Breastfeeding foods to make baby poop
Constipation in breastfeeding babies: Treatments and causes
Constipation is uncommon in infancy, particularly in breastfed babies, but it can happen. Breastfed babies tend to have fewer episodes of constipation and diarrhea than formula-fed babies because breast milk is easier than formula to digest.
In older children, constipation is common and accounts for about 3% of visits to pediatric outpatient clinics and up to 25% of visits to pediatric gastroenterologists.
A baby might be constipated if they are passing hard pebble-like stools or have a distended belly. As every baby poops on their own schedule, the frequency of bowel movements is not always an accurate indicator of constipation.
In this article, we examine the possible causes of constipation in breastfed babies. We also look at the symptoms of constipation in babies and the treatments and home remedies.
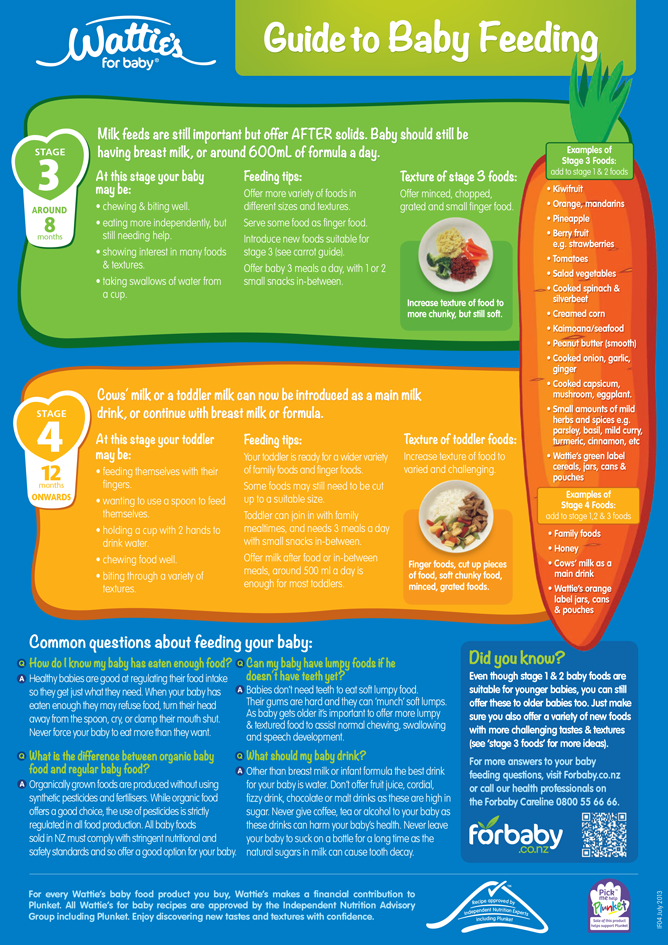
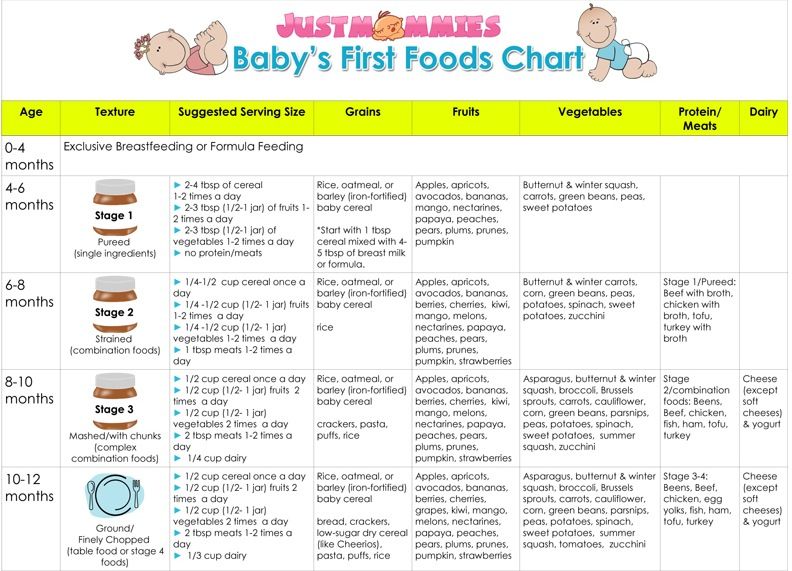
The American Academy of Pediatrics recommend that babies exclusively have breast milk until 6 months after birth. During this time, they advise not giving any additional foods or fluids to the baby unless a doctor recommends it. After the first 6 months, parents or caregivers can then introduce solid foods to the baby’s diet.
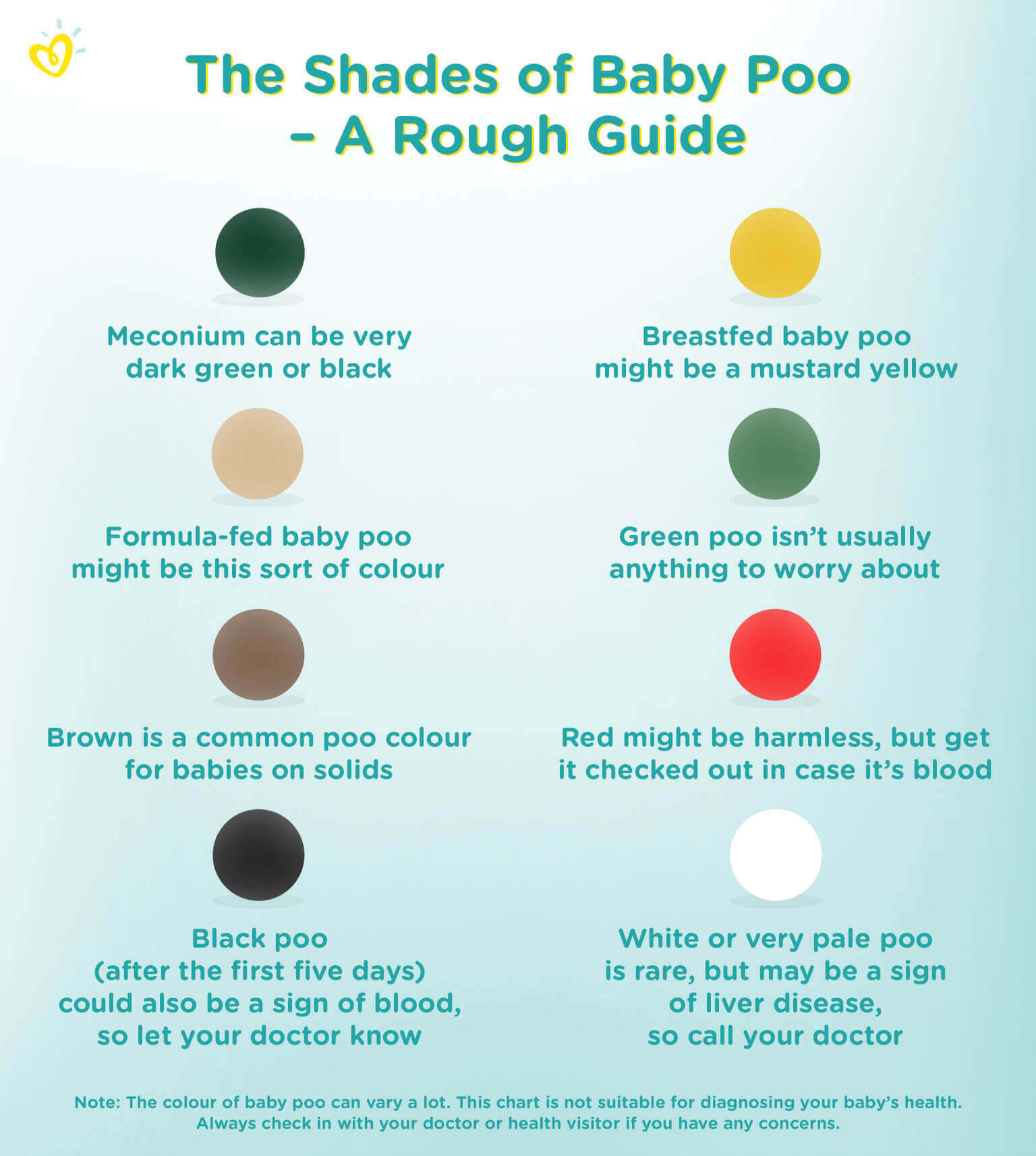
A parent or caregiver may notice changes in the baby’s bowel habits and the color and consistency of their stools if they decide to switch to infant formula or when they begin introducing solid foods.
