Feeding a baby with bottle
Bottle-feeding babies: giving the bottle
About bottle-feeding
If your baby can’t always feed directly from your breast, you might choose to bottle-feed with expressed breastmilk. Or you might need to feed your baby infant formula, which is the only safe alternative to breastmilk.
Before you bottle-feed your baby, it’s important to know how to clean and sterilise bottle-feeding equipment, as well as how to prepare, store and warm bottles of formula. This will help to keep your baby safe from infection and make sure baby is getting the right nutrition.
Getting the right flow when bottle-feeding
To test the flow of the formula or breastmilk, hold the bottle upside down when it’s filled with liquid at room temperature. The liquid should drip steadily from the teat but not pour out.
If you have to shake the bottle vigorously to see the drip, the flow is too slow. Your baby might go to sleep before drinking what they need.
When you feed your baby, you might see a little leakage at the corners of your baby’s mouth. This doesn’t mean the flow is too fast. It’s nothing to worry about. It will stop as your baby gets older.
If you have trouble finding a teat with a flow to suit your baby, try a faster teat rather than a slower one. You might need to try a few different teats before you find one that suits.
Giving baby the bottle
Make yourself comfortable and cuddle your baby close to you, holding baby gently but firmly. It’s better for your baby to be on a slight incline so any air bubbles rise to the top, making burping easier.
Put the teat against your baby’s lips. Your baby will open their mouth and start to suck. Keep the neck of the bottle at an angle so it’s filled with formula or breastmilk.
When your baby stops sucking strongly or when about half of the formula or breastmilk has gone, gently remove the bottle and see whether baby wants to burp. Once you’ve tried burping your baby, you can offer the bottle again.
Paced bottle-feeding
Babies who are normally breastfed might find it hard to pace themselves when bottle-feeding, particularly if they’re premature. This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
Paced feeding can sometimes help. This involves holding your baby in an upright position and letting them rest every few minutes. If you’re interested in paced bottle-feeding, it’s best to get help from your child and family health nurse or a lactation consultant.
Holding, cuddling and talking to your baby during feeding will help baby develop and grow. It’s also a great opportunity to bond with your baby.
When baby doesn’t finish the bottle or goes to sleep while feeding
Don’t worry if your baby doesn’t finish the bottle. Babies are very good at judging how much they need, so you can let your baby decide when they’ve had enough formula or breastmilk.
If your baby goes to sleep during a feed, put baby over your shoulder, rub their back, and stroke their head, legs and tummy. This can help your baby to wake up. A nappy change is a good way to wake up your baby if that doesn’t work.
Wait until your baby is properly awake before offering the rest of the formula or breastmilk.
If there’s any formula or breastmilk left in the bottle, throw it away after one hour. When your baby drinks from a bottle of formula or breastmilk, bacteria from their mouth get into the milk. The bacteria can grow and make your baby sick if you give your the baby the half-finished bottle later.
When baby refuses the bottle
Babies sometimes refuse a bottle altogether. Here are things to try if this happens:
- Try a new feeding position or change the feeding environment. For example, move around while you’re feeding, find a quieter place to feed, or play some relaxing background music.
- Try again later when your baby is more settled. For example, give your baby a bath and then try again.
- Ask your partner or another family member to give your baby the bottle.
- Try using a different teat. If the flow of formula or breastmilk is too slow, it might frustrate your baby.

- Let your baby open their mouth for the bottle when they’re ready, rather than putting the teat into their mouth.
- Offer the formula or breastmilk from a small cup or spoon. To do this, sit your baby up and offer them small sips.
If your baby is regularly refusing the bottle, you could try adjusting your routine.
If you think your baby is refusing the bottle because they’re unwell, treat your baby’s symptoms or take your baby to see your GP.
How much do bottle-feeding babies drink?
