Can feeding a baby lying down cause ear infections
Will lying down to nurse cause ear infections? • KellyMom.com
By Kelly Bonyata, BS, IBCLC
You might hear that breastfeeding your baby in a lying down position will cause ear infections. Research indicates that this is not true. No matter what positioning you use, breastfeeding actually works to decrease the incidence of ear infections.
This myth is one of many that has come from a mistaken application of bottle-feeding information to breastfeeding. There is good evidence that if baby is given a bottle of formula while lying flat, the formula can get into the Eustachian tubes and middle ear and cause an infection. However, there are two problems with applying this fact to breastfeeding: (1) breastmilk and formula are not the same — breastmilk inhibits the formation of bacteria, while formula encourages bacteria; and (2) breastfeeding and bottle feeding are not the same — milk does not pool in the mouth when baby is nursing, as as it does when baby drinks from a bottle.
Now infants can get
all their vitamin D
from their mothers’ milk;
no drops needed with
our sponsor's
TheraNatal Lactation Complete
by THERALOGIX. Use PRC code “KELLY” for a special discount!
Also, keep in mind that with most nursing positions, baby is lying down while nursing anyway – whether mom is lying down or not!
So don’t be afraid to lie down to nurse your baby. Go ahead and get your rest… while you nurse your baby.
General information on ear infection prevention and treatment
Detecting an Ear Infection by Alan Greene MD FAAP
Ear infections from AskDrSears.com
Cause and Treatment of Ear Infections by Dr. Jay Gordon
Alternative Treatment for Ear Infections by Dr. Jay Gordon
Ear infection articles from Mothering.com
Ear infections and the Breastfed Baby by Paula Yount
Ear Infection Information from the American Academy of Pediatrics
Bottle Feeding And Ear Infections: A Formula For Disaster? by Craig Brown, MD
Research on breastfeeding and ear infections
The Diagnosis and Management of Acute Otitis Media from the American Academy of Pediatrics
Sabirov A, Casey JR, Murphy TF, Pichichero ME. Breast-feeding is associated with a reduced frequency of acute otitis media and high serum antibody levels against NTHi and outer membrane protein vaccine antigen candidate P6. Pediatr Res. 2009 Nov;66(5):565-70.
Breast-feeding is associated with a reduced frequency of acute otitis media and high serum antibody levels against NTHi and outer membrane protein vaccine antigen candidate P6. Pediatr Res. 2009 Nov;66(5):565-70.
Vogazianos E, Vogazianos P, Fiala J, Janecek D, Slap�k I. The effect of breastfeeding and its duration on acute otitis media in children in Brno, Czech Republic. Cent Eur J Public Health. 2007 Dec;15(4):143-6.
Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007 Apr;(153):1-186.
Chantry CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics. 2006 Feb;117(2):425-32.
Scariati PD, Grummer-Strawn LM, Fein SB. A longitudinal analysis of infant morbidity and the extent of breastfeeding in the United States. Pediatrics 1997;99:e5
Dewey KG, Heinig J, Nommsen-Rivers LA. Differences in morbidity between breastfed and formula fed infants. J Pediatr 1995;126:696-702 (risk also increased in FF infant for diarrhea)
Differences in morbidity between breastfed and formula fed infants. J Pediatr 1995;126:696-702 (risk also increased in FF infant for diarrhea)
Sassen ML, Brand R, Grote JJ. Breastfeeding and acute otitis media. Am J Otolaryn 1994;15:351-7