A 2018 study examined the bowel habits of 83,019 newborn babies in Japan. According to the authors, most instances of constipation coincided with the transition from breastfeeding to infant formula, regardless of whether the woman gave birth vaginally or by cesarean delivery.
A baby may develop harder stools and constipation after starting solid foods. Certain foods, such as rice cereal and dairy milk, may cause constipation in babies younger than 1 year.
Other possible causes of constipation in breastfed babies include:
- Not having enough liquids.
 Liquids help stool pass through the bowels smoothly.
Liquids help stool pass through the bowels smoothly. - Illness. Infections can cause a decrease in a baby’s appetite or lead to vomiting and diarrhea, which may result in dehydration and constipation. Medical conditions that affect the gastrointestinal (GI) tract, such as Hirschsprung disease, can cause constipation and other digestive symptoms.
- Withholding stool. Babies may purposefully avoid passing hard or painful stools —a behavior that doctors refer to as withholding. Babies who have diaper rash may also withhold to avoid pain.
- Stress. Exposure to new environments, traveling, or weather changes may be stressful for a baby. Stress can affect their physical health and may result in a change in stool frequency and possibly constipation.
A woman who is breastfeeding may wonder how her diet affects her breast milk and whether her choice of foods can influence the baby’s digestive health.
According to the Centers for Disease Control and Prevention (CDC), women do not need to avoid specific foods while breastfeeding.
However, babies may appear to avoid feeding after a woman eats a particular food. In this case, the woman may wish to refrain from eating that food for a while and reintroduce it later.
Women may also want to limit or avoid caffeine while breastfeeding because small amounts of caffeine pass from the woman to the baby through breast milk.
Experts suggest that most women who breastfeed can safely ingest 300–500 milligrams of caffeine per day. Excessive amounts of coffee may lower the iron concentrations in breast milk, which may cause mild iron deficiency anemia in some babies.
Although most women do not need to restrict their diets while breastfeeding, they should aim to eat a nutritious and diverse diet.
Although changes in the frequency of a person’s bowel movements may indicate constipation in older children and adults, this is not necessarily the case for babies.
Newborn babies may have multiple bowel movements each day. According to the National Institute of Child Health and Human Development, from 3–6 weeks of age onward, breastfed babies may have only one bowel movement per week because breast milk leaves minimal solid waste to pass through the digestive tract.
Breastfed babies older than 6 weeks can go several days to a week between bowel movements.
Babies often show signs of straining, such as crying or getting red in the face, while having a bowel movement. However, straining does not necessarily mean that a baby has constipation. Babies may take a while to learn how to have bowel movements.
Symptoms of constipation in breastfed babies may include:
- being excessively fussy
- crying for prolonged periods
- refusing to feed
- having a hard, distended belly
- having rectal bleeding
- passing hard or bloody stools
- crying during a bowel movement
- experiencing weight loss or poor weight gain
Normal bowel habits vary from baby to baby. Parents and caregivers should monitor their baby’s bowel habits and take note of any changes. Doing this may help them decide when they need to take the baby to a doctor.
It is possible to treat constipation in breastfed babies at home using various remedies. However, constipation in exclusively breastfed babies is so uncommon that parents and caregivers may wish to speak to a pediatrician before trying home remedies.
However, constipation in exclusively breastfed babies is so uncommon that parents and caregivers may wish to speak to a pediatrician before trying home remedies.
Dietary changes
Dietary changes for a baby who is taking formula or foods other than breast milk may help relieve constipation. Breastfeeding women can also try eliminating foods that have an association with infant constipation, such as dairy, from their diet. However, changes to the woman’s diet may not affect the baby’s digestion.
Babies who eat solids may have difficulty digesting high fiber foods or dairy products if parents or caregivers introduce them too early.
High fiber foods may also help relieve constipation in babies who can tolerate most solid foods. These foods include:
- whole grains, such as oatmeal or barley cereal
- skinless fruits
- broccoli
- peas
- pureed prunes
Liquids help move stools through the digestive tract. Increasing a baby’s fluid intake may also help relieve constipation.
Exercise
Exercise can stimulate a baby’s bowels and help them pass stools. However, babies who cannot walk or crawl will require a parent or caregiver to help them exercise.
Parents and caregivers can help relieve constipation by gently moving the baby’s legs in a bicycling motion with the baby lying on their back.
Putting a baby on its stomach to squirm, reach, and play with toys can also stimulate a bowel movement.
Massage
Parents and caregivers can gently massage a baby’s stomach to help try to relieve constipation.
Massage techniques to consider include:
- using the fingertips to make circular motions on the stomach
- gently bending the baby’s knees and pushing the feet toward the belly
- gently sweeping an open palm from the top of the baby’s ribcage down their stomach
Warm bath
A warm bath may help relax a baby’s abdominal muscles, which might make stools pass through the digestive tract more easily.
Parents and caregivers should speak with a doctor or pediatrician if their baby:
- appears distressed or in pain
- has a hard, distended belly
- passes bloody stools
- has rectal bleeding
- refuses to eat
- has a fever
- vomits
- loses weight or is unable to gain weight
- frequently struggles passing stools
A doctor can diagnose constipation in babies by reviewing their medical history and performing a physical exam. Rarely, a doctor may order additional laboratory tests, such as a stomach X-ray, to diagnose or rule out other conditions.
If home remedies and dietary changes do not relieve a baby’s constipation, a doctor might prescribe a mild laxative or suppository.
Parents and caregivers should never give these treatments to a baby without speaking to a trained healthcare professional first.
Constipation is not a common occurrence in breastfed babies. It usually happens as a result of changing to formula or starting solid foods.
Having infrequent bowel movements is not always an indication that a baby is constipated. Constipated babies are likely to pass hard, pebble-like stools.
Home remedies may help relieve constipation in breastfed babies. If a parent or caregiver is concerned about their baby’s bowel movements and accompanying symptoms, they should take them to see a doctor.
Breastfed Children's Bowel Movements | Happy Baby Organics
Read time: 6 minutes
What should I know about my baby’s stool?Understand what is normal when it comes to a breastfed baby’s bowel movement
How to treat both diarrhea and constipation
Know when you should contact your child’s healthcare provider
When it comes to bowel movements in exclusively breastfed children, there is a wide range of normal. You might think and speak about the color, frequency, and consistency of stool more than you ever thought possible. It’s important to notice what your baby’s ‘normal’ is, so that you can tell when your little one shifts into constipation or diarrhea.
In the first few days of life, your baby may only have 1-2 soiled diapers. The first stool to pass is called meconium, a thick and dark tar-like substance your baby had stored up during pregnancy.1 Within about 3-5 days when your mature milk begins to come in and your baby begins to eat more, stools will become more frequent, typically 4 or more per day, and will look like a seedy yellow or have a slight green tint.2 Normally, breastfed baby’s stools are soft and sometimes fairly runny.3
Most babies tend to poop less as they get older, while some continue to stool after every time they eat. During growth spurts, your little one may go several days without pooping.4 However often your baby poops, they’ll be considered normal and healthy as long as baby’s stools are soft and a normal color.5
Infant diarrheaIt can be easy to mistake the common soft and loose stools breastfed babies pass for diarrhea. Changes in your baby’s stool, like more stools per day than usual, multiple stools per feeding, or very watery stools, can indicate diarrhea.6
Changes in your baby’s stool, like more stools per day than usual, multiple stools per feeding, or very watery stools, can indicate diarrhea.6
Diarrhea can occur due to a virus, parasite, antibiotics, or a reaction to changes in mom’s diet.6 Some believe that diarrhea may occur due to teething or nasal congestion, but research does not support this.7,8
If your infant does have diarrhea, usually it will not last very long and will resolve on its own.3 However, it’s important to track color, frequency, and consistency because one of the consequences of diarrhea may be dehydration. Infants are more susceptible to dehydration, so be on the look-out for symptoms of dehydration should diarrhea last longer than a few days.