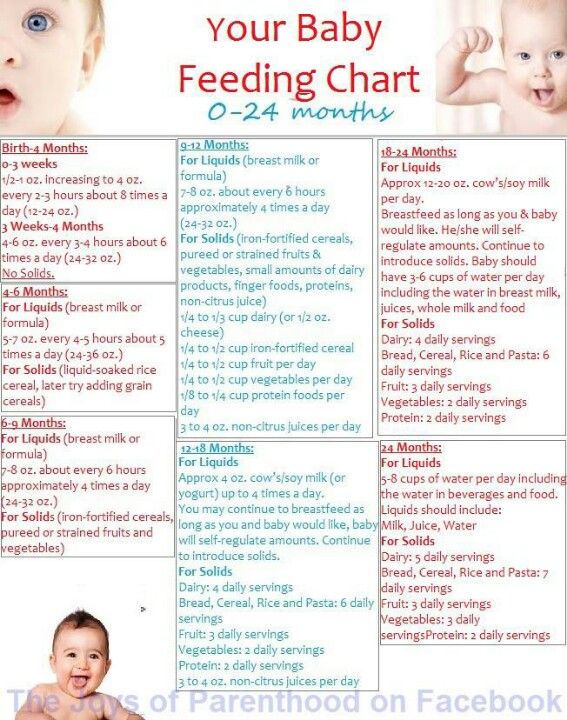
Newborn babies commonly have 6-8 feeds every 24 hours, but there’s no set amount of food or number of feeds your baby should have. Different babies drink different amounts of formula or breastmilk. Some might have feeds close together and others further apart. And it can change from day to day.
Just feed your baby whenever they’re hungry. You’ll see baby cues that say ‘I’m hungry’ – for example, your baby will make sucking noises or start turning towards the breast or bottle. If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
As your baby eats more and more solid food, the total amount of breastmilk or formula they take in a day will decrease. The amount of breastmilk or formula will also decrease as your baby starts to drink from a cup instead of a bottle.
Some babies never drink the ‘recommended amount’ for their age and size, and others need more. Plenty of wet nappies, consistent healthy weight gains, and a thriving, active baby mean all is well. If you’re concerned about how much breastmilk or formula your baby is taking, talk to your child and family health nurse or GP.
Bottle-feeding in bed: issues and risks
Sleep associations
If your baby gets used to falling asleep with a bottle in bed, they might depend on it to get to sleep. This can make it more difficult for your child to fall asleep or settle for sleep independently.
Bottle-feeding in bed also has several risks for your baby.
Choking
Babies who fall asleep while bottle-feeding can draw liquid into their lungs. They might then choke on it or inhale it.
Tooth decay
Babies have less saliva in their mouths to protect their teeth during sleep. If your baby falls asleep with a bottle, the lactose in the milk can build up on your baby’s teeth, putting your baby at risk of tooth decay.
Ear infections
If your baby drinks while lying flat, milk can flow into the ear cavity, which can cause ear infections.
It’s best to put your baby to bed without a bottle or to take the bottle away after your baby has finished feeding.
Using a feeding cup
When your baby is around 6 months old, you can help your baby start leaning to drink from a cup. It’s best to stop using bottles by the time your baby is 12 months old.
You should continue to thoroughly wash and sterilise feeding cups containing infant formula or breastmilk until your baby is 12 months old.
How to Bottle-Feed a Baby
Whether you’re breastfeeding, formula-feeding or doing a combination of both, chances are you’ll eventually use a bottle with your infant. No big deal, right? But while images of a parent blissfully holding a bottle make the process look easy, there’s a learning curve when it comes to proper bottle-feeding. Here, everything you need to know about how to bottle-feed a baby safely and happily.
In this article:
How to choose the right bottle and nipple
How to make a baby bottle
Best bottle-feeding positions
What is pace feeding?
How to get baby to take a bottle
When to wean baby off the bottle
How to Choose the Right Bottle and Nipple
When it comes to figuring out how to bottle-feed a baby, selecting an appropriate bottle and nipple is step one. If people gifted you a bunch of bottles at your baby shower, you may want to hold off before opening and sterilizing them until baby is born, or at least take out just a few to try in the early days of feeding. Why? Because you won’t know what kind of bottle is best until you figure out what baby’s feeding needs are.
Why? Because you won’t know what kind of bottle is best until you figure out what baby’s feeding needs are.
“Certain bottles work better for certain babies,” explains Jamie O’Day, BSN, RN, CLC, a registered nurse, certified lactation consultant and cofounder of Boston NAPS, a pre- and postnatal resource center in the Boston area. “For example, some babies who have issues with gas may do better with a bottle that has a filtration system, like a Doctor Brown’s style bottle, while babies who are used to being breastfed may have more success drinking from a bottle that aims to mimic the shape and feel of a mother’s breast, like the Comotomo.”
That said, O’Day has a universal tip for all parents: Look for a bottle that’s easy to take apart and clean. That generally means a nice wide neck and the fewest parts possible. “Proper cleaning is so important, so I always tell parents to choose the simplest bottle, which may just have a nipple, bottle and collar,” she says. If your child seems happy and easily takes the bottle, then there’s no need to switch.
