Can i feed baby with mastitis
Mastitis | The Royal Women's Hospital
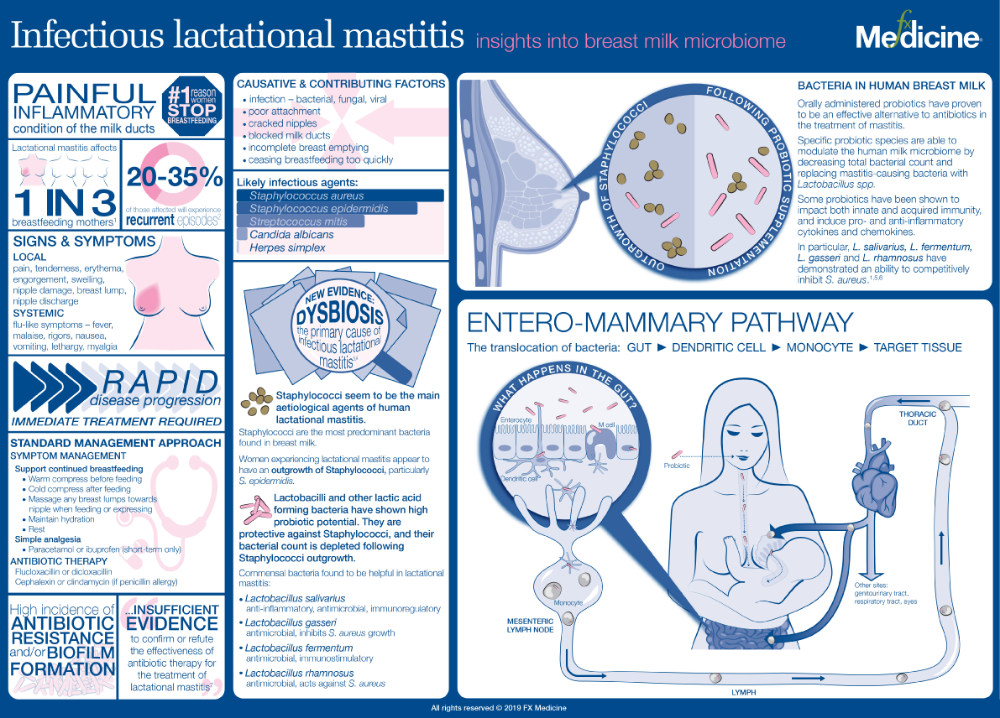
Mastitis is an inflammation of the breast that can lead to infection. Mastitis can feel like you have the flu; you may feel hot and have body aches and pains.
Common causes
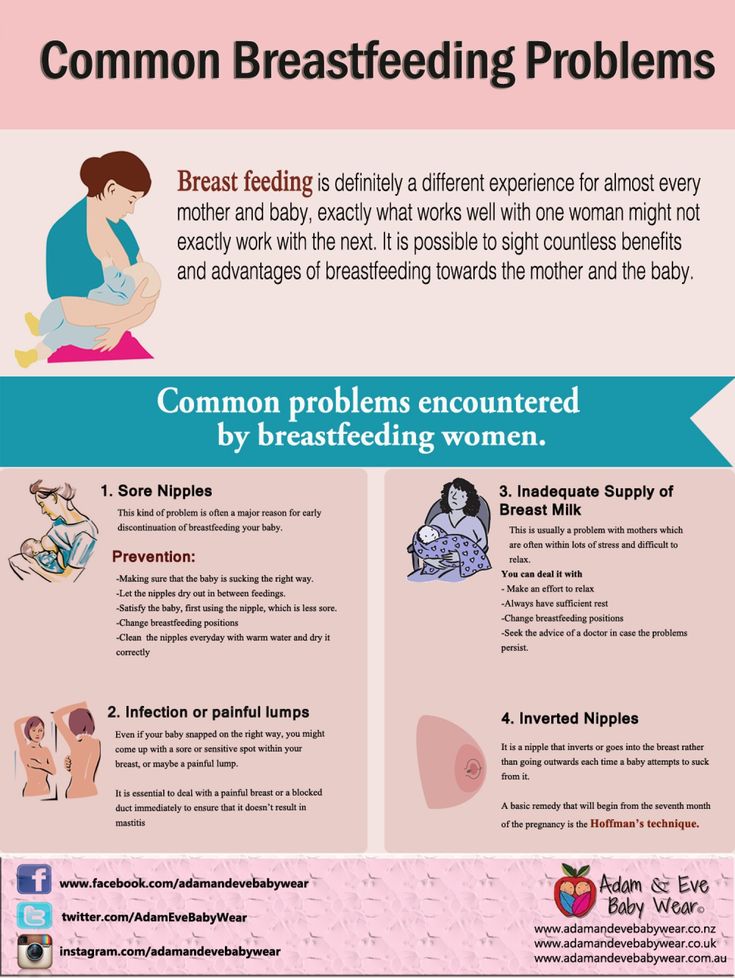
- Poor attachment to the breast
- Nipple damage
- A long break between breastfeeds
- Breasts that are too full