According to the National Institutes of Health, signs of dehydration in babies include:
Dry eyes or mouth
Little to no tears when crying
Fewer wet diapers than normal
Lethargy (less active than normal)
Sunken eyes and fontanelle (soft spot on the top of baby’s head)5
It is important to continue nursing frequently if your baby is experiencing diarrhea to help keep them hydrated.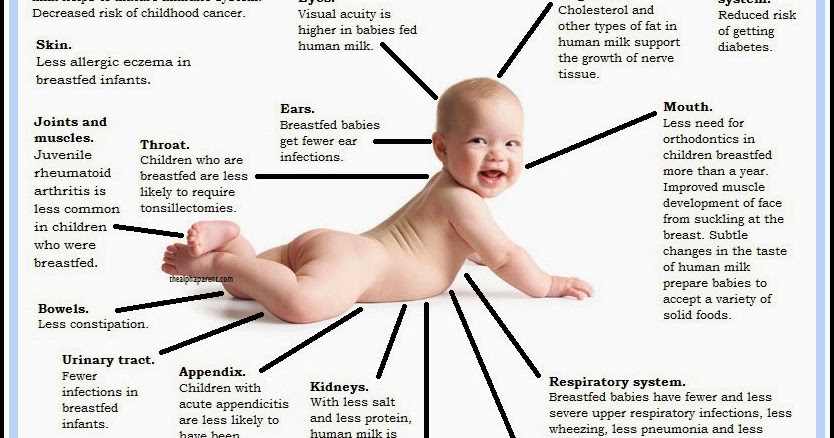 If your infant is under 3 months and has diarrhea; or your child (at any age) has diarrhea along with blood, mucus, pus, or continuous vomiting, contact baby’s pediatrician.
If your infant is under 3 months and has diarrhea; or your child (at any age) has diarrhea along with blood, mucus, pus, or continuous vomiting, contact baby’s pediatrician.
Read more: Diarrhea in Older Babies and Toddlers
Infant constipationConstipation is extremely rare in healthy exclusively breastfed infants. When passing stool, it is completely normal for your baby’s face to turn red, grunt, or make other noises.5 Your baby’s abdominal muscles are still weak so they must work harder to have a bowel movement.10 As they become older and their muscles get stronger, they’ll be able to pass stool much easier! These noises are common and do not necessarily mean your baby is constipated.
Causes of constipation in infantsThe introduction of solid foods is one of the most common times for children to become constipated because the digestive system needs time to adapt.5 Also note that a change in stool, such as it becoming firmer and less frequent, is normal when introducing solids.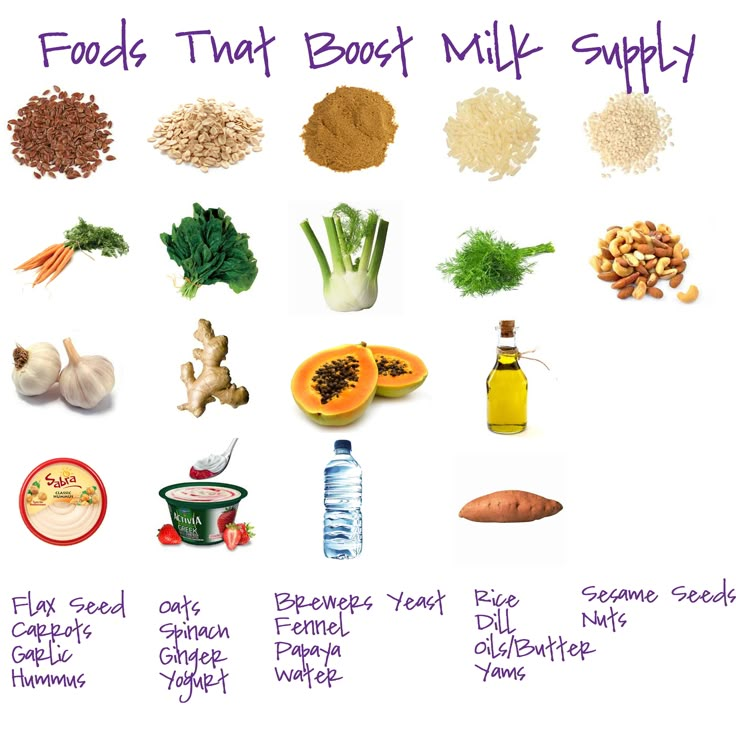 11 Adding in some formula may also cause constipation.5 And occasionally, an iron supplement with higher amounts of iron may cause constipation in an infant.10
11 Adding in some formula may also cause constipation.5 And occasionally, an iron supplement with higher amounts of iron may cause constipation in an infant.10
Your baby may have constipation if his bowel movements are small, hard, and dry. The consistency of the stool is a better indicator of constipation than the frequency.
Other signs of constipation include:
Fussiness
Spitting up more than normal
Belly pain and bloating
Having many less stools than your baby’s normal amount
Straining for more than 10 minutes without passing stool 5,9
If your baby’s constipation is accompanied by vomiting, blood in stool, a swollen abdomen or weight loss, contact the pediatrician.
For more information on constipation in older children or in formula fed-babies, read: How Can I Relieve Constipation for my Baby and Toddler?.
How can I help baby with constipation or diarrhea?Keep your baby hydratedContinue breastfeeding, as nursing can help keep your little one hydrated.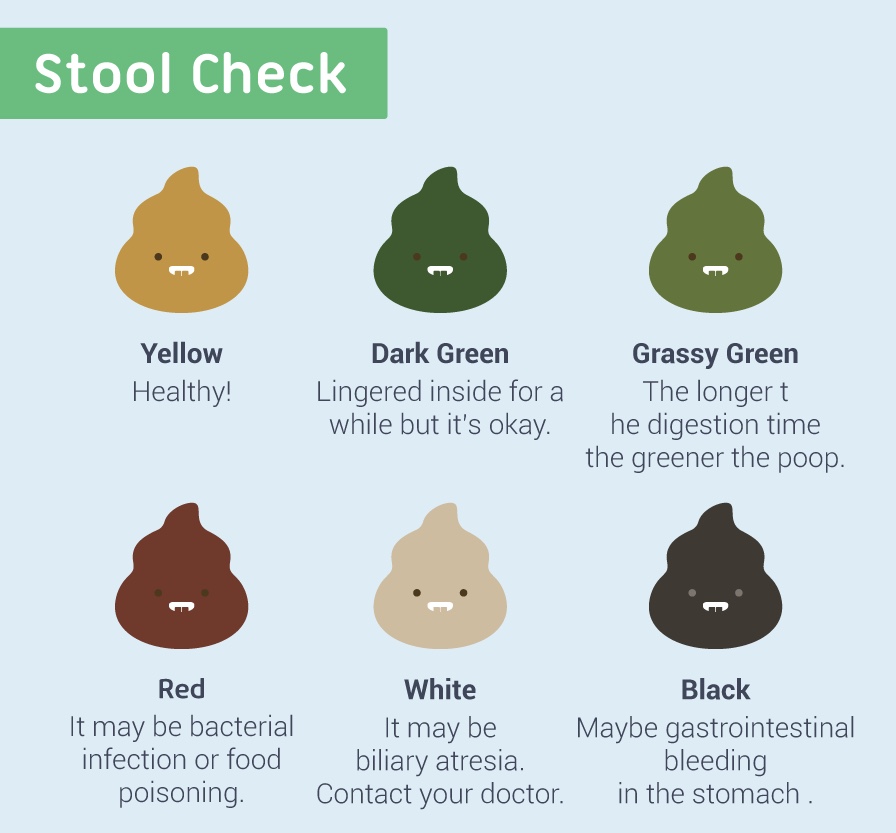 If your baby is older and has started solids, you can also offer additional fluids such as water.
