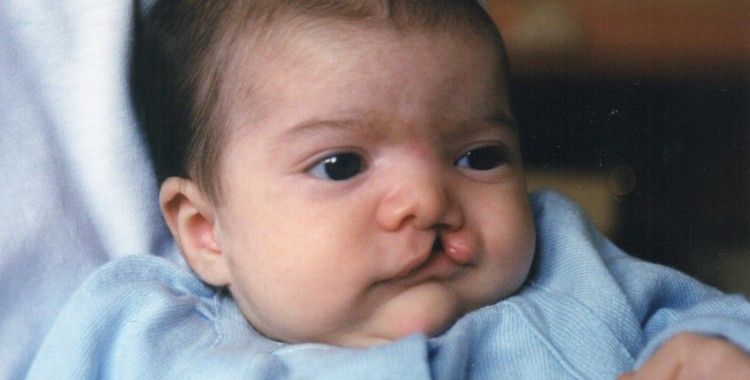
Cleft lip baby feeding
Cleft lip and palate – infant feeding
To feed well, babies need to position their lips and tongue around the nipple or artificial teat, and create both suction and compression during sucking.
Sucking is more difficult when a baby is born with a cleft palate or combined cleft lip and cleft palate. There are a number of ways to help these babies feed well, including the use of specially designed bottles and teats.
To learn more about cleft lip and cleft palate, read our fact sheet Cleft lip and cleft palate.
Feeding your baby
Your cleft coordinator, speech pathologist or Maternal and Child Health Nurse will be able to help show you what it should look like when your baby is feeding properly. Signs that your baby is feeding well are that they have five or six wet nappies per day, regular bowel motions and they are healthy and alert.
Feeding with a cleft lip
Babies born with a cleft lip alone usually feed well. Some babies breastfeed better with the cleft facing upwards. The breast tissue usually fills the gap where the cleft is and allows efficient feeding. Some bottle-fed babies feed better on a wide-based teat.
Feeding with a cleft palate
Babies with cleft palate often look like they are feeding well, because the lips and tongue close around the nipple or artificial teat like non-cleft babies and the jaw moves well during sucking.
However, most babies with cleft palate cannot generate suction during feeding. This is because air leaks from the mouth through the cleft into the nose during feeding. The lack of suction makes it difficult – and for some babies, impossible – to breastfeed or drink from a bottle efficiently. This means that feeding can take a long time and is tiring for your baby, who may not get enough milk to grow and develop well.
Feeding with a cleft lip and palate
Babies with cleft palate can't create enough suction during feeding to draw milk from the breast or bottle easily. If your baby also has a cleft lip, they may not be able to compress the breast or teat well enough to push milk from the breast or bottle.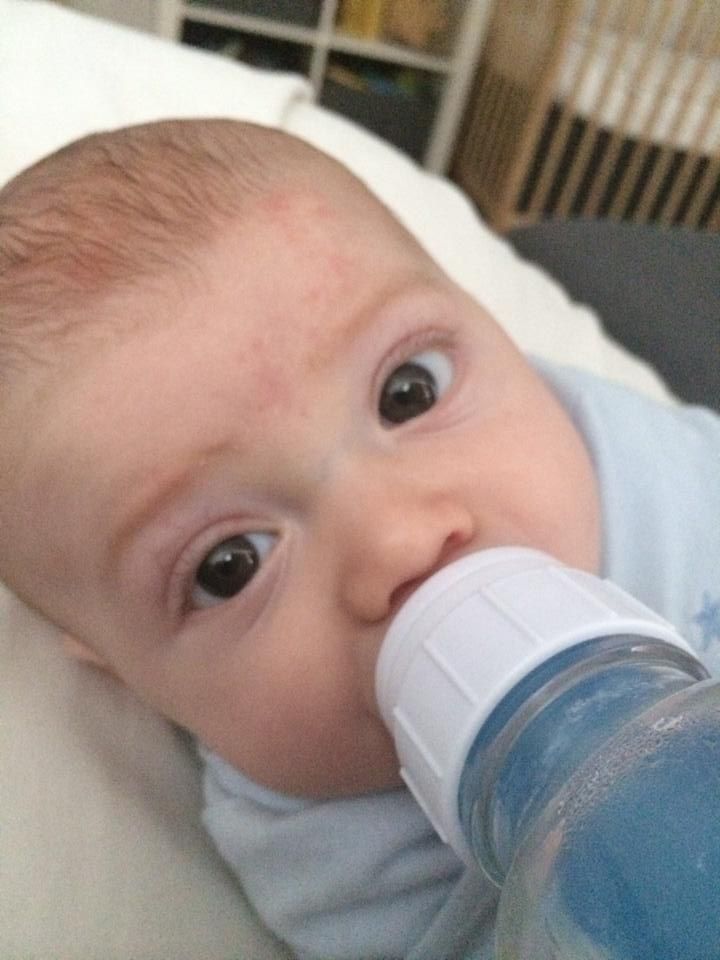 In either case, feeding is usually slow
and tiring, and your baby may not drink enough to grow well.
In either case, feeding is usually slow
and tiring, and your baby may not drink enough to grow well.
Feeding options
Breastfeeding
If your baby can't feed well directly from the breast, you may choose to feed your baby expressed breastmilk (EBM) from a bottle. Lactation consultants and Maternal and Child Health Nurses are able to provide advice and support to new mothers who wish to express breastmilk for their baby.
