Cup feeding baby video
Cup Feeding a Newborn - Breastfeeding Support
Breastfeeding SupportCreated with Sketch.Evidence-based breastfeeding tips and resources
Editor in Chief Philippa Pearson-Glaze
- Home
- Articles
- Our Picks
- Find IBCLC
- About
- Contact
- Newsletter
- Terms & Privacy
- Log in
- Special Circumstances
Author
By Philippa Pearson-Glaze IBCLC
Last Revised
Cup feeding is an alternative to bottle feeding if a baby can’t latch to the breast and needs to be given some milk. It can also be used for supplementing a baby who is not getting enough milk or for a baby who is separated from his mother for a while. It is thought to be a useful short-term alternative to using a bottle teat as it avoids a baby getting confused by the different sucking action required on an artificial bottle nipple (nipple preference/confusion). However, there are disadvantages as well as advantages to cup feeding. This article looks at the pros and cons of cup feeding and how to cup feed a newborn baby.
Search Articles
Need to look something up?
Baby must be awake and alert to cup feedPros and cons of cup feeding
Advantages of cup feeding
- Better oxygen saturation and heart rate. A premature baby can feed at his own pace which may improve his oxygen saturation and heart rate making him more physiologically stable123
- Cup feeding may help preserve breastfeeding by avoiding bottles.
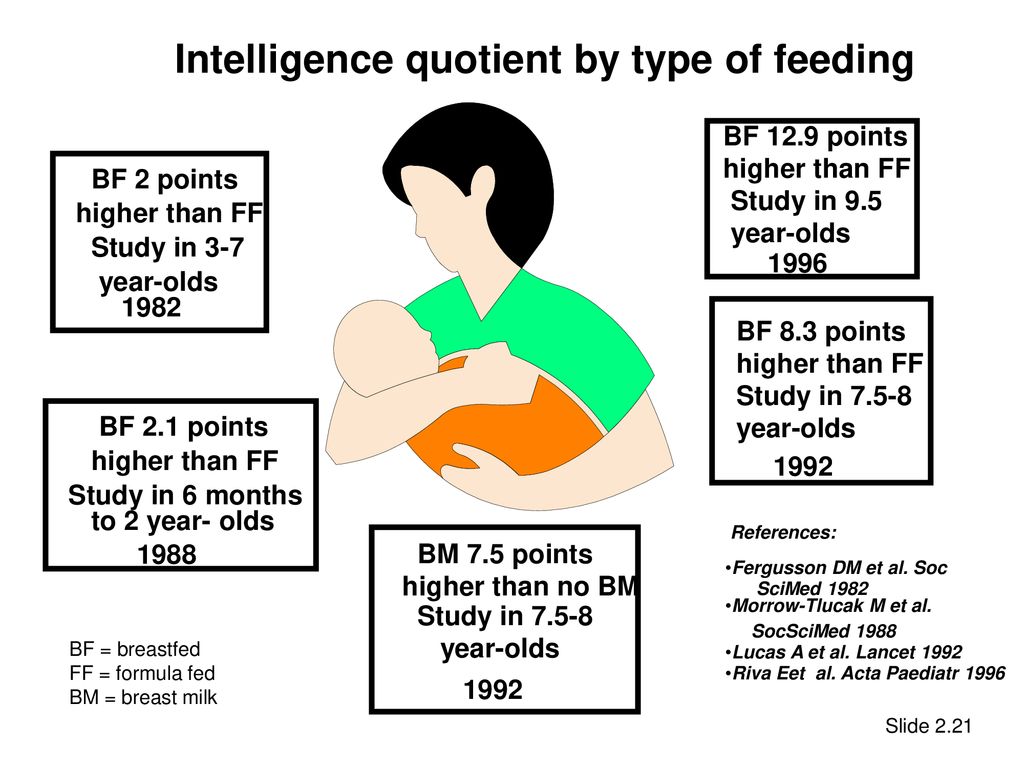
 Studies show cup feeding premature babies instead of using bottles can increase the number of babies who breastfeed and increase the length of time they breastfeed45
Studies show cup feeding premature babies instead of using bottles can increase the number of babies who breastfeed and increase the length of time they breastfeed45 - Cup feeding can prepare a baby for breastfeeding. Feeding technique (use of muscles) while cup feeding is thought to be closer to breastfeeding than using a bottle6 and may help prepare a baby for breastfeeding by encouraging the tongue to come forward for lapping/sipping
- Open cups are easily available, inexpensive and very easy to clean in resource poor areas or emergencies compared with teats, bottles or feeding tubes
- Suitable for very young babies.