If your baby is older and has started solids, you can also offer additional fluids such as water.
*If your baby is between 6 and 12 months, the only additional fluid that is recommended is water, and only a few extra ounces per day is needed.12
Being adequately hydrated can also help improve constipation as well.
If you’re still noticing signs of dehydration or constipation even with continued nursing, contact your child’s pediatrician.
Read more: Dehydration in Kids: How to Keep your Baby or Tot Hydrated
Be mindful of your own diet while breastfeedingOccasionally babies will react to something in their mother’s breastmilk, and this may sometimes cause diarrhea or constipation.6 Certain foods in mom’s diet can also affect the stool color, but this is normal!
If you’re concerned that your baby may be reacting to something in your diet, reach out to the Happy Baby Experts. Chat Now!
Read more: Is my baby reacting to something in my milk?
Inform baby’s healthcare providerIf diarrhea occurs and your baby is under 3 months old, or there is also blood, mucus, pus or continuous vomiting; or if the diarrhea will not go away, contact your child’s pediatrician right away.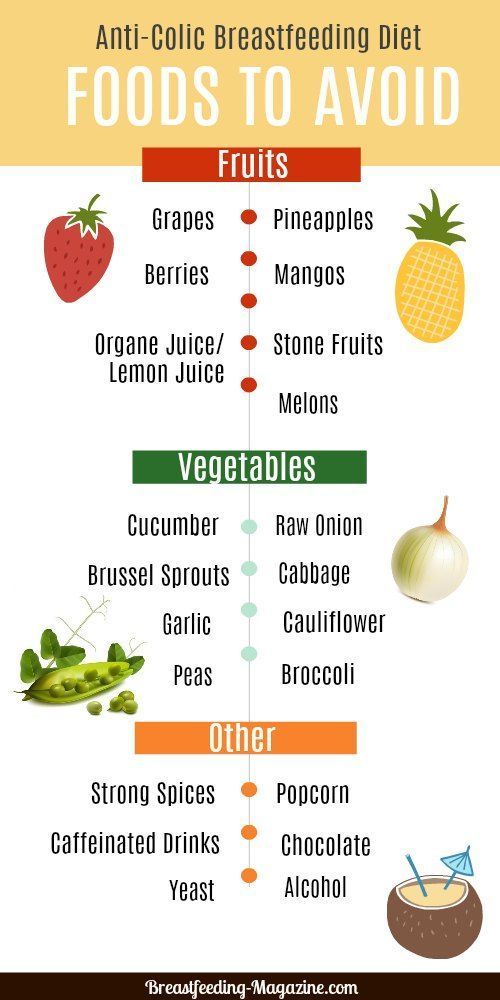
If your child is experiencing persistent constipation for 2 weeks or constipation is accompanied by fever, vomiting, blood in stool, swollen abdomen or weight loss, contact your little one’s pediatrician.
A bit of JuiceIf constipation does not improve, a small amount of 100% prune, apple, or pear juice may be added to breastmilk in a bottle as long as your baby is older than 1 month.9 The sugars in fruit juices can draw water into the intestines to help baby pass the stool.
The general recommendation is giving 1 oz per day for every month of life up to 4 months. For example, a 3-month-old would be allowed to have 3 oz per day. This technique should only be used cautiously; always contact baby’s pediatrician before trying it.
Note that juice is not recommended for infants younger than 1 year old at any other time.
Massage your babyThe “I love you” massage for babies and toddlers can be helpful in reducing constipation, abdominal pain, bloating, and gas.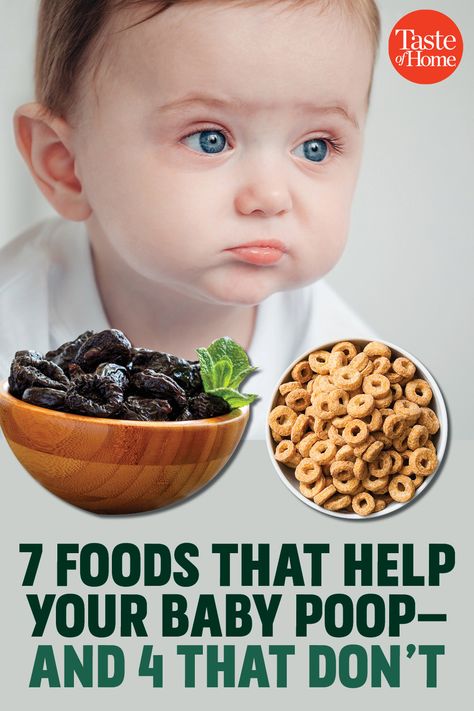
Read: Baby massage: Benefits and techniques for all the details.
If eating solids, increase the amount of fiber in your child’s dietIf your little one has started solids, offer higher fiber foods to your baby twice per day, such as: fruits, vegetables, beans and whole grains.5, 9 Make sure these foods are in the consistency your little one can handle, and be sure to offer extra fluids anytime you increase fiber in your baby’s diet.
Read more: Why does Fiber Matter for Babies, Tots, and Mama
Avoid adult treatments for constipationTreatment for constipation in babies is different than for adults. Be sure to avoid using mineral oil, stimulant laxatives, and enemas to treat constipation in infants unless a doctor instructs you to do so.
Let’s Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.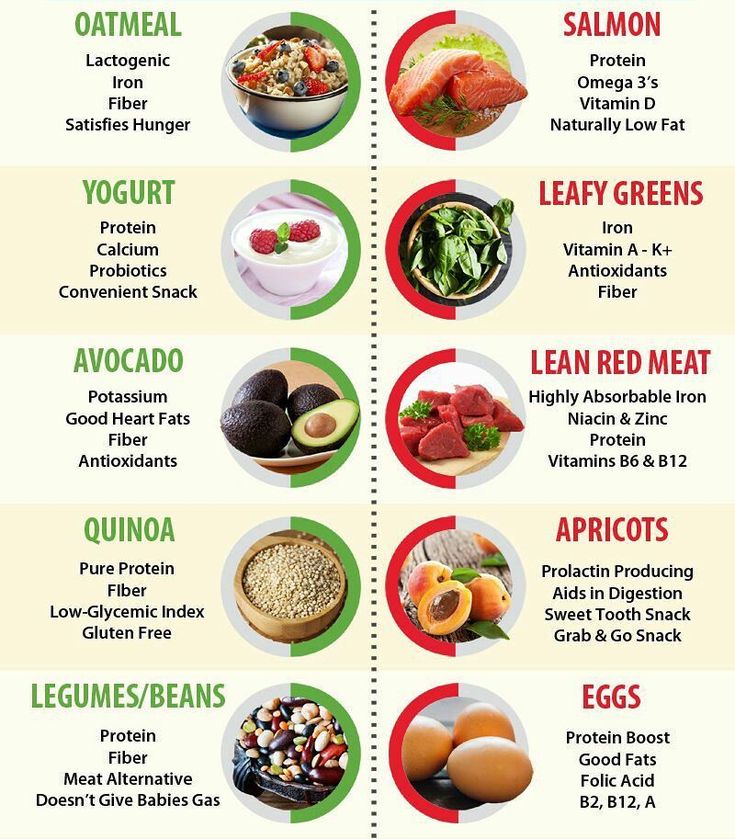
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday through Friday, from 8am–6pm (ET). Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:Should I Breastfeed On Demand or on a Schedule?