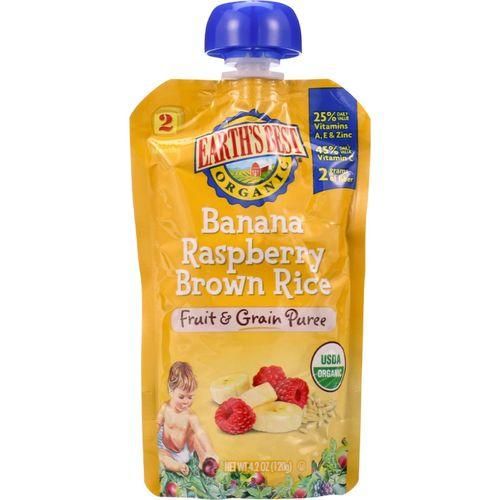
Bottle feeding
For babies with a cleft lip only, there is no need to use special equipment if your baby feeds well from a standard teat or bottle bought from a supermarket or pharmacy. But if your baby has a cleft palate or cleft lip and palate they generally cannot generate suction and/or compression during feeding, therefore they will need a specialised cleft bottle to feed. There are a number of special teats and bottles available. Bottles and
teats that can be squeezed while your baby is sucking compensates for a lack of suction.
Your cleft coordinator can show you the different bottles and teats available and demonstrate how to use them. Some commonly used teats and bottles include:
- The SpecialNeeds® Feeder: Previously known as the Haberman feeder, this has a long narrow teat which is squeezed during feeding to release milk into the baby's mouth. The teat has a 'slit' cut and allows slow, medium or fast flow depending on the orientation of the slit during feeding. The teat also has a one-way valve to minimise swallowing of air, and maximise response to compression.
- Dr Brown's Specialised Feeding System: The Dr Brown bottle has three critical elements to ensure the functionality of the speciality feeding system. A one way infant paced feeding valve. Internal vent system creating the vacuum-free feeding experience. Consistent and reliable teat flow rates. Unique one way valve means no manual assistance is required for feeding.
- Queensland CleftPALS Bottle: This is a soft polythene bottle made by Queensland CleftPALS Inc.
 It works well with a number of different teats and is gently squeezed during feeding to assist the baby in receiving milk.
It works well with a number of different teats and is gently squeezed during feeding to assist the baby in receiving milk. - Pigeon Cleft Teat: This is an isoprene rubber teat that can be used with a squeeze bottle or a normal rigid bottle. It comes with a plastic regulator that can be inserted into the teat to assist with milk flow. The thicker part of the teat must be facing upwards (towards the roof of the mouth) for efficient feeding.
- Chu Chu Easy Feed Teat: This is a silicone rubber teat (nitrosamine free), that can be used with a squeeze bottle or normal bottle. When feeding, ensure the flat part of the teat is facing upwards (towards the roof of the mouth).
- Chu Chu Cross-cut Teat: This is an isoprene rubber teat (nitrosamine free) that can be used with a squeeze bottle or normal bottle. It has a cross-cut in the top, which stops milk dripping into the baby's mouth when they have stopped for a rest during a feed.

See the end of this fact sheet for details on where to get these teats and bottles.
Feeding tips
Each baby is unique, so different techniques will suit different babies, even if they have the same kind of cleft. However, some general tips are:
- Feed your baby in a calm quiet environment. Make sure you are sitting in a comfortable chair.
- Have several breaks for burping, as your baby may experience a lot of wind.
- Keep each feed to 20–30 minutes. Longer feeds mean your baby will use too much energy during feeding.
- Seat your baby fairly upright for bottle feeding (see diagram below). This may prevent milk coming out of your baby's nose during sucking. Hold your baby close to you so they are well supported during feeding.
- If your baby has a cleft lip, avoid placing the teat into the cleft.
- Once your baby starts sucking, squeeze the bottle gently to deliver milk into the mouth.
 If you are using the SpecialNeeds Feeder, the teat rather than the bottle should be squeezed. A squeeze every three to four sucks is usually enough.
If you are using the SpecialNeeds Feeder, the teat rather than the bottle should be squeezed. A squeeze every three to four sucks is usually enough. - Some parents find it helpful to practise squeezing a water-filled bottle to get an idea of how the flow changes with more rapid squeezing or stronger squeezing of the bottle.
- Watch how your baby reacts to the pulsing or prolonged squeezing of the bottle. If they look uncomfortable or are not managing the mouthful of milk, stop squeezing and let your baby rest and swallow before more milk is given.
- Some babies have serious feeding problems (dysphagia), which mean they need specialised help to manage feeding. If your baby is showing signs of swallowing difficulties, talk to your child's doctor or cleft coordinator.
