Breast feeding lactose intolerant baby
Lactose intolerance and Breastfeeding - The Breastfeeding Network
This information can also be viewed as a PDF by clicking here.
The information provided is taken from various reference sources. It is provided as a guideline. No responsibility can be taken by the author or the Breastfeeding Network for the way in which the information is used. Clinical decisions remain the responsibility of medical and breastfeeding practitioners. The data presented here is intended to provide some immediate information but cannot replace input from professionals.
Lactose is the sugar in all mammalian milks.The amount of lactose in breastmilk is independent of the mother’s consumption of lactose and hardly varies.The quantity of lactase, the enzyme needed to breakdown the sugar, does vary. |
Lactose intolerance occurs when a person does not produce the enzyme lactase, or does not produce enough of it, and is therefore unable to digest lactose. If it is not digested and broken down, lactose cannot be absorbed. The undigested lactose passes rapidly through the gut until it is broken down by bacteria, producing acids and gas. The production of lactase decreases in most humans from the age of two years although symptoms of intolerance are rare before the age of six. Lactose intolerance in adults is very common. Lactose intolerance is not the same as intolerance to cows’ milk protein (Anderson).
Primary lactose intolerance is a rare, inherited metabolic disorder. It is incompatible with life without medical intervention and a lactose free diet. A truly lactose-intolerant baby would fail to thrive from birth (i.e. not even start to gain weight) and show obvious symptoms of malabsorption and dehydration (Kellymom). Savilahti et al identified only 16 cases of congenital lactase deficiency over 17 years despite the fact that the genes are very common in Finland. In each case the mother reported watery diarrhoea usually after the first breastfeed but up to 10 days after birth. Poor absorption of lactose was confirmed between 3 and 90 days after delivery at which time all infants were dehydrated and 15 of the 16 weighed less than at birth. On a lactose feed diet the children all caught up with their growth. Some premature babies are temporarily lactose intolerant due to their immaturity.
Poor absorption of lactose was confirmed between 3 and 90 days after delivery at which time all infants were dehydrated and 15 of the 16 weighed less than at birth. On a lactose feed diet the children all caught up with their growth. Some premature babies are temporarily lactose intolerant due to their immaturity.
Secondary lactose intolerance can appear at any age due to damage to the brush borders of gut villae (where lactase is produced) by infection, allergy or inflammation. This reduces lactase activity. It is a temporary condition and removal of the cause permits the gut to heal. It may also become apparent in a breastfed baby following maternal use of antibiotics but resolves without treatment even with continued breastfeeding (Anderson).
Healthcare professionals should only recommend the use of lactose-free artificial baby milk if the baby is artificially-fed and is very malnourished and/or losing weight. Breastmilk remains the optimal milk and will assist with gut healing in secondary lactose intolerance (Shulman). Average recovery time for the gut of a baby with severe gastroenteritis is 4 weeks, but may be up to 8 weeks for a baby under 3 months. For older babies, over about 18 months, recovery may be as rapid as 1 week. Medical advice should be sought for any baby with long-term symptoms and/or who is failing to thrive.
Average recovery time for the gut of a baby with severe gastroenteritis is 4 weeks, but may be up to 8 weeks for a baby under 3 months. For older babies, over about 18 months, recovery may be as rapid as 1 week. Medical advice should be sought for any baby with long-term symptoms and/or who is failing to thrive.
Lactose intolerance is often blamed as being a contributory factor for colic, resulting in cessation of breastfeeding and substitution of lactose free formula. Infants with gastrointestinal symptoms on exposure to cows’ milk are more likely to have cows’ milk allergy than lactose intolerance (Jones)
Green and frothy bowel motions may be a sign that the baby is receiving too much lactose, which has a rapid gut transit time. This may be due to an excess of the early less fat-rich milk or switching the baby between breasts before emptying one breast first. Babies may be very unsettled and windy. Mothers may have an overactive letdown reflex.
Assessment by an experienced breastfeeding worker may be beneficial to ensure optimal milk removal by the baby is taking place before considering lactose free formulae. Imbalance of milk transfer (caused by less than perfect attachment) can produce similar symptoms i.e. loose bowel motions, which may be green and frothy. This is due to the rapid transit time of large volumes of lower fat milk and consequently an excessive consumption of lactose (Woolridge 1988). Breast compression when the baby is not actively sucking may improve milk transfer.
Imbalance of milk transfer (caused by less than perfect attachment) can produce similar symptoms i.e. loose bowel motions, which may be green and frothy. This is due to the rapid transit time of large volumes of lower fat milk and consequently an excessive consumption of lactose (Woolridge 1988). Breast compression when the baby is not actively sucking may improve milk transfer.
Babies can exhibit excess wind and gastric discomfort, which may be diagnosed as lactose intolerance, but which in fact is transitory lactase deficiency i.e. too much lactose for the available lactase.
Addition of lactase enzymes (Colief®) to breastmilk has been suggested as a treatment for colic. Kanabar et al (2001) conducted a study of 53 babies Formula or expressed “fore-milk” had lactase or placebo added and incubated for a period before being given to the baby. Formula was refrigerated for four hours, and then re-warmed. “Fore-milk” was incubated during the feed and given at the end of the feed. Total crying time over the 10-day treatment period was reduced in all 46 and in the 32 compliant families reached statistical significance. Lack of compliance (undefined), was possibly due to a high proportion of non-native English speakers.
Total crying time over the 10-day treatment period was reduced in all 46 and in the 32 compliant families reached statistical significance. Lack of compliance (undefined), was possibly due to a high proportion of non-native English speakers.