 Cup feeding can begin from as early as 29 weeks gestational age.7
Cup feeding can begin from as early as 29 weeks gestational age.7
Disadvantages of cup feeding
- There is a risk of aspiration or choking if cup feeding is not done correctly
- Feeds can take a long time
- There can be a lot of spilled and wasted milk compared with bottle feeding or tube feeding 8
- Long term cup feeding can dampen the sucking reflex or create a preference for the cup
- Not suitable for sleepy babies as there is a risk of choking.
Can cup feeding help preserve breastfeeding?
One review found cup feeding had no significant benefit in maintaining breastfeeding after discharge from hospital and that the length of hospital stay was likely to be a lot longer with cup feeding in some settings. 9 However more recent studies have found the opposite —more cup fed babies were exclusively breastfeeding at discharge, and beyond, with no apparent increase in hospital stay for term10, late preterm11 and premature babies (Penny et al. 2018). The Academy of Breastfeeding Medicine12 states cup feeding may help preserve breastfeeding and the World Health Organisation13 recommends cups or spoons rather than bottles and teats for premature babies.
9 However more recent studies have found the opposite —more cup fed babies were exclusively breastfeeding at discharge, and beyond, with no apparent increase in hospital stay for term10, late preterm11 and premature babies (Penny et al. 2018). The Academy of Breastfeeding Medicine12 states cup feeding may help preserve breastfeeding and the World Health Organisation13 recommends cups or spoons rather than bottles and teats for premature babies.
How to cup feed a baby
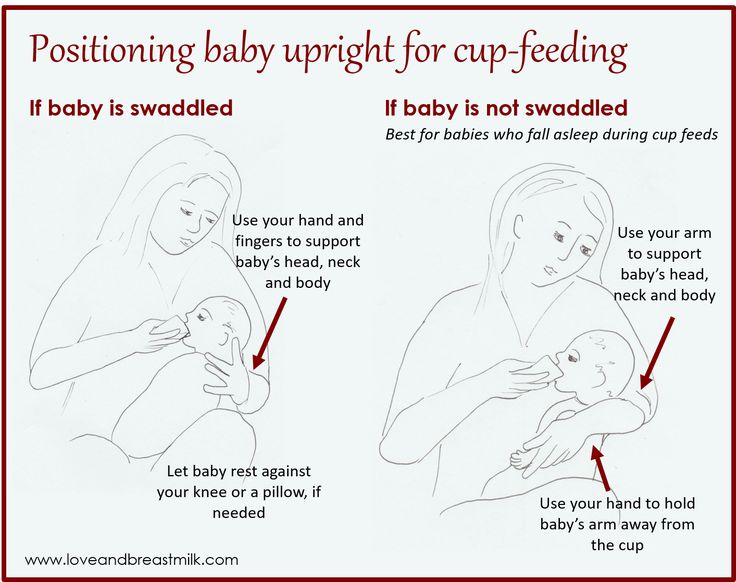
Cup feeding is best taught by a demonstration from your experienced health care professional if possible. They will advise you whether the technique is suitable for your baby. To cup feed a baby needs to be awake and alert, and in an upright position. Never cup feed a sleepy baby or a baby who is lying flat and never pour milk into a baby’s mouth as these all increase the risk of your baby choking.