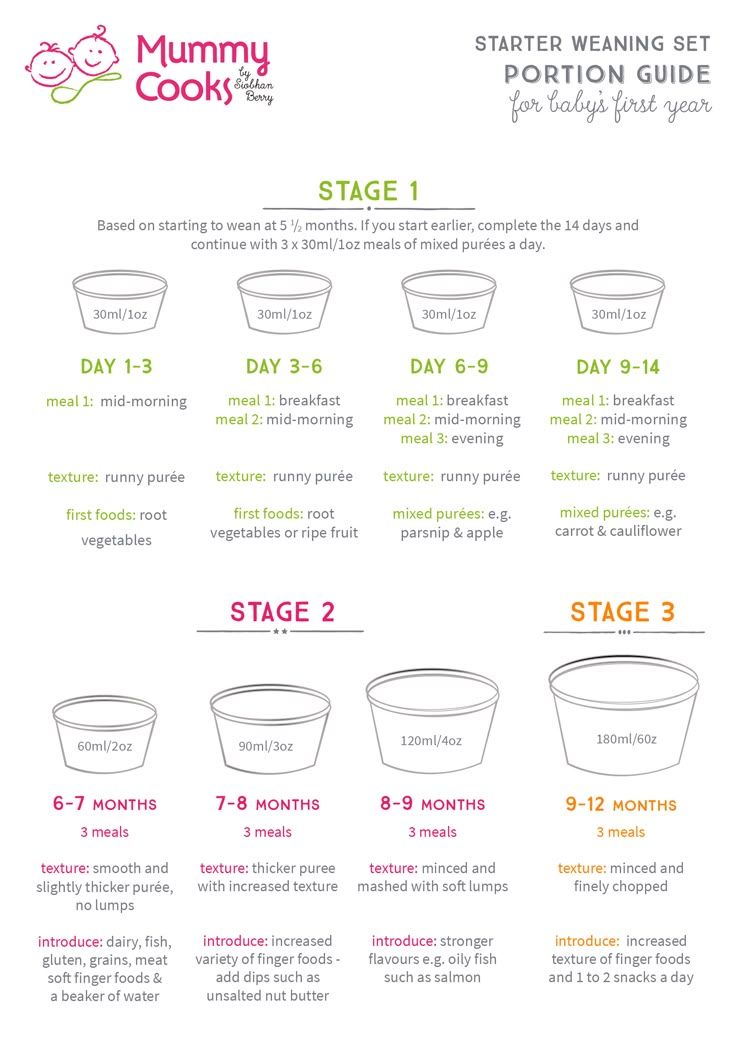
Introducing solids
Babies with cleft lip, cleft palate or cleft lip and palate usually start taking solids at the same time as other babies (between four to six months of age).
Sometimes food may come out through your baby's nose during feeding. This may improve if you sit your baby more upright or make the food a little runnier. If problems persist, you can contact your speech pathologist for advice.
Feeding your baby after cleft lip or cleft palate repair
Your plastic surgeon will give specific instructions on how to feed your child in the first few days after the surgery. In general, babies are encouraged to return to their usual method of feeding (breastfeeding or bottle feeding) after surgery. If the baby has progressed to solids, these can also be reintroduced quite quickly after palate repair surgery. The food should be a soft, sloppy consistency for the first three weeks.
For more information
- Kids Health Info fact sheet: Cleft lip and cleft palate
- The Royal Children's Hospital: Cleft lip booklet
- The Royal Children's Hospital: Cleft palate booklet
- The Royal Children's Hospital: Cleft lip and palate: Infant feeding booklet
- The Royal Children's Hospital: Department of Plastic and Maxillofacial Surgery
- The Royal Children's Hospital: Department of Speech Therapy
- Parent support group: CleftPALS Victoria, ph 0425 784 130 (general support)
- See your cleft coordinator or GP.

Where to get equipment
You can get specialist bottles and teats from:
- The Royal Children's Hospital Equipment Distribution Centre, ph. (03) 9345 5325
- CleftPALS Victoria, ph. 0425 784 136 (feeding and equipment)
- Your local pharmacy (although you may need to make a special order)
Common questions our doctors are asked
How do I know if my baby is not feeding properly?
Newborn babies can lose up to 10 per cent of their birth weight, but usually regain it in two to three weeks. If your baby is having five or six wet nappies per day, regular bowel motions and is healthy and alert, then it is likely that they are feeding well. Slow weight gain or
weight loss may mean the feeding method needs to be changed. If you are worried about your baby's feeding, talk to your GP, cleft coordinator or Maternal Child and Health Nurse.
Developed by The Royal Children's Hospital Speech Pathology and Plastic and Maxillofacial Surgery departments.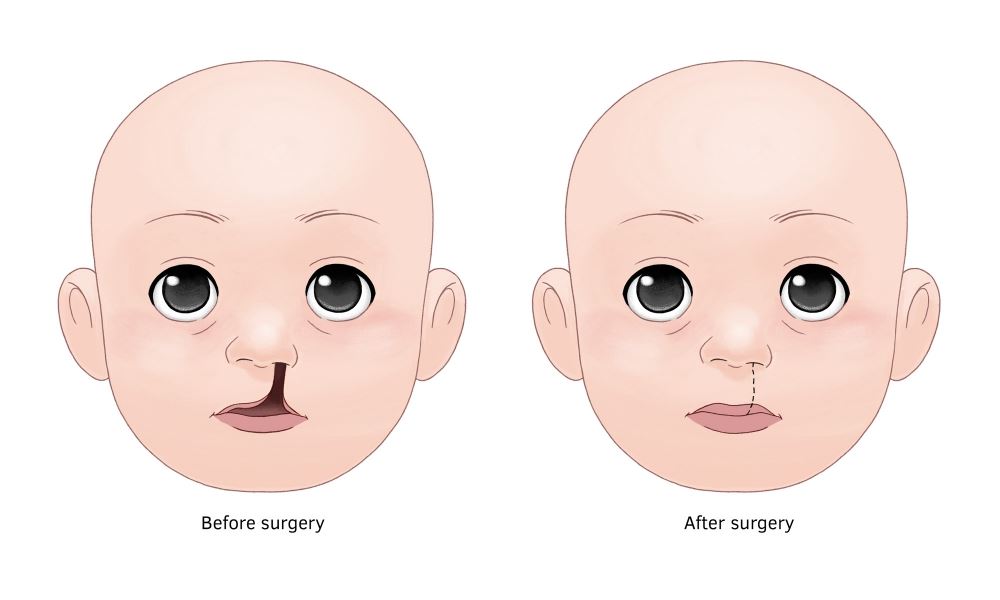 We acknowledge the input of RCH consumers and carers.