- Blocked milk ducts
- Stopping breastfeeding too quickly
- Overly tight bra
- A baby with tongue-tie who is having problems attaching to the breast
Signs and symptoms
- A red, sore area on the breast
- Flu-like symptoms – feeling hot and cold with aching joints
Prevention
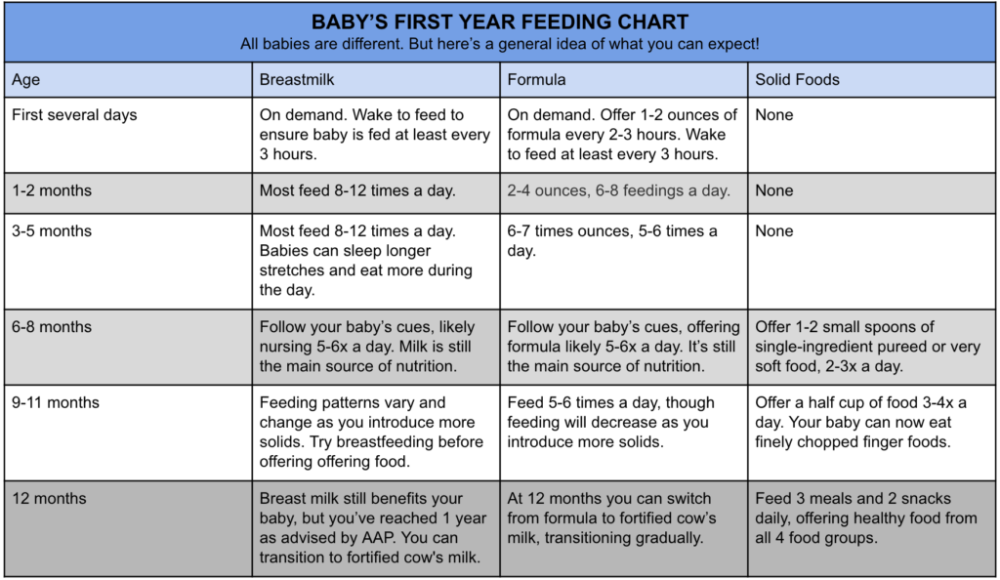
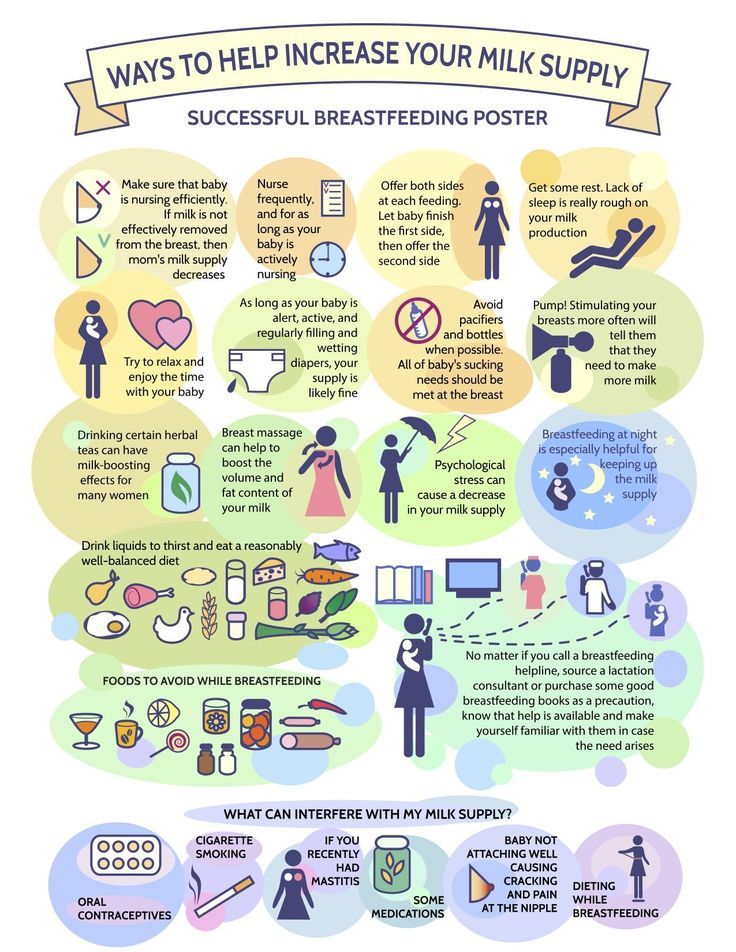
- Breastfeed as often as your baby needs (normally 8 to 12 times in 24 hours for a new baby).
