Can i pass food poisoning to my baby
Food poisoning during pregnancy | March of Dimes
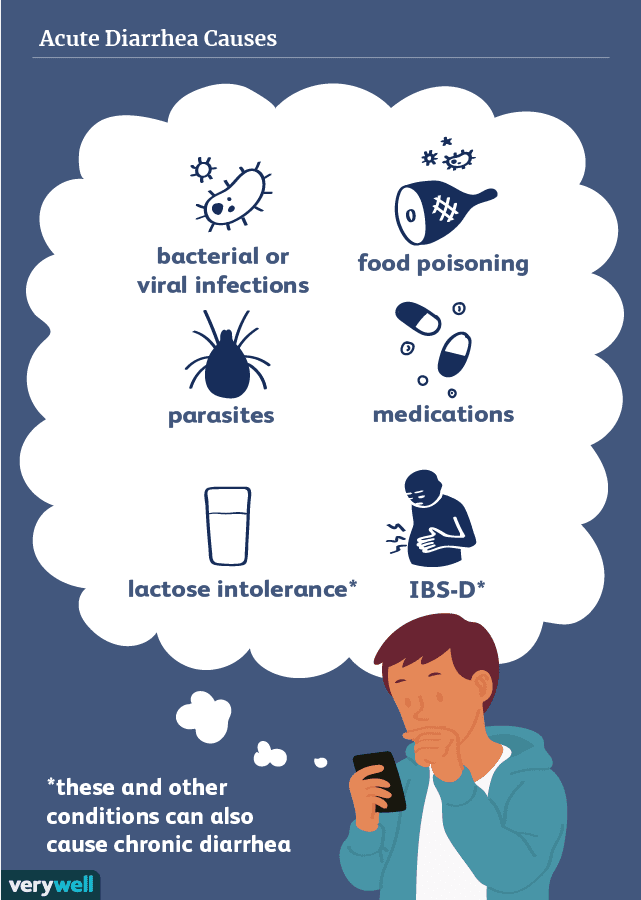
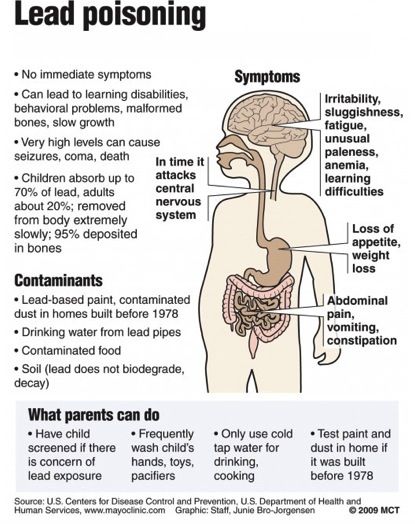
Food poisoning happens when you eat or drink something with harmful bacteria (germs) in it.
Normal changes in your body during pregnancy may make you more likely to get food poisoning.
During pregnancy, food poisoning can cause serious problems for you and your baby, including premature birth, miscarriage and stillbirth.
Wash your hands before handling food and learn how to handle food safely. Don’t eat foods that commonly cause food poisoning.
If you think you have food poisoning, call your health care provider right away.
What is listeriosis and how can it affect pregnancy?
Listeriosis is a kind of food poisoning caused by Listeria bacteria. During pregnancy, you can pass the bacteria to your baby. This can cause problems, including:
- Miscarriage. This is when a baby dies in the womb before 20 weeks of pregnancy.
- Stillbirth.
This is when a baby dies in the womb after 20 weeks of pregnancy.
- Preterm labor and premature birth. These are labor and birth that happen too early, before 37 weeks of pregnancy. Babies born prematurely may have health problems and birth and later in life.
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
- Life-threatening infections in your baby, including bacteria in the blood (called bacteremia) and meningitis. Meningitis is an infection that causes swelling in the brain and spinal cord. Infected babies may have health problems after birth, including seizures, blindness and problems with the brain, heart and kidneys.
Listeria may be in the soil, water, on animals and in animal waste. The most common cause of listeriosis is eating food with Listeria in it. Foods that are most likely to have Listeria include:
- Unpasteurized milk and foods made with it. If milk is pasteurized, it’s been heated to kill germs.
 Look for the word “pasteurized” on the label.
Look for the word “pasteurized” on the label. - Soft cheeses, like feta, Brie, Camembert, Roquefort and Mexican-style cheeses, like queso fresco, queso blanco, Panela and Asadero
- Deli meat, hot dogs, juice from hot dogs and dry sausages that are chilled or at room temperature
- Unwashed fruits, vegetables or sprouts
- Cold salads from delis or salad bars
- Refrigerated patés or meat spreads (Canned meat spreads are safe.)
- Refrigerated smoked seafood, including nova-style, lox, kippered, smoked and jerky
How do you know if you have listeriosis?
Signs and symptoms of listeriosis usually start a few days after eating food contaminated by Listeria, but they may not happen for up to 2 months. They’re usually mild and flu-like. Your health care provider can test your blood to see if you have listeriosis.
Call your provider right away if you have:
- Being confused or having trouble with balance
- Fever or chills
- Headache
- Muscle aches
- Nausea (feeling sick to your stomach) or diarrhea
- Seizures
- Stiff neck
What is salmonellosis and how can it affect pregnancy?
Salmonellosis is a kind of food poisoning caused by Salmonella bacteria. Salmonellosis can cause problems during pregnancy, including:
Salmonellosis can cause problems during pregnancy, including:
- Dehydration. This is when you don’t have enough water in your body. Signs and symptoms of dehydration include feeling dizzy or lightheaded, having a fast heartbeat, having dark-colored urine and having a dry mouth and lips.
- Bacteremia
- Meningitis
- Reactive arthritis (also called Reiter’s syndrome). This condition can cause swelling or pain in joints, like the knees, ankles and toes.
You can pass salmonellosis to your baby during pregnancy. If your baby is born with salmonellosis, she may have diarrhea and fever after birth. She also may develop meningitis.