Paradise JL, Elster BA, Tan L. Evidence in infants with cleft palate that breast milk protects against otitis media. Pediatrics 1994;94:853-60
Aniansson G, Alm B, Andersson B, Håkansson A, Larsson P, Nylén O, et al. A prospective cohort study on breastfeeding and otitis media in Swedish infants. Pediatr Infect Dis J 1994;13:183-8
Harabuchi Y, Faden H, Yamanaka N, Duffy L, Wolf J, Krystofik D. Human milk secretory IgA antibody to nontypeable Hæmophilus influenzæ: Possible protective effects against nasopharyngeal colonization. J Pediatr 1994;124:193-8
Owen MJ, Baldwin CD, Swank PR, Pannu AK, Johnson DL, Howie VM. Relation of infant feeding practices, cigarette smoke exposure and group child care to the onset and duration of otitis media with effusion in the first two years of life.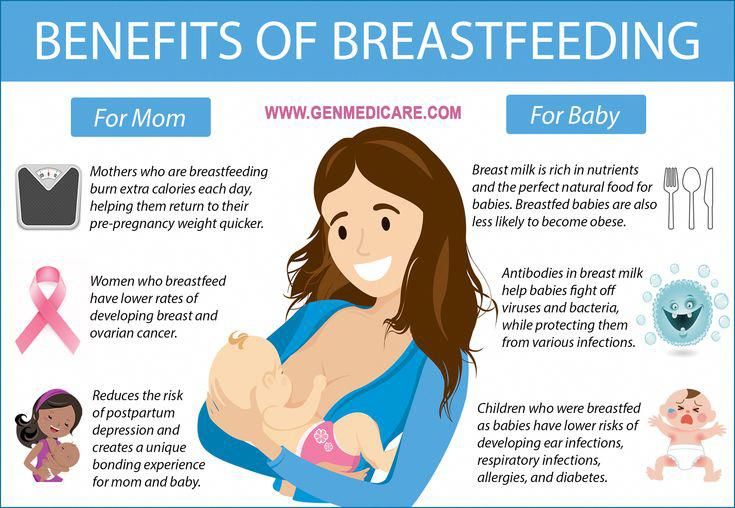 J Pediatr 1993;123:702-11
J Pediatr 1993;123:702-11
Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LJ. Exclusive breastfeeding for at least 4 months protects against otitis media. Pediatrics 1993;91:867-72
Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective cohort study. J Infect Dis 1989;160:83-94
Saarinen UM. Prolonged breastfeeding as prophylaxis for recurrent otitis media. Acta Pediatr Scand 1982;71:567-71
Why breastfeeding lying down is bad for your child’s ear —Expert
Breastfeeding is already known to offer a number of health and developmental benefits. Predominantly breastfeeding an infant for at least 6 months offers significant protection against the development of ear infection until at least age 3 years.
Still, researchers say the protective effect of breastfeeding against ear infections may be compromised when mothers breastfeed in a lying position.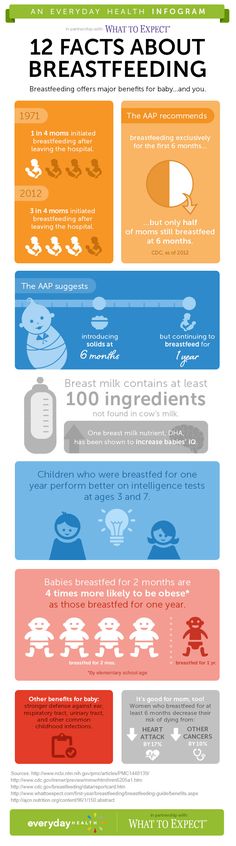 In fact, children that lay down flat whilst breastfeeding end up with more ear infections.
In fact, children that lay down flat whilst breastfeeding end up with more ear infections.
“It’s supposed to be protective but we now found out in a few studies, especially in this environment that mothers who were breastfeeding their children tend to have more children with an ear infection known as, otitis media. And we now discovered that it was the technique of breastfeeding; when mothers breastfeed the child while lying down,” said Dr Adekunle Daniel, a consultant Ear, Nose and Throat Surgeon at the University College Hospital (UCH), Ibadan.
According to Dr Daniel, “When breastfeeding the child lying down, there’s a possibility that when the child regurgitates, it goes into the ear. The enzyme that helps to break down protein in the stomach called renin has been found in the middle ear because of this regurgitation that the child has. The sugar in the milk causes germs to grow.”
Children are more likely to suffer from ear infections than adults for two reasons. Their immune systems are underdeveloped and less equipped to fight off infections. Also, their Eustachian tube (the tube that connects the middle ear to the nose and the back of the throat) is smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
Their immune systems are underdeveloped and less equipped to fight off infections. Also, their Eustachian tube (the tube that connects the middle ear to the nose and the back of the throat) is smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
Ear infections in babies and toddlers are extremely common. In fact, a study to determine the prevalence of ear infection in children aged 6 months – 10 years attending a primary health care facility in Samaru, Zaria, observed the infection to be higher in children in the age range, six months to two years.