We acknowledge the input of RCH consumers and carers.
Reviewed August 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
Feeding a Child with a Cleft Lip or Cleft Palate - Pediatric Cleft and Craniofacial Center - Golisano Children's Hospital
Golisano Children's Hospital / / Feeding a Child with Cleft Lip
Babies born with cleft lip and palate, like any other babies, need to learn how to feed successfully in order to thrive and grow. If the baby has a cleft lip only (with a normal palate), he/she should be able to eat normally using standard techniques. Babies with cleft lip only can even breastfeed, if you desire.
However, babies born with a cleft lip and palate, or cleft palate only, have an opening in the roof of their mouth- between the mouth and nose. This opening in the palate makes it difficult to create the suction needed to pull milk out of the bottle or to latch on to the breast to breastfeed. This means that babies with cleft palate are at risk for poor weight gain because they use a lot of energy to feed.
This opening in the palate makes it difficult to create the suction needed to pull milk out of the bottle or to latch on to the breast to breastfeed. This means that babies with cleft palate are at risk for poor weight gain because they use a lot of energy to feed.
Our job is to work with parents and teach them how to feed their baby with a specialized cleft bottle and nipple. Our nurse practitioner, Melisande Ploutz, will see you and your baby weekly until your child is eating well and gaining weight appropriately. Babies should be able to feed comfortably within a reasonable amount of time, without struggling to breathe, choking, or working very hard to get the milk out of the bottle. The feeding goal is to help the baby get the right amount of milk in the right amount of time, and to avoid taking in too much air. Here are some simple guidelines:
- Use a specialized cleft palate bottle as demonstrated by your baby’s medical team.
- Place your baby in an upright, sitting position to prevent the formula from flowing back into the nose area.

- Keep the bottle tilted so the nipple is always filled with milk and pointed down away from the cleft. Your baby will move the nipple into the most comfortable position for him/her.
- As your baby feeds, some milk may escape through the nose. This is very common and expected, and it does not mean the baby is choking. Hold your baby in a more upright position as this will lessen the amount of milk coming through the nose.
- Babies with a cleft need to be burped more often because they take in more air while feeding. Watch for signs of discomfort; your baby will give you signs when it’s time to stop and burp.
How will you know it’s working? Your baby should feed in about 30 minutes or less. Longer feedings can cause exhaustion and burn up too many calories that the baby needs to gain weight.
Secondly, your baby should return to birth weight by about 2 weeks of age and gain between a half an ounce to one ounce per day. This is an average, so be sure to follow the guidelines of your medical team.
This is an average, so be sure to follow the guidelines of your medical team.
Please click here for more information about feeding your baby with a cleft (use link): http://www.cleftline.org/who-we-are/what-we-do/feeding-your-baby/
All of these bottles are available for you at our clinic. Call 585-273-FACE.
- Dr. Brown’s Specialty Feeding System®
- Mead Johnson Cleft Palate Nurser
- Medela SpecialNeeds® Feeder
How to feed a baby before surgery to close a cleft
nutrients.
Babies with only cleft lip without palatal integrity usually have no problems with nipple latch and sucking. Children with cleft lip and palate or one cleft palate require some modification of the feeding method, as they have an abnormal communication between the nasal and oral cavity, which prevents the creation of negative pressure necessary for full sucking. Newborns with a cleft palate must squeeze milk out of the nipple by pinching it between the tongue and the rest of the hard palate and alveolar process of the upper jaw.
When milk is squeezed into the mouth of a child with cleft palate, some of it will go into the nose. In addition, during feeding, more air can enter the stomach than in healthy children. This requires frequent changes in the position of the baby when feeding to ensure regurgitation of air. In the first weeks of life, this swallowing of air can lead to disorders such as colic, regurgitation of food, or even slight vomiting. Usually, the child outgrows all these problems within a few months, as the tone of the stomach muscles increases and the activity of the muscles of the digestive tract is coordinated. If some of these symptoms persist for a long time, contact your pediatrician.
Feeding babies with cleft lip and/or palate
For babies with clefts, as with all newborns, there are two best ways to feed: breastfeeding and bottlefeeding. Cup feeding is not the method of choice, and in the case of normal breastfeeding or bottle feeding, there is no need to resort to this method.