Lactose is a specific nutrient for infancy, supplying about 40% of the baby’s energy needs, facilitating calcium, magnesium, zinc and iron absorption, promoting a normal healthy gut by promoting the growth of bifidobacterium, and providing the galactose which is incorporated directly as galactolipids into the tissues of the central nervous system (Akre 1990). Soya formula is not recommended for children under six months
Soya milk is not recommended as substitute milk for babies under six months due to phyto-oestrogens and high sugar content. Babies who are cow’s milk protein allergic are likely to be allergic to soya protein as well (Chief Medical Officer, COT)
Lactose intolerance is very common in adults. The production of lactase decreases from approximately 2 years of age although symptoms are rare before 6 years of age.
- Akre J (ed) 1990 Infant Feeding: the physiological basis supplement to vol 67 of the WHO Bulletin WHO, Geneva. 27-28.
- Anderson J Lactose intolerance and the breastfed baby. www.breastfeeding.asn.au/bf-info/lactose
- CMO update 37. 2007 soya milk (infant formula) www.dh.gov.uk/en/Publichealth/Nutrition/Nutritionpregnancyearlyyears/DH_127640
- Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment (2003). Phytoestrogens and Health. http://cot.food.gov.uk/sites/default/files/cot/cotlsumphytos.pdf
- First Steps Nutrition Specialised Infant Formula www.firststepsnutrition.org/pdfs/draft_specialised_milks_mar_2013.pdf
- Jones W Breastfeeding and Medication Routledge 2018
- Kanabar D1, Randhawa M, Clayton P. Improvement of symptoms in infant colic following reduction of lactose load with lactase. J Hum Nutr Diet. 2001 Oct;14(5):359-63.
- KellyMom Lactose Intolerance http://kellymom.com/health/baby-health/lactose-intolerance/
- NHS Lactose Intolerance includes dietary sources of lactose.
 www.nhs.uk/Conditions/lactose-intolerance/
www.nhs.uk/Conditions/lactose-intolerance/ - Noble R & Bovey A Resolution of Lactose Intolerance and Colic in Breastfed Babies www.health-e-learning.com/articles/Lactose.pdf
- Savilahti E, Launiala K, Kuitunen P. Congenital lactase deficiency. A clinical study on 16 patients. Arch Dis Child 1983;58:246-252
- Shulman R, Feste A, Ou C (1995). Absorption of lactose, glucose polymers or combination in premature infants. Journal of Pediatrics, 127, 626-631.
- Woolridge MW, Fisher C. Colic, “overfeeding”, and symptoms of lactose mal-absorption in the breast-fed baby: a possible artifact of feed manage-ment?Lancet
©Dr Wendy Jones MBE, MRPharmS and the Breastfeeding Network Sept 2019
Lactose Intolerance in Babies - Breastfeeding Support
Lactose is the main sugar found in breast milk. It is produced in the breast, it doesn’t come from a mother’s diet. Lactose is very important for the normal health and development of human babies. It provides about 40% of a baby’s energy needs, helps with calcium and iron absorption, promotes friendly bacteria Lactobacillus bifidus, keeps pathogenic bacteria in the gut at bay, and is important for development of the large and complex human brain and central nervous system 1.
Sign Up to the Newsletter
Get breastfeeding articles in your inbox
Lactose intolerance in babies
Lactose intolerance is the inability to digest lactose. True lactose intolerance is very rare in babies because breast milk, the biologically normal food, is full of lactose and babies are usually very well adapted to digest it. This article looks at types of lactose intolerance in babies, causes and symptoms of lactose overload and ways to avoid it.
Types of lactose intolerance in babies
Babies are either born with lactose intolerance due to a metabolic disorder (a rare but serious risk to health) or they can get a temporary form of it with several possible causes (much less serious). Different names are used for the different types of lactose intolerance and these vary slightly between authors.
#1 True lactose intolerance
(also called primary or congenital lactose intolerance)
A specific enzyme called lactase breaks lactose down into glucose and galactose (more sugars). It is produced in tiny folds (called brush borders) in the lining of a baby’s intestine. There are a few rare metabolic disorders that mean a baby doesn’t produce enough of this enzyme. True lactose intolerance is very rare, but when present it will be diagnosed within a few days of birth due to the severe and serious symptoms like vomiting, diarrhoea, jaundice and failure to thrive2. Your health professionals will advise on a special diet for your baby.
It is produced in tiny folds (called brush borders) in the lining of a baby’s intestine. There are a few rare metabolic disorders that mean a baby doesn’t produce enough of this enzyme. True lactose intolerance is very rare, but when present it will be diagnosed within a few days of birth due to the severe and serious symptoms like vomiting, diarrhoea, jaundice and failure to thrive2. Your health professionals will advise on a special diet for your baby.
#2 L
actose overload(also called secondary or temporary lactose intolerance.)
If there is too much lactose in the gut for the enzyme to digest, symptoms of wind (gas), tummy ache and copious frothy green or watery stools may be seen. This is much more common than “true” lactose intolerance. The rest of this article discusses causes, symptoms and remedies for this type of temporary lactose intolerance in babies.
Is lactose intolerance the same as cows’ milk allergy?
No. Having a reaction to traces of cows’ milk protein that enter breast milk via the mother’s diet is not the same as lactose intolerance or lactose overload. However an ongoing food allergy can damage the lining of the gut where the enzyme needed to digest lactose is produced, causing symptoms of lactose overload. Lactose overload and cows’ milk allergy can therefore both be present at the same time.
Eliminating lactose from a mother’s diet won’t help a baby’s symptoms of lactose overload because lactose is added to breast milk in the breast. However, if the real issue is sensitivity to cows’ milk protein then avoiding foods with lactose probably will help the symptoms because cows’ milk proteins and lactose tend to be found in the same foods.
What causes lactose overload?
Anything that prevents lactose being digested properly in the intestines can cause lactose overload. This might be damage to the special cells that produce the enzyme in the intestine, or if the volume of low fat breast milk passing through the intestines overwhelms the available enzyme.