- Don’t miss or put off breastfeeds.
- Wake your baby for a feed if your breasts become too full. If your baby doesn’t want to feed you may need to express a small amount of milk.
- See a lactation consultant or maternal and child health nurse to make sure your baby is attaching and feeding well at your breast.
- Offer both breasts at each feed. If your baby only feeds from one breast make sure to offer the alternate breast at the next feed.
- Express a small amount of milk after feeds if your breasts still feel full – express only until your breasts feel comfortable.
- Avoid giving your baby formula feeds or other fluids unless advised to by a midwife, nurse or doctor.
- Avoid pressure on your breasts from clothes or from your fingers when feeding.
- Try to get some rest during the day when your baby is asleep.
Treatment
It is important to start treatment at the first signs of mastitis.
- Your breast milk is safe for your baby even if you have mastitis, so continue to breastfeed or express from the affected breast.
- Place a heat pack or warm cloths on the sore area before feeding or expressing to help with your milk flow.
 If your milk is flowing easily then warm packs are not needed.
If your milk is flowing easily then warm packs are not needed. - Gently massage any breast lumps towards the nipple when feeding or expressing or when in the shower or bath.
- Continue to breastfeed or express your sore breast until it feels more comfortable.
- Place a cool pack, such as a packet of frozen peas wrapped in a cloth, on the breast after feeding or expressing for a few minutes to reduce discomfort.
- You can take tablets for the pain such as paracetamol or ibuprofen. They are safe to take while breastfeeding.
- Drink plenty of water throughout the day (up to 8 glasses).
- Rest as much as possible. Ask your partner, family or friends for help with household tasks.
- If you don’t start to feel better after a few hours, you should see a doctor as soon as you can. When making the appointment tell the clinic you think you have mastitis.
- If antibiotics are prescribed by your doctor, take as directed. It is safe to continue to breastfeed when taking these antibiotics.

Related Health Topics
-
- Mastitis
Mastitis is inflammation of the breast, which may lead to infection.
-
- (English) PDF (326 KB)
- (Arabic) PDF (301 KB)
- (Chinese) PDVF (335 KB)
- (Turkish) PDF (306 KB)
- (Vietnamese) PDF (319 KB)
- Mastitis
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Mastitis - Symptoms - Treatment
What is mastitis?
Mastitis is an inflammation of the breast. It is usually caused by an infection. It often happens while a woman is breastfeeding, especially during the first 6-12 weeks.
What are the symptoms of mastitis?
Women who have mastitis may feel ill. They may feel run down or achy. In addition to an inflamed breast, they may feel like they have the flu. Other symptoms may include:
- Breast pain
- Swelling
- A tender, red, wedge-shaped area on the breast
- A breast that is warm or hot to the touch
- A burning sensation while breastfeeding
- Discharge from the nipple
- Fever
- Chills
- Nausea or vomiting
Mastitis usually affects only one breast at a time.
What causes mastitis?
Mastitis is usually caused by germs (bacteria) that are found on the skin or in your baby’s mouth. These bacteria can enter your breast through a milk duct opening or a crack in the nipple.