You can get infected with Salmonella in two ways:
- By touching an infected animal. Salmonella can be found in poop, soil, water (including fish tank water), food and bedding of infected animals, including pets. Salmonella germs can spread easily to an animal’s fur, feathers and scales. Animals that are most likely to carry Salmonella include reptiles (turtles, lizards, snakes) and poultry (chickens, ducks, geese).
- By eating foods that are contaminated with Salmonella. These foods may look and smell normal, even if they’re contaminated.
Foods that often have Salmonella include:
- Raw or undercooked poultry, meat or fish. Cooking these items fully kills Salmonella.
- Raw or undercooked eggs and foods made with them. Salmonella can pass from chickens to their eggs. Even eggs that look normal can have Salmonella. Don’t eat food made with raw eggs, including homemade mayonnaise, hollandaise sauce, Caesar salad dressing, cookie dough, frostings and homemade ice cream.
- Unpasteurized milk, milk products and juice, or foods made from them. Milk and juice often are pasteurized. Look for the word “pasteurized” on the product label.
- Foods that come in contact with animal poop in the soil or water where they grow. These include mushrooms, fruits, vegetables and vegetable sprouts, like alfalfa, clover, radish and mung beans.
- Food that comes into contact with Salmonella while you’re making or serving it.
 For example, if you’re infected and don’t wash your hands after using the bathroom, you can spread the infection to food. Or if you use the same knife to cut raw chicken and tomatoes and don’t wash the knife in between, the knife can pass Salmonella from the chicken to the tomatoes.
For example, if you’re infected and don’t wash your hands after using the bathroom, you can spread the infection to food. Or if you use the same knife to cut raw chicken and tomatoes and don’t wash the knife in between, the knife can pass Salmonella from the chicken to the tomatoes.
How do you know if you have salmonellosis?
You may be at increased risk of getting salmonellosis if you:
- Have reduced stomach acid from using medicines for heartburn (called antacids), like Tums®.
- Have recently used antibiotics. Antibiotics are medicines that kill infections caused by bacteria.
- Have a digestive condition called inflammatory bowel disease (also called IBD). Digestion is the process of how your body breaks down food after you eat.
- Have a weak immune system or an illness like HIV, sickle cell disease or malaria
- Travel to places that don’t have good sanitation systems. This means they don’t have toilets and clean water for cooking and washing.
- Have a pet bird or reptile
- Live and eat in group housing, like a dormitory
Signs of salmonellosis usually start a half day to 3 days after contact and last for 4 to 7 days. To test for salmonellosis, your health care provider takes a stool sample (a sample of your poop) and sends it to a lab for testing.
Call your provider right away if you have any signs or symptoms of salmonellosis, including:
- Belly pain
- Blood in your poop or dark or amber-colored urine (pee)
- Dehydration
- Fever or chills
- Headache
- Muscle pains
- Nausea, diarrhea or throwing up
How is food poisoning treated?
Treatment depends on how sick you are. You may not need any treatment, or your provider may treat you with antibiotics to help keep you and your baby safe. If you have food poisoning, drink lots of water to help you stay hydrated (have water in your body). If you’re severely dehydrated (don’t have enough water in your body), you may need to go to the hospital for treatment.
How can you protect yourself and your baby from food poisoning during pregnancy?
Here’s what you can do:
- Wash your hands right before handling food. Wash your hands well with soap and water after using the bathroom.
- Wash your hands well with soap and water after touching animals or their food, bedding, tanks or waste.
- Don’t eat foods that are likely to be contaminated with Listeria or Salmonella.
- Handle foods safely whenever you wash, prepare, cook and store them. Wash knives, cutting boards and dishes used to prepare raw meat, fish or poultry before using them for other foods.
More information
Centers for Disease Control and Prevention
Food and Drug Administration
Last reviewed: May, 2016
What to Do and How to Treat It
It can seem like there’s nothing worse than food poisoning — except maybe getting food poisoning while parenting. Not only do you feel terrible, but it can feel like you can’t catch a break.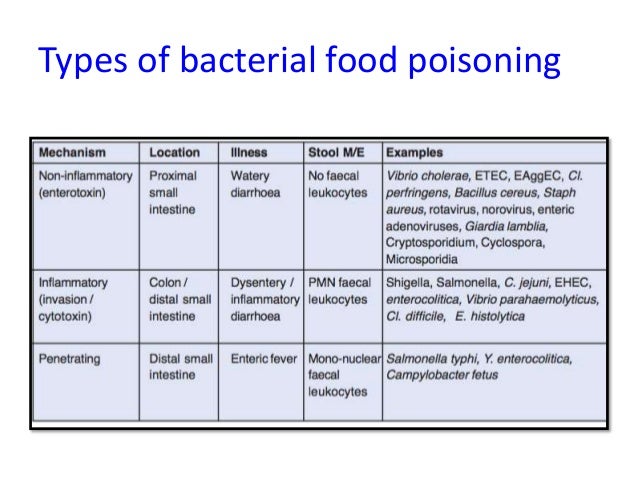 The parenting must go on, multiple trips to the bathroom and all.
The parenting must go on, multiple trips to the bathroom and all.
And if you’re a nursing parent, you may face an added stress: the uncertainty of whether you can continue.
That’s a valid worry — after all, you don’t want your child somehow catching a food-borne illness through your milk. But thankfully, having food poisoning while breastfeeding is generally not a problem, according to 2017 research.
So you can (and should) keep nursing your baby.
As the Centers for Disease Control and Prevention (CDC) explains, you don’t have to stop breastfeeding when you have food poisoning, which is a non-medical term for a food-borne disease or infection.
In fact, the CDC actually recommends that you should continue breastfeeding.
But wait, there’s more: The CDC also encourages you to nurse even more frequently, while also increasing your own fluids.