Cup feeding videos
Global Health Media has a lovely series of videos about breastfeeding, the first clip below (9 minutes long) discusses how to safely cup feed a small baby who isn’t breastfeeding yet and includes spoon feeding, using a paladai (see below) and using a nifty cup:
Cup feeding description
The following description is summarised from the video above. Use a small cup with a smooth edge such as a medicine cup, sherry glass or shot glass—your maternity hospital may give you one. You can also buy little plastic cups specially for the purpose which can be shaped slightly during feeding. You may need a cloth under baby’s chin in case any milk spills.
You may need a cloth under baby’s chin in case any milk spills.
- Half fill or two thirds fill a small cup with slightly warmed breast milk or infant formula
- Ensure your baby is fully awake, alert and interested in feeding. Never cup feed a sleepy baby
- If needed, wrap your baby to prevent him knocking the cup out of your hands
- Sit your baby in a comfortable, upright position on your lap. Never cup feed a baby who is lying flat on their back
- Rest the rim of the cup lightly on your baby’s lower lip or their lower gum ridge
- Tip the cup just enough so that milk reaches the rim of the cup, don’t put the cup too far into baby’s mouth
- Your baby will quickly learn to sip or lap milk from the rim of the cup with his tongue
- DO NOT pour the milk into his mouth, go slowly always keeping the milk just at the rim of the cup
- Leave the cup in position when baby pauses to rest between swallows and is not drinking, avoid putting pressure on the lower lip
- Continue to tip the cup enough to keep the milk at the rim of cup resting lightly on baby’s lower lip
- Burp baby if needed during the feed.

Short film clips of cup feeding
In the following short clip from Global Health Media, a premature baby is cup feeding. Notice how the baby’s tongue extends to lap the milk.
Jack Newman is a Canadian paediatrician and breastfeeding expert. Here is a clip of cup feeding from his International Breastfeeding Centre:
Using a paladai
Mothers in India have used a small spouted cup called a paladai for centuries. One study compared the use of a bottle, cup and a paladai in 100 newborn babies. Infants took the most milk in the least time and stayed calmest with the paladai 14. However a more recent pilot study comparing the paladai with bottle feeding in preterm infants found increased spillage, longer feed times and more stress cues 15.
Alternatives to cup feeding
Alternatives to cup feeding for the breastfed baby who needs supplementing include:
- Supplementing at the breast. A breastfed baby who is latching well to the breast but who needs additional milk can be supplemented while they are breastfeeding by way of a small feeding tube alongside the nipple. The free end of the feeding tube is placed in a container of milk and provides milk when baby suckles with a good seal around breast and tube. For much more information about the pros and cons of this system see Supplementing at the Breast.
- Finger feeding. Finger feeding is another method of providing supplemental milk to a breastfed baby by way of a feeding tube (above). In this case the feeding tube provides additional milk while the baby suckles on a clean finger. For more information on the pros and cons of finger feeding see What is Finger Feeding?
- Bottle feeding.
 A traditional way to provide supplemental milk is by bottle and teat. Feeding from an artificial teat has a number of differences to breastfeeding which could cause nipple preference or confusion in some babies. However there are several ways to reduce the differences to help preserve breastfeeding, see Tips to Bottle Feed a Breastfed Baby and Best Bottle for a Breastfed Baby?
A traditional way to provide supplemental milk is by bottle and teat. Feeding from an artificial teat has a number of differences to breastfeeding which could cause nipple preference or confusion in some babies. However there are several ways to reduce the differences to help preserve breastfeeding, see Tips to Bottle Feed a Breastfed Baby and Best Bottle for a Breastfed Baby?
Summary
Used correctly, cup feeding can be a useful way to give a newborn baby supplementary milk for short term feeding. Other options for supplementary feeds include using a supplemental nursing system at the breast, or a bottle using our tips to minimise nipple confusion. Your breastfeeding specialist or health professional can help you decide which option is best for you and your baby.
Footnotes & References
-
Penny et al. Cup Feeding as a Supplemental, Alternative Feeding Method for Preterm Breastfed Infants: An Integrative Review. Matern Child Health J.