This might be damage to the special cells that produce the enzyme in the intestine, or if the volume of low fat breast milk passing through the intestines overwhelms the available enzyme.
Damage to the intestinal lining
If there is any damage to the intestinal lining it can affect the production of the enzyme lactase which is produced in the delicate brush borders of the baby’s intestines. Types of damage include inflammation (e.g. irritation from cows’ milk allergy or gluten), bacterial or viral infection (e.g. gastroenteritis) or antibiotic use. Other possible causes of damage include partially digested formula, parasites, and some mothers notice a connection with live vaccines such as rotavirus (Minchin, 2015). If there is not enough enzyme, large amounts of lactose can pass undigested to the lower bowel. Here it will be fermented by bacteria giving the familiar symptoms of gas, discomfort and lots of green watery stools.
Damage to the brush borders may take some time to heal. Joy Anderson says:
Joy Anderson says:
Excerpt from
Lactose Intolerance and the Breastfed Baby, Australian Breastfeeding Association, 2017
Average recovery time for the gut of a baby with severe gastroenteritis is 4 weeks, but may be up to 8 weeks for a baby under 3 months. For older babies, over about 18 months, recovery may be as rapid as 1 week.
Too much lactose
A big breast milk feed with a normal lactose content but low fat content can pass through to the lower bowel too quickly for the lactose to be digested properly. This can lead to colic type symptoms of wind (gas), tummy ache and green or watery stools. When breast milk has a higher fat content, it slows the transit time in the bowel, giving time for proper digestion3. Possible causes for an excess of low fat milk tend to be connected to breast storage capacity and how often a baby changes breasts while breastfeeding.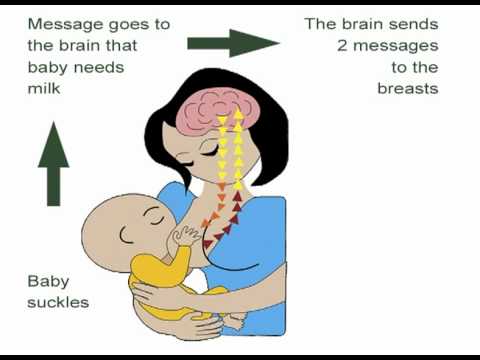 A lactose overload is more likely for the mother who has a very large amount of breast milk or who tends to stop a feed before a baby has finished draining one breast. An IBCLC lactation consultant can help you identify how to avoid this type of lactose overload, and see:
A lactose overload is more likely for the mother who has a very large amount of breast milk or who tends to stop a feed before a baby has finished draining one breast. An IBCLC lactation consultant can help you identify how to avoid this type of lactose overload, and see:
- Oversupply of Breast Milk
- One Breast or Two per Feed
- What is a Fast let-Down?
- Colic in the Breastfed Baby (by Dr Jack Newman).
Immaturity
Some premature babies might not produce enough lactase until they mature. This is known as developmental lactase deficiency4.
What causes lactose intolerance in adults?
In many cultures across the world, levels of the enzyme lactase start to fall after three to seven years of age (to correspond with weaning). They often fall so low (particularly in non-Caucasian groups) that an individual may become lactose intolerant (unable to digest lactose). This may not happen until adulthood and will affect consumption of cows’ milk products with lactose. This is not the same as lactose intolerance in babies 5. Mohrbacher, 2010 reserves the name primary lactose intolerance for this adult type.
This may not happen until adulthood and will affect consumption of cows’ milk products with lactose. This is not the same as lactose intolerance in babies 5. Mohrbacher, 2010 reserves the name primary lactose intolerance for this adult type.
Symptoms of lactose overload in babies
Good weight gain but windy, unsettled, lots of poop
A baby with lactose overload might typically gain weight very well but show several of the following colic type symptoms:
- Flatulence. Note that swallowing of air during a feed is not thought to be a cause of a baby’s flatulence or colic symptoms as excess air is burped out through the mouth67
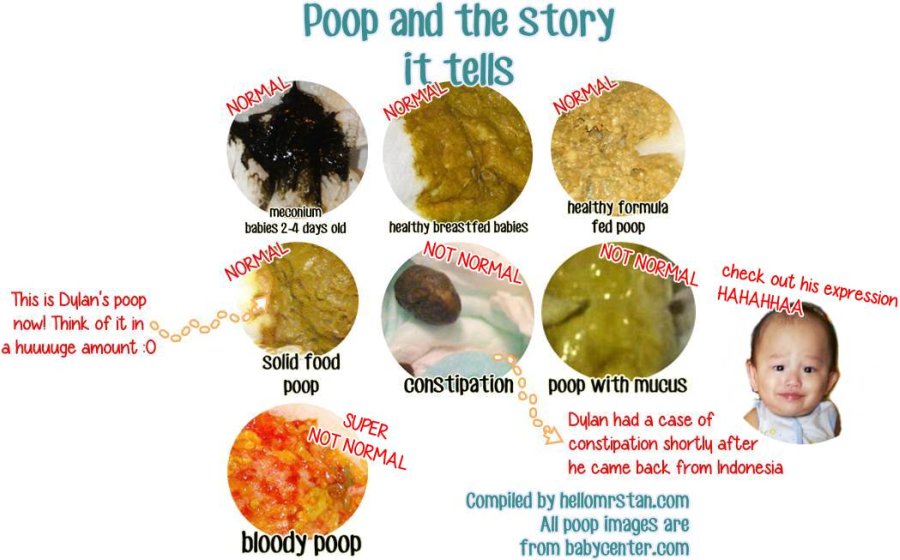
- Loads of explosive green or yellow frothy, foamy or watery poop.
 Note: there can be several other causes of green poop too.