Why? Because breastfeeding more frequently while you have food poisoning helps protect your baby from contracting the illness, too. It’s also excellent rehydration therapy if your baby has diarrhea.
It’s also excellent rehydration therapy if your baby has diarrhea.
No one wants their baby to be exposed to a pathogen that causes uncomfortable and potentially worrisome symptoms. So it makes sense to want to know about the potential risks of breastfeeding while you have a bout of food poisoning, despite expert assurance that you should continue.
Here’s what to know about the potential (but unlikely) risks of breastfeeding with food poisoning:
Danger to breastfeeding parent
Although food poisoning certainly isn’t a comfortable experience, most adults fare well and are back to health after a couple of days. However, adults who are older, immunocompromised, or pregnant may have a tougher time and may require medical attention if the situation becomes severe.
But it’s important to remember that even moderate cases of food poisoning can cause dehydration. Some breastfeeding parents notice drops in their milk supply after illnesses like food poisoning. That’s why it’s important that you stay well hydrated.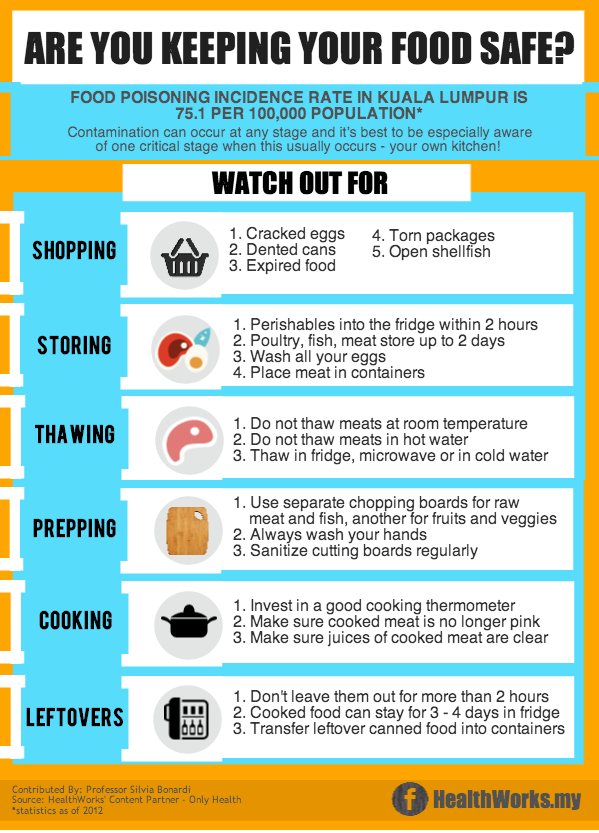
If you do notice a drop in your milk supply, it should be temporary. Nursing more frequently and replenishing your fluids should resolve things.
Danger to breastfed baby
As the CDC notes, almost all the organisms that cause food poisoning don’t get into breast milk, so there’s virtually no danger of your baby getting food poisoning from breastfeeding.
However, it’s possible that your baby could pick up the germ that made you sick from another source outside of your breast milk — for example, if baby had a taste of whatever food contained the pathogen.
Regardless, your breast milk can help protect your little one from infection. And if they do get sick, your milk will keep them properly hydrated and nourished.
It can be easy to try to just push yourself through when you’re parenting with food poisoning. But it’s important to take care of yourself, too.
Additionally, you’ll want to be sure to take some steps to minimize passing an infection onto your baby or other children.
Here are some tips for getting through food poisoning while breastfeeding:
- Stay hydrated. Dehydration is the biggest concern when it comes to food poisoning. Even if you can’t keep food down, it’s important to continue drinking plenty of water. Consider adding some fluids meant to replenish and balance your electrolytes, too.
- Avoid Pepto Bismol. Products with oral rehydration salts are compatible with breastfeeding. However, products containing bismuth subsalicylate compounds, like Pepto Bismol, may not be safe.
- Seek medical attention. If your symptoms are lasting more than 1 or 2 days, you have a persistent fever, or you’re severely dehydrated, seek medical attention. In some cases, your doctor may prescribe medication to help your symptoms or to treat the infection.
- Ask a doctor about medication. If you’re unsure whether a product, medication, or antibiotic used to treat food poisoning is compatible with breastfeeding, talk with your doctor.
 You can also check the LactMed database, where you can find information about different substances and medications as well as their impact on breastfeeding.
You can also check the LactMed database, where you can find information about different substances and medications as well as their impact on breastfeeding. - Wash your hands frequently. Over the course of your illness, wash your hands frequently with soap and water after using the toilet and after vomiting. Give your hands an extra wash before holding or nursing your baby.
- Minimize risk to others. Consider sanitizing any high touch surfaces like door handles, light switches, and toilet handles. Clean food prep areas well. Additionally, make sure that anything your baby touches or puts into their mouth — such as pacifiers, nipples, and teethers — have been thoroughly cleaned.
Remember, it’s important to take care of you so you can take care of your baby.
Most food poisoning symptoms — which can include nausea, vomiting, diarrhea, and stomachache — resolve within 1 or 2 days and don’t require medical attention.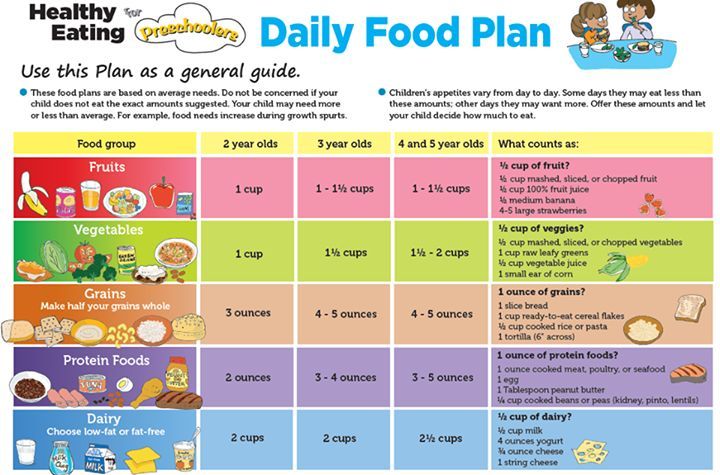
However, visit a healthcare professional if you experience any of the following symptoms:
- bloody diarrhea
- high fever of over 102°F (38.8°C)
- inability to keep fluids down
- dehydration
- diarrhea that lasts for 3 or more days
Food poisoning is linked to a food or drink you ingested that was contaminated. The main symptoms of food poisoning are gastrointestinal — such as vomiting, diarrhea, and upset stomach.
