Feeding babies too early
Risks of introducing solids too early or too late
The gradual addition of solid foods to your baby’s diet is an exciting transition for your baby and you. Eating solids is just one of the many steps your baby will take toward greater independence. Between 4 and 6 months of age, babies start to observe and mimic their parents’ or other caregivers’ eating habits—a sign that they’re getting ready to advance to complementary foods.
What experts say about when to introduce solids
Babies should be breastfed exclusively for about the first 6 months of life, according to trusted health authorities like the American Academy of Pediatrics (AAP). During that time, breast milk (or infant formula) provides all the calories and nutrients your baby needs.
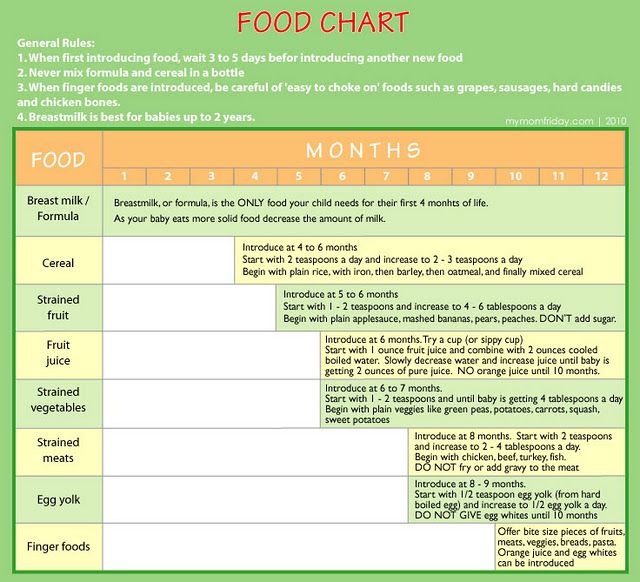
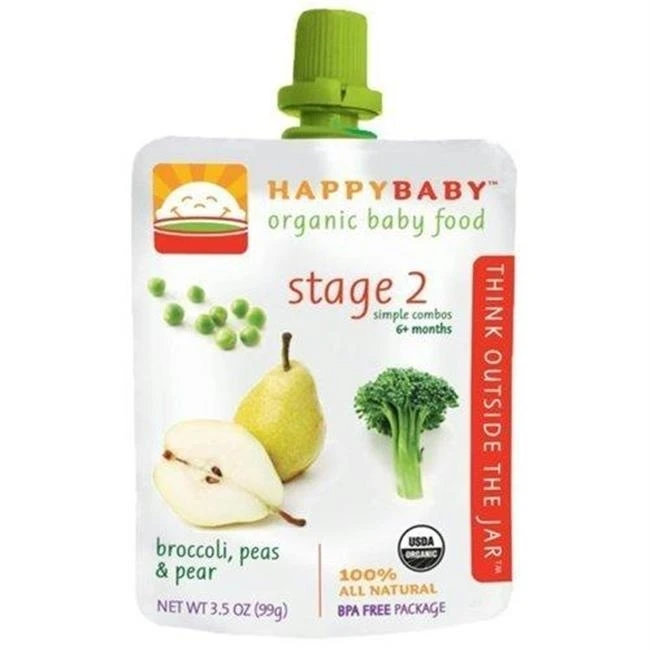
Around 6 months, you can start introducing solids. Some babies may be ready for solid foods a bit sooner (4-6 months) and others a bit later (6-8 months). As with all milestones (sitting, eating solids, crawling, etc. ), parents are always urged to watch their baby, not the calendar.
Once your baby starts solids, the AAP recommends that breastfeeding continue for at least the first year of life, and beyond, as mutually desired by mother and baby. If your baby is drinking infant formula, she should continue doing so until about 12 months of age. (Consult your child's health care provider before transitioning to cow's milk, and remember, children under the age of 1 should not be given fruit juice.)
Why the timing of solid foods matters
Introducing solids too early or too late can make a difference. Introducing solids before 4 months of age can increase the risk of choking and cause your infant to drink less than the needed amount of breast milk.
But introducing solids too late can increase the risk of your child developing allergies. One study found that late introduction of solid foods (after 7 months of age) may actually increase the risk of food allergies, suggesting a window of opportunity when it comes to starting solids. (A 2007 AAP report notes that breastfeeding is the best protection against allergic disease.)
(A 2007 AAP report notes that breastfeeding is the best protection against allergic disease.)
Why 6 months of age is ideal for beginning solids
Human milk provides all the nutrients (including iron) that babies need for about the first 6 months of life. Once the iron stored in your baby's liver during pregnancy is used up (at about 6 months of age), iron-rich foods such as meats or iron-fortified cereals need to be added to your baby’s diet. Around 6 months is also when most babies show signs that they are developmentally ready solid foods, so be sure to watch for the following:
- Your baby shows an interest in food others are eating.
- Your baby sits up with little or no support.