Understanding your Baby’s Hunger and Fullness Cues: Responsive Feeding
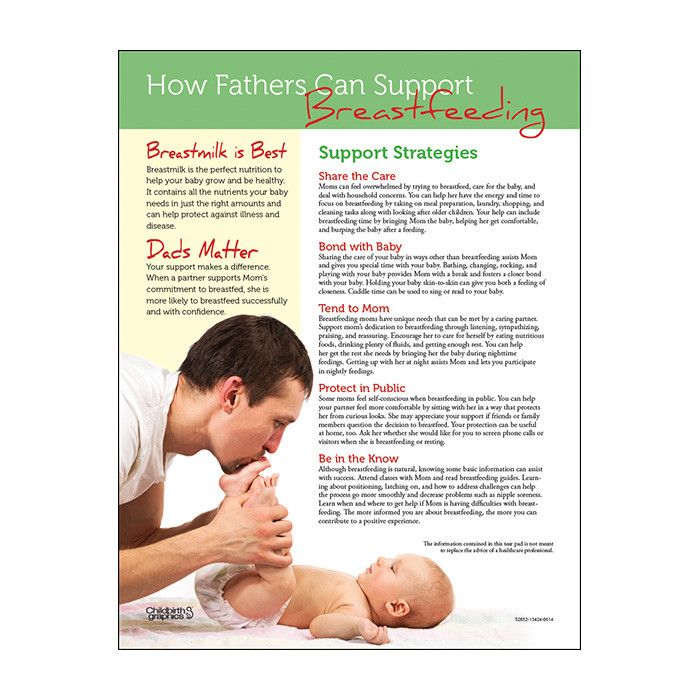
Breastfeeding: How to Support a Good Milk Supply
Meal Plan: Getting the Right Nutrition While Breastfeeding
Mother's nutrition in case of constipation in a child
Co-author, editor and medical expert - Volosov Dmitry Dmitrievich.
Views: 283 340
Last update date: 24.11.2022 G.
Average Reading time: 8 minutes
Content:
- Classification of constipation in newborn and pectorals
- Causes of constipation in infants
- Importance of maternal nutrition in constipation in the infant
- Recommended products
- Products not recommended
- Maternal and child feeding rules to avoid constipation
- Feeding mother's menu for several days
Breast milk allows the baby to receive all the nutrients necessary for its growth and full development, and saves the mother from worrying about the correct selection of milk formulas, the temperature of the prepared baby food, etc.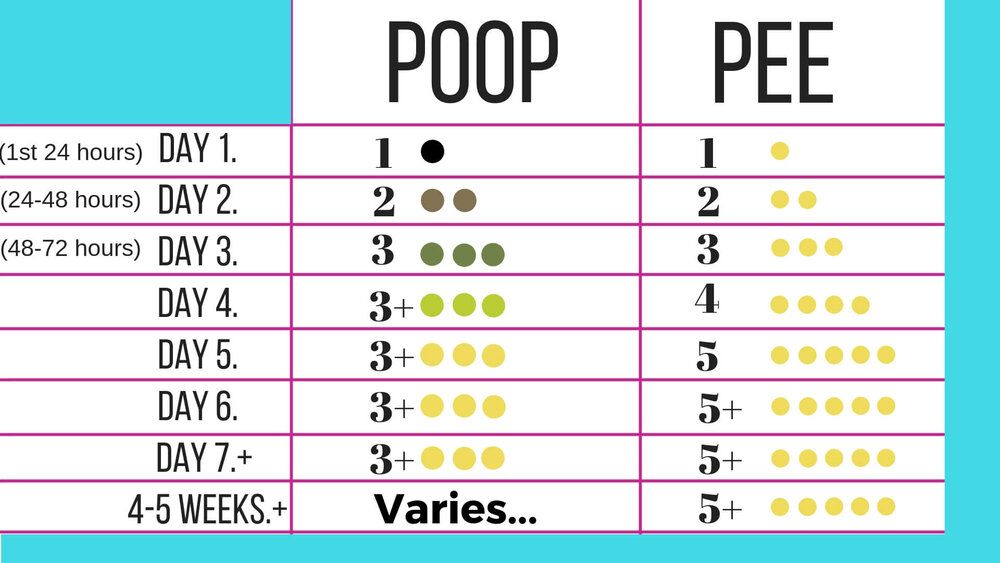 But there is a nuance in breastfeeding: the quality of the baby’s digestion directly depends on maternal diet. Therefore, quite often women turn to the doctor with the question of what to eat for the mother if the child has constipation, and how to normalize the stool of the newborn by correcting the diet of the mother.
But there is a nuance in breastfeeding: the quality of the baby’s digestion directly depends on maternal diet. Therefore, quite often women turn to the doctor with the question of what to eat for the mother if the child has constipation, and how to normalize the stool of the newborn by correcting the diet of the mother.
Classification of constipation in newborns and infants
Delayed stool in children can be acute or chronic. In the first case, it occurs once or is observed periodically, but with large intervals between episodes. In a chronic condition, this problem is relevant for a long period: the symptoms of constipation are observed constantly for several weeks or months.
In addition to classification by flow, constipation is divided into atonic and spastic. In the first case, the peristalsis is sluggish and weak, and the excreted feces are dense and voluminous. With spastic constipation, excessive peristalsis is observed in one of the sections of the intestine, which leads to a temporary "blockage" of feces and its difficult movement. Feces with spastic constipation are heterogeneous, divided into small, dry and hard lumps.
Feces with spastic constipation are heterogeneous, divided into small, dry and hard lumps.
Back to content
Causes of constipation in infants
The most common causes of constipation in infants are:
- Improper nutrition of the mother. Maternal nutrition for constipation in a breastfed infant should be considered first. It is the violations of the diet in the mother that often lead to a delay in the stool in the child. The diet of a nursing mother with constipation in a baby often includes foods that have a fixing property.
- Features of the nervous system of the newborn. A kind of immaturity of the mechanisms responsible for innervation (that is, the supply of organs and tissues with nerves, ensuring their connection with the central nervous system) of the intestine can cause constipation due to an insufficient response of receptors to irritation by fecal masses.
- Maternal medication. A number of drugs necessary for the treatment of various diseases and conditions in a nursing mother give side effects in the form of a decrease in intestinal tone, slowing down peristalsis, etc.
 Therefore, when prescribing drug therapy, a woman should inform the doctor that she is breastfeeding.
Therefore, when prescribing drug therapy, a woman should inform the doctor that she is breastfeeding.
Back to Contents
Importance of Maternal Nutrition in Constipated Infants
Nursing Nutrition in Constipated Infants is much more important than it might seem at first glance. So, the lack of liquid in the diet leads to an increase in the fat content of milk, which can cause a delay in stool in a child. Consumption of a large amount of sweets and baked goods can change the chemical composition of milk. It also negatively affects the functions of the intestines in the baby. And the lack of plant products in the menu - vegetables and fruits, vegetable oils, etc. - reduces the amount of vitamins and minerals in breast milk, which can provoke not only constipation, but also other medical problems.
Back to content
Recommended foods
What to eat for constipated nursing mothers, you can choose from the list of recommended foods:
- Cereals .
 Wheat, oatmeal, corn, buckwheat porridge, whole grain bread, wholemeal or bran bread.
Wheat, oatmeal, corn, buckwheat porridge, whole grain bread, wholemeal or bran bread. - Meat products. All varieties of lean meat boiled, baked or stewed, soups in weak broths.
- Vegetables . Table beets, pumpkin, zucchini, cucumbers, cabbage, potatoes, tomatoes in the form of salads from fresh or boiled vegetables, side dishes, independent dishes (soups, stews, casseroles, etc.).
- Dried fruits . Dried apricots and prunes are the best laxative foods, but they should be limited to 3-5 per day. per day, as if consumed in excess, they can cause diarrhea.
Back to Contents
Unrecommended Foods
A diet rich in laxatives and fiber is not the only requirement for a constipated infant diet. It is equally important to exclude from the maternal menu products that produce a fixing effect. These include rice, semolina, pasta, muffins, sweets, pears, pomegranates, strong brewed tea, coffee, cocoa, chocolate.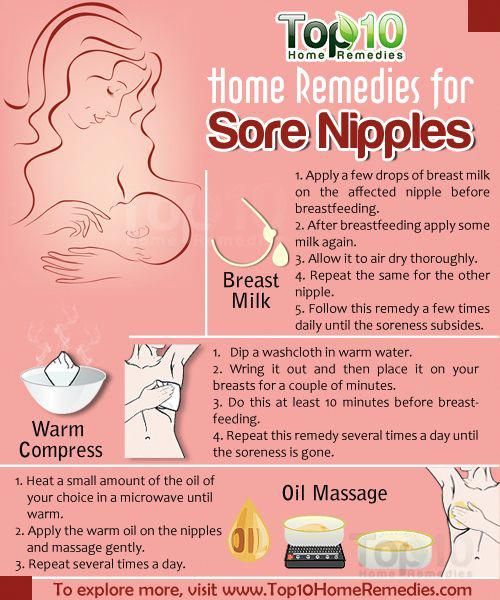
If constipation in a baby is accompanied by intestinal colic and increased gas formation, all legumes should also be excluded from the diet, and vegetables and fruits from the recommended list should be consumed only in processed form (soups, mashed potatoes, stews, etc.). Laxative products while breastfeeding should also be limited if the baby has unstable stools - alternating constipation and diarrhea.