Respiratory symptoms such as coughing, sneezing, or congestion are usually not caused by food poisoning.
However, food poisoning can sometimes cause fever. If you’re unsure if you’re experiencing food poisoning or something else, consult with your doctor.
It’s never fun getting sick, and you might worry about what food poisoning in particular means for you as a breastfeeding or chestfeeding parent.
The good news is, you can — and should — continue breastfeeding your baby even if you get food poisoning.
Your breast milk should not give your baby food poisoning, and in fact, it can help protect them from contracting the germ that caused the food poisoning.
If you have any questions about a food-borne illness while breastfeeding, talk with your child’s pediatrician. And if you or your baby have severe symptoms or become severely dehydrated, seek emergency medical care.
Treatment of food poisoning in a child
Food poisoning is an acute infectious-toxic pathology. It occurs when eating poor-quality products that contain pathogens, toxic substances and poisons. The main manifestations are diarrhea, vomiting, fever, signs of dehydration and severe intoxication. The task of treatment is to quickly stop the symptoms of poisoning, replenish fluid deficiency, and prevent the development of complications.
Class
Food poisoning is referred to as toxic infection or intoxication. Pathology develops after the use of low-quality food, water, plant, chemical or medicinal toxic substances.
There are two types of food poisoning in children:
- Infectious. The causative agents are microbes and their toxic waste products.
- Non-infectious. Caused by toxic substances of plant, animal origin, toxic impurities.
The asymptomatic or latent stage of food poisoning begins from the moment the toxins enter the body until the first symptoms appear. The duration depends on the individual characteristics and age of the child, the amount and rate of absorption of poisons. This stage is most favorable for therapy, since toxic substances have not yet penetrated into the blood.
The toxicogenic stage begins with the appearance of the first symptoms of poisoning and lasts until bacteria and poisons are completely eliminated from the body. This period is characterized by the manifestation of all symptoms of poisoning. In order for the treatment to be effective, it is necessary to identify toxins and accelerate the process of elimination.
At the last stage of convalescence, the disturbed functions of the organs of the digestive, excretory, and immune systems are restored.
Causes
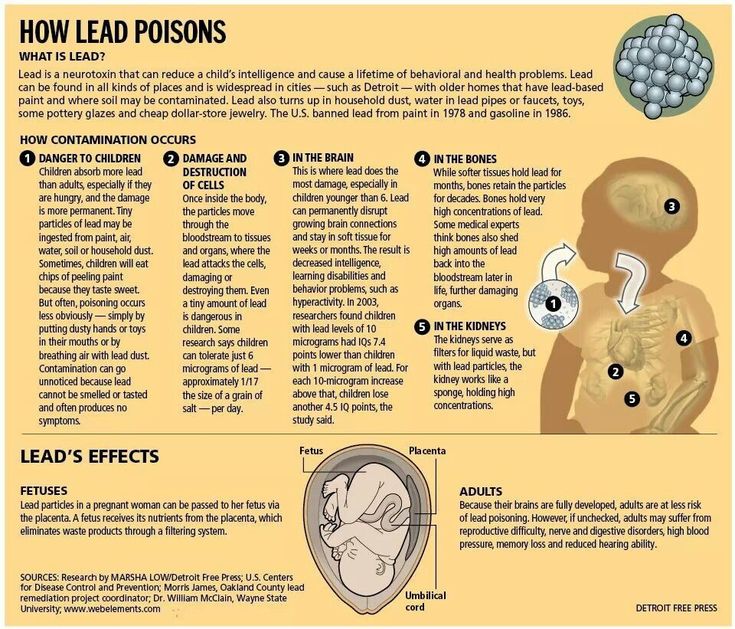
Food poisoning is one of the most common problems in pediatrics. In children, intoxication is more severe than in adults. This is due to the characteristics of the child's body: low acidity of gastric juice, incompletely formed intestinal microflora, rapid absorption of poisons and the spread of toxins throughout the body.
The main causative agents of food poisoning in children are staphylococci, proteus, klebsiella, enterotoxigenic strains of E. coli, clostridia. Pathogens enter the body only with food, in which they multiply, release toxins.
Causes of violation of food quality:
- non-compliance with sanitary and hygienic standards;
- violation of the rules for storage, preparation and sale of food products;
- contamination of food by people with intestinal infections, purulent pathologies - tonsillitis, furunculosis, panaritium, mastitis, streptoderma;
- contamination of soil and plants by animal feces.
Spoiled products may have an unpleasant taste, smell, uncharacteristic texture, but often organoleptic indicators remain within the normal range.
Non-infectious poisoning - a consequence of accidental consumption of poisonous berries or plants, mushrooms. Intoxication can occur after eating agricultural products that are contaminated with poisonous fungicides, insecticides.
Which products are classified as potentially hazardous?
In children, food poisoning often occurs after drinking unboiled water, missing milk or dairy products.
Dangerous products include:
- eggs;
- cream confectionery;
- fish and seafood;
- sausages;
- meat, vegetable preserves;
- mushrooms.
Food poisoning is most often diagnosed in summer and autumn. During this period, the conditions for the reproduction of microbial pathogens are the most favorable.