Note: there can be several other causes of green poop too. - Tummy ache or “colic”
- Unhappy, unsettled baby
- Nappy rash
- Mucousy poop
Where milk allergy is the underlying cause other symptoms may be present as well see Milk Allergy in Babies.
Poor weight gain is possible
Not all babies continue to gain weight well and some may even fail to thrive as the milk is passing through the gut too quickly to be digested and absorbed;
Excerpt from
Milk Matters: Infant feeding & immune disorder Maureen Minchin, 2015, p586
Some babies lose so much weight from the rapid passage of all food that they fail to thrive, although the mother often has a booming milk supply from all the stimulation, needing breast pads to mop up leakage.
Blood in the stools?
Constant irritation to the intestines may also give rise to small amounts of bleeding in the stools. Linda Palmer explains:
Excerpt from
Baby Poop: What Your Pediatrician May Not Tell You … about Colic, Reflux, Constipation, Green Stools, Food Allergies, and Your Child’s Immune Health, Linda Palmer, 2015
Lactose may come in faster than baby’s available amounts of lactose digesting enzyme, lactase, can respond.
In this case, some of the lactose can sit undigested in the bowel, causing water to rush in to dilute the sugar, leading to loose stools, and allowing bacteria to ferment it, which causes smelly gas. Over time this situation can keep the intestines irritated and cause a little bleeding. Such chronic irritation can cause a drop in lactase enzyme production. This can create a vicious cycle.
Evening colic
Some breastfed babies seem to have colic type symptoms every evening at a set time but are quite cheerful the rest of the day or night. Author Maureen Minchin hypothesises that this could be due to “lactose overload” from the first feed in the morning i.e. when there is a lot of low fat, lactose rich breast milk on a relatively empty tummy (Milk Matters, 2015).
How to avoid lactose overload
Finding the reason for lactose overload and knowing what to do about it will usually improve the symptoms without needing to stop breastfeeding. To help find the right answer for you from the ideas below ask your IBCLC lactation consultant for help. Options include:
Options include:
Finish the first breast, offer the second
The fat content of breast milk increases during a feed and also increases the closer together the feeds are. If a mother is shortening feeds (perhaps because of painful nipples) or feeding on a schedule this could lower the fat content in breast milk. Less fat reduces the time spent in the stomach (gastric clearance time) resulting in the lactose passing through the stomach and bowel without being properly digested (Noble & Bovey, 1998). Finishing the first breast before offering the second side will help your baby to get the proportion of higher fat milk he needs.
Stay on one breast per feed if needed
If a mother has a very large storage capacity she may only need to feed from one breast per feed so that her baby can get a good balance of higher fat milk. Jack Newman explains (with a caution!):
Excerpt from
Dr. Jack Newman’s Guide to Breastfeeding (updated edition)Jack Newman and Teresa Pitman, 2014, p.
 181
181 In some situations where the baby is colicky from getting too much milk too quickly, and fixing the latch and finishing one side before offering the other breast does not work, it may be worthwhile to try giving one breast at a feeding or even two feedings in a row. The mother needs to be aware that this may cause her milk production to decrease, and that the baby may fuss because he’s not getting as much milk as he wants—even if he is still gaining weight well.
Breast compressions
Using breast compressions and breast massage can help to mix the fat content of breast milk and release more higher fat milk. 8 9.
Be flexible
Feeding plans such as block feeding (staying on one breast per feed or for a set period of time) need to be flexible.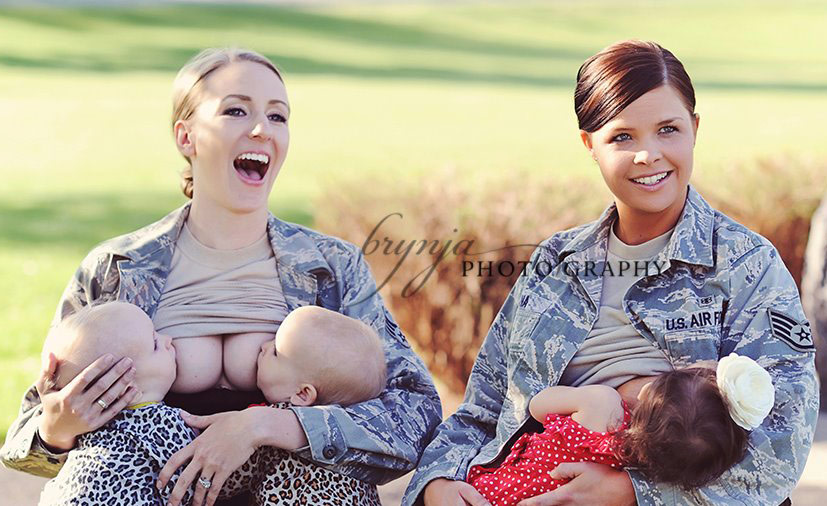 Just because a baby wants one breast in a morning may not be the case by the evening when he might need both breasts per feed. Similarly what works at two months of age to cure fussy behaviour may need changing in a few weeks time or during a growth spurt.
Just because a baby wants one breast in a morning may not be the case by the evening when he might need both breasts per feed. Similarly what works at two months of age to cure fussy behaviour may need changing in a few weeks time or during a growth spurt.
Excerpt from
Colic in the Breastfed Baby, Jack Newman & Edith Kernerman, 2009
It is not a good idea to feed the baby on just one side, to follow a rule. Yes, making sure the baby “finishes” the first side before offering the second can help treat poor weight gain or colic in the baby, but rules and breastfeeding do not go together well. If the baby is not drinking, actually getting milk, there is no point in just keeping the baby sucking without getting any milk for long periods of time. You should “finish” one side and if the baby wants more, offer the other.
Is food allergy the cause?