Of course, it’s not just the bottle that you have to consider. It’s also important to pay attention to the flow of the nipple, which varies based on infant age. Generally speaking, young babies need a slower flow, while older babies who’ve mastered the art of bottle-feeding can handle a faster flow. The nipple may be called “slow flow,” “medium flow” or “fast flow” or may be numbered from one to three, with one being the slowest flow. There is no standard of flow between different brands, but most newborns should begin on level one or slow flow.
So how can you tell when it’s time to change the nipple size? That depends. Some infants happily use the same flow nipple throughout their infancy, while others may need a faster flow nipple. “If you notice your child taking a long time to finish a bottle, or losing interest midway through feedings, a faster flow nipple may be needed,” O’Day says, adding that this might happen at around 3 or 4 months of age, with another potential upgrade around 6 or 7 months.
If your infant finishes a bottle quickly (say, under five minutes), seems gassy or cranky, or spits up a lot of milk right after feedings, it may be time to go back to a slower-flow nipple. Your pediatrician can also help determine if it may be time to switch the flow of the nipple.
How to Make a Baby Bottle
If you’re wondering how to bottle-feed a baby, you’re probably new to prepping baby bottles. Take a new skill, add in sleep deprivation and sprinkle in some very real safety concerns and you’ve got the somewhat daunting process of making a baby bottle (at least at first). Don’t despair. By reading directions, following the advice of a pediatrician and making sure to err on the side of caution, you’ll get the hang of it in no time.
How to make a baby bottle with formula
Baby formula comes in three different forms: ready-to-feed, concentrate and powder. The Centers for Disease Control and Prevention (CDC) recommends that babies under 3 months start off with ready-to-feed formula because of the small but real risk of cronobacter, a bacteria that can live in powdered infant formula.
• Preparing ready-to-feed formula: These require very little prep, since they come ready to be poured into a bottle and fed to an infant. Some ready-to-feed formulas come in bottles that can accomodate disposable nipples—all you need to do is screw a nipple on, feed and discard.
• Preparing concentrate formula: To prepare a baby body with this liquid formula, you’ll need to add water. It’s important to read the directions to learn the right ratio of water to concentrate. As for what type of water should you use, that depends on where you live, your pediatrician’s recommendation and your own wishes. If your tap water is safe, feel free to use it—just run it for several minutes before you fill the bottle to remove any trace contaminants in the water. You can also use filtered water, bottled water or boiled (and cooled) tap water.
• Preparing powdered formula: Just like concentrate, it’s important to follow directions on the right ratio of scoops of powder to ounces of water, says Carmen Baker-Clark, an International Board Certified Lactation Consultant (IBCLC) in Hoboken, New Jersey. When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
Regardless of what kind of formula you choose, Baker-Clark recommends sticking with the same brand or being deliberate as you try new ones, instead of just using whatever formula is on sale. While all infant formulas are regulated by the FDA and must pass the same nutrient tests, babies may react differently to various brands of formula. If an infant has frequent reflux, crying episodes or seems uncomfortable after a feeding, speak with your pediatrician. Your child may have an allergy or intolerance and may need a special formula.
Whether you warm the bottle up is up to you. “Many infants have no problem taking a cold bottle and the advantage is that you then don’t need to warm a bottle when you’re on the go,” Baker-Clark says. Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
How to make a baby bottle with breast milk
Preparing a bottle of breast milk is of course much more straightforward, since the milk itself is ready to go. But when grabbing a bag of breast milk to use, it’s important to keep an eye on when it was pumped and how it’s been stored since. According to breast milk storage guidelines, it’s safe to use freshly pumped milk that’s been stored at room temperature for up to four hours, in the fridge for up to four days or in the freezer for up to 12 months. Always use the oldest milk first. If baby doesn’t finish a bottle, you can offer it again within two hours of the last feeding.
Before giving baby the bottle, you can warm the milk up by placing the bottle (or milk storage bag) in a cup of warm water for a few minutes, or pop the bottle into a bottle warmer. Whatever you do, steer clear of the microwave, which can cause dangerous hot spots.