Symptoms of food poisoning in a child
Despite the variety of toxic infections, clinical manifestations are largely similar. The latent stage lasts an average of 2-6 hours, sometimes no more than 30 minutes or more than a day. Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
The latent stage lasts an average of 2-6 hours, sometimes no more than 30 minutes or more than a day. Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
Poisoning always begins acutely - nausea, repeated vomiting with particles of undigested food. The child complains of abdominal pain, watery stools, mucous membranes, green impurities, blood streaks. Bowel emptying occurs up to 5-10 times a day.
Simultaneously with dyspeptic disorders, the temperature rises to 38–39 degrees. Signs of intoxication quickly increase: refusal to eat, headache and muscle pain. Symptoms of dehydration appear: the skin is pale and dry, facial features are sharpened, the number of urination decreases, the mucous membranes dry out. In infants, the fontanel sinks. With food poisoning, convulsions often occur, acidosis develops.
In most cases, signs of poisoning gradually disappear after 2-3 days, but weakness and abdominal pain may persist for several weeks.
Severe forms of food poisoning are predominantly observed in young children with weakened immunity. The risk of developing complications against the background of intoxication increases with prematurity, malnutrition and dysbacteriosis in history.
If a child is poisoned by poisonous plants, berries, lesions of the central nervous system are observed:
- retardation of reactions;
- euphoria;
- hallucinations;
- impaired speech, vision;
- convulsions.
If the cardiovascular system is damaged by toxins, the heart rate speeds up or slows down, blood pressure decreases.
Mushroom poisoning is very dangerous for children. After eating a pale toadstool, indomitable vomiting, cholera-like diarrhea with impurities of blood in the feces begins. Other symptoms are intestinal colic, respiratory disorders, convulsions. Toxins adversely affect the liver, which leads to the development of toxic hepatitis. AT 90% of cases are fatal due to acute liver failure.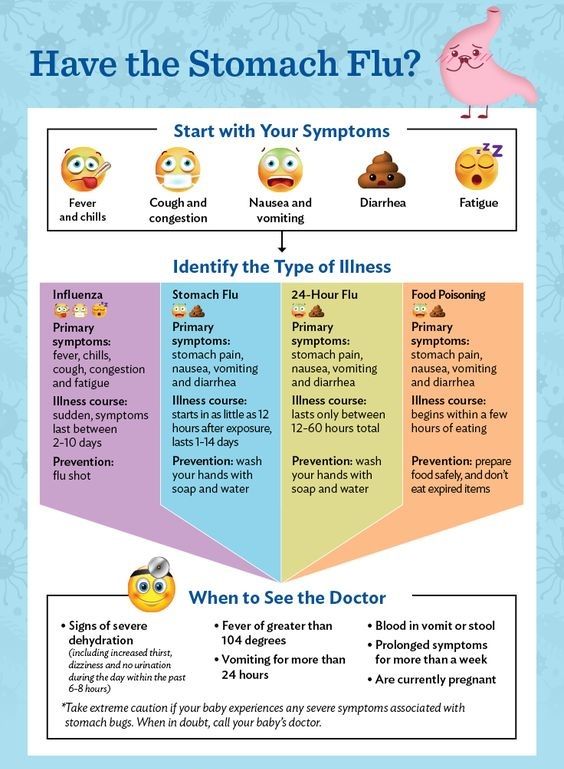
Signs of fly agaric poisoning are increased salivation, shortness of breath, severe vomiting, convulsions, bronchospasm, hallucinations, nystagmus or strabismus. But the mortality rate is less than 1%.
Botulism develops when poor-quality canned food is consumed. The toxin affects the nervous system, which manifests itself in the form of paralysis and paresis. Poisoning in children can cause the development of acute respiratory failure, heart rhythm disturbances. The first symptoms appear after 4-6 hours. Worries about pain in the epigastric region, nausea, vomiting, diarrhea. Sometimes there are problems with vision. When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops.
First aid for child poisoning
Act immediately. First aid rules:
- In case of poisoning with mushrooms, berries, medicines, induce vomiting.
- Gastric lavage with clean water to remove toxins from the intestines.
 Babies should not do the washing themselves, as the child can inhale the vomit. Instead, you can do a cleansing enema. The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg.
Babies should not do the washing themselves, as the child can inhale the vomit. Instead, you can do a cleansing enema. The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg. - Taking enterosorbents - these drugs collect toxins in the intestinal lumen, remove them with feces.
- More to drink. You need to drink in small portions, but often. You can give your child water with a weak saline solution, weak tea, mineral water without gas.
- Call a doctor.
Timely first aid will help to avoid the development of complications of poisoning.
In case of poisoning, children should not:
- give painkillers, drugs, drugs for vomiting and diarrhea;
- apply hot or cold compresses to the abdomen;
- use soda to induce vomiting, potassium permanganate to wash the stomach;
- give milk and dairy products.
Diagnosis of food poisoning in a child
Diagnosis of food poisoning in a child can be done by a pediatrician or an infectious disease specialist. The examination begins with the collection of anamnesis, examination of the patient.
The examination begins with the collection of anamnesis, examination of the patient.
Specific diagnostic tests are prescribed to isolate the pathogen. Biomaterial - feces and vomit, gastric lavage, the remains of contaminated food. With a generalized form of infection, a blood culture is prescribed. Auxiliary methods - RIF, PCR, ELISA. Additionally, you may need to consult a neurologist, gastroenterologist, surgeon.
Be sure to carry out differential diagnosis to exclude acute gastritis, cholecystitis, pancreatitis, giardiasis, acute intestinal infection, inflammation of the appendix, meningitis. A blood test is prescribed to rule out a viral, bacterial infection, a stool test to detect infections caused by pathological bacteria.
How to treat
Treatment of poisoning in a child begins with the elimination of signs of dehydration. Apply oral, parenteral rehydration therapy.
Auxiliaries:
- enzymes;
- sorbents;
- prebiotics to restore the balance of intestinal microflora;
- antimicrobials are necessary for severe toxic infection.

In case of toadstool poisoning, emergency hemosorption is performed to cleanse the blood of toxins.