Infection is more likely to happen when milk is trapped in the breast. Stagnant milk sitting in the breast makes bacteria grow, which leads to infection. Trapped milk can happen due to inexperience or poor technique in breastfeeding. Or sometimes a milk duct can get blocked, causing milk to back up in the breast.
You may be at higher risk of developing mastitis if you:
- Have sore or cracked nipples
- Use only one position to breastfeed (using different positions helps make sure you completely drain the breast)
- Wear a tight-fitting bra or put pressure on your breasts (which can restrict milk flow)
How is mastitis diagnosed?
Your doctor will ask you about your symptoms and examine the affected breast. He or she will check for swelling, tenderness and a painful, wedge-shaped area on the breast that is a tell-tale sign of mastitis.
If you are not breastfeeding and you have symptoms of mastitis, your doctor may order other tests. These could include a breast ultrasound, MRI, mammogram, or biopsy.
Can mastitis be prevented or avoided?
Below are some basic breastfeeding techniques to lower your risk of developing mastitis.
- Your baby should latch onto the nipple with his or her mouth open wide.
- Allow your baby to empty one breast before switching to the other breast.
- Change your baby’s position from one feeding to the next to help empty all the areas of the breast.
- If you need to stop a feeding, break the suction using your finger.
- Don’t wear tight-fitting bras or breast pads that cause your nipples to stay moist after breastfeeding.
- Air your nipples out when possible.
- Tell your doctor or lactation consultant if you have nipple pain during nursing.
Mastitis treatment
Sometimes breast infections go away on their own.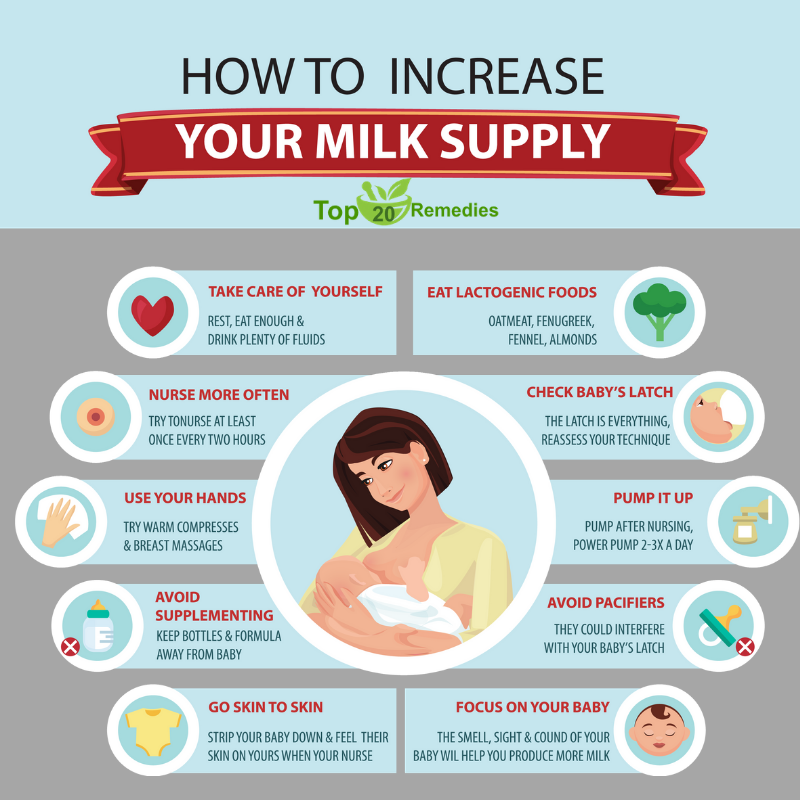 If you notice you have symptoms of mastitis, try the following:
If you notice you have symptoms of mastitis, try the following:
- Breastfeed on the affected side every 2 hours, or more frequently. This will keep your milk flowing and prevent your breast from getting too full of milk.
- Massage the area. Start behind where it is sore and use a circular motion toward the nipple.
- Apply warm, moist compresses to the sore area.
- Wear a supportive, well-fitting bra. Make sure it isn’t too tight. You don’t want to constrict your milk ducts.
If you don’t start feeling better 24 hours after trying these tips, or if your symptoms are getting worse, call your doctor. You may need medicine.