Back to Contents
Maternal and Infant Feeding Rules to Avoid Constipation
Maternal nutrition in constipated infants is of great importance. But the diet and food hygiene mean no less: they help eliminate a number of factors that have an undesirable effect on the mother's body and, as a result, on the quality of breast milk.
Observe meal and feeding times . A clear regimen will make mom's digestion more efficient and, accordingly, improve the absorption of nutrients. And meals in small portions 4-5 times a day will ensure a uniform supply of nutrients to the milk. Feeding the baby should be based on the same principle. Teach him to eat at strictly allotted hours according to his age - a "disciplined" digestive system is much less prone to constipation.
Feeding the baby should be based on the same principle. Teach him to eat at strictly allotted hours according to his age - a "disciplined" digestive system is much less prone to constipation.
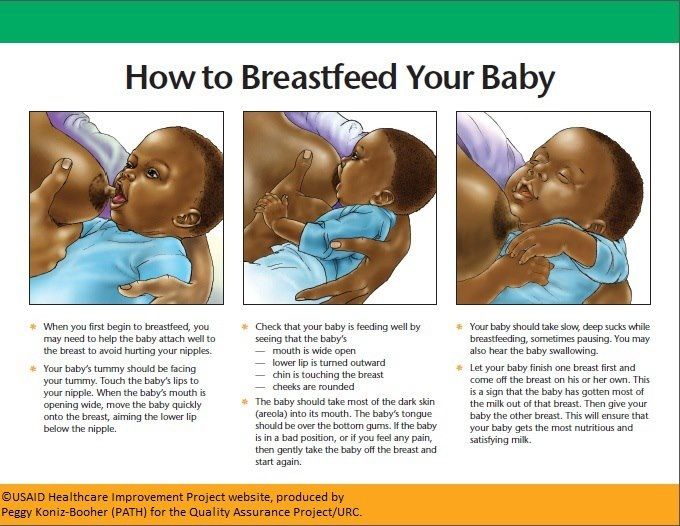
Maintain good feeding hygiene . In addition to traditional hygienic procedures before feeding (washing hands, wiping the nipple and areola), it is necessary to ensure that the child grasps the nipple correctly. With sucking movements, he should not swallow air - this can provoke disruption of the digestive tract. To ensure better hygiene and to make the mother feel more confident during breastfeeding, we recommend using JOHNSON’S ® 9 Breast Pads0134 Baby.
MICROLAX ® prepared a visual material especially for mothers of babies prone to constipation:
Up to content
Menu for a nursing mother for several days
If the baby has constipation, what should the mother eat and in what quantities? Here is the approximate composition of the diet for two days:
| 1st breakfast | Monday: 100 g of muesli filled with 100 g of yogurt or low-fat kefir, and weak tea with crispbread. Tuesday: 100 g porridge (oatmeal, buckwheat, barley), 150 g vegetable salad, dried fruit compote. |
| 2nd breakfast | Monday: apple, whole grain bread with a slice of cheese. Tuesday: Bran bread sandwich with honey, weak green tea. |
| Lunch | Monday: Serving of vegetable soup, 150 g of mashed potatoes with boiled beetroot salad and 100 g of boiled or baked fish, compote. Tuesday: cup of weak beef broth with whole grain toast, 150 g vegetable casserole, weak tea with 1 tsp. honey. |
| Snack | Monday: 2-3 pcs. dried apricots, 200 ml of kefir. Tuesday: 150 g finely grated fresh apple and carrot salad dressed with 1 tbsp. l. low fat sour cream. |
| Dinner | Monday: 200 g syrniki, prunes decoction. Tuesday: 150 g chicken breast, 100 g fresh or boiled vegetable salad, kefir - 200 ml. |
Further, your diet should be built similarly to this example, taking into account the recommended and undesirable products.
Back to Contents
The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
What to eat while breastfeeding | Breastfeeding Diet
You know that breast milk is the best food for your baby. What about your own nutrition while breastfeeding? We asked the nutritionist a few questions about the nutrition of a nursing mother.
Share this information
Priya Tew, UK-based registered dietitian :
Priya is a nutritionist, M.D., multi-award winning member of the British Dietetic Association and the Health Professions Council. She has three children, and she breastfed each of them for up to 18 months.
She has three children, and she breastfed each of them for up to 18 months.
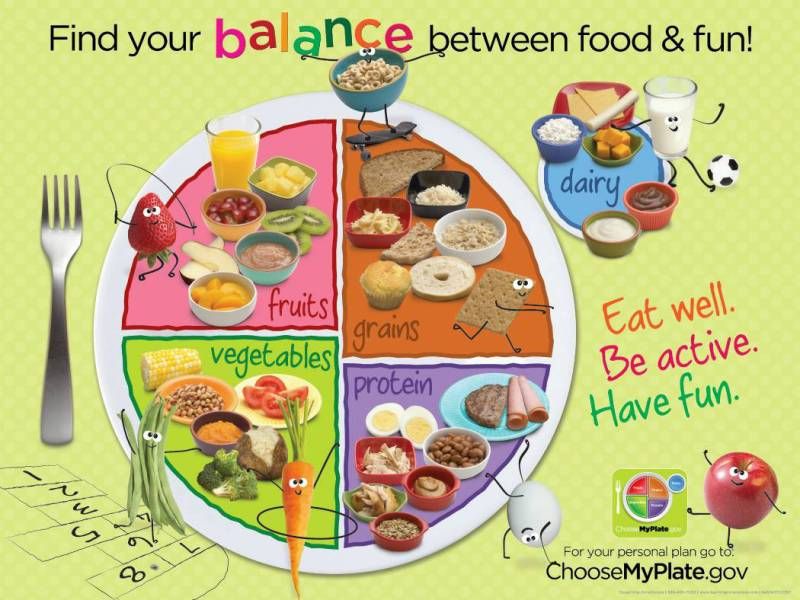
During breastfeeding, there is no need to follow a special diet, the main thing is that your diet is balanced. It should include plenty of fruits and vegetables, whole grains such as oats, brown rice, various cereals, and breads labeled "whole grain", "wholemeal" or "wholemeal". These foods, along with potatoes, pasta, and couscous, are high in starch, an important source of energy.
In addition, you need lean proteins found in chicken, eggs, legumes, lentils, fish, and lean beef, as well as healthy fats found in olive oil, nuts, seeds, avocados, and fatty fish such as salmon and mackerel. Oily fish is very good for your health and development of your baby, but you should not eat more than two servings per week (about 140 g), as it may contain harmful impurities. 1
Should I take vitamins while breastfeeding?