The underlying cause of difficulty digesting lactose could be an allergy or intolerance to cows’ milk protein (in breast milk via mother’s diet). Over time an allergy may cause inflammation and irritation to baby’s gastrointestinal tract causing the symptoms of lactose overload. For further information see Milk Allergy in Babies and Elimination Diet for further reading.
Over time an allergy may cause inflammation and irritation to baby’s gastrointestinal tract causing the symptoms of lactose overload. For further information see Milk Allergy in Babies and Elimination Diet for further reading.
Not enough milk?
An unhappy baby with scant green nappies may not be getting enough milk rather than the problem being milk allergy or lactose overload. Sometimes a fussy baby who seems to want to feed a lot is just “hanging out” at the breast but not getting enough milk. Advice to stay on one breast per feed or for several feeds is not appropriate here. Your IBCLC can help you decide what is going on and see How to Make More Breast Milk for lots of ideas to increase your milk supply.
Jack Newman points out on his Facebook page:
Many babies diagnosed with “allergy” to something in the milk get better when put on special formulas. Why? Not because they are no longer exposed to the mother’s milk, but rather because now the baby gets more milk.

Mother’s diet
Lactose is produced in the breast, and the amount of lactose containing foods a mother eats won’t make a difference to the lactose content in breast milk. However maternal diet can be important:
- If there is inadequate fat in the mother’s diet this can make lactose overload worse for baby ( Noble and Bovey, 1998). See Best Breastfeeding Diet and Foods to Avoid for more information.
- If a baby is sensitive to cows’ milk protein (in breast milk via mother’s diet) this may cause inflammation and irritation to baby’s gastrointestinal tract which can then cause symptoms of lactose overload. See Elimination Diet for more information.
Lactase drops
There are anecdotal reports that drops containing the enzyme lactase can be used to predigest lactose in expressed milk (Joy Anderson, 2012)(Palmer, 2015).
Continue to breastfeed
Jack Newman, Canadian paediatrician and breastfeeding expert, discusses breastfeeding management in more detail in Colic in the Breastfed Baby. He explains that the best way to deal with lactose overload is to improve the baby’s latch, know how to spot when a baby isn’t really swallowing milk, to use breast compressions before switching sides and then offer the second breast and repeat. If baby is gaining weight and feeding well he advises continuing to breastfeed.
He explains that the best way to deal with lactose overload is to improve the baby’s latch, know how to spot when a baby isn’t really swallowing milk, to use breast compressions before switching sides and then offer the second breast and repeat. If baby is gaining weight and feeding well he advises continuing to breastfeed.
My doctor said I should stop breastfeeding
Some doctors are confused about temporary lactose intolerance, milk allergy and colic. They may recommend lactose-free formula or newer ‘special’ formulas. However the answer to most cases of temporary lactose intolerance is to get help with breastfeeding rather than switch to industrial formulas. A baby with an irritated intestine needs the anti inflammatory effects of breast milk and a breastfeeding specialist can help suggest changes to feeding management10.
Excerpt from
Breastfeeding Works! Even With Allergies, Noble, 2015
it is sinister that artificial baby milks, however specialised are promoted as being superior milks for allergic babies.
It is even more insidious to hear such messages reiterated by paediatric specialists working with these children and their families. p46
…formulas are
- concentrated sources of the problem proteins
- without the advantage of having been processed by maternal digestion
- utterly devoid of the other benefits bestowed by her milk. p47
My doctor says tests confirm my baby has lactose intolerance
Some doctors might diagnose lactose intolerance if they measure excess acid (reducing sugars) in a baby’s poop or hydrogen gas in a baby’s breath due to temporary lactose intolerance (Palmer, 2015, p 141). Noble and Bovey state that the presence of reducing sugars in a baby’s poop can be quite normal for breastfed babies particularly under six weeks of age11 while the Australian Breastfeeding Association says both a hydrogen breath test and a test for reducing sugars in the stool are often positive in normal breastfed babies under three months of age12. James Akre explains:
James Akre explains:
Excerpt from
James Akre, Infant Feeding the Physiological Basis, WHO, 1992
It is usual to find reducing substances such as sugars in the stools of healthy breast-fed infants; they contribute to maintaining the acid environment that retards the growth of pathogens. In contrast, the delayed gut transit time of industrially prepared milks permits almost total metabolism of these sugars.
Summary
Lactose is the main sugar in breast milk. It is made in the breast and does not come from the mother’s diet. It is very rare for a baby to be truly intolerant to lactose. However there can be times when there is so much lactose it is difficult for the baby to digest. This is often called a lactose overload and, when undigested in the gut, lactose gets broken down or fermented by bacteria to give gas, discomfort and lots of frothy watery poop. A food allergy can be a cause of symptoms of lactose overload or certain breastfeeding management regimes. An IBCLC lactation consultant can help identify causes and work with you to help avoid a baby getting symptoms of lactose overload.
An IBCLC lactation consultant can help identify causes and work with you to help avoid a baby getting symptoms of lactose overload.
Footnotes & References
-
Core Curriculum for Lactation Consultant Practice, ILCA, 2013
-
Bonyata, Is my baby lactose intolerant? 2018
-
Anderson, Lactose Overload in Babies, Australian Breastfeeding Association, 2019
-
Mohrbacher, Breastfeeding Answers Made Simple, 2010
-
Wambach & Riordan, Breastfeeding and Human Lactation, 2015
-
Breastfeeding Works! Even With Allergies, Noble, 2015
-
Resolution of Lactose Intolerance and Colic in Breastfed Babies, Noble & Bovey, 1998
-
Smillie, From the perils of block feeding to the magic of a milkshake: addressing the challenges of hyperlactation, iLactation, 2019
-
Morton et al, Combining hand techniques with electric pumping increases the caloric content of milk in mothers of preterm infants, J Perinatology, 2012
-
Baby Poop What Your Pediatrician May Not Tell You, Linda Palmer, 2015, p 141
-
Noble and Bovey, Resolution of Lactose Intolerance and “Colic” in Breastfed Babies, health-e-learning.