Best Bottle-Feeding Positions
How you hold your little one during a feeding is a crucial part of knowing how to bottle-feed a baby properly. Chances are, you’ve come across loads of images of parents bottle-feeding babies—but the positions you sometimes see in photos or on TV may not actually be the best for baby. For one, forget about laying baby across your lap. “Have you ever easily drank something while you lay on your back?” O’Day asks. (Answer: no.) “It’s the same for baby.” Not only can a back position lead to reflux, but it may also cause ear infections. Try these bottle-feeding positions instead:
• Cradle baby in your arms. This is the classic position you probably think of when you imagine giving baby a bottle. In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
• Hold baby upright. Instead of lying down, baby should be almost in a seated position, with his head on your chest or in the crook of your arm. “This position can work especially well for infants who have reflux,” Baker-Clark says. Tilt the bottle so the milk completely fills the nipple, since a nipple filled only halfway with milk may lead to baby gulping some air, which can lead to gassiness or reflux.
• Use a pillow. A nursing pillow can be helpful in keeping baby’s chest and head propped up at an angle. Bonus: It can give your arms a break too as you cradle baby in your lap.
• Switch sides. Regardless of whether you’re breastfeeding or bottle-feeding exclusively, switching baby from one side to another can help prevent your little one from developing a side preference and can give your arms a break. Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
As baby gets older, she may toy with holding the bottle. That’s fine, if she wants to, but it’s not a developmental milestone. “She may want to hold the bottle at 6 months, so you can let her, but you should still be close by, holding her and supervising her,” O’Day says. And if baby doesn’t show any interest in holding her bottle? As long as she’s reached other developmental milestones, like reaching or grasping for toys, it’s totally normal if your older infant wants his bottle served to him.
What is Pace Feeding?
You may have heard of “pace feeding” and wondered how to bottle-feed a baby using this method. “Paced bottle-feeding is where you follow baby’s cues and allow for breaks,” Baker-Clark says. “Taking the bottle away and re-offering it benefits both breastfed and exclusively bottle-fed babies.”
Pace feeding helps babies learn to regulate their hunger and allows ample time for digestion. It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
Plus, paced bottle-feeding makes a feeding session—which can last about 15 to 20 minutes—a great time for baby and his caregiver to bond. Here, some tips for how to pace feed:
• Hold the bottle at a horizontal angle. When the bottle is held horizontally, baby has to work to pull milk from the bottle, instead of the milk dripping into her mouth.
• Give baby some breaks. Instead of pulling the bottle away from baby’s mouth, lean the bottle back so the milk leaves the nipple. That way, baby has a chance to catch his breath. If he seems like he’s still rooting for milk, offer him more.
• Burp mid-feed. “If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
“If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
How to Get Baby to Take a Bottle
Even if you’re planning to exclusively breastfeed, at some point you’ll likely need some pointers on how to get baby to take a bottle. “I tell my clients to introduce baby to a bottle once breastfeeding has been established, which depends on each mother-baby dyad, but on average, it’s around one month,” O’Day says. “Even if they’re not planning to regularly bottle-feed, doing so can give peace of mind if an emergency comes up, and can also be a way for mom to get a break.”
Some babies take a bottle no problem—after all, sucking is an instinctive reflex, which is why bottle-fed babies tend to get the hang of it in the first few days of life. But other breastfed babies may initially be reluctant to take a bottle. And sometimes breastfed babies have no issue taking a bottle when they’re one month old, but if a bottle hasn’t been regularly offered, by 3 or 4 months of age, they’re less happy to accept a bottle. Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
• Offer often. Even if you’re breastfeeding, O’Day recommends giving baby at least one bottle a week, once breastfeeding has been established. “That way it’s part of their routine, so they’re less likely to resist it,” she says.
• Don’t offer it when baby is starving. If you’re regularly nursing your infant, O’Day suggests offering a bottle in between nursing sessions. “If they’re too hungry, they may be too worked up to take a bottle. If they’re calm and not super hungry, they may take it,” she explains.
• Let others try bottle-feeding. Some moms have success leaving the house and allowing their partner to try feeding baby a bottle. Again, try it at a time that’s not baby’s “must-feed” time.
• Don’t get frustrated. If baby isn’t taking the bottle, O’Day suggests putting it down and trying again later rather than forcing it, which can make both you and baby upset.
• Ask for help. A lactation consultant can suggest some techniques to help get even the most resistant bottle-feeders to accept a bottle. They may check your infant’s mouth and tongue for any latch problems that could contribute to the difficulty, suggest the best bottle for your infant, troubleshoot any behavioral issues or offer alternate nutritive methods, such as cup- or syringe-feeding.