Breastfeeding
There are different opinions about breastfeeding children with clefts. Although it is undeniable that breast milk is the best food for a baby. When a child with a cleft lip or palate is first placed on the breast, there may be some difficulties that are automatically associated with the existence of the cleft. Meanwhile, feeding a baby requires a certain period of trial and error before normal feeding is established.
A baby born with only a cleft lip often has no more difficulty feeding than a baby without a cleft lip, as the breast tends to fill the empty space, adapting and sealing the baby's mouth as much as possible.
Feeding children with perforated cleft lip and palate is also possible if there are no other problems. However, additional patience and modification of feeding technique will be needed to provide the baby with an adequate supply of nutrients, reduce maternal stress, and optimize the baby's responses.
The following tips may be helpful to you.
- Massaging the breast before feeding promotes reflex milk release, which in turn facilitates the flow of milk into the baby's mouth.
Warm compresses applied to the breasts for 20 minutes prior to feeding ensure good blood flow to them.
Frequent breastfeeding (every 2-3 hours) in the first 2 weeks of life is often recommended to establish normal lactation.
Mothers are sometimes advised to increase their fluid intake. - Uses the areola (dark area around the nipple) digital pressure technique to help increase the protrusion of the nipple, making it easier to grab and hold in the baby's mouth. The nipple will enlarge during breastfeeding.
Sometimes the process of feeding is complicated by the appearance of cracks in the nipple. Such cracking may be due to infection or drug therapy. In such cases, to facilitate the feeding of the child, special pads are used to ensure the normal shape of the nipple and alleviate the mother's condition. Subsequently, when the cracks disappear, the nipple will bulge normally.
Subsequently, when the cracks disappear, the nipple will bulge normally. - If, after several attempts, the baby is unable to hold on to the nipple, or if you feel that the baby is not fully satiated, collect the remaining milk with a breast pump and finish feeding this milk from the bottle. In any case, when you are supplementing a baby from a bottle, you should always give the baby the breast first and then the bottle. With gradual adaptation, increasing strength and patience of your baby, the process of breastfeeding can become longer.
Bottle-feeding
It happens that it is not possible to establish normal sucking strength during attachment to the breast, especially in children with bilateral cleft lip and palate, in which the child cannot compensate for the pathological communication between the mouth and nose . In such cases, the only way to obtain breast milk is to bottle feed expressed breast milk. It is advisable to feed the baby with milk expressed using a breast pump for several weeks or, if possible, longer. Even when your baby has been breastfed but breastfeeding has been delayed due to surgery or other reasons, you can bottle feed your baby with expressed milk until you can return to normal breastfeeding. In addition, there are currently ways to harvest breast milk for a certain period. Questions about how and when to store milk should be discussed with your pediatrician. In addition, there are currently a large number of breast pumps that significantly reduce the pumping time and ensure the maintenance of lactation for a long time.
Even when your baby has been breastfed but breastfeeding has been delayed due to surgery or other reasons, you can bottle feed your baby with expressed milk until you can return to normal breastfeeding. In addition, there are currently ways to harvest breast milk for a certain period. Questions about how and when to store milk should be discussed with your pediatrician. In addition, there are currently a large number of breast pumps that significantly reduce the pumping time and ensure the maintenance of lactation for a long time.
Formula feeding
Formula feeding is a simple and reliable substitute for breast milk. For this type of feeding, the same principles are acceptable as for breastfeeding, with the exception of small additions to the technique if necessary. In addition, the easier intake of food with wide cleft lip and palate will help your child more easily compensate for the difficulties that arise from pathological communication of the oral cavity and nose.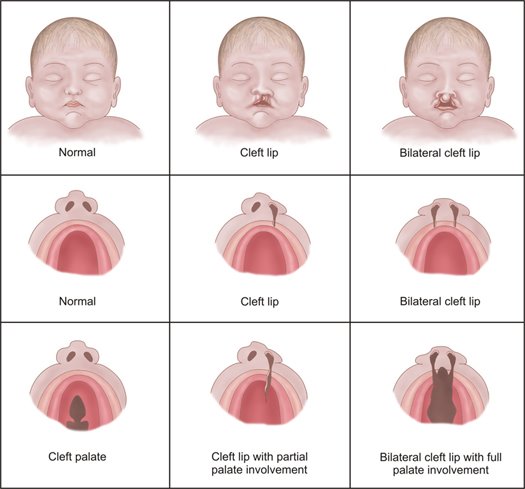 The selection of the necessary mixture for your baby can be adequately carried out by your pediatrician, who is guided by the peculiarities of the metabolism and digestive system of each child. Remember that you need to carefully study the instructions for preparing the mixture, which is usually located on the label of each package. Sometimes the pediatrician may recommend increasing the concentration of the mixture to speed up the weight gain of the child. This is a temporary measure, since the intake of water into the child's body is no less important than the amount of food consumed. For children with a cleft, a pacifier and bottle may need to be matched. Usually, parents start with simple types of nipples and bottles, and often, especially for children with small cleft lips, they are suitable. If the baby is not satisfied with the proposed devices, you can try using special orthodontic nipples and soft bottles. Your main task is to select the nipple and bottle that will make feeding the baby easy and complete.
