Bottle feeding positions for premature babies
Elevated side lying bottle feeding — Feed Eat Speak
Infant feedingFeeding difficultiesBottle Feeding
Written By Stacey Zimmels
Elevated side lying is a bottle-feeding position that’s being used more and more for preterm babies and infants who have feeding difficulties. In this blog post I’ll tell you why I like it for all new born babies. I’ve put together a visual step by step guide for you so go ahead and give it a try…
This position is a natural and physiologically normal feeding position just like how a baby feeds at the breast. It means the baby doesn’t have to do any work at all to support its body while it feeds which makes for an easier and more relaxed feed for both the baby and you.
Baby is positioned on a cushion which means that you don’t have to take the baby’s weight on your arms which is more comfortable especially as your baby grows.
You have a hand free if you need it to read to a toddler or have a drink while you’re feeding your baby.
If the flow of milk is too fast - which it often can be at the start while your baby is mastering its suck swallow and breathe co-ordination – this position allows the milk to safely dribble out of your babies mouth instead of coughing or choking.
You are able to clearly see your baby’s face and watch for signs that she may need a pause or a break for winding.
This is a great position for babies who have reflux or who are prone to vomiting. If you place the baby on its left side to feed it increases the space from the bottom of its stomach to the oesophagus making it less likely for them to vomit or reflux.
This feeding position is more typically recommended for formula fed babies, rather than the paced bottle feeding technique. which tends to be recommended for breastfed babies who also take the bottle. However I would suggest that with the horizontal presentation of the teat and the pacing as per the paced bottle feeding technique that this feeding position can be used in both groups of infants.
Step by step guide to elevated side lying bottle feeding
Sit comfortably on the sofa and place your feet on a footstool. This plastic childrens' one from ikea does the trick. Your legs should be sloping from the knees to your hips
Place your baby on its side with her bottom against your tummy. Her legs should be out in front of her. If you're right handed then baby on her left side and visa versa
Your baby will bring her hands together on her chest in a flexed position. Offer the bottle, wait for her to open her mouth and place inside. Note how relaxed and content your baby looks
Chelsey and Jaxon's story
I had my baby boy Jaxson in April 2020 and he was born with a tongue tie which meant he wasn't able to latch comfortably when breast feeding. I could tell this was the issue from day one as his older brother was also born with one and we had the same feeding issue.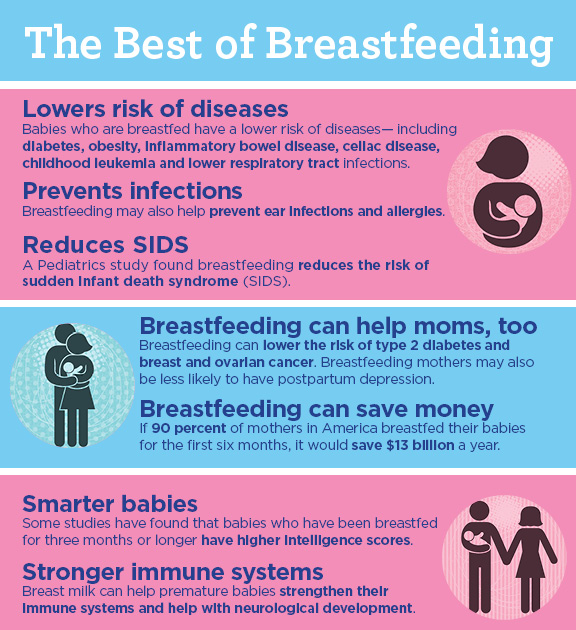
Due to the covid19 circumstances I wasn't able to get the tie cut with Jaxson as quickly as I did my 2 year old. So for 4 months I expressed every feed and bottle fed him. His tie was cut privately at 10 weeks old and I chose to continue to bottle feed.