Diet for child poisoning
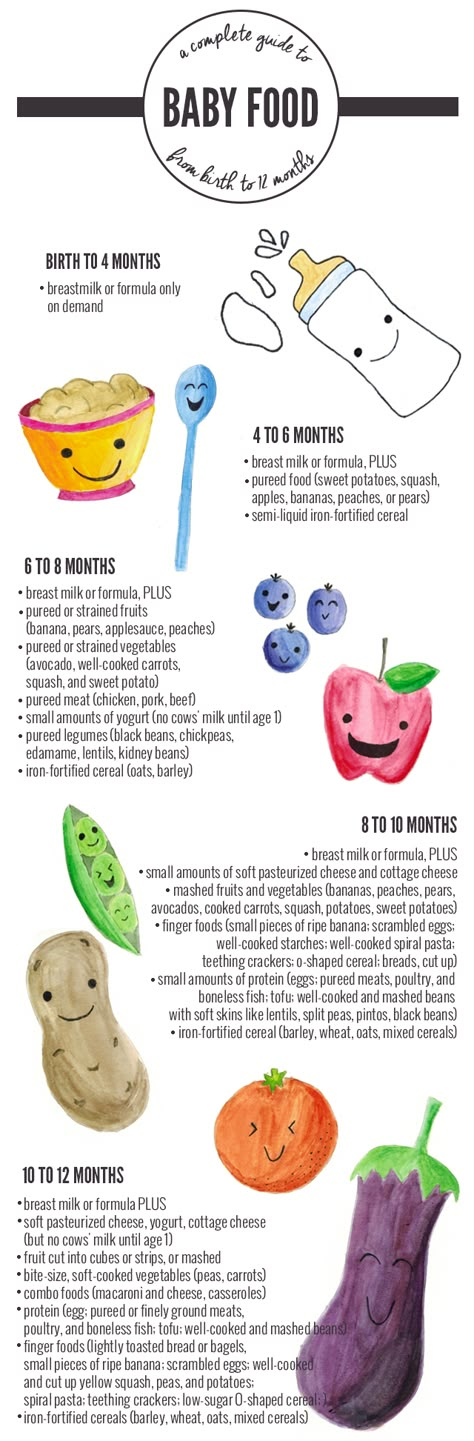
It is best not to feed the child for 12-24 hours after poisoning. When vomiting stops, a sparing diet is indicated. Breastfed babies under one year of age need to skip a few feedings.
How to feed a child after poisoning:
- liquid porridge - rice, buckwheat, cooked in a mixture of equal amounts of water and milk;
- slimy soups;
- crackers;
- kefir;
- compotes;
- after a few days - vegetable puree, children's cottage cheese or kefir, yogurt without additives;
- gradually introduce meat and fish soufflé into the menu.
List of prohibited products - pastries, whole milk, black bread, fresh white bread. You can not give your child pasta, chocolate, ice cream, chips, sweet carbonated drinks, wheat and barley porridge. From vegetables, cucumbers, tomatoes, cabbage are contraindicated.
The duration of the diet is 14 days.
Possible consequences of food poisoning in a child
Complications occur in case of severe poisoning, lack of correct and timely therapy.
Possible effects:
- dysbacteriosis;
- renal and hepatic insufficiency;
- disturbances in the functioning of the nervous and immune systems;
- chronic diseases of the gastrointestinal tract.
Prognosis and prevention
Poisoning in a child of mild and moderate severity ends in complete recovery.
Methods of prevention:
- properly store food, observe the temperature regime and other storage conditions;
- observe the rules of heat treatment, children should absolutely not be given raw fish, poorly fried meat;
- drink only boiled, purified water, do not swallow water when swimming in reservoirs;
- wash hands, vegetables and fruits thoroughly;
- store medicines, chemicals out of the reach of children;
- to tell children about poisonous mushrooms, berries, plants, the dangers of their use.
.jpg)
People who work in the kitchen in children's institutions should have regular medical check-ups. In the presence of pustular skin pathologies, respiratory diseases, signs of an intestinal infection, the worker is not allowed into the catering unit.
Treatment of food poisoning in Moscow
Food poisoning in a child is a dangerous condition, you should not self-medicate, you should immediately consult a doctor. Call our clinic, describe the symptoms, the patient's condition, the possible cause of the poisoning. The administrator of the "Miracle Doctor" center will write you to the doctor in the near future.
Q&A
Why is acute poisoning dangerous for a child?
Fever, vomiting more often 3–5 times, diarrhea in a child is a reason to immediately call an ambulance.
Poisoning in a child at any age leads to a breakdown of the immune system. Dehydration is very dangerous for babies. In children under 4 years of age with profuse vomiting and loose stools, the critical phase of dehydration can occur within a few hours.
How to give water to a baby if he vomits very often?
Even if the vomiting is severe and persistent, the child must be given water. The consequences of dehydration are extremely dangerous for the child's body. You need to water the child in small portions - 1 tsp each. every 5 minutes. Water should not be cold, so as not to cause spasm and vomiting. The optimal temperature is a few degrees above body temperature.
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- А
- Б
- В
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- Й
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Ю
- Я
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- case studies
- Questions and answers
- Speeches
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Salmonella (non-typhoid)
- Salmonella is one of the four main causes of diarrheal disease worldwide.
- Most cases of salmonellosis are mild; however, sometimes salmonellosis can be life threatening. The severity of the disease depends on host-related factors and Salmonella serotype.
- Antimicrobial resistance is a public health concern worldwide and Salmonella is among the microorganisms that have developed a number of resistant serotypes found in the food chain.
- As a preventive measure against salmonellosis, it is recommended that basic food hygiene practices be followed, such as thorough cooking.
- The bacterium Salmonella is widespread in domestic and wild animals, mainly in animals used for food, such as poultry, pigs and cattle; as well as among domestic animals, including cats, dogs, birds, and reptiles such as turtles.