Your doctor will likely prescribe antibiotics to clear up the infection. You should start to feel better a few days after starting the antibiotics. But make sure you take all the antibiotics your doctor prescribes to prevent antibiotic resistance.
Over-the-counter pain medicines such as acetaminophen (brand name: Tylenol) or ibuprofen (brand name: Advil) can help relieve pain. Warm showers can also help relieve the pain.
Warm showers can also help relieve the pain.
Although it may be painful, it is important to keep breastfeeding when you have mastitis. Your breast milk will not be bad for your baby, even if you have mastitis, although some infants may not like the taste. If you stop breastfeeding, germs can spread in the milk that is left in your breast. This could make your infection worse. If you cannot nurse your baby, you should pump your breasts to remove the milk.
Getting enough rest and drinking extra fluids can help you feel better faster. Talk to your doctor if your symptoms get worse.
Living with mastitis
If mastitis isn’t treated properly, an abscess (collection of pus) may develop. This could form a mass in your breast. Abscesses are usually painful. They normally have to be drained surgically.
Call your doctor right away if you notice any of the following symptoms:
- Infection in both breasts
- Pus or blood in your breastmilk
- Red streaks near the affected area
- Symptoms came on severely and suddenly
- A painful lump that might be an abscess
To prevent these types of complications, call your doctor when you first notice symptoms of mastitis.
Questions to ask your doctor
- What is the likely cause of my mastitis?
- Is my milk still safe for the baby?
- Do I need antibiotics? How should I take them? Are they safe for the baby?
- I’d like someone to observe my breastfeeding technique. Do you have a lactation consultant on staff?
- Where can I find breastfeeding support?
- Is there anything else I should do to help prevent mastitis?
Resources
American Cancer Society: Mastitis
La Leche League International: Mastitis
Pampers: What Causes Mastitis & How Do You Treat It?
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Mastitis: symptoms and treatment | Philips Avent
search support iconSearch Keywords
Home ›› Breastfeeding mastitis symptoms and treatment
Home ›› Breastfeeding mastitis symptoms and treatment
↑ top
breastfeeding - one of the most natural processes for a woman, but it is not always easy. Along with the individual aspects of breastfeeding, there are some general problems that new breastfeeding mothers may face.
Along with the individual aspects of breastfeeding, there are some general problems that new breastfeeding mothers may face. One of them is mastitis, an inflammatory disease that causes tenderness and tenderness in the breast tissue.
The frequency of lactational mastitis among women in different countries ranges from 2% to 33% and averages about 10%*.
Mastitis in breastfeeding women is caused by a bacterial infection of the milk ducts that enters through cracks, irritation of the nipple, or a nipple piercing.
Lactational mastitis is dangerous because it can cause pain while breastfeeding, interfere with the bonding process between mother and baby, or even interfere with milk production.
To protect the health and comfort of mother and baby, and the mother's milk supply, this problem must be addressed urgently.
So, here are the answers to the most frequently asked questions about mastitis and the fight against it: “How does mastitis occur?”, “What are the symptoms of mastitis?” and "Is it possible to breastfeed with mastitis?".
Ask your doctor for more information.
Signs of mastitis
What does mastitis feel like? In addition to pain and discomfort, symptoms of mastitis can also include fatigue and a feeling of exhaustion.
How mastitis manifests:
- fever (>38.5°C) and/or flu-like symptoms;
- nausea;
- vomiting;
- yellowish discharge from the nipple;
- chest warm or hot to the touch;
- pink or red breasts.
These symptoms of mastitis are similar to the symptoms of breast engorgement, but there is a fundamental difference between these conditions. Mastitis differs from engorgement in that it usually only affects one breast, not both.
Causes of mastitis
Mastitis can develop in a new mother at any time, but it usually occurs within the first two to three weeks after childbirth. A common cause of this disease is long breaks between feedings - for example, when the baby begins to sleep through the night.
Other possible causes of mastitis are:
- improper breastfeeding;
- incomplete outflow of milk from the mammary glands, for example, due to blockage of the milk duct;
- unattended breast engorgement;
- regular pressure on some part of the breast, wearing tight clothing;
- chest injury caused by injury or impact.
In short: mastitis usually develops as a result of too much milk in the breast, known as milk stasis. Stagnation of milk provokes the growth of bacteria, which causes mastitis and symptoms of pain and fever. Therefore, to prevent mastitis and stagnation of milk, it is important to make sure that it is removed from the breast properly.