The most important is vitamin D. It is essential for healthy bones, you and your baby.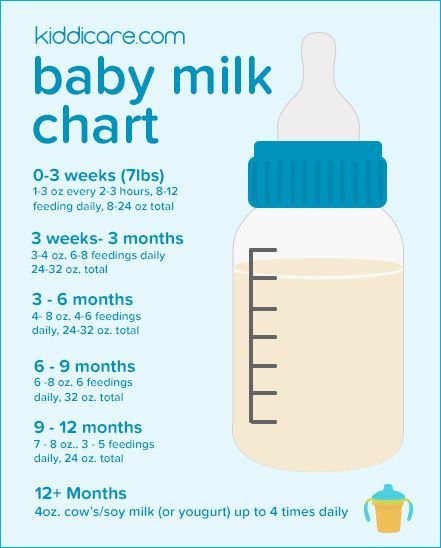 We get most of this vitamin from the sun. If you live in a region with insufficient solar activity, especially in winter, your body may lack it. In this case, the doctor may advise taking vitamin D supplements. 2
We get most of this vitamin from the sun. If you live in a region with insufficient solar activity, especially in winter, your body may lack it. In this case, the doctor may advise taking vitamin D supplements. 2
You also need to get enough calcium, as it is excreted from the body during breastfeeding. 3 Try to eat four servings of foods rich in this mineral a day. These can be dairy products such as milk, yogurt, and cheese, or non-dairy products such as nuts, tofu, sesame seeds, and leafy vegetables. One serving may consist of, for example, half a cup of green vegetables or a small piece of cheese (50 g).
What foods should I avoid while breastfeeding?
The good news is that you can eat almost anything while breastfeeding. Only the consumption of oily fish should be limited. In small quantities, even caffeine is acceptable - more on this below.
If you are not allergic to peanuts, there is no reason to deny yourself products that contain peanuts.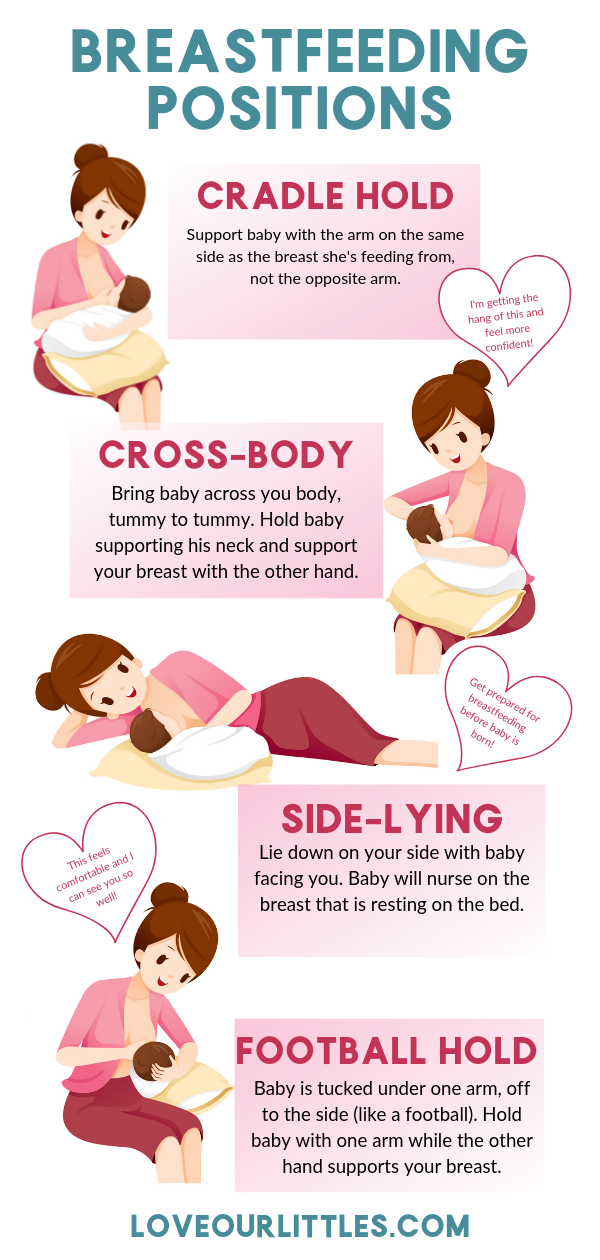 Recent studies show that if you eat peanuts while breastfeeding and gradually introduce them into your baby's diet during the first year, your baby will be less likely to become allergic to them in the future. 4
Recent studies show that if you eat peanuts while breastfeeding and gradually introduce them into your baby's diet during the first year, your baby will be less likely to become allergic to them in the future. 4
Are extra calories needed while breastfeeding?
Breastfeeding mothers need about 500 more calories a day. 5 But every mother is unique and your energy needs will change throughout your breastfeeding period. The number of calories you need depends on your baby's age, appetite, height, and weight, as well as your body mass index (BMI), your activity, and factors such as whether you are exclusively breastfeeding or not, and whether you are breastfeeding twins or multiple babies.
Can I go on a diet while breastfeeding?
Trying to lose weight while breastfeeding is not a good idea because you need to get enough nutrients for you and your baby. The fat accumulated during pregnancy is used to produce milk, so breastfeeding in itself will help you shed those extra pounds.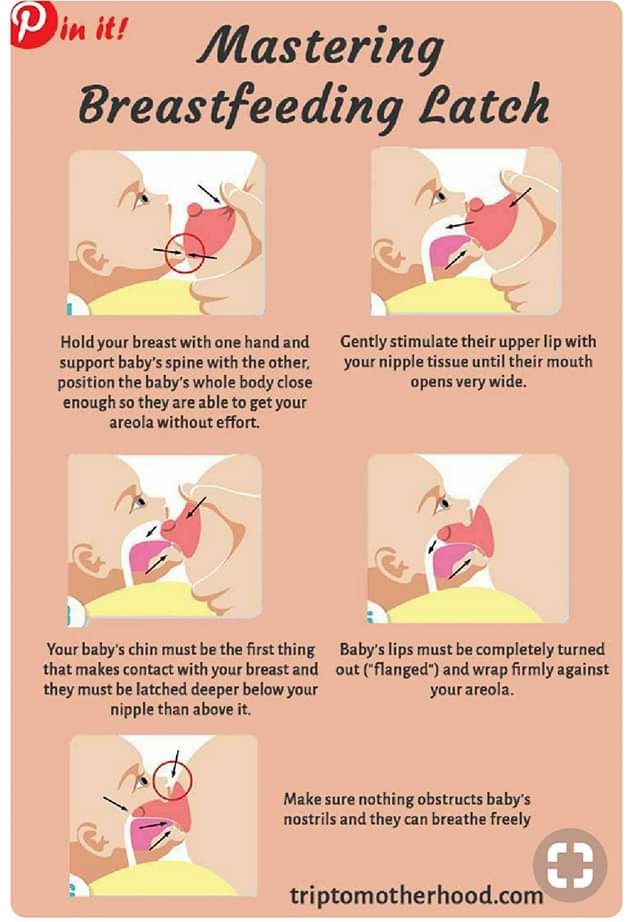
If your weight changes by more than 1 kg per week, check if you are eating a healthy and balanced diet and adjust if necessary. You can also ask your doctor for advice.
How do you find time to prepare healthy meals?
Having devoted yourself to feeding a child, you can forget about your own nutrition. However, it is important to ensure that your diet does not consist only of sweets and cookies. Of course, sweet snacks are easy and quick, but they do not bring any benefit to your body.
Opt for quick yet nutritious meals like scrambled eggs with spinach or fried chicken with brown rice. Oatmeal is great for breakfast, as it provides a slow release of energy from grains and soluble dietary fiber, which is what you need to restore strength in the morning after a night of breastfeeding.
Store pre-cut fruits and vegetables in the refrigerator for light snacks, or carry unsalted nuts in your bag. It's much easier than peeling tangerines with one hand while holding a baby with the other.
Should I drink more water while breastfeeding?
Breastfeeding can make you thirsty, so it's important to drink enough water. A person needs six to eight glasses of fluid a day, and even more if breastfeeding. 6 Make it a habit to drink a glass of water, milk or fruit juice without sugar every time you feed your baby.
I love coffee. Do I need to quit caffeine?
Coffee, like everything you eat or drink, passes into your breast milk, so it is advisable to limit your intake while breastfeeding. Legal coffee limits vary by country, but the average recommendation is not to exceed 200-300 mg of caffeine per day (300 mg is equivalent to two cups of filtered coffee or four cups of tea). Talk to your doctor about the acceptable amount of coffee consumption for you. Also, don't forget that caffeine is found in cola and energy drinks, and a small bar of dark chocolate can contain up to 50 mg. 7
If I eat a varied diet, will my baby be less picky about food?