 2018
2018 -
Rocha et al, Cup or bottle for preterm infants: effects on oxygen saturation, weight gain, and breastfeeding, 2002
-
Marinelli et al, A comparison of the safety of cupfeedings and bottlefeedings in premature infants whose mothers intend to breastfeed, 2001
-
Collins et al. Avoidance of bottles during the establishment of breast feeds in preterm infants. Cochrane database of systematic reviews. 2016
-
Penny et al. Cup Feeding as a Supplemental, Alternative Feeding Method for Preterm Breastfed Infants: An Integrative Review. Matern Child Health J. 2018
-
Franca et al. Electromyographic analysis of masseter muscle in newborns during suction in breast, bottle or cup feeding. BMC Pregnancy and Childbirth volume 14, 2014
-
Gupta et al, Cup feeding: an alternative to bottle feeding in a neonatal intensive care unit, 1999
-
McKinney et al, Feeding Neonates by Cup: A Systematic Review of the Literature, 2016
-
Han AM, Cup-feeding versus other forms of supplemental enteral feeding for newborn infants unable to fully breastfeed, 2010
-
McKinney et al, Feeding Neonates by Cup: A Systematic Review of the Literature, 2016
-
Yilmaz et al, Effect of cup feeding and bottle feeding on breastfeeding in late preterm infants: a randomized controlled study, 2014
-
ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Academy of Breastfeeding Medicine, Revised 2017
-
Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services, WHO, 2017
-
Malhotra et al, A controlled trial of alternative methods of oral feeding in neonates, 1999
-
Aloysius & Hickson, Evaluation of paladai cup feeding in breast-fed preterm infants compared with bottle feeding, 2007
Further Reading
- ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed NeonateAcademy of Breastfeeding Medicine, 2017
- Cup Feeding Versus Other Forms of Supplemental FeedingCochrane Database, 2010
- Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn ServicesWHO, 2017
- What is Finger Feeding?Breastfeeding Support 2018
- Finger and Cup feedingJack Newman, 2009
Important
This article should not be construed as medical advice. Information found online should always be discussed with your own IBCLC lactation consultant and doctor to ensure it is appropriate for you and your baby’s situation. Contact your doctor, paediatrician or health care provider with any concerns about your baby’s health and welfare.
Information found online should always be discussed with your own IBCLC lactation consultant and doctor to ensure it is appropriate for you and your baby’s situation. Contact your doctor, paediatrician or health care provider with any concerns about your baby’s health and welfare.
Find an IBCLC Read our full disclaimer
International BreastFeeding Centre | Finger feeding and cup feeding
Finger feeding is a technique the main purpose of which is to prepare the baby to take the breast when the baby is unable to latch on. See our blog on the baby who does not latch on. Though finger feeding can be used to feed a baby and thus avoid artificial nipples, this is not what it is meant to do really. Furthermore, if the baby is actually taking the breast (latching on) and requires supplementation, this supplementation should be given with a lactation aid at the breast not by finger feeding. See the blog on the Lactation Aid and the video clips. Too often finger feeding is used to feed the baby when a mother has sore nipples, and the baby is taken off the breast. This is seen as not interfering with breastfeeding while, at the same time, the “nipples are given a rest”. Taking a baby off the breast for any reason, including sore nipples, should be a last resort only. See the blogs What is a good latch, Sore Nipples which contains information on the all purpose nipple ointment (APNO). See also the information on Candida Protocol.
Too often finger feeding is used to feed the baby when a mother has sore nipples, and the baby is taken off the breast. This is seen as not interfering with breastfeeding while, at the same time, the “nipples are given a rest”. Taking a baby off the breast for any reason, including sore nipples, should be a last resort only. See the blogs What is a good latch, Sore Nipples which contains information on the all purpose nipple ointment (APNO). See also the information on Candida Protocol.
Finger feeding may be used if:
1. The baby refuses the breast for whatever reason, or if the baby is too sleepy at the breast to breastfeed well. Good flow of milk to the baby will tend to wake the baby up, as, for another example, to wake up a sleepy baby during the first few days of life and there are concerns about intake.
2. The baby does not seem to be able to latch on to the breast properly, and thus does not get milk well. (However, if the baby is latching on, even not well, then it is better to use a lactation aid at the breast to give extra milk).