When to Wean Baby Off the Bottle
The American Academy of Pediatrics recommends parents stop offering bottles by 18 months due to tooth decay concern, but it’s smart to talk with your pediatrician about exactly when baby should wean from the bottle around the 9-month mark, O’Day says. “How and when to wean depends on how much table food baby is eating, any developmental concerns and your pediatrician’s assessment,” she says. Note, though, that cow’s milk shouldn’t be introduced until baby is 12 months old.
When baby is around 6 months old, offer a sippy cup or straw cup for water, O’Day says, since learning to drink from cups can help make the transition from bottles seamless. Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Whether you’re breastfeeding and offering the occasional bottle, combo-feeding or exclusively bottle-feeding, you might hit some bumps along your bottle-feeding journey. But there are ways to navigate through any problems that arise. If you’re struggling to find the best baby bottle for your child, need some pointers on how to bottle-feed a baby in an optimal position or encounter a full-on bottle strike, reach out to your pediatrician or lactation consultants for guidance.
Published August 2018
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
14 Best Bottles for Every Feeding Need
Pumping 101: How to Pump Breast Milk
The Best Baby Formulas for Your Child’s Needs
How to properly bottle feed
Feeding your baby is not only an important process for healthy growth and development, but also a way to establish close emotional contact with the baby and build trusting and loving relationships. The transition from breastfeeding to bottle feeding should be carried out after the mother and the child are fully prepared for this. We are talking about both the moral aspect, and about choosing the right bottle and getting adults the necessary skills so that eating brings only positive emotions and benefits to the baby. In this article, we will talk more about how to properly bottle feed your baby and where to start. nine0003
How to prepare your baby for bottle feeding
If this method of feeding is a completely new experience for the baby, or if parents decide to bottle feed their baby from a very young age, slow flow nipples should be preferred. So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
Feeding bottle selection and daily care
All baby accessories should be kept clean and sterilized regularly and thoroughly.
There are several ways to sterilize dishes:
- select the appropriate mode when using the dishwasher;
- or place the bottle and teat in a vessel of boiling water for 5 minutes.
Before using this method of cleaning the bottle, make sure that the material it is made of can be exposed to high temperatures. Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles. nine0003
The need for thorough cleansing of everything that the baby will touch is caused by the fact that in the first months of life, the child's immune system is just beginning to strengthen. Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
How to bottle feed your baby
Before starting a meal, mom or dad should wash their hands well with soap and warm running water. Particular attention should be paid to the area between the fingers and under the nails. The hand washing process should take at least 20 seconds. And after carrying out this hygienic procedure, hands should be wiped dry with a paper towel or clean towel. nine0003
The next step is to prepare for the meal. If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
Breast milk is the most beneficial for a newborn. Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture. nine0003
Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture. nine0003
In the first six months after birth, cow's or goat's milk or its substitute in the form of soy milk should not be included in the baby's diet. Valid options for supporting healthy development of a newborn are breast milk or formula milk only.
What temperature should the bottle filler be? Under no circumstances should the bottle be heated on the stove or in the microwave. If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method:
- put a saucepan on the stove with a little water;
- bring the water to a boil, then remove the pan from the heat;
- place a bottle of milk in a vessel and heat it up to 37◦С;
- check the temperature with a pre-cleaned thermometer or a special device for measuring the temperature of foodstuffs.

You can also check the temperature of the ready-to-use bottle as follows:
- turn the bottle over;
- drip several times into your wrist area.
In this way, you can check not only the temperature of the milk or formula, but also how well the liquid flows out of the bottle. If you have to shake or squeeze the bottle hard to drip, the nipple is blocked and needs to be cleaned out. If, on the contrary, the filler pours out when the bottle is turned over, this means that the nipple is damaged and another nipple should be used to feed the baby, having previously sterilized it. nine0003
How to bottle feed your baby lying down
There are several techniques for feeding your baby. However, it is the feeding of the child lying down from the bottle that young parents consider the most comfortable. It is worth noting that eating in this position will only be safe when the baby's head is slightly raised. Otherwise, the child may simply choke. In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest. nine0003
In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest. nine0003
Make sure that the feeding bottle is closed correctly: the ring at the connection of the nipple to the bottle must not be too tight. Air must enter the bottle, otherwise a vacuum will be created there, which, in turn, will complicate the consumption of food for the child.