The selection of the necessary mixture for your baby can be adequately carried out by your pediatrician, who is guided by the peculiarities of the metabolism and digestive system of each child. Remember that you need to carefully study the instructions for preparing the mixture, which is usually located on the label of each package. Sometimes the pediatrician may recommend increasing the concentration of the mixture to speed up the weight gain of the child. This is a temporary measure, since the intake of water into the child's body is no less important than the amount of food consumed. For children with a cleft, a pacifier and bottle may need to be matched. Usually, parents start with simple types of nipples and bottles, and often, especially for children with small cleft lips, they are suitable. If the baby is not satisfied with the proposed devices, you can try using special orthodontic nipples and soft bottles. Your main task is to select the nipple and bottle that will make feeding the baby easy and complete.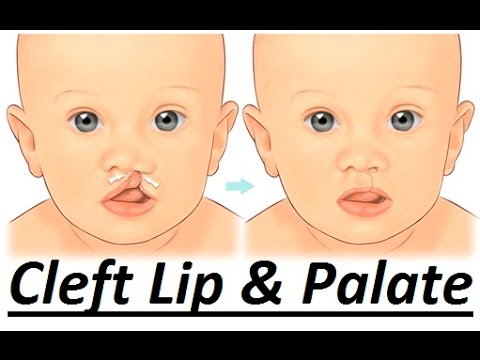
Soft nipples are usually better than hard nipples. You can soften the nipple by boiling. Subsequently, with the strengthening of your baby's chewing muscles, soft nipples can be replaced with soft orthodontic or harder nipples.
Some children with clefts may have difficulty with both very long and very short nipples. Short nipples cannot provide good contact with the tongue and palate, while long nipples can provoke a gag reflex.
One of the ways to regulate the flow of milk into the baby's mouth is the cross hole on the tip of the nipple. Such cuts facilitate the flow of liquid from the bottle. Cross-shaped incisions are very convenient, as they allow the child to regulate the strength and speed of milk flow with a constant sucking rhythm, preventing choking. A simple enlargement of the opening in the nipple causes a steady increase in the flow of milk into the baby's mouth, which leads to difficulty in sucking control and disruption of the interaction between swallowing and breathing. On the contrary, the cruciform incision ensures the flow of milk only at the moment of squeezing the nipple. Any nipple can be made into a cross-cut nipple with a regular razor blade. If it is required to make an incision on the orthodontic nipple, then it is better to perform it not at the very top, but a little closer to the lingual surface, as this will contribute to a dosed flow of fluid.
On the contrary, the cruciform incision ensures the flow of milk only at the moment of squeezing the nipple. Any nipple can be made into a cross-cut nipple with a regular razor blade. If it is required to make an incision on the orthodontic nipple, then it is better to perform it not at the very top, but a little closer to the lingual surface, as this will contribute to a dosed flow of fluid.
Another way to make milk flow easier while conserving baby's energy is to use soft bottles. The compression of such a bottle should be carried out rhythmically and correspond to the frequency of sucking and swallowing food by the child (approximately every 2-3 sips). Following the rhythm of the child, you can be sure that there will be no excessive intake of milk into the oral cavity and its reflux into the respiratory tract. The bottle must be squeezed and then released without continued compression. Feeding is usually easier if the bottle is angled to the opposite side of the mouth from the cleft, so that the nipple can be compressed between the tongue and the remaining normal part of the alveolar process of the maxilla and hard palate. Your baby will make the necessary adjustments on his own, adjusting to the position of the nipple, making it easier for him to get milk from the bottle. To do this, you only need to hold the bottle in one position and give the child the opportunity to shift the nipple from one corner of the mouth to another.
Your baby will make the necessary adjustments on his own, adjusting to the position of the nipple, making it easier for him to get milk from the bottle. To do this, you only need to hold the bottle in one position and give the child the opportunity to shift the nipple from one corner of the mouth to another.
When choosing a method of feeding, parents should understand for themselves some of the main advantages of bottle feeding:
- the most adequate supply of milk to the baby's body;
- saving physical energy spent on feeding, both by the child and the parent;
- the method allows to normalize suckling;
- is the most affordable, inexpensive and easiest way to feed.
Other feeding recommendations
Feeding position
It is very important that the breastfeeding parent finds the most comfortable position for himself. Sometimes, for comfort, it is useful to use a pillow to support the child. It also makes it easier to support the child with a footrest, on which the parent can lean with both one and two legs. Since feeding a baby can take up to 30 minutes. several times a day, the adult feeding the child should choose the most comfortable and relaxed position for himself.
It also makes it easier to support the child with a footrest, on which the parent can lean with both one and two legs. Since feeding a baby can take up to 30 minutes. several times a day, the adult feeding the child should choose the most comfortable and relaxed position for himself.
The baby should be well supported during feeding, usually in a slightly elevated position or sitting. This position helps prevent milk from entering the nose and choking the baby.
While breastfeeding, the mother can use several positions that can make the process much easier. The first position, when the child sits on a mattress or pillow, his back is supported by the mother's forearm, and her head by her brush. In this position, gravity helps the nipple to be placed in the baby's mouth.
It is very important to push the chest away from the baby's nose so as not to interfere with adequate breathing.
Another position where the child sits on the mother's lap, facing her, with the child's legs wide apart, embracing the mother's stomach. Sometimes it is necessary to use a pillow in order to lift the child higher.
Sometimes it is necessary to use a pillow in order to lift the child higher.