- Salmonella can pass through the entire food chain, from animal feed, through primary production, to the home or food service establishments.
- Humans become infected with salmonellosis usually through consumption of contaminated food of animal origin (mainly eggs, meat, poultry and milk), although other foods, including manure-contaminated green vegetables, may be implicated in transmission.
- Human-to-human transmission by the fecal-oral route can also occur.
- Human cases also occur through contact with infected animals, including pets. Infected animals often show no signs of the disease.
- Ensure food is properly cooked and still hot when served.
- Avoid raw milk and products made from raw milk. Drink only pasteurized or boiled milk.
- Avoid ice unless it has been made from safe water.
- If there is any doubt about the safety of the water, boil it or, if this is not possible, disinfect it with a reliable, slow-acting disinfectant (usually available from pharmacies).

- Wash hands thoroughly and use soap frequently, especially after contact with pets or farm animals, and after going to the toilet.
- Wash fruits and vegetables thoroughly, especially if consumed raw. If possible, remove the skin from vegetables and fruits.
- Guide to safe food for tourists
- Food processors and food processors, whether professional or at home, should be vigilant in food preparation and practice good hygiene practices regarding food preparation.
- Professional food handlers who develop a fever, diarrhea, vomiting, or visibly infected skin lesions should report this to their employer immediately.
- The WHO Five Essentials for Safer Eating serves as the basis for educational programs to train food handlers and preparers and to educate consumers. These principles are especially important for preventing food poisoning.
 These five principles are as follows:
These five principles are as follows: - The Five Essential Principles of Safe Food
- Practice good personal hygiene.
- Protect fields from animal faeces.
- Use treated faeces.
- Assess and manage the risks posed by irrigation water.
- Keep harvest and storage equipment clean and dry.
- Five Essential Principles for Growing Safer Fruits and Vegetables
- Practice good personal hygiene.

- Keep the pond clean.
- Monitor water quality.
- Keep your fish healthy.
- Use clean equipment and containers to collect fish.
- Five Essential Principles for Improving Aquaculture Product Safety for Public Health
WHO/c. Doan
Doan
© Photo
","datePublished":"2018-02-20T08:31:00.0000000+00:00","image":"https://cdn.who.int/media/images/default-source/imported/ chicken-food-vietnam.jpg?sfvrsn=7fbf11eb_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":" ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2018-02- 20T08:31:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/salmonella-(non-typhoidal)","@context ":"http://schema.org","@type":"Article"};
Key facts
Overview
The burden of foodborne disease is significant, with almost one in ten people falling ill each year, resulting in the loss of 33 million healthy life years. Foodborne illness can be severe, especially in young children. Diarrheal diseases are the most common diseases caused by unhealthy food. They affect 550 million people every year, including 220 million children under 5 years of age. Salmonella is one of the four leading causes of diarrheal disease worldwide.
Salmonella is a genus of Gram-negative, rod-shaped bacteria belonging to the Enterobacteriaceae family. To date, within two species - Salmonella bongori and Samonella enterica - more than 2500 different serotypes or "serovars" have been identified. Salmonella is a ubiquitous and persistent bacterium that can survive for weeks in a dry environment and several months in water.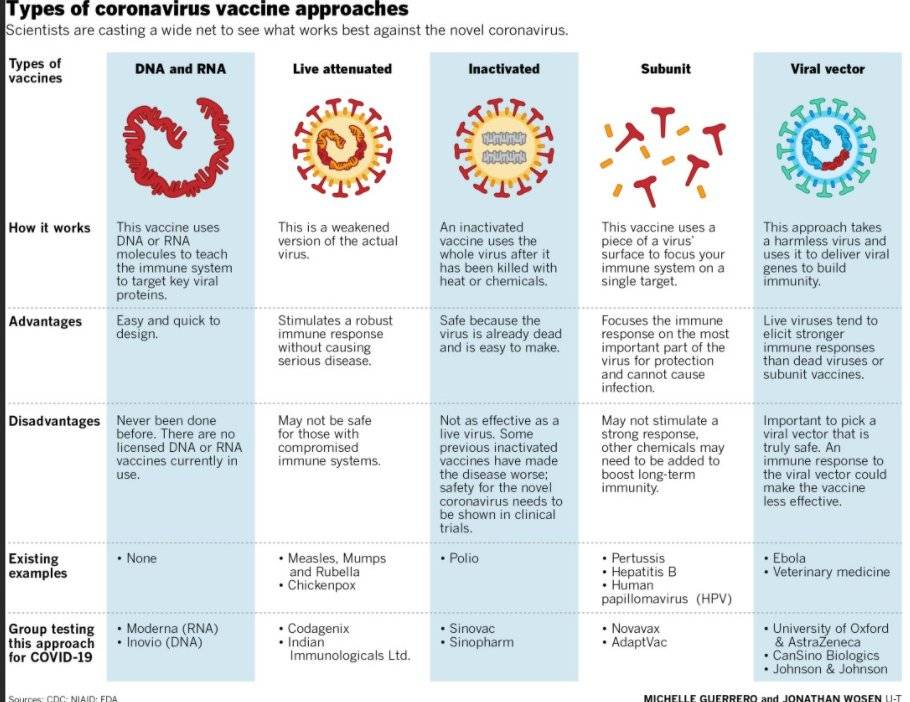
Although all serotypes can cause disease in humans, some are host-specific and can only live in one or a few animal species: for example, the Dublin Salmonella enterica serotype lives in cattle, and the Choleraesuis Salmonella enterica serotype lives in cattle. in pigs. When these particular serotypes cause disease in humans, the disease is often invasive and can be life-threatening.
However, most serotypes are present in a wide range of carriers. These serotypes commonly cause gastroenteritis, which is often uncomplicated and does not require treatment, but can be severe in children, the elderly, and immunocompromised patients. This group includes the serotype Enteritidis Salmonella enterica and serotype Typhimurium Salmonella enterica are the two most important Salmonella serotypes transmitted from animals to humans in most regions of the world.