3. The baby is separated from the mother, for whatever reason. However, in such a situation, feeding the baby with an open cup is probably a better method of feeding the baby. Since finger feeding should be used primarily to help a baby take the breast when he is reluctant or temporarily unable, the best technique is not finger feeding if the mother is not present to breastfeed him.
4. Breastfeeding is stopped temporarily (there are very few legitimate reasons to stop breastfeeding. However, in this case too, an open cup would be better. See our blog on medication and 2 blogs on maternal illness 1 and 2.
5. Your nipples are so sore that you cannot put the baby to the breast. Finger feeding for several days may allow your nipples to heal without causing more problems by getting the baby used to an artificial nipple. However, see the first paragraph above about taking the baby off the breast. Cup feeding, even a baby only a few hours old (see photo below), is also more appropriate in this situation and takes less time.
6. Taking a baby off the breast should be a last resort only but too often is recommended as a first resort. Proper positioning and a good asymmetric latch will help sore nipples far more than finger feeding. And our “all purpose nipple ointment”, described in several blogs, including this one, will help as well. This so called “nipple holiday” is not advisable and if suggested within the first few days of life may be a terrible mistake. Taking the baby off the breast does not always result in painless feedings once you start again and sometimes the baby, fed away from the breast, will refuse to latch on.
This newborn is being cup fed with his mother’s expressed colostrum. Why is a bottle better? It is not.
It is true that finger feeding is much more similar to breastfeeding, if done properly, than is bottle feeding. In order to finger feed, the baby must keep his tongue down and forward over the gums, his mouth wide (the larger the finger used, the better so using a baby finger to do finger feeding is not a good idea), and his jaw forward.![]() Furthermore, the motion of the tongue and jaw is similar to what the baby does while feeding at the breast. Finger feeding is best used to prepare the baby who is refusing to latch on to take the breast. It needs to be done only for a minute or two, at the most, just before trying the baby on the breast if the baby is refusing to latch on. See video clip Finger feed to latch.
Furthermore, the motion of the tongue and jaw is similar to what the baby does while feeding at the breast. Finger feeding is best used to prepare the baby who is refusing to latch on to take the breast. It needs to be done only for a minute or two, at the most, just before trying the baby on the breast if the baby is refusing to latch on. See video clip Finger feed to latch.
What does this video show? Finger feeding is a useful technique to help a baby who is reluctant to latch on to latch on. Finger feeding calms an upset baby and wakes up a sleepy baby. Once the baby is sucking well on the finger, it is time to move the baby over to the breast. Do not try to force the baby to take the breast. As seen in the video, it took a couple of tries to get the baby to latch on. Letting the baby come off the breast if he has not latched on works better than trying to force him into the breast when he resists staying there, does not work at all, but only makes things worse. The baby did not take the right breast because he had already fed on the right and the flow of milk was slower than ideal even with the lactation aid. The baby took the left breast because he had not yet fed on the left so that the combination of flow from the breast and flow from the lactation aid in combination with an asymmetric latch gave him what he needed. This baby was born 8 weeks prematurely, is now 2 months old in the video and has never in his life latched on though the mother was producing all the milk the baby needed. Why was the baby not latching on? See these two blogs on the premature baby: 1 and 2. A third blog on the premature baby is also available on our website.
The baby took the left breast because he had not yet fed on the left so that the combination of flow from the breast and flow from the lactation aid in combination with an asymmetric latch gave him what he needed. This baby was born 8 weeks prematurely, is now 2 months old in the video and has never in his life latched on though the mother was producing all the milk the baby needed. Why was the baby not latching on? See these two blogs on the premature baby: 1 and 2. A third blog on the premature baby is also available on our website.
If the mother is not present to feed the baby or if the baby still doesn’t latch on after the finger feeding is attempted, then feeding the baby with a cup is better than finger feeding which can be slow.
Please Note: If the baby is taking the breast, it is far better to use the lactation aid tube at the breast, if supplementation is truly necessary (See information sheet Protocol to Increase Breastmilk Intake and Lactation Aid).![]() Again, finger feeding is not a good method of supplementation in the latching baby.