 com, 1998
com, 1998 -
Lactose Intolerance and the Breastfed Baby, Australian Breastfeeding Association, 2017
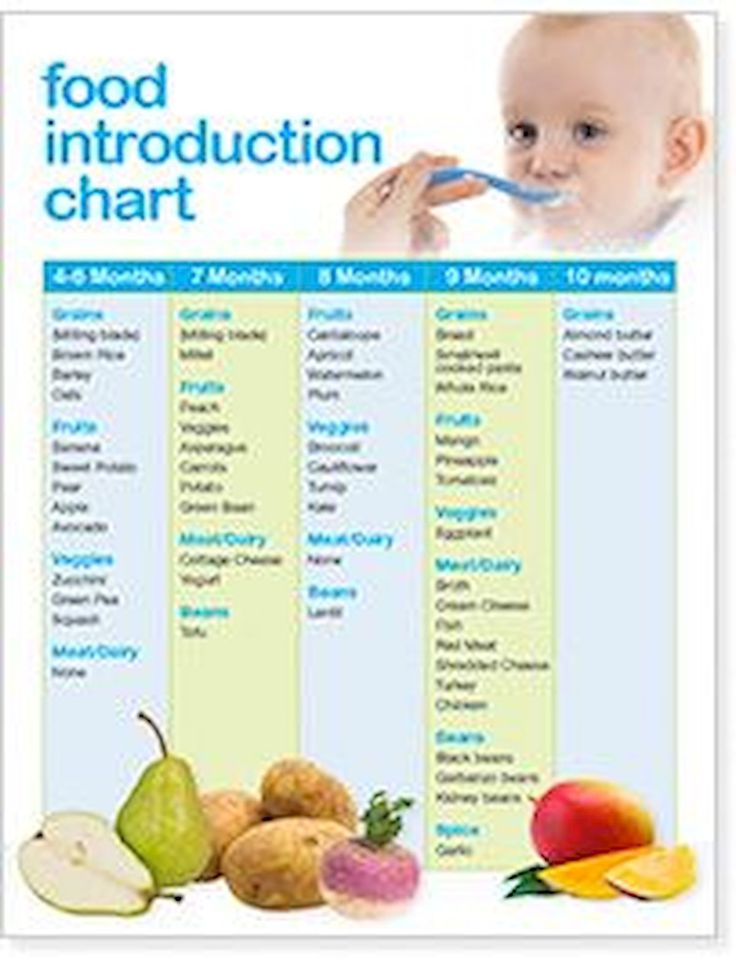
Feeding a child with lactase deficiency
Lactase deficiency in a baby gives rise to many questions and fears in parents. The reason is the lack of lactase enzyme in the child's body. Lactase is responsible for the breakdown of milk sugar (lactose) into simpler substances that are absorbed and used by the body as a source of energy and nutrients.
It is divided into primary - congenital (transient) in immature newborns and adult type LN (genetic defect) and secondary - when intestinal cells are damaged by infection, celiac disease, etc.
In children of the first months of life, lactose deficiency is more often transient (temporary) against the background of immaturity of the gastrointestinal tract, after an intestinal infection, allergies and other causes. Congenital complete lactase deficiency is rare, occurring in 5-6% of cases. These are lifelong lactose-free mixtures or ready-made lactase enzyme in breast milk.
These are lifelong lactose-free mixtures or ready-made lactase enzyme in breast milk.
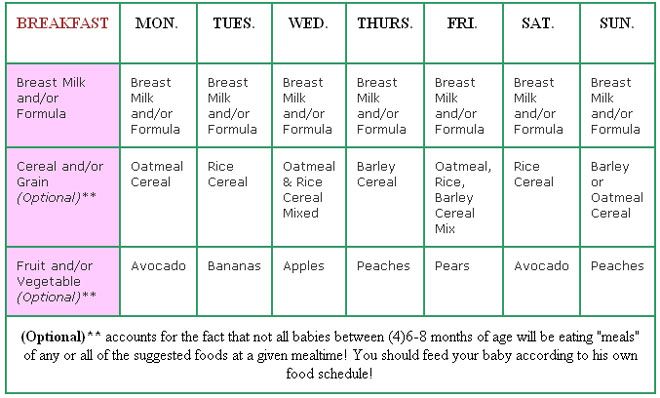
Recommendations for nutrition in case of lactase deficiency
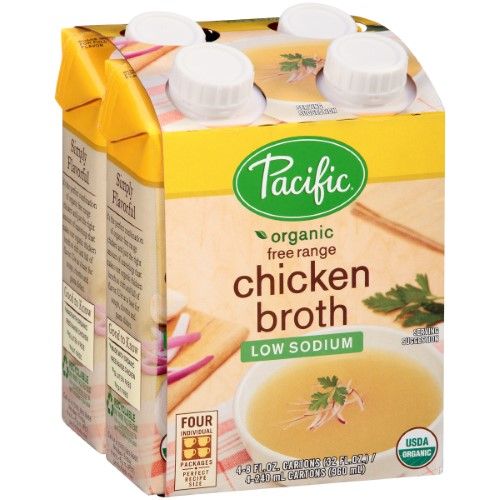
If the child is breastfeeding, then lactase dissolved in warm milk is given before meals, then breastfeeding. If artificial feeding - lactose-free mixtures in a short course or low-lactose, sour-milk, which the doctor selects, according to the condition of the child. nine0003
If the baby has already received complementary foods of cottage cheese and yogurt, then as the intestines recover, fermented milk products are slowly introduced - yogurt, but not kefir.