Jaxson was a very windy baby and in the early days he really struggled to feed comfortably, he had lots of trapped wind which would not come up easily. He would cry in pain after most feeds which was very upsetting for both of us. I tried everything I could buy from the pharmacy as us mums do and also turned to social media where I found @feedeatspeak. I was scrolling though Stacey's feed and saw posts of the elevated side lying position. I immediately tried this with Jaxson who at the time was around 4 weeks old and he was a changed baby! He was able to bring up wind much easier and seemed so much more content. He actually started enjoying his feeds and upped the amount he was having quite soon after. I was one very happy Mama with a much happier baby!
So thanks to Stacey and her wonderful page, Jaxson now at 6 months old is still feeding is this position and he is one happy thriving baby!
I am so grateful for Stacey sharing this advice and information especially during lockdown as us new mums didn't really have anywhere to turn.![]() So thank you so much for helping my baby!
So thank you so much for helping my baby!
I tell all my mummy friends about this feeding position and Stacey's page hoping to help their babies who struggle with bottle feeding. It really made a huge difference with Jaxson!
bottlebottle feedingfeedingbaby feedingsidelyingelevated side lying
Stacey Zimmels
How to Bottle Feed a Premature Baby?
- Home
- Baby
- Feeding Effective Tips for Bottle Feeding Premature Babies
By Tian C - Updated: October 2, 2020
Every parent wants to make sure that their baby is taken care of right from the time of conception. Having a preterm baby comes with its own set of challenges; however, not being able to feed the baby can physically and emotionally draining. Being able to bottle feed their preemie in the NICU is a moment of pure joy for all parents, especially after having seen their baby being fed through tubes. Bottle feeding premature babies, however, is not as simple as bottle feeding a term infant and can be very tricky. Nurses are always around to assist, but here are a few tips you should know on bottle feeding your preemie.
Having a preterm baby comes with its own set of challenges; however, not being able to feed the baby can physically and emotionally draining. Being able to bottle feed their preemie in the NICU is a moment of pure joy for all parents, especially after having seen their baby being fed through tubes. Bottle feeding premature babies, however, is not as simple as bottle feeding a term infant and can be very tricky. Nurses are always around to assist, but here are a few tips you should know on bottle feeding your preemie.
When Can You Start Bottle-Feeding Your Preemie?
Usually, premature babies can bottle feed around 32 to 36 weeks of gestational age. The decision to bottle feed, however, is made by your team based on how well your baby is doing.
How to Bottle Feed a Premature Baby
Premature babies are often sleepy and not cooperative when you need to feed them; they may also not be strong enough to drink all the milk they need to support their growth. These factors make it hard to feed them initially. Keep these tips in mind before you bottle-feed your infant:
Keep these tips in mind before you bottle-feed your infant:
- Getting the time right is essential. Some babies wake up and cry when hungry, and others need to be fed on a schedule every 3 to 5 hours. Understand your baby’s rhythms and feed him when he most needs it. Feeding times ideally shouldn’t exceed 30 minutes.
- Feed the baby in a seated up position and not cradled in the arms. This is one of the best bottle feeding positions for premature babies as it ensures that they stay awake and feed on a good position. Bring him to your lap while supporting his head with your non-dominant arm. Your dominant arm can then feed the baby with a bottle.
- Offer chin and cheek support using your dominant hand while you feed your baby. The index finger and thumb go on the baby’s cheeks to give a forward and inward support. Your middle finger supports the baby’s chin to help improve sucking on the bottle nipple.
- Perform oral stimulation exercises to prepare your baby for feeding.
 Circle his lips with your fingers and gently squeeze the cheeks together to help him build a stronger suckling action.
Circle his lips with your fingers and gently squeeze the cheeks together to help him build a stronger suckling action.
- Preemies can have trouble with coordinating breathing and bottle feeding. This can lead to apnea or bradycardia in the middle of a feed. Therefore, observe for signs of danger while feeding and pause when he gags or shows signs such as a decrease in heart rate or oxygen saturation.
- Burp him frequently to release air that is swallowed during feeds. Make him sit upright and gently pat his backs for 1 to 3 minutes in between feeds or at the end.