In order to suckle effectively, the baby's lower jaw must be in a stable position. If the mother supports the child by the lower jaw or chin, then the baby will not get tired so quickly. It is also useful for the baby's head to be turned first to one side and then to the other during feeding. Such a change allows the muscles of the oral region to work evenly. When bottle feeding, it is important that the baby is supported in an elevated position. The nipple should be placed in the area where all tissues are most preserved.
How to choose the right time to feed
When a baby starts crying loudly and seems agitated, there is a good chance that he is very hungry and this can make feeding very difficult. It is necessary to feed the child before he becomes too hungry. The child eats better when he is slightly hungry and does not feel much discomfort.
Many parents find that they can learn their baby's feeding schedule by watching for certain "signals" of the baby during awakening (moving the eyes under closed eyelids, moving the mouth, or moving the hands to the mouth). However, it must be remembered that the child does not eat the same amount of liquid during each feeding. It depends on the time elapsed between feedings.
However, it must be remembered that the child does not eat the same amount of liquid during each feeding. It depends on the time elapsed between feedings.
Help with food in the nose
Even when a fed baby is in a semi-elevated position, there is a risk of milk entering the nose (nasal regurgitation). Sometimes such regurgitation can be associated with a sudden change in body position. Parents should not be overly concerned about this, as food getting into the nose is quite common at first. It does not harm the child and gradually decrease with the growth of the baby. When regurgitation occurs, it is necessary to temporarily stop feeding and give the baby some time to cough or sneeze. This will allow the baby to clear the nasal passages and you can continue feeding. However, if the child has persistent regurgitation, cough is frequent and severe, you should consult your doctor.
Use of palatal obturators
Some specialists involved in the treatment of children with cleft lip and palate believe that obturators (special palatal plates that follow the curvature of the palate) should be used when feeding children with cleft palate, as they separate the oral and nasal cavity, which can greatly facilitate feeding. Such obturators tend to damage the mucosa. A more reliable result is obtained when the fitting of the obturator is carried out in the first few days of life. If you agree to use such a device, then you must be in close contact with a specialist who will manufacture, try on and adjust the device, periodically replacing it with a new one.
Such obturators tend to damage the mucosa. A more reliable result is obtained when the fitting of the obturator is carried out in the first few days of life. If you agree to use such a device, then you must be in close contact with a specialist who will manufacture, try on and adjust the device, periodically replacing it with a new one.
Most babies born with cleft palate and lip can be adequately fed without the use of such a machine when parents use combinations of feeding positions, appropriate feeding pattern (bottle or while breastfeeding), and appropriate technique.
Solid food introduction
Your child should be ready for pureed food at the same age as other children. Pureed food should be introduced at 4–6 months of age. Feeding should be done with a spoon, not a bottle. This is the time when the child begins to be interested in the difference in tastes and states. Again, moving from an elevated position to a sitting position reduces the number of episodes of regurgitation. Initially, the child should receive a small amount of liquid (no lumps) cereal porridge mixed with artificial formula until he learns to feel the pieces of food in his mouth. Pureed food should be given to the child until he is very hungry, otherwise the child will refuse to eat. The child must be gradually accustomed to more adult food, which takes time and patience. At first, the baby will try to suck in new food, which can again lead to episodes of food entering the nose. If this happens, give the child some water to drink. As soon as the child learns to swallow food, the density of porridge can be increased by mixing it with less milk. After that, you can add other complementary foods. If a child continues to have difficulty learning to eat solid foods for a long time, it is necessary to seek advice from specialists involved in the treatment of children with cleft lip and palate.
Initially, the child should receive a small amount of liquid (no lumps) cereal porridge mixed with artificial formula until he learns to feel the pieces of food in his mouth. Pureed food should be given to the child until he is very hungry, otherwise the child will refuse to eat. The child must be gradually accustomed to more adult food, which takes time and patience. At first, the baby will try to suck in new food, which can again lead to episodes of food entering the nose. If this happens, give the child some water to drink. As soon as the child learns to swallow food, the density of porridge can be increased by mixing it with less milk. After that, you can add other complementary foods. If a child continues to have difficulty learning to eat solid foods for a long time, it is necessary to seek advice from specialists involved in the treatment of children with cleft lip and palate.
Recommended feeding steps
| 4-6 months | introduction of porridge and puree soups |
| 8 months | give liquid, pureed food, introduce more hard or crushed food |
12 m. | give liquid, coarser chopped food, include chewy meat food |
| 18 mo. | give liquid, coarser chopped food, increase the amount of meat food, and increase the amount of raw vegetables |
General questions
1. How often does the baby need to burp?
Frequent regurgitation usually occurs in children who swallow large amounts of air during feeding. The baby usually signals impending regurgitation by slowing down or stopping suckling. This is the time when the baby can burp, and not at the moment of active sucking.
2. Does the cleft area need cleaning?
A child's mouth, whether it has a cleft or not, tends to clean itself. Some newborns with cleft lip do not need additional cleaning, but you should come to such a decision with your pediatrician. Removal of small amounts of curdled milk in the area of the cleft can be successfully carried out by giving the child a few sips of water. In any case, it may be necessary to gently wipe the baby's face and mouth area with a damp cloth. The use of cotton swabs or rinsing with a syringe is not recommended, as this can damage the baby's delicate mucous membrane.