Blockage of the milk ducts can also be the cause. Mastitis is indeed caused by milk stagnation or too long milk in the breast, but this condition and the subsequent symptoms of mastitis - fever and pain - are precisely due to the rapid multiplication of bacteria due to milk stagnation.
Prevention of mastitis while breastfeeding
The good news is that there are many ways to prevent mastitis. Below you will find some tips on how to avoid mastitis.
1. Care for your breasts to prevent nipple irritation. Proper breast care can help prevent mastitis by gently massaging and keeping your nipples dry with soft bra pads.
Find out more about breast care in our article here.
2. Feed your baby often. For complete emptying of the breast, it is important to feed regularly and on time. Even if the baby is sleeping, it should be woken up when it's time for feeding. If the mother cannot be with the baby during feeding, she should express milk from the breast using a breast pump.
Choose an easy-to-use breastpump, such as a single electric breastpump. It allows you to express gently and naturally thanks to the special Natural Motion technology. Many of the complications of breastfeeding can be avoided if the baby latch on properly. Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
4. Wean your baby gradually. To minimize the chance of complications, it is necessary to reduce milk production by gradually reducing the number of breastfeeds.
If you're interested in stopping breastfeeding, check out our tips for weaning your baby in the article here.
Treatment of mastitis in women
One of the most common questions that breastfeeding mothers face with mastitis is: “Can I continue to breastfeed?” Answer: yes. What's more, breastfeeding for mastitis can help clear the infection without causing harm or side effects.
An important point: if you have symptoms of mastitis, contact your doctor immediately. Doctors usually prescribe antibiotics (such as acetaminophen or ibuprofen) to relieve symptoms of mastitis after making sure that the prescribed drug is safe for breastfeeding.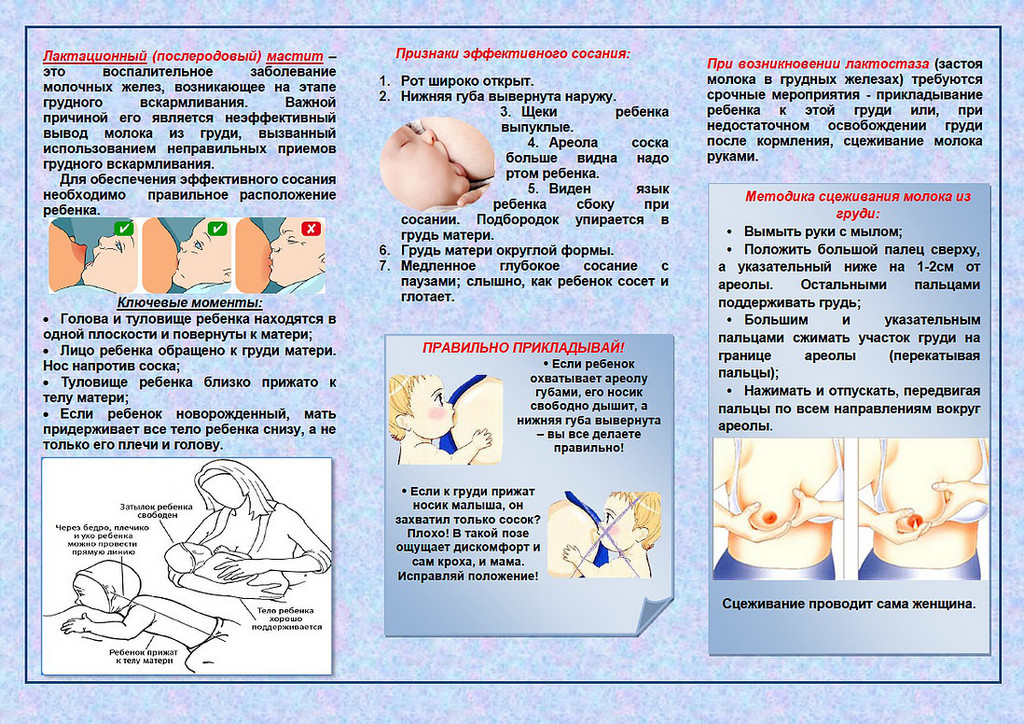
Mastitis can be uncomfortable, but there is no reason to panic or despair. This is a common problem that many new mothers experience when breastfeeding for the first time. By following the advice in this article, you can reduce the likelihood of developing mastitis, but if something bothers you, you should seek the help of a specialist.