- Some babies feed better when their NG tubes are removed. Request the nurses to take out the tube during feeds as he starts feeding better and develops strength.
- Feed him in a quiet place that is preferably dimly lit, so the feeding session goes without much fuss.
- Try the side-lying bottle feeding method for premature infants as they get stronger.
 Switching sides aids in physical development.
Switching sides aids in physical development.
- Look out for signs of choking such as spitting up, sputtering, or the baby’s face turning pale blue.
What If Your Baby Chokes While Bottle-Feeding?
Choking is one of the most concerning preemie bottle-feeding issues, and parents must always be on the watch for signs of it during feeding. If you notice that your baby starts to sputter or spit, it is a sign that you are giving more than what he can handle. When he chokes on milk or holds his breath or turns pale and blue, take the bottle out of the baby’s mouth, and make him sit upright on your lap and gently pat his backs until he looks comfortable again.
Although it is tricky at first, you’ll eventually get it right. Babies are resilient and develop every day. Keep feeding your little one and get help and guidance from doctors and nurses to feed your baby in a proper way. Enjoy this time in bonding with your infant and be patient as he progresses and learns how to feed well.
Also Read: How to Take Care Premature Baby at Home?
Previous article « 5 Nutrition Facts To Remember When You Are Breastfeeding
Next article Milk Alternatives for Toddlers »
- RELATED ARTICLES
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
Professor Katsumi Mizuno, Department of Pediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. 1 The causes of preterm birth are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth.
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit.
Why is breast milk so important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for premature babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that make it easier for the baby to digest, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended that the deficiency be replenished with donor milk rather than formula.
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious diseases that preterm infants are susceptible to, 8 such as severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
The more milk your baby gets, the lower the risk of developing diseases. 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
Most importantly, premature infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. 14 They also have a 6% lower risk of readmission in the first year of life. 15
15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. 15 In addition, their cardiovascular system works better during their lifetime. 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy. After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first.
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. 19 This is why it is important to start expressing breast milk as early as possible.
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If your baby is too weak to latch on and suckle milk, you can use a breast pump* available at the hospital or maternity hospital to “do the job for the baby”. Breast stimulation with research-based technology, 20 mimics the rhythm of the baby's suckling, plays an important role in starting and maintaining milk production in the first hours after birth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This is how your baby learns the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. You can be involved in the care of your premature baby in a variety of ways - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk.
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply.
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding?
At whatever gestational age a baby is born, if the baby is stable enough for skin-to-skin contact, it can seek the breast for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breastmilk, so you can put some milk on the nipple before putting your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety.
You can put your baby to the breast for sedative suckling as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood. You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization. Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization. Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. Prog Lipid Res . 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
2012: 985646.
4 Underwood Ma. Human Milk Formature North Am . 2013;60(1):189-207. - Underwood, M.A., "Breast milk for the premature baby." 1):189-207.
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight. Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312.