- Your baby holds her head up.
- Your baby picks up soft foods.
- Your baby puts those foods in her mouth.
- Your baby keeps her tongue in the bottom of her mouth and accepts a spoon.
- Your baby keeps food in her mouth and swallows rather than pushing it out with her tongue.

- Your baby indicates fullness by turning her head away or refusing to open her mouth.
If your baby makes no effort to pick up foods and feed herself or reacts negatively to a spoon touching her lips, she’s likely telling you she’s not yet ready for solid foods. Consider trying a different food. If she still refuses, wait a few days and try again.
For more on introducing solids, including which foods to offer first, read this.
Last updated December 28, 2021
Over half of American babies are given solids too early
A recent study that investigated when infants are first given solid foods has found that more than half of babies receive non-milk products earlier than recommended.
Introducing babies to complementary foods, or anything other than breast milk or formula, too early can mean that a baby may miss out on important nutrients from milk.
Similarly, if complementary foods are introduced too late, there is an increased risk of allergies, micronutrient deficiencies, and a poorer diet during adulthood.
For these reasons, it is vital that guidelines are correct, understood, and adhered to by the majority of the population.
In the past 60 years, recommendations have shifted significantly. In 1958, for example, guidelines were released saying that babies should be introduced to complementary foods in their third month of life.
In the 1970s, however, this was pushed back to their fourth month. And in the 1990s, the timing was pushed back further to 6 months old, which is where it stands today, according to the American Academy of Pediatrics.
Given these fluctuations, the lack of adherence to current guidelines is perhaps unsurprising.
A study published this week in the Journal of the Academy of Nutrition and Dietetics delved into data from the 2009–2014 National Health and Nutrition Examination Survey. The researchers wanted to explore whether or not the current 6-month guideline was being adhered to.
The team was led by Chloe M. Barrera, of the Division of Nutrition, Physical Activity, and Obesity at the National Center for Chronic Disease Prevention and Health Promotion at the Centers for Disease Control and Prevention (CDC) in Atlanta, GA.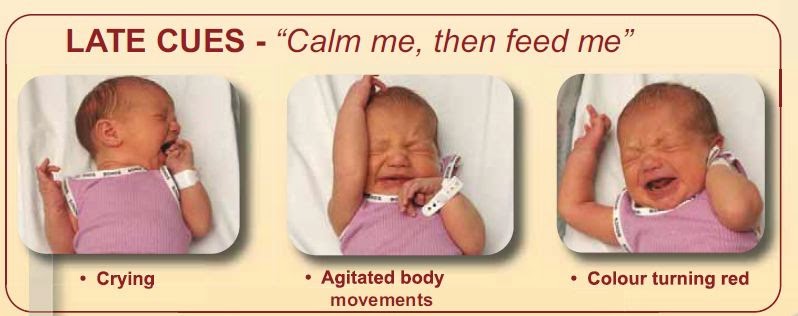
In total, data were taken from 1,482 children aged 6–36 months. Information was gathered through household interviews: the parent or guardian was asked at what age the child was given anything other than breast milk or formula. This includes sugar water, cow’s milk, and baby food.
The researchers found that only 32.5 percent of babies in the United States were introduced to complementary foods at around the 6-month mark. And, more than half of infants (54.6 percent) were introduced to complementary foods before 6 months of age.
Breaking it down still further, 16.3 percent received complementary foods before 4 months, 38.3 percent at 4–5 months, and 12.9 percent at 7 months or older.
Babies who were not breast-fed, or who were breast-fed for 4 months or under, were more likely to be introduced to complementary foods earlier than 6 months. This link remained significant even after controlling for various factors, including sex of the baby, age of mother, race, and smoking during pregnancy.
The findings give a snapshot of the current state of compliance in the U.S. Earlier studies found that 20–40 percent of children were introduced to complementary foods before 4 months.
However, these studies did not use a nationally representative sample, and some of them are now a decade old, which might explain the substantial differences in their findings.
Additionally, the older studies did not take into account the introduction of fluids other than milk or formula; they only focused on solids. This distinction is important, as the authors explain:
“The timing of when non-milk liquids are introduced is important to consider, as early introduction of non-milk liquids is thought to compromise adequate intake of nutrients that come from breast milk and infant formula, and reduce the duration of breast-feeding among breast-fed infants.”
The findings mark the first study to have looked at this question using a nationally representative dataset, and there is still a worrying deviation from the guidelines.
As the authors explain, “Efforts to support caregivers, families, and healthcare providers may be needed to ensure that U.S. children are achieving recommendations on the timing of food introduction.”
For the very first time, the U.S. Department of Agriculture and Department of Health and Human Services are writing federal dietary guidelines for children under 2 years of age. Barrera and colleagues hope that this might help to rectify the situation.
They write, “Inclusion of children under 2 in the 2020–2025 Dietary Guidelines for Americans may promote consistent messaging of when children should be introduced to complementary foods.”