Also, risk factors such as the use of cotton buds in cleaning the ear, the posture of the child during breastfeeding and not being exclusively breast-fed were shown to be very prominent among the children studied.
Fifty swabs from ear discharge and imparted wax were obtained from the study subjects regardless of whether they were presenting with symptoms of otitis media or not. Information on certain symptoms, as well as demographic and risk factors, was obtained through the use of questionnaires. It was in the 2021 edition of Ife Journal of Science.
It was in the 2021 edition of Ife Journal of Science.
Dr Daniel said it is important that babies after breastfeeding be allowed to burp before laying them down to sleep so that they do not regurgitate and the milk finds its way into their ear and predisposes them to develop an ear infection.
Much more, he declared that when children sleep in an overcrowded room that is not properly ventilated, they tend to have a higher incidence of ear infections.
“Again, children exposed to smoke during indoor cooking, especially with kerosene stoves, have the tendency to have ear infections more than others. Also, if the child is in a room with an individual who smokes regularly, the child can also have a higher incidence of ear infections. Those are the things that we know apart from the breastfeeding technique that can predispose children to an ear infection.”
Studies show that children who are exposed to secondhand smoke are up to three times more likely to develop ear infections than those who don’t have those exposures.
In addition, babies also get ear infections when they have a sore throat, cold, or an upper respiratory infection, which causes the lining of the Eustachian tube to swell, become congested and accumulate fluid. Common signs that your baby has an ear infection include crying, irritability, tugging at the ear, difficulty feeding, ear drainage, and fever.
The good news is that most ear infections go away on their own and those that don’t are typically easy to treat. “If you bring the baby early, there is help. The physicians can treat but of course, if the child returns to that environment, there is a possibility that it can repeat itself,” he added.
Simple steps can also be taken to reduce a child’s risk of developing ear infections such as vaccination. Children who are up-to-date on their vaccines get fewer ear infections than their un-vaccinated counterparts. The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria. Wash of hands with soap and water frequently is also the best way to protect a child against cold and flu.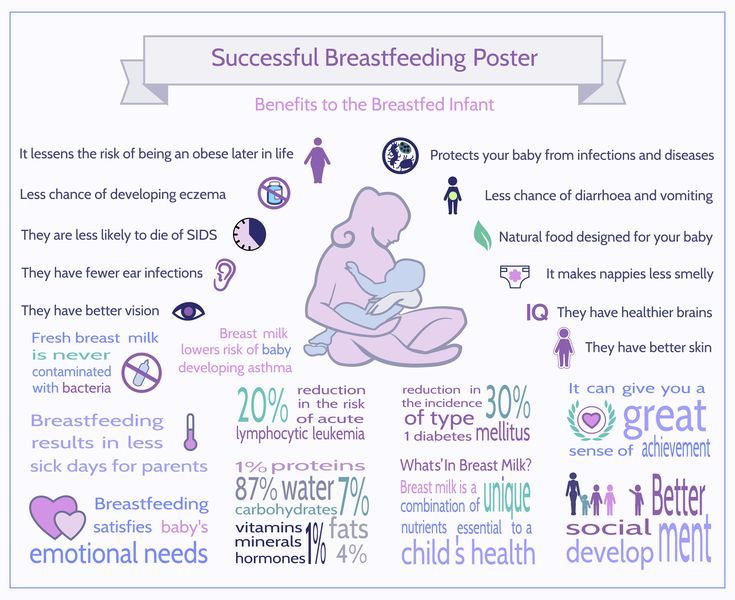
Many parents are concerned that an ear infection will affect their child’s hearing irreversibly—or that an ear infection will go undetected and untreated. But, the importance of exclusive breastfeeding and good personal hygiene cannot be emphasized to ensure children are free from an ear infection.