Articles and tips from Philips Avent
*Lactational mastitis and lactostasis: tactical contraversion. O.A. Void. Peoples' Friendship University of Russia, Moscow, 2013
Baby+ app
Download the app and track your child's development and growth with trackers, and save these special moments forever.
Download App:
App Pregnancy+
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website.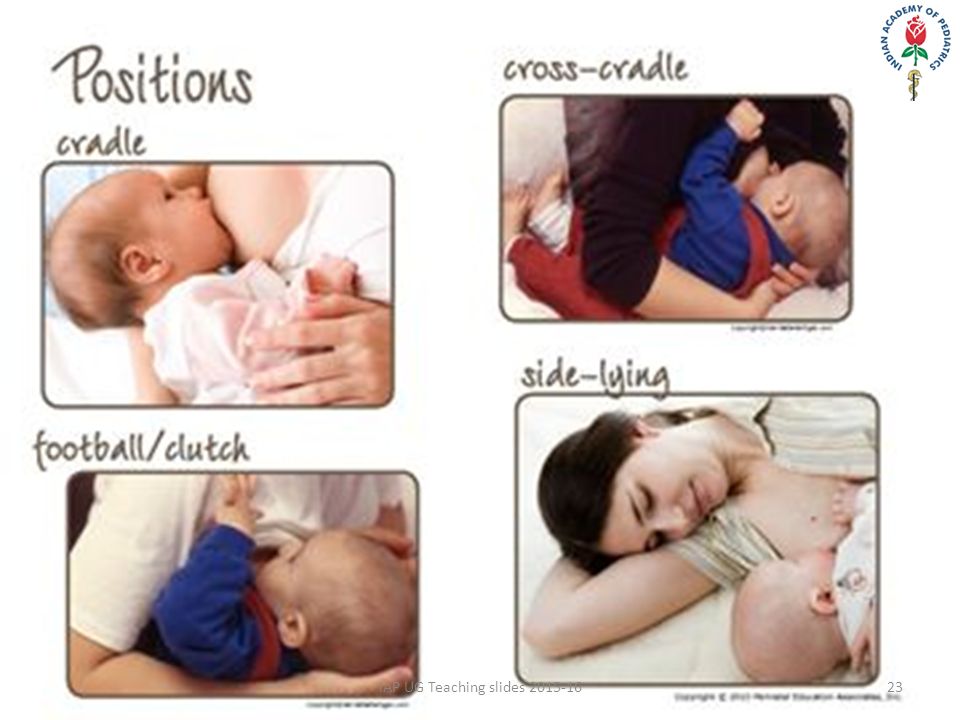 Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Laktostasis symptoms and treatment
search support iconSearch keywords
One of the most common problems breastfeeding mothers face is blocked milk ducts, also known as milk stasis or lactostasis. What sensations arise with a clogged milk duct? A sensitive seal appears in the chest, and slight pain and discomfort may occur.
We'll cover the most common questions about this problem and provide all the important information about blocked ducts, from the symptoms of blocked ducts in the breast to treatments and tips to prevent the condition.
If you need more information, ask someone else.
Signs of blocked milk duct
What is blocked milk duct and how is it different from other breast conditions like mastitis? Blockage of the milk duct, also known as milk stasis or lactostasis, is a condition in which a milk clot forms in the breast, preventing milk from flowing out of the duct. A painful lump forms in the chest, and there may be a feeling of discomfort around it.
Common symptoms of blockage of the breast duct are:
- pain in a certain area of the breast;
- painful lump in the mammary gland the size of a pea or more;
- slight increase in temperature in the area of blockage;
- sometimes a small white bubble forms on the nipple.
In a nutshell, duct blockage is the formation of a localized lump in the chest that causes discomfort in the absence of any other signs of illness or fever. If there is a fever or flu-like symptoms and if the chest feels hot to the touch, it may be mastitis.
More information on symptoms and treatment for mastitis can be found here.