Again, finger feeding is not a good method of supplementation in the latching baby.
FINGER FEEDING (BEST LEARNED BY WATCHING AND DOING).
See also the video clip Not Yet Latching; Finger feed to Latch (same as the video above). The video shows the information below much better than words.
1. Wash your hands. It is better if the fingernail on the finger you will use has been cut short, but this is not necessary.
2. It is best to position yourself and the baby comfortably. The baby’s head should be supported with one hand behind his shoulders and neck; the baby should be on your lap, half seated. It may be easiest if he is facing you. However, any position which is comfortable for you and the baby and which allows you to keep your finger flat in the baby’s mouth will do. See the video clip Finger feed to latch
.
3. You will need a lactation aid, made up of a feeding tube (#5 French, 93 cm or 36 inches long), and a feeding bottle with an enlarged nipple hole, filled with expressed breast milk or supplement if breastmilk is not available. The feeding tube is passed through the enlarged nipple hole into the fluid.
The feeding tube is passed through the enlarged nipple hole into the fluid.
4. Line up the tube so that it sits on the soft part of your index, thumb, or middle finger. The end of the tube should line up no further than the end of your finger. It is easiest to grip the tube, about where it makes a gentle curve, between your thumb and middle finger and then position your index finger under the tube. If this is done properly, there is no need to tape the tube to your finger.
5. Using your finger with the tube, tickle the baby’s upper lip lightly until the baby opens up his mouth enough to allow your finger to enter. If the baby is very sleepy, but needs to be fed, the finger may be gently insinuated into his mouth. Pull the baby’s lower lip out if necessary by exerting some downward pressure on the baby’s chin. Generally, the baby will begin to suck even if asleep and as s/he receives liquids s/he will then wake up.
6. Insert your finger with the tube so that the soft part of your finger remains upwards. Keep your finger as flat as possible, thus keeping the baby’s tongue flat and forward. Usually the baby will begin sucking on the finger, and allow the finger to enter quite far. The baby will not usually gag on your finger even if it is in his mouth quite far, unless the baby is not hungry or he is very used to bottles.
Keep your finger as flat as possible, thus keeping the baby’s tongue flat and forward. Usually the baby will begin sucking on the finger, and allow the finger to enter quite far. The baby will not usually gag on your finger even if it is in his mouth quite far, unless the baby is not hungry or he is very used to bottles.
7. Gently pull down the baby’s chin, if his lower lip is sucked in.
8. The technique is working if the baby is drinking. If feeding is very slow, you may raise the bottle above the baby’s head, but usually this should not be necessary. Try to keep your finger straight, flattening the baby’s tongue. Try not to point your finger up, but keep it flat. Do not apply pressure to the roof of baby’s mouth.
9. The use of finger feeding with a syringe to push milk into the baby’s mouth is, in our opinion, too difficult for the mother to do alone and definitely not more effective than simply using a bottle with the nipple hole enlarged and the tube coming from it. The idea of finger feeding is not really to feed the baby! The idea is to train the baby to suck properly so that pushing milk into his mouth defeats the whole purpose of finger feeding.
The idea of finger feeding is not really to feed the baby! The idea is to train the baby to suck properly so that pushing milk into his mouth defeats the whole purpose of finger feeding.
If you are having trouble getting the baby to latch on to or to suckle at the breast, remember that a ravenous baby can make the going very difficult. Take the edge off his hunger by using the finger feeding technique for a minute or so. Once the baby has settled a little, and sucks well on your finger (usually only a minute or so is necessary), try offering the breast again. If you still encounter difficulty, do not be discouraged. Go back to finger feeding and try again later in the feed or next feeding. This technique usually works. Sometimes several days, or on occasion a week or more, of finger feeding are necessary, however.
CUP FEEDING
See photo above, and this video. This baby in the video is already 4 months old and has been essentially bottle fed from birth. He is not at first liking this new way of feeding, but improved with time.
He is not at first liking this new way of feeding, but improved with time.