Otitis in children - safe treatment at the Fantasy clinic in Moscow
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Video Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.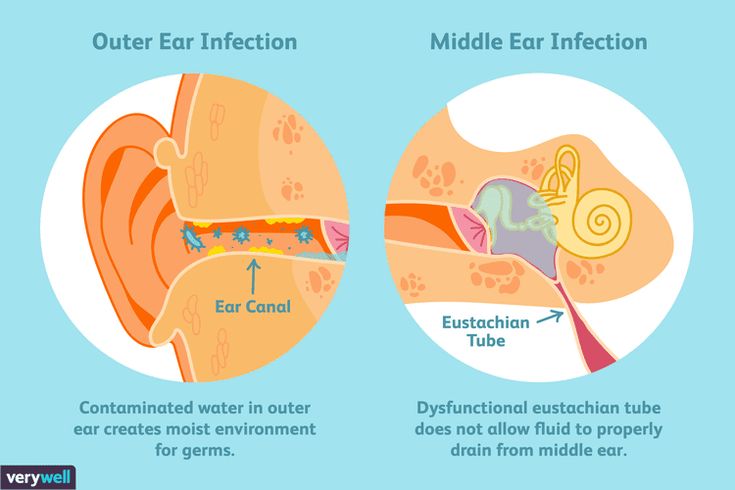
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate safety of treatment
We have made children's medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other services under "Pediatric otolaryngology (ENT diseases)"
- Consultation of a pediatric ENT doctor
Manipulations, procedures, operations
- Opening of a tonsil cyst in children
- Removal of a foreign body from the ear or nose of a child
- Stopping nosebleeds in children
- Opening of abscesses and hematomas of the nasal septum for children
- Reposition of the bones of the nose for a child
- Opening and drainage of hematomas in a child
- Removal of adenoids in children
- Shunting of the eardrums for a child installation of ventilation tubes
- Washing the lacunae of the tonsils for a child
Frequent calls
- Snoring in a child: causes and treatment
- Obstructive sleep apnea syndrome (OSAS) in children
- Hearing impairment in children: diagnosis and treatment
- Allergic rhinitis in a child: diagnosis and treatment
- Sulfur plug in a child
- Laryngitis in children: treatment
- Enlarged cervical lymph nodes in a child
- Treatment of adenoids without surgery
- Angina (acute tonsillitis) in a child: diagnosis and treatment
Online payment
Documents online
Online services
symptoms, treatment 🦷 Dnepr Amel Dental Clinic
The disease does not seem dangerous and almost every parent had to deal with it. However, behind the mask of imperceptible ailments lies a source of serious complications associated with the auditory organ and the central nervous system. Most often, this affects the youngest children - those who attend nurseries and kindergartens.
However, behind the mask of imperceptible ailments lies a source of serious complications associated with the auditory organ and the central nervous system. Most often, this affects the youngest children - those who attend nurseries and kindergartens.
How do I recognize an ear infection in myself or my child? How to treat them? Is there an alternative home therapy that will be equally effective? Let's find out in this article.
Ear infections are much more common in children than in adults. This is due to the immaturity of the immune system, more frequent upper respiratory tract infections, contact with other babies, and anatomical factors that make it easier for bacteria to travel from the throat to the ear. It is these microorganisms that are the main causes of acute otitis media.
Symptoms
Symptoms of otitis media can vary, and if one of them is found, then it is necessary to use the services of an ENT, and not self-medicate.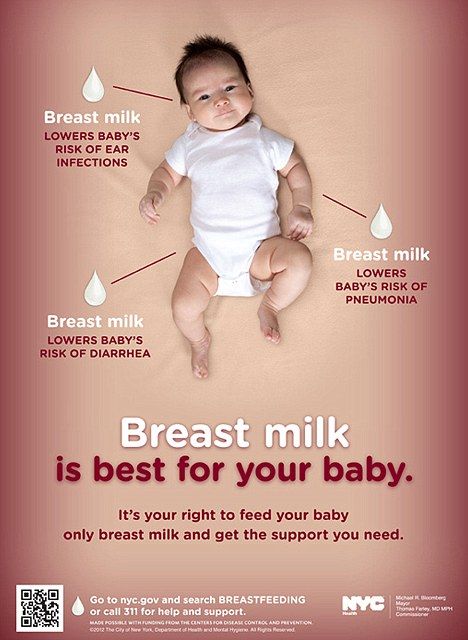 The type of disease that appears depends on many factors such as etiology, age, and anatomical predisposition.