If a child after a year after suffering an intestinal infection, then during the period of manifestations, milk is also removed from the diet, we cook cereals without milk, instead of milk, you can use lactose-free mixtures for medical nutrition older than a year (clinutren junior, nutrini).
You can have a little hard cheese (parmesan), it does not contain lactose, as the condition improves, slowly yogurt (not kefir, not snow) and cottage cheese in the form of a casserole.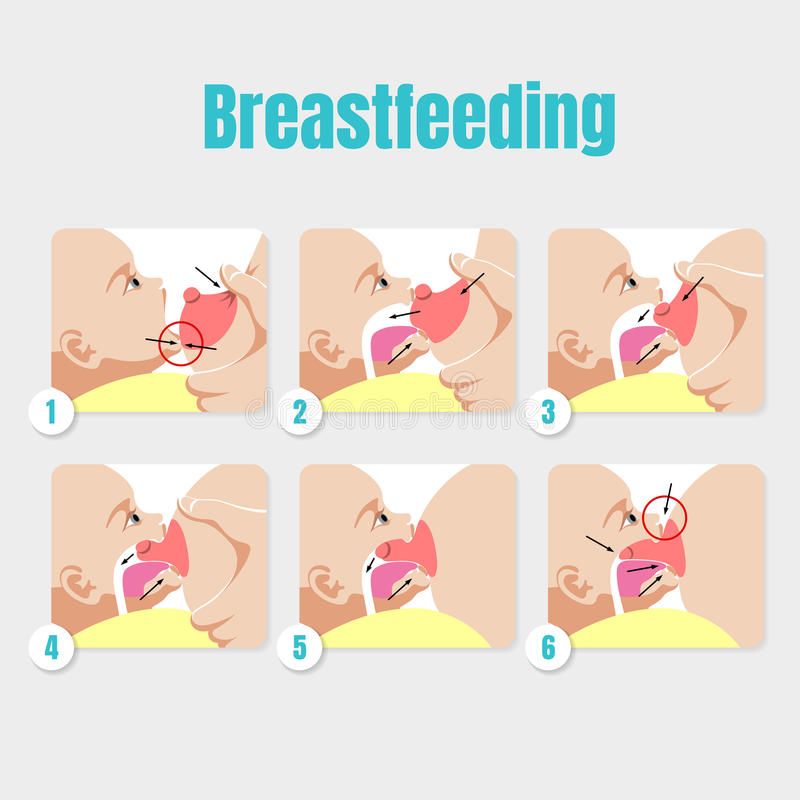 nine0003
nine0003
What to do if the child has lactase deficiency
If parents see that the child has signs of lactase deficiency, the first thing to do is contact a specialist. Only an experienced pediatrician will be able to figure out why the baby has colic or green stools, what the numbers in the tests say, and what is the norm for one baby and the pathology for another.
And of course, it is not necessary to cancel breastfeeding and immediately prescribe lactose-free or low-lactose artificial formulas (even as a supplement). By itself, milk sugar lactose is very necessary for a child, when lactose is broken down, its components (glucose and galactose) go to the development of the brain, retina, for the life of normal intestinal microflora. So do not completely eliminate this sugar, you need to help it break down. With a strongly pronounced LN, the missing enzyme is given before each feeding (it has long been learned to produce and it is sold in pharmacies), with a dim clinic, its dose can be reduced.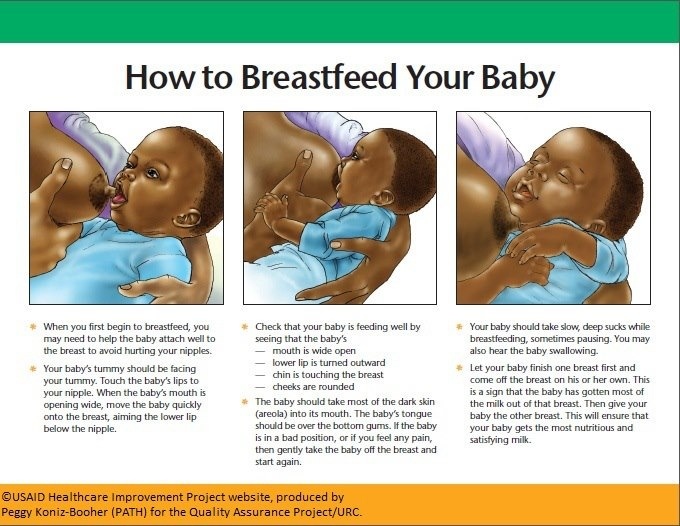 nine0003
nine0003
Schedule of doctors. ✔ Price list for the services of MC Trust.
To make an appointment, get advice, please call:
+7 (423) 267-61-30; +7 (423) 274-32-22; +7 914-704-32-22.