Breast milk has the flavor of everything you eat.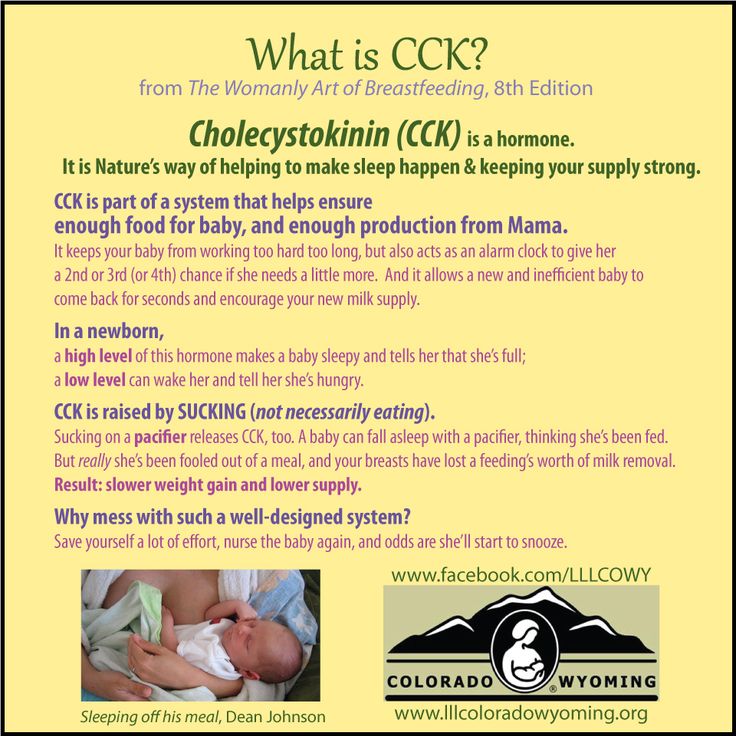 8 Therefore, if you eat a varied diet during breastfeeding, giving your baby a chance to taste different flavors, he may like them in the future.
8 Therefore, if you eat a varied diet during breastfeeding, giving your baby a chance to taste different flavors, he may like them in the future.
If you like spicy and spicy foods, there is no reason to refuse them while breastfeeding. When my first child was born, I ate a lot of spicy food. When my daughter was two years old, we went to Sri Lanka, coincidence or not, but she ate absolutely everything.
Can something in my diet be unsuitable for a child?
At an early age, babies often suffer from colic or are picky eaters, so mothers naturally wonder if their diet is causing this. Probably not. Studies show that the proportion of children who are allergic to any component of breast milk is only slightly more than 1%. 9 Cow's milk, eggs, corn, and soy proteins in moms' diets are much more likely to cause allergic reactions than spicy foods, hot sauces, or cruciferous vegetables, which moms usually worry about.
If your baby is allergic to substances in your milk, it can cause profuse vomiting, rash, bloody stools, or prolonged constipation. If your baby has an intolerance to any food, you will notice symptoms such as moodiness and crying after feeding, burping, diarrhea, or the baby will press his knees to his chest. Contact your doctor if something is bothering you. He may suggest eliminating certain foods for a couple of weeks, and then see if the child's behavior changes after eating them again.
If your baby has an intolerance to any food, you will notice symptoms such as moodiness and crying after feeding, burping, diarrhea, or the baby will press his knees to his chest. Contact your doctor if something is bothering you. He may suggest eliminating certain foods for a couple of weeks, and then see if the child's behavior changes after eating them again.
You can also keep a food diary: write down everything you eat and drink, as well as your child's symptoms, and you may notice some patterns. However, before cutting out any foods, such as dairy, always check with your doctor, as it's important to know that you're getting the nutrients you need from other sources. Depending on where you live, you will be referred to a nutritionist or other specialist.
Does a vegetarian diet affect breast milk?
If you are getting enough calories and all the nutrients your body needs (carbohydrates, proteins, fats, vitamins and minerals), then you have nothing to worry about. A vegetarian or vegan diet requires plenty of vitamin B12, vitamin D, calcium, and omega-3 fatty acids while breastfeeding, so opt for foods and supplements that provide you with these essential nutrients.
A vegetarian or vegan diet requires plenty of vitamin B12, vitamin D, calcium, and omega-3 fatty acids while breastfeeding, so opt for foods and supplements that provide you with these essential nutrients.
If you are on a vegetarian, vegan, macrobiotic, or other special diet, you may need additional medical advice to make sure you are getting all the nutrients your baby needs.
Literature
1 National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. Should pregnant and breastfeeding women avoid some types of fish?; 2015 Jul 06 [cited 2018 Apr 12]; Available from: https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.aspx - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. "Should a pregnant and lactating woman refrain from eating certain types of fish?"; July 6, 2015 [cited April 12, 2018]; See article on site https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.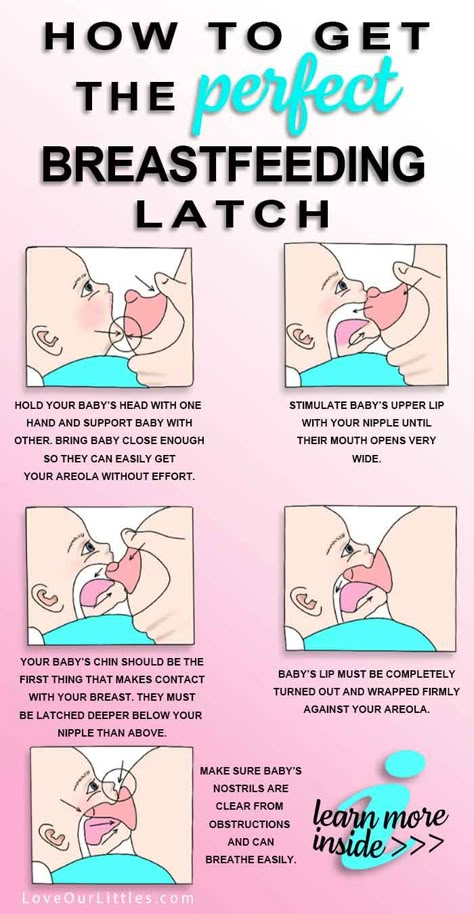 aspx
aspx
2 Oberhelman SS et al. Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1378–1387. - Oberhelman S.S. et al., Introduction of Vitamin D to the Diet of Nursing Mothers to Increase Vitamin D in children: a randomized controlled trial. Mayo Clean Proc. 2013;88(12):1378–1387. : effects on the mother and the fetus. Am J Obstet Gynecol. 2006;194(4):937-945. - Thomas M., Weisman S. M., "Calcium supplementation during pregnancy and lactation: effects on the mother and on the fetus". Am J Obstet Ginekol (American Journal of Obstetrics and Gynecology). 2006;194(4):937-945.
4 Pitt and al . Reduced risk of peanut sensitization following exposure through breast-feeding and early peanut introduction. J Allergy Clinic Immunol. 2018;141(2):620-625. e 1 - Pitt et al., "Reducing the Risk of Peanut Allergy by Introducing Peanuts into the Breastfeeding Mother's Diet and as a Baby's First Food." G Allergy Clean Immunol. 2018;141(2):620-625.e1
J Allergy Clinic Immunol. 2018;141(2):620-625. e 1 - Pitt et al., "Reducing the Risk of Peanut Allergy by Introducing Peanuts into the Breastfeeding Mother's Diet and as a Baby's First Food." G Allergy Clean Immunol. 2018;141(2):620-625.e1
5 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr. 1997 Jul;17(1):19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Annu Rev Nutr . 1997 Jul;17(1):19-36.
6 Food Standards Agency (FSA) [Internet]. London, UK: Crown copyright 2002. Eating for breastfeeding; [cited 2018 Apr 13]; Available from: https://www.food.gov.uk - Food Standards Agency (FSA) [Internet]. London, UK: State Copyright 2002. "Eat to feed" [cited April 13, 2018]. See article on https://www.food.gov.uk
7 National Health Service (NHS) [Internet].