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 12 MEIER PP ET AL AL AL AL . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." Perinatol wedge. (Clinical perinatology). 2010;37(1):217-245. 13 Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523. 14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. 15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123. 16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". 17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." Pediatrix (Pediatrics). 2016;138(1):pii:e20160050. 18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499. 19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. 20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-110. 21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. 22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366. - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. 23 Prime PK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping. 24 Uvn ä s Moberg K Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206. 25 Boundy EO et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". Pediatrix (Pediatrics). 2015;137(1): e20152238. 26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. J Hum Lact . 27 Nyqvist KH et al. Towards universal kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on kangaroo mother care. Acta Paediatr . 2010;99(6):820-826.- Nukvist K.H. et al., "On the Universality of the Kangaroo Method: Recommendations and Report from the First European Conference and the Seventh International Kangaroo Method Workshop". Akta Pediatr. 2010;99(6):820-826. 28 American Academy of Pediatrics - Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics . 2012;129(3): e 827-841.- American Academy of Pediatrics - Section "Breastfeeding", "Breastfeeding and the use of breast milk". *RU No. ФСЗ 2010/06525 dated 03/17/2021 complain Updated Content: Preparation for feeding Proper feeding of a bottle of What to do after feeding Feature features of a bottle of premature 9000 9000 You can bottle feed your baby with both expressed breast milk and an adapted formula recommended by your pediatrician. Despite the seeming simplicity, this process must be organized correctly, step by step performing all the necessary steps. How is it right for a mother to bottle feed a newborn? Wash your hands thoroughly with soap and warm water before feeding your baby. The bottle and nipple must be sterilized beforehand. Before expressing breast milk, you should also wash your hands and rinse your breasts. If the baby is receiving formula milk, boil the water for formula and then cool it to 40 degrees. Tap and spring water contains not only microorganisms that are destroyed by boiling, but also various impurities (chemicals, salts of heavy metals, etc.) that can harm the health of the crumbs. Pour the required amount of mixture into a sterilized bottle of prepared water. Do not shake the bottle to avoid foam formation. It is better to roll it between the palms so that the mixture dissolves. Check the temperature of the formula before offering it to your baby. If milk formula or expressed milk has been stored in the refrigerator, it is necessary to warm it up using a water bath or a special heater. It is not recommended to use a microwave oven to heat formula or milk. It is better to hold the baby in the same way as when breastfeeding: the baby is reclining on the mother's arm bent at the elbow, while the head is slightly above the body. Make sure there is air in the bottle to prevent flattening of the nipple. The absence of air bubbles entering the bottle may indicate that the baby is not grasping the nipple correctly. If a mother is breastfeeding her baby and supplementing her with formula, then the baby must first receive the breast and then bottle formula. After feeding, the baby should be held upright for a while to let the air out. Then you can once again offer him a bottle in order to make sure that he is satisfied. Leftover formula should not be stored until the next feeding. It is better to pour them out, and wash the bottle and nipple immediately. If the baby falls asleep immediately after feeding, do not leave him sleeping with a bottle. This can cause choking. An acidic environment can lead to oral diseases. Preterm infants can be bottle-fed if their sucking and swallowing are coordinated and there are no breathing problems requiring oxygen support. The volume and type of the adapted mixture is prescribed by a pediatrician who monitors the weight gain and physical development of the baby on a daily basis. During feeding, the mother monitors the baby's breathing, skin color, and general condition. In case of deterioration of health, feeding should be stopped and urgently consult a doctor. Of course, the best food for a newborn is breast milk. But if for some reason breastfeeding is not possible, do not despair. Feeding a baby from a bottle does not mean at all that he will somehow grow and develop differently. Find advantages in this alternative. For example, not only mom can feed a baby from a bottle, but also dad, and other relatives of the baby, which means that he will never be deprived of attention and care. And if the family is replenished with twins or triplets, bottle feeding will be a very good way to feed all the babies at the same time if necessary. References  2017;102(3): F 256- F 261.
2017;102(3): F 256- F 261.  Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406.
Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406.  Lancet (Lancet). 2016;387(10017):475-490.
Lancet (Lancet). 2016;387(10017):475-490.  J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209.
J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209.  Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91.
Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91.  " Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
" Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.  2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46
2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46  Pediatrix (Pediatrics). 2012;129(3): e 827-841.
Pediatrix (Pediatrics). 2012;129(3): e 827-841. Read instructions before use. Consult a specialist about possible contraindications.
How to properly bottle feed a newborn: postures and rules
Preparation for feeding

 To do this, put a few drops of milk on the inside of the wrist. The skin here is sensitive, as in the mouth of the crumbs.
To do this, put a few drops of milk on the inside of the wrist. The skin here is sensitive, as in the mouth of the crumbs. Proper bottle feeding of a newborn
 The nipple should always be filled with formula or milk. If the bottle is held vertically, the baby may choke.
The nipple should always be filled with formula or milk. If the bottle is held vertically, the baby may choke.

What to do after feeding
Features of bottle feeding premature babies

videos