Disease
Salmonellosis is a disease caused by the bacterium Salmonella .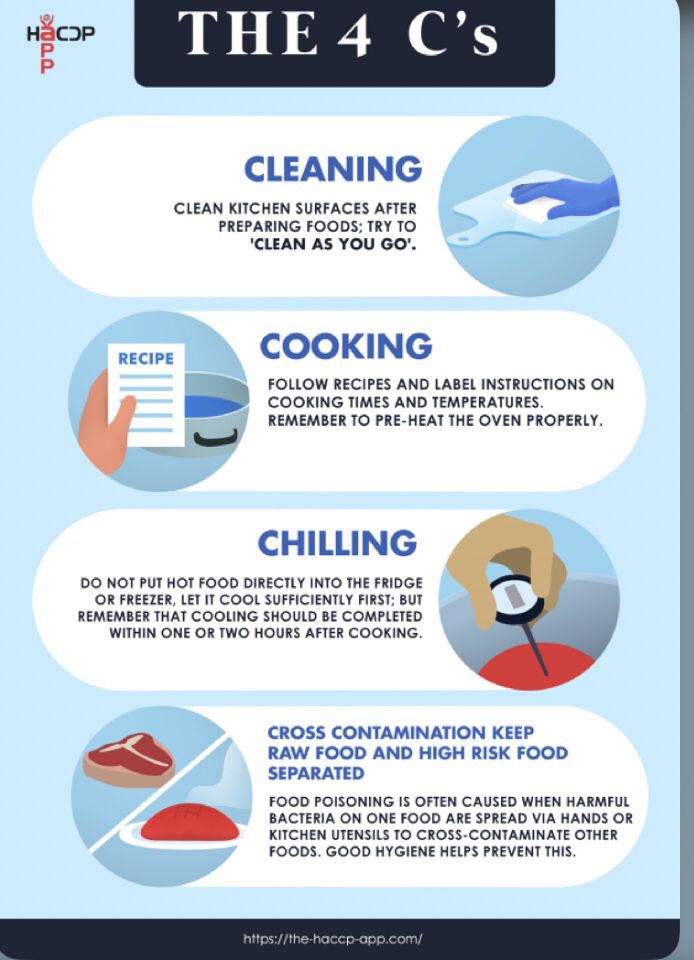 It is usually characterized by a sudden increase in temperature, pain in the abdomen, diarrhea, nausea, and sometimes vomiting.
It is usually characterized by a sudden increase in temperature, pain in the abdomen, diarrhea, nausea, and sometimes vomiting.
Disease symptoms appear 6-72 hours (usually 12-36 hours) after ingestion of Salmonella and the illness lasts 2 to 7 days.
Symptoms of salmonellosis are relatively mild, and in most cases, patients recover without special treatment. However, in some cases, especially in children and elderly patients, disease-related dehydration can become severe and life-threatening.
Although large outbreaks of Salmonella usually receive media attention, 60 to 80% of all Salmonella cases are not reported in known outbreaks. Such cases of the disease are classified as sporadic or not diagnosed at all as such.
Sources and transmission of infection
Treatment
In severe cases, treatment consists of electrolyte replacement (to ensure the body receives electrolytes such as sodium, potassium and chloride ions excreted with vomiting and diarrhea) and rehydration.
For mild or moderate disease in healthy individuals, conventional antimicrobial therapy is not recommended. This is because antimicrobials may not completely eradicate the bacterium and encourage the selection of resistant strains, which may subsequently cause the drug to become ineffective. .
This is because antimicrobials may not completely eradicate the bacterium and encourage the selection of resistant strains, which may subsequently cause the drug to become ineffective. .
However, risk groups such as infants, the elderly, and immunocompromised patients may need antimicrobial treatment. Antimicrobials are also commonly prescribed when the infection has spread from the intestines to other parts of the body.
Due to the global increase in antimicrobial resistance, treatment guidelines need to be reviewed regularly, taking into account the bacterial resistance model, taking into account data from the local surveillance system
Methods of prevention
Prevention requires control measures in all parts of the food chain, from agricultural production to food processing, production and preparation, both in commercial organizations and in the home.
Preventive measures to protect against Salmonella in the home are similar to those taken to protect against other bacterial foodborne diseases (see "Guidelines for food handlers and preparers" below).
Contact between infants or young children and pets (cats, dogs, turtles, etc.) that may be carriers of Salmonella should be closely monitored.
National and regional foodborne disease surveillance systems are important tools for studying and monitoring the situation of foodborne diseases, as well as for detecting and responding to salmonellosis and other intestinal infections at an early stage, thus preventing the further spread of such diseases.
Advice for the public and travelers
The following tips will help you stay safe while traveling:
Advice for food processors and preparers
WHO has made the following recommendations for food processors and food processors:
Recommendations for fruit, vegetable and fish producers
The WHO brochures Five Keys to Growing Safer Fruits and Vegetables: Improving Health through Microbial Contamination and Five Keys to Safer Aquaculture for Public Health introduce agricultural workers, including small-scale farmers growing fresh fruits and vegetables and fish for themselves, their families and for sale in local markets, with key practices to prevent microbial contamination.
The five essential principles for growing safer fruits and vegetables are:
“Five Essential Principles for Improving Aquaculture Safety for Public Health”
WHO activities
In collaboration with other stakeholders, WHO strongly advocates the important role of food safety as a key element in ensuring access to a safe and nutritious diet. WHO develops policies and recommendations that span the entire food chain from production to consumption, drawing on different types of expertise and experience in a wide range of areas.
WHO is working to strengthen food safety systems in an increasingly globalized world. Setting international food safety standards, improving disease surveillance, educating consumers and training food handlers in the safe handling of food are among the most important ways to prevent foodborne illness.
WHO is strengthening the capacity of national and regional laboratories for surveillance of foodborne pathogens such as Campylobacter and Salmonella .