In any case, it may be necessary to gently wipe the baby's face and mouth area with a damp cloth. The use of cotton swabs or rinsing with a syringe is not recommended, as this can damage the baby's delicate mucous membrane.
3. How to feed during the early postoperative period?
The surgeon who will operate on your child will definitely tell you about the features of feeding the baby after the restoration of the lip or palate. Mostly, parents should change the way of feeding immediately after surgery, and then the usual way of feeding will be restored. You will undoubtedly receive advice on restrictions and the introduction of a new way of feeding a few weeks before the operation so that you can gradually get used to this way.
4. When can cup feeding be introduced?
A cleft baby can be cup fed in the same way as other babies. Most babies are ready for this way of eating at 8-9 months of age. There are many types of cups for babies, which can greatly reduce the adjustment period, as some cups may make a baby drink better than others. This helps to establish this way of feeding before palate plasty, especially if your child is already ready for the operation. Drinking from a cup does not adversely affect the newly operated lip and will allow you to return to your usual way of feeding after the operation. Since bottle-feeding is not allowed after palate plasty, gradually weaning the child from it will allow you to avoid unnecessary whims after the operation.
This helps to establish this way of feeding before palate plasty, especially if your child is already ready for the operation. Drinking from a cup does not adversely affect the newly operated lip and will allow you to return to your usual way of feeding after the operation. Since bottle-feeding is not allowed after palate plasty, gradually weaning the child from it will allow you to avoid unnecessary whims after the operation.
The experience of feeding a baby is extremely important for both parents and their baby. Newborn children adapt more easily, and infants learn faster if the parents have the necessary support, patience and love. Remember that there are many experienced professionals ready to provide you with the support you need.
Cleft lip and palate: breastfeeding and prenatal diagnosis
Cleft palate and cleft lip and palate are congenital malformations that occur in the embryonic period and alter the normal formation of the lip, palate, or both.
A cleft lip, also known as a cleft lip, is a hole or cleft in the upper lip. A cleft palate is an opening in the palate (roof of the mouth).
Cleft lip is a malformation in which cleft lip and palate occur simultaneously.
Some children with cleft lip have a small cleft in the upper lip, others have a hole or a larger hole that can reach up to the nose.
The reasons are still not entirely clear.
Scientific studies show that the malformation is caused by both genetic and environmental factors.
In some cases, cleft palate or cleft lip may be associated with genetic syndromes or other disorders, the best known of which is the Pierre Robin sequence or syndrome.
Other possible causes are oligohydramnios, myotonia, or connective tissue disorders.
One third of patients have velocardiofacial syndrome.
NETWOK CHILD PROFESSIONALS: VISIT THE MEDICHILD STAND AT EMERGENCY EXPO
Cleft lip and cleft lip and palate: how to breastfeed?
A child with cleft lip and palate may find it difficult to suckle breastmilk in the first few years of life and later eat.
The football or rugby position is recommended for breastfeeding.
It is necessary to perform tongue lowering exercises before attachment to the breast, filling the cleft (schisis) with breast tissue to prevent milk from escaping through the nose, and finally manually squeezing the milk into the baby's mouth during suckling.
Babies with these problems may find it difficult to suckle from a regular bottle, so it is recommended to enlarge the holes in the nipple or use a special nipple.
Possible alternatives are syringe or drip feeding, spoon feeding and/or the use of an acrylic plastic plate in the mouth to create an artificial separation between the oral and nasal cavities and progressively flatten the nose. gingival arches.
This will also make the operation easier.
In more severe cases, a nasogastric tube should be used, but for as short a time as possible.
It is important that the mother encourages the baby to suck with her finger or pacifier in order to maintain her suckling function.
Symptoms:
Main symptoms:
- Sucking problems: mother's milk, bottle;
- Dental problems: A child with cleft lip and palate often has missing, overlapping or crooked teeth. This requires check-ups and dental and orthodontic corrections;
- Speech problems: some children with cleft lip and palate have difficulty expressing themselves and need speech therapy to learn to speak well;
- Recurrent ear infections (otitis media): Multiple episodes of otitis media can cause hearing loss. Therefore, specialist visits to the ENT specialist are necessary to determine if a tympanic drain (a small tube in the eardrum) should be placed to drain the fluid that accumulates inside and promotes infections.
Cleft palate and cleft palate diagnosis
Cleft palate is diagnosed by a neonatologist/pediatrician after birth during the first visit. In addition to the lips, the integrity of the sky is checked.
Prenatal diagnostics
In some cases it is possible to perform prenatal diagnostics during fetal ultrasound in utero.
The gynecologist will be able to see any malformations of the lip on ultrasound, but it is difficult to see any malformations of the palate.
If the fetus has a cleft lip or suspected cleft palate on ultrasound, the doctor will need to examine the fetus more closely and carefully evaluate other organs that may be affected.
He will recommend prenatal genetic diagnosis.
Treatment of cleft lip and palate is mainly surgical.
Prevention:
Certain factors are now known to increase the chances of these changes during pregnancy.
Value for money:
- Avoid anticonvulsants and methotrexate;
- I don't smoke;
- Do not drink alcohol;
- Take a multivitamin containing at least 400 micrograms of folic acid for women who are pregnant or planning to become pregnant.