Or fill out the online form:
PediatricianGeneral practitionerUltrasound doctorGastroenterologistHematologistGynecologistImmunologist-allergistInfectionistCardiologistNeurologistOtorhinolaryngologist (ENT)Orthopedist-traumatologistOphthalmologistPsychiatristUrologist-andrologistPhysiotherapistPhthisiatricianSurgeonEndocrinologistHouse doctorVaccinationMedical examinationTestsOnline consultation Conclude an observation agreement (subscription)
I agree to the processing of data
Please enable JavaScript to pass the CAPTCHA test
If you have any questions, please use the comment form below↓↓↓
Leave This Blank:Leave This Blank Too:Do Not Change This: Your email:
Breastfeeding and Lactose Intolerance Manufacturing Companies
infant formula milks like to use the label to their advantage, such as in the advertisement for Similac Sensitive®: For restless behavior and gas caused by lactose intolerance.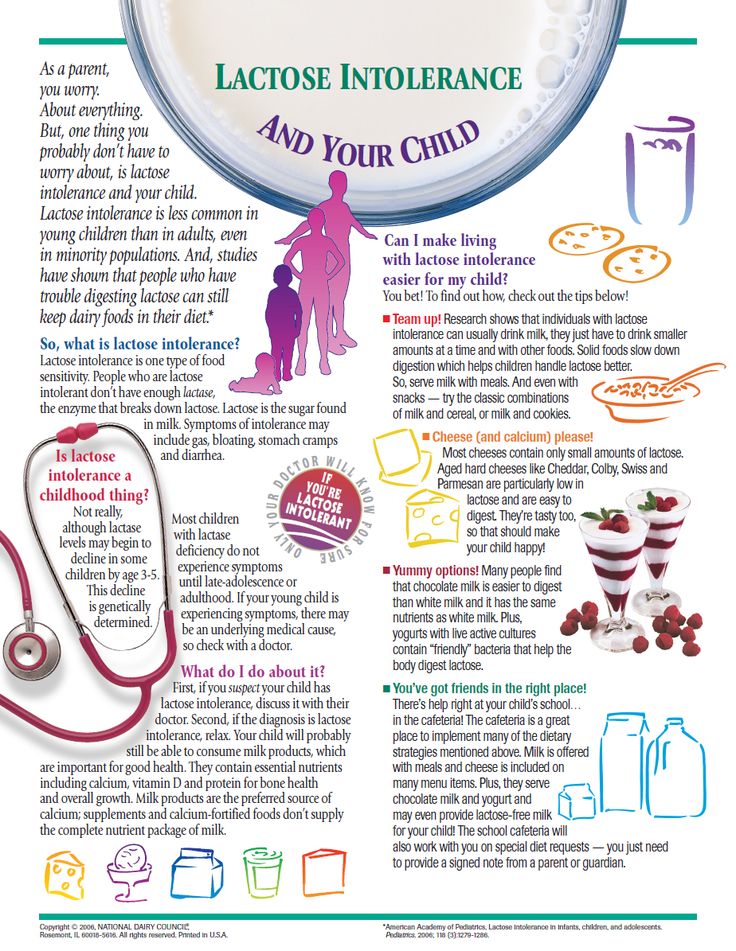 Many children sometimes act up and suffer from colic. But if it seems to you that whims and bloating have become more frequent, this may be a sign that the baby needs a different milk formula. You can trust Similac Sensitive to start effective development of your children's digestive system." nine0003
Many children sometimes act up and suffer from colic. But if it seems to you that whims and bloating have become more frequent, this may be a sign that the baby needs a different milk formula. You can trust Similac Sensitive to start effective development of your children's digestive system." nine0003
In fact, you can't trust the advice of infant formula companies about breastfeeding, as it's in their best interest to have a mother replace her breast milk with artificial formula. Would you go to a tobacco company for advice on how to quit smoking? Probably not.
Many newborn babies spit up and suffer from colic because their digestive system is still immature, it has just begun the transition from intrauterine nutrition (where it received nutrients through the placenta) to self-digestion of milk. nine0003
Starting with a small amount of colostrum, it is easier for a newborn's digestive system to accept more breast milk later on. After the milk has “come”, the next step in the nursing mother is transitional milk (a mixture of colostrum and milk), and a little later mature milk, about 7-10 days after the birth of the baby.
Although breast milk is much easier to digest than formula milk, occasional regurgitation, restless behavior and gas are to be expected in all newborns, whether breastfed or formula fed. Many mothers worry about their babies having frequent watery stools, but this is normal for exclusively breastfed babies. nine0003
In addition to an immature digestive system, regurgitation and gas, and even belching, can also be caused by supplements such as fluoride or iron, or gastrointestinal illnesses (eg, stomach flu).
Mothers of babies with gas go to the doctor with questions about how to avoid bloating or spitting up, and in most cases doctors cannot answer. Doctors simply hate these kinds of questions, because for most of them they cannot give an exact answer: what caused it and how to treat it. Unhappy baby - unhappy parents, especially if they see that they can do nothing to improve his well-being. nine0003
Over time, most children's digestive system matures and they outgrow the symptoms - some sooner, some later, but most by 3-4 months. Of course, when your child is ill or in pain, even a couple of minutes seem like an eternity.
Of course, when your child is ill or in pain, even a couple of minutes seem like an eternity.
What you need to know about breastfeeding and lactose intolerance:
Lactose is a sugar found in all dairy products, including breast milk and formula.
Lactose intolerance is caused by a lack of the enzyme lactase, which breaks down lactose (milk sugar) for easier digestion in the intestines. nine0003
All babies are already born with lactose in their intestines. As they grow and are weaned, the amount of the lactase enzyme decreases. This is why sometimes lactose intolerance can show up before the age of 3-4 years, since around this age weaning is natural.
"Primary lactose intolerance" is the inability to digest the lactose found in all dairy products, including both breast milk and formula. This deviation is very rare and is congenital. It is estimated that only 1 in 85,000 children is born with galactosemia. Children with this genetic disorder can become overweight, dehydrated, and unhealthy from the start. They need to be fed a dairy-free formula in order to develop normally. nine0003
They need to be fed a dairy-free formula in order to develop normally. nine0003
There is another, much more common type of lactose intolerance called Secondary Lactose Intolerance. Gastrointestinal diseases such as stomach flu (more common among formula fed babies) can cause diarrhea that irritates the stomach lining. This inflammation can cause a temporary decrease in lactase production.
This type of temporary lactose intolerance continues until the child's stomach lining recovers. nine0003
No matter what a breastfeeding mother eats or drinks, her breast milk will contain the same amount of lactose.
Most exclusively breastfed infants regulate their milk intake and do not overfeed, but they may become lactose overloaded due to excess milk in the mother. The problem is not the lactose in milk itself - the fact is that the baby eats more milk (and therefore more lactose) than his digestive system can process. This can lead to an imbalance of "front" and "hind" milk.