How to bottle feed without spitting up
Since the newborn is not able to fully control the process of feeding, along with milk, he can also take in air. This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding. nine0003
As soon as you notice that the baby has stopped sucking on the pacifier, is tired or thoughtful, pick him up and press his face to you, holding his head and back. To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
The air will quickly rise up and the baby will burp it without any extra effort. However, you should be prepared for the fact that, along with the air, part of the consumed mixture or milk may also return. Therefore, before taking the baby in your arms, cover yourself with a diaper, because it will be easier to wash it than clothes. nine0003
Never leave your baby alone with the bottle or let him fall asleep while using it. After eating, mom or dad must help their child burp. This will help to avoid colic, bloating and other manifestations of stomach discomfort.
Where to buy baby accessories
It's safe to say that I Love Mommy online store is one of the best places to buy baby food. Our catalogs feature products from world-famous brands, the quality of which you will not have to doubt for a minute. Bottles, baby dishes, pacifiers, baby bibs - all this and much more you can buy for your son or daughter from us at affordable prices in just a few minutes. nine0003
nine0003
Bottle feeding | Canpolbabies.com
Find out how to bottle feed your baby safely, how to help your baby feel safe while feeding, and how to set feeding times based on your baby's needs.
The most important thing is to choose the right position when feeding
When bottle feeding, avoid lying down as the milk flows out of the bottle under the force of gravity (at a constant speed controlled by alternating pressure on the nipple). nine0003
An infant may choke on milk if fed in a horizontal position. Therefore, it is very important to choose the right - more upright - position for feeding (the baby's head should always be slightly higher than the rest of the body).
Your baby's head should be in the crook of your arm, in line with his spine. The bottle feeding position should resemble the natural feeding position - especially when you feed him with two different feeding methods. nine0003
Remember:
- Never leave your baby alone with a bottle as they may choke
- Never let a baby sleep with a bottle in his mouth
How to give your baby a bottle
Put the bottle in your baby's mouth so that it forms a right angle with his face. Your baby should not encircle the entire nipple with his lips, but only its oblong part, while the lips should rest against the rounded part. The oblong part should always be full of milk. Otherwise, the baby will swallow a lot of air during feeding, which can cause colic. Air bubbles in the bottle mean your baby is suckling properly. nine0003
Your baby should not encircle the entire nipple with his lips, but only its oblong part, while the lips should rest against the rounded part. The oblong part should always be full of milk. Otherwise, the baby will swallow a lot of air during feeding, which can cause colic. Air bubbles in the bottle mean your baby is suckling properly. nine0003
Emotional connection
Young children need parental love and affection. Your closeness helps him feel safe. Therefore, it is very important to talk affectionately with the baby as often as possible, hug and stroke him. Feeding is the best time to build an emotional relationship with your baby.
This is very easy to do when you are breastfeeding because you are already in physical contact with each other. However, bottle feeding also allows you to be closer to your baby as he feels the warmth of your body. Bottle feeding also allows other family members - the father, brothers and sisters to get closer to the child, since not only the mother can feed the baby in this way. nine0003
nine0003
Calm emotional background
Never feed your baby when you are irritated or tense. Take some time for yourself first, take a deep breath and try to relax. When you have calmed down, sit in a comfortable chair, place a pillow under your arm, place your baby on the pillow, and start feeding while speaking gently to your baby. Your child feels your emotions. If you are tense, he will also feel restless. Also, never feed your baby when he is excited, crying or screaming. When he is in this state, his airways are not protected and food can enter his larynx instead of his esophagus. nine0003
Feeding by the hour
Formula milk is not as easily digested by the baby's stomach as breast milk, so according to generally accepted rules, it should be given every 3 hours.
Some pediatricians say it's best to give your baby formula on demand, that is, when the baby is hungry. In their opinion, it is better to feed the child than to wait another hour and keep him in suspense because he wants to eat. However, you still need to control the number of feedings and your baby's weight gain. nine0003
However, you still need to control the number of feedings and your baby's weight gain. nine0003
During the first month of life, the baby should eat > 7-8 times a day, 90-100 ml for each feeding, in the second month of life: 6-7 times a day, 100-120 ml for each feeding. During the first six months, the baby should gain approximately 150-200 g per week.
Feeding breaks
When your baby suckles milk from a bottle, he also swallows air. Therefore, he may feel full even before he drinks half the bottle. When feeding a child, breaks should be taken every few minutes to allow the baby to take in air - after such a break, he should ask for food again. During feeding, hold the baby in an upright or semi-recumbent position for a while (sometimes even for several minutes) to give him the opportunity to release air accumulated during feeding from the digestive tract. Help the child by holding him on your shoulder, putting his hands on your back. Bend and spread his legs a little.![]()