The type of disease that appears depends on many factors such as etiology, age, and anatomical predisposition.
First of all, pain is typical for children. You can experience sensations of pulsation in the ear or the surrounding area (temples and mastoid process - part of the temporal bone).
When is soreness usually present? At night or during rest, that is, when the supine position is taken. Older children suffering from otitis media may self-report comorbidities, while toddlers will simply cry in pain.
Throbbing pain is also quite common in adults. Most children with inflammation of the middle ear also have a fever, the temperature is usually quite high, most often it exceeds 38-39 degrees Celsius.
Crying children may seem hot - but this is not the main symptom of otitis media. It is necessary to calm the baby and only then take measurements.
Symptoms:
- noise, pulsation - common symptoms resulting from inflamed vascular changes in the ear;
- a sick child will certainly not sleep peacefully at night, and during the day he may be very agitated, irritable and tired;
- lack of appetite is another alarming symptom, quite vague when it comes to otitis media, but it should always be of concern to parents;
- vomiting in a baby is a frequent signal of problems in the middle of the hearing organ;
- ear rubbing is often aimed at reducing discomfort, so children with inflammation will be overly active in that area;
- Hearing loss, sensation of blockage, foreign body and fullness are symptoms affecting both young and elderly patients;
- ear discharge.

A characteristic feature is the frequent relief of pain after cleaning. The discharge disappears, and the pressure drop in the middle cavity brings relief from pain. It is also worth paying attention to whether there have been recent infections of the upper respiratory tract or throat. The most common route for the spread of causative factors for acute otitis media is through the Eustachian tube, which connects the throat to the central part of the hearing organ.
Sometimes the disease may be accompanied by skin rashes covering the auricle: vesicles, spots, purulent lesions. If we notice a secretion from the ear canal for a long time, but there is no sign of pain after that, then this inflammation, unfortunately, can become chronic.
Otoscopic examination
An ENT or general practitioner, looking into the ear with a special viewing glass - an otoscope, will notice typical signs of inflammation, that is, dilated vessels that give the impression of redness of the eardrum.
Most often, this picture indicates the initial stage of infection. In the advanced phase, the membrane will be clearly convex, due to the pressure of secretions from its inner side. You can see a crack inside or leakage of purulent contents - this, unfortunately, indicates an advanced stage.
Treatment regimens
The first question is: should we use any therapy at all, and if so, when should we do it? Otitis often resolves on its own and there is no need to start antibiotic therapy.
However, we can use other drugs that act symptomatically to reduce the associated inflammation. The so-called vigilant observation technique is currently being used. The disease should subside without treatment within 1 to 2 days of symptom onset.
Relief of symptoms
This is definitely the most commonly used treatment. We refuse antibiotic therapy and fight fever, pain, using two main substances - ibuprofen and paracetamol in oral form.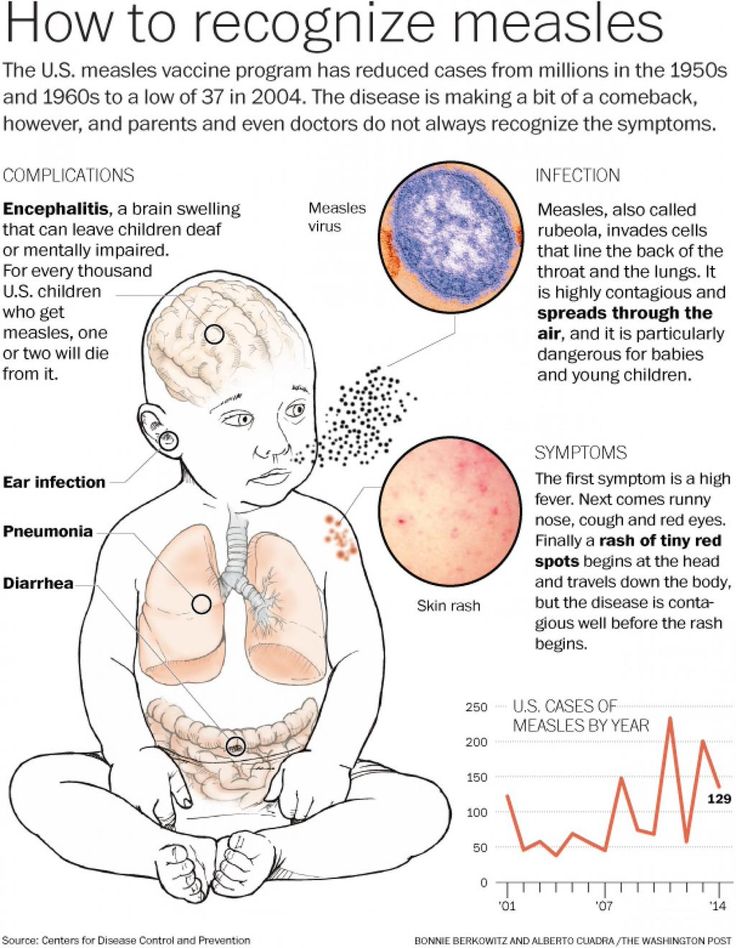