Causes of blockage of the breast duct
Blockage of the milk duct can occur for several reasons:
- incomplete flow of milk from the breast during feeding;
- incorrect attachment of the child, because of which he cannot fully suckle the breast;
- engorgement;
- excess milk production;
- abrupt cessation of breastfeeding;
- putting pressure on the mammary gland: for example, wearing tight clothing that squeezes the chest.
Blockage of the milk duct usually occurs as a result of incomplete emptying of the breast or excessive pressure on the breast for a long period of time.
How to remove blockage of the milk duct?
To prevent a breast infection, it is important to find a way to clear the blocked milk duct as soon as possible.
Here's what to do if your milk duct is blocked:
- Continue breastfeeding.
 If the milk duct is blocked, you should continue to feed the baby and try to do it so that the baby sucks out all the milk. You can also try breastfeeding a baby with a blocked duct every two hours. This will help keep the milk flowing and possibly clear blockages. Continuous stimulation of the flow of milk is the key to eliminating blockage of the duct.
If the milk duct is blocked, you should continue to feed the baby and try to do it so that the baby sucks out all the milk. You can also try breastfeeding a baby with a blocked duct every two hours. This will help keep the milk flowing and possibly clear blockages. Continuous stimulation of the flow of milk is the key to eliminating blockage of the duct.
These bra pads help prevent milk stains on clothing while breastfeeding. Their porous top layer and excellent absorbency will help keep clothes dry and comfortable.
- Massage and express between feeds. Before each feeding, it is recommended that the mother massage the breast with stroking movements from the periphery of the breast to the nipple. This stimulates the flow of milk even before the start of feeding. After breastfeeding, a mother can express any milk left in a breast with a blocked duct to ensure that the ducts are completely emptied. Stimulating the flow of milk can help prevent blockages in the milk ducts, but there are times when a mother cannot be with her baby during breastfeeding.
 To stimulate the flow of milk in such situations, it is very important to express milk manually.
To stimulate the flow of milk in such situations, it is very important to express milk manually.
Check out these manual breast pumps for expressing milk anywhere, anytime.
- Latch the baby correctly to the breast. Attaching the baby to the breast in such a way that his chin is directed towards the blocked duct can help solve the problem. Such attachment to the breast will help the baby, when sucking, empty exactly the area of \u200b\u200bthe mammary gland where there is a blockage. You can try to apply the baby in different ways, so that it is more convenient for him to extract all the milk from different parts of the breast.
- Apply warm and cold compresses. As compresses, you can use a towel, as well as thermal pads 2 in 1. It is recommended to apply a warm thermal pad to the area of the clogged duct several times a day, while doing a light massage. Breast discomfort after feedings can be alleviated somewhat by using cooled thermal pads.

- Wear comfortable, loose-fitting clothing. One of the causes of blockage of the milk ducts is excessive pressure on the mammary glands for an extended period of time. This pressure can be exerted by tight clothing or bras, so it is important to wear loose clothing to clear a blocked duct. Sometimes mothers also notice clogged pores on their breasts - loose clothing and a bra will also help to cope with this problem.
- Tight clothing encourages more sweating and prevents sweat from evaporating, resulting in clogged pores. Moms should wear loose-fitting clothing to clear clogged pores and clear blocked milk ducts.
If following these tips fails to open the milk duct, it is recommended that you contact your doctor or lactation consultant to prevent infection.
How to prevent clogged milk ducts?
Every mother would like to avoid the problem of blocked milk ducts altogether. No one will give a 100% guarantee against blockage of the milk ducts, but you can try to prevent it by using a few useful tips.
- After each feeding, check that there is no feeling of fullness and discomfort in the chest. If it is, then it is necessary to additionally express milk, until a feeling of comfort.
- Feed your baby regularly for as long and as often as he wants
- Express milk between feedings if you experience discomfort and fullness in your breasts.
- Place the baby on the breast without undue pressure.
- Wear loose, comfortable clothing and bralettes.
When should I seek professional help?
When a blockage of the milk duct occurs, the mother should not panic. Despite the discomfort and pain, this condition is quite normal and usually goes away if treated immediately.
If you want to know how to clear a blocked milk duct, or if you are feeling a blocked milk duct, you should seek help from your doctor.
Find out more about other common breastfeeding problems and how to deal with them.
Philips Avent Articles & Tips
Links
The New Breastfeeding Guide for Mothers 3rd Edition (2017)
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.