it’s much easier to just touch the nipple to the baby’s lips (stimulate the capture reflex), wait until the baby opens her mouth wide, and quickly give him the breast.
Sometimes, in order to give a breast to a child, a mother pinches the nipple and areola with her fingers and tries to push them into the baby's mouth. You don’t need to do this, it’s much easier to just touch the nipple to the baby’s lips (stimulate the capture reflex), wait until the baby opens her mouth wide, and quickly give him the breast.
simple postures
Immediately after delivery, especially if there was a caesarean section or episiotomy (or just want to lie down), you can feed the baby lying on its side . You lie in bed, put the baby next to you, bend your lower arm at the elbow, and support the back of the child with your upper palm. The baby should lie on the bed parallel to your body, his mouth should be at the same level and very close to your nipple.
The second easiest position for feeding - sitting position . To do this, take the baby in your arms, bend your arm at the elbow from the side of the breast with which you will feed the baby. At the same time, the baby's head lies on a bent arm. To make it more convenient for you, put a pillow under your elbow (regular or special for feeding), you can also put something under your legs.
At the same time, the baby's head lies on a bent arm. To make it more convenient for you, put a pillow under your elbow (regular or special for feeding), you can also put something under your legs.
For variety
We have mastered simple poses - now you can try to feed the baby from other positions, for example, in position "jack" : mother and baby lie on their sides parallel to each other, but now their legs and head look in different directions. There is also such a pose - "chest on top" : the baby lies on its side, and the mother, as it were, hangs over him. In this position, it is easier for milk to go down the ducts, and it is easier for the child to get it. To make everyone comfortable, the baby should be put on some kind of elevation (for example, on a pillow).
Prevention of lactostasis
Laxtostasis, or stagnation of milk, is a very unpleasant thing. It occurs when any lobule of the mammary gland is not emptied of milk to the end. To prevent it or if it has already occurred, you need to feed the baby from under hands (from under the arm). In general, if you feed in this position at least once a day, then the lower and lateral lobes of the breast (the most frequent places of lactostasis) will be better emptied.
To prevent it or if it has already occurred, you need to feed the baby from under hands (from under the arm). In general, if you feed in this position at least once a day, then the lower and lateral lobes of the breast (the most frequent places of lactostasis) will be better emptied.
In this position, you put the baby on the pillow, the baby's head is located at your chest, and the body and legs are behind you (facing towards your armpit). Here's the important thing: the baby's mouth should be at the level of the nipple, then your back will not get tired during feeding.
The child likes it
If your milk flows out too quickly and the baby does not have time to swallow it, then you can feed the baby in position "baby on top" . You lie on your back (with your head on the pillow), and the baby is applied from above. Grown up children still love this pose because it is more convenient for them to observe the world around them “from above”.
The second favorite position of older children is that the baby sits or stands while feeding .