Treatment
The treatment depends, of course, on the etiology. Antibiotic therapy will become the basis of a bacterial infection. For acute otitis media, Streptococcus pneumoniae and Haemophilus influenzae are common causative agents - so we treat empirically, assuming each patient's illness is caused by one of these bacteria.
A popular drug in the medical community is amoxicillin, which is administered in high doses. Alternatively, amoxicillin in combination with clavulanic acid or intravenous or intramuscular clarithromycin may be used in the absence of improvement or increased sensitivity to penicillin drugs.
Antibiotic therapy will be included in severe disease, high fever and vomiting in all children who have factors predisposing to the development of the disease and its frequent relapses: in children under 6 months of age due to the immaturity of the immune system and the inability to independently cope with infection, in children under 2 years of age with inflammation in both ears.
Otitis media appears among other diagnoses. Its symptoms are earache, irritability and high fever.
Interesting fact
Diet
Complex carbohydrates, hot liquids, vegetables and soups prepared from these products are an ally in the fight against pathological conditions of the hearing organs. Substances with antibacterial activity, natural antibiotics are also allowed: garlic, onion, ginger. It is important to drink plenty of water to facilitate the outflow of colonies of pathogens that colonize the mouth or throat.
Wraps
Two things are needed to make them: an anesthetic that simultaneously destroys the etiological factor, and a thin scarf, gauze, to wrap him/her and attach to the patient's ear.
Organic ingredients will also help in this: chamomile, ginger, onion or garlic. Onions, ginger and garlic should be peeled and then chopped. Then wrap the ingredient in gauze or a thin scarf, heat it to a temperature of about 37 degrees Celsius and then place it on the ear. It is worth putting a cap on your head, which increases the surface of the compress. It should stay on the body for about an hour. Instead of onion or garlic, gauze can be filled with dried chamomile. However, such a compress should be placed in a closed vessel over a water bath in order to warm it up significantly and make it moist. This composition should be kept in the ear area for about 45 minutes - 1 hour.
It is worth putting a cap on your head, which increases the surface of the compress. It should stay on the body for about an hour. Instead of onion or garlic, gauze can be filled with dried chamomile. However, such a compress should be placed in a closed vessel over a water bath in order to warm it up significantly and make it moist. This composition should be kept in the ear area for about 45 minutes - 1 hour.
Essence
It can be prepared with an oil base, with or without an antibacterial agent (ginger, garlic). You will get a consistency that will allow you to deliver a few drops to the patient's ear. It is best to reheat the medicine before serving. However, it is important to check the temperature of the solution on the back of the hand before use.
Another way is to use a cotton swab soaked in the compound to be placed in the ear. The wonderful properties of tea tree oil, which is applied directly to the ear or on a cotton pad, are also known.
Extracts
In a mortar, we can grind garlic or onion cloves, squeeze the pulp through cheesecloth, and then put a few drops of the juice on the ear affected by inflammation.