Cup feeding (and similar vessels like spoon, etc) is a method of feeding baby that has been around for a very long period of time. It should be used to feed a baby who is not yet taking the breast and is better than a bottle. This should not be used to supplement a baby who is taking the breast (see the information sheets Lactation Aid and The Baby Who Does Not Yet Latch).
1. Sit baby upright on your lap with baby’s head supported while you have one hand behind his shoulders and neck
- Use a small medicine cup or shot glass when first learning how to cup feed
2. Place the edge of the cup gently on baby’s lower lip or gum
3. Bring the liquid to baby’s lower lip so baby will lap it up like a pussycat. Do not pour the liquid in baby’s mouth
4. It is important to maintain the level of the liquid as best as possible so baby can continually lap it up.![]()
5. Go slowly as the two of you learn how to do this. Eventually, this can become a very fast and efficient way of feeding until baby learns to take the breast, and this is a good method to use to avoid artificial nipples and teats.
If you are leaving the hospital finger or cup feeding the baby, make an appointment with the clinic within a day or so of discharge, or get other good hands-on help quickly. The earlier the better. Once the baby is taking the breast, s/he may still require the lactation aid to supplement for a period of time; because although the baby may take the breast, the latch can still be less than ideal, and the suck may still not be efficient enough to ensure adequate intake.
The information presented here is general and not a substitute for personalized treatment from an International Board Certified Lactation Consultant (IBCLC) or other qualified medical professionals.
This information sheet may be copied and distributed without further permission on the condition that it is not used in any context that violates the WHO International Code on the Marketing of Breastmilk Substitutes (1981) and subsequent World Health Assembly resolutions. If you don’t know what this means, please email us to ask!
If you don’t know what this means, please email us to ask!
©IBC, updated July 2009, 2021
Questions or concerns? Email Dr. Jack Newman (read the page carefully, and answer the listed questions).
Make an appointment at the Newman Breastfeeding Clinic.
CUP FEEDING - La Leche Liga Russia
Diseases and special conditions of the baby, Breastfeeding doctors and specialists, breastfeeding, Books and articles, Childbirth. Starting breastfeeding., Lifestyle and breastfeeding, Pumping, The amazing benefits of breast milk, What to do if ...01/16/2021
A baby who does not breastfeed can be fed from a cup
Cup feeding can be used from birth. This method is suitable for both breast milk and formula. You can use any clean cup with a smooth surface.
Cup feeding does not have a noticeable difference with bottles in average feeding time.
Cups are safer than bottles. Bottle nipples and screw caps keep germs out that can get into milk and cause illness in babies. The cups are easy to clean with soapy water and do not need to be sterilized like bottles.
The cups are easy to clean with soapy water and do not need to be sterilized like bottles.
Use disposable cups in case of emergency.
Feeding time is a time of togetherness: lots of hugs, eye contact, talking, smiling, humming and singing.
1-2-3 Cup Feeding
- Place your baby on your knees and support their back and neck. With young children, loose swaddling can help to keep their hands from rattling on the cup.
- Take a small cup of milk and press the rim lightly against the child's lower lip. Then tilt the cup so that the milk stays on the edge of the cup, but so that it reaches the baby's lips. The baby must be awake in order to be able to open its mouth on its own.
- Continue slowly. DO NOT pour milk into baby's mouth. Always let your baby lead the pace of sips and pauses. Continue to keep milk only on the edge of the cup. When the baby is full, he will close his mouth and will no longer continue feeding
Babies will suck or drink milk, or may use their tongue to lap it, as in the picture.
Cup feeding gives babies the freedom to move their tongue in a way that is closer to the “sucking” reflex used in breastfeeding.
Did you know that you can restore breastfeeding through a process called relactation?
Breastfeeding saves lives, especially in emergencies.
Contact a La Leche League Volunteer Consultant for more information.
Adapted from the World Health Organization - Infant Feeding in Emergencies: A Guide for Mothers and a 20 Hour Hospital Course for the UNICEF/WHO Baby Friendly Hospital Initiative by Magdalena Woolery (PhD Health Studies, BSc Nursing, Dip HE Nursing) and Julie Fogarty (BFA, GradDipTchg), January 2020 (updated April 2020). The poster is endorsed by the following organizations: International Infant Food Surveillance Network (IBFAN, breastfeeding advocacy), Safe Feeding Canada, Breastfeeding Advocacy Australia, La Leche League International (LLLI).
Poster also available in PDF format:
Cup Feeding
Cup Feeding B/W
How to teach your baby to drink from a cup
Search Support IconSearch Keywords
- Video, Audio, Communication Personal care
- Everything for mother and child
- Home appliances
- Lighting
- Health
- Automotive
- Accessories
When learning a new skill, break it down into several stages - this will greatly simplify the process.
 That's exactly what we did when we developed a solution that will help your baby move from a bottle to a non-spill cup. Use this guide to learn about the four stages of learning to drink from a cup and which cup is best for a child at a given developmental stage.
That's exactly what we did when we developed a solution that will help your baby move from a bottle to a non-spill cup. Use this guide to learn about the four stages of learning to drink from a cup and which cup is best for a child at a given developmental stage. At what age should you start teaching your child to drink from a cup?
On average, it takes about 15 months for babies from 4 months to go from a bottle to a cup. We have labeled our non-spill cups by age, but remember that every child is different and develops at their own pace.
Take it step by step
To learn to drink like adults, your baby needs to learn more complex oral motor skills and be able to coordinate movements.
We've broken down the process into steps to help you learn.
Step 1: Learn to drink by holding handles
First, teach your baby to hold a non-spill cup. You can make the process easier by starting training while your baby is bottle-feeding with our training set: your baby will hold the bottle by the soft, comfortable handles and drink through the familiar nipple.
Matching non-spill cup: Bottle to Cup Training Set
Ideal solution for babies from 4 months who have learned to sit upright with support
Step 2: Learn to drink through the spout
As your baby transitions to solid foods, you can teach him the new skill of drinking through the spout. Here the baby will need a little more skill than when feeding from a pacifier. This skill will also help your baby develop the suction needed to drink from a cup, which a baby usually starts learning around 6 months of age. To help you at this stage, we have created a soft and flexible spout that does not damage the gums. When the child begins to chew food with his teeth, you can switch to a denser, bite-resistant nose.
Matching non-spill cup: cup with spout
Ideal solution for babies from 6 months old who have learned to sit on a high chair
Step 3. Learn to drink through a straw
When the next baby learns to drink naturally through a spout step is to learn to drink through a straw. This is a more complex oral motility, which will help develop a full-fledged skill, like an adult.
This is a more complex oral motility, which will help develop a full-fledged skill, like an adult.
Suitable non-spill cup: cup with straw
Ideal solution for babies from 9 months old who have learned to crawl
Step 4. Learn to drink from a cup
Finally you can move on to the main thing - drinking from a cup over the edge, like real adults do. Don't worry, this step won't cause you much inconvenience: our "adult" cup is equipped with a leak-proof valve that only opens when it comes into contact with a child's lips.
Suitable non-spill cup: "Adult" cup
Ideal solution for babies aged 9 months to crawl
Choosing the best non-spill cup to help your baby develop properly
First look at the age markings to find the right cup for your baby at this stage of development. However, remember that there are no clear and hard rules here: perhaps the baby has not yet learned how to sit on his own or he needs a little more time to figure out how to hold the cup. It is important to choose a cup that will help the child develop correctly and move on to the next stage of learning.
It is important to choose a cup that will help the child develop correctly and move on to the next stage of learning.
Convenient solution
But don't rush to think: "How many cups do you need to have with you!". Most Philips Avent non-spill cups, spouts and lids are interchangeable. This means that you can use the same spout with different cups or put it on a bottle. Convenient, right?
We recommend changing the spouts and caps of baby bottles and non-spill cups every three months.
Would you like to know more about our children's non-spill cups? Click here to view the range.
Learn more about this topic
-
Baby cups
Learn to drink on your own
Learn more
You are leaving the official Philips Health website. Any links to third party websites that may be included on this site are provided solely as a convenience to you.