Hopefully, as the message becomes clearer and the guidelines are disseminated more thoroughly, the gap between recommendation and reality will steadily close.
Pediatricians agreed on what to feed children from one to three years old - Picture of the Day - Kommersant
pediatricians and nutritionists. Based on these studies, the National Program for Optimizing Children's Nutrition has been developed. Her recommendations are planned to be included in the programs of higher and postgraduate medical education, as well as to familiarize teachers and psychologists with them. nine0003
Her recommendations are planned to be included in the programs of higher and postgraduate medical education, as well as to familiarize teachers and psychologists with them. nine0003 Photo: Svetlana Privalova, Kommersant / buy photo
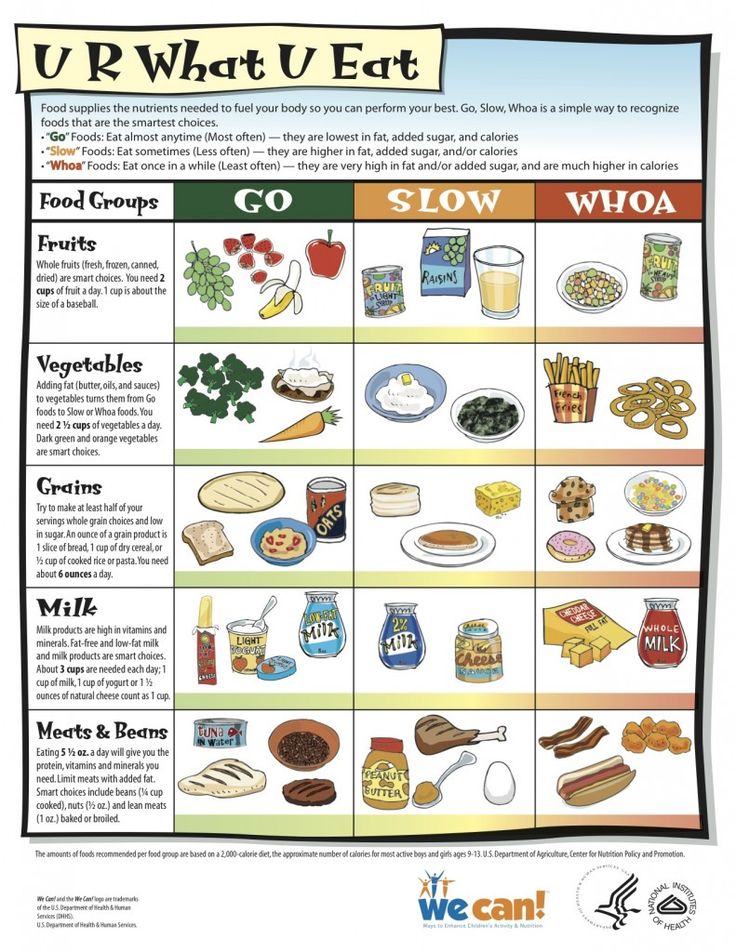
Pediatricians and nutritionists presented the National Nutrition Program for children from one to three years old. It was developed by 40 Russian specialists under the guidance of the chief nutritionist of the Ministry of Health Viktor Tutelyan and the chief pediatrician of the Ministry of Health Alexander Baranov. The appearance of the program was preceded by studies that showed that the nutrition of most Russian children is unbalanced: it is dominated by proteins and fats, lacking vitamins, calcium, and iron. At the same time, children are transferred too early to the so-called adult table and begin to be fed with non-children's food - chocolate, fast food, dumplings, sausages, ketchup and mayonnaise. “Insufficient consumption of vegetables and fruits is noteworthy: 70.9% of children in the second year of life and 65.9% of the third receive fruits daily, and only 46% and 35.4% receive vegetables daily, the study says. 48% of children in the second year of life receive meat at least seven times a week and 56% of the third year of life." At the same time, the average consumption of dairy products only half satisfies the need for calcium in children.
“Insufficient consumption of vegetables and fruits is noteworthy: 70.9% of children in the second year of life and 65.9% of the third receive fruits daily, and only 46% and 35.4% receive vegetables daily, the study says. 48% of children in the second year of life receive meat at least seven times a week and 56% of the third year of life." At the same time, the average consumption of dairy products only half satisfies the need for calcium in children.
Deputy Director of the Scientific Center for Children's Health of the Ministry of Health of Russia Leila Namazova-Baranova blamed both parents and doctors for the improper organization of children's nutrition: “Everything will go wrong if we recommend something to parents, but they do not recommend our recommendations perform. But if the doctor does not apply his knowledge in practice, then this will lead to the same effect. She noted that at the first stage of the program implementation, the main task will be to work with pediatricians: “We use this program for widespread implementation in pediatric circles and will try to implement the recommendations as quickly as possible in undergraduate and postgraduate education programs for doctors throughout the country. ” nine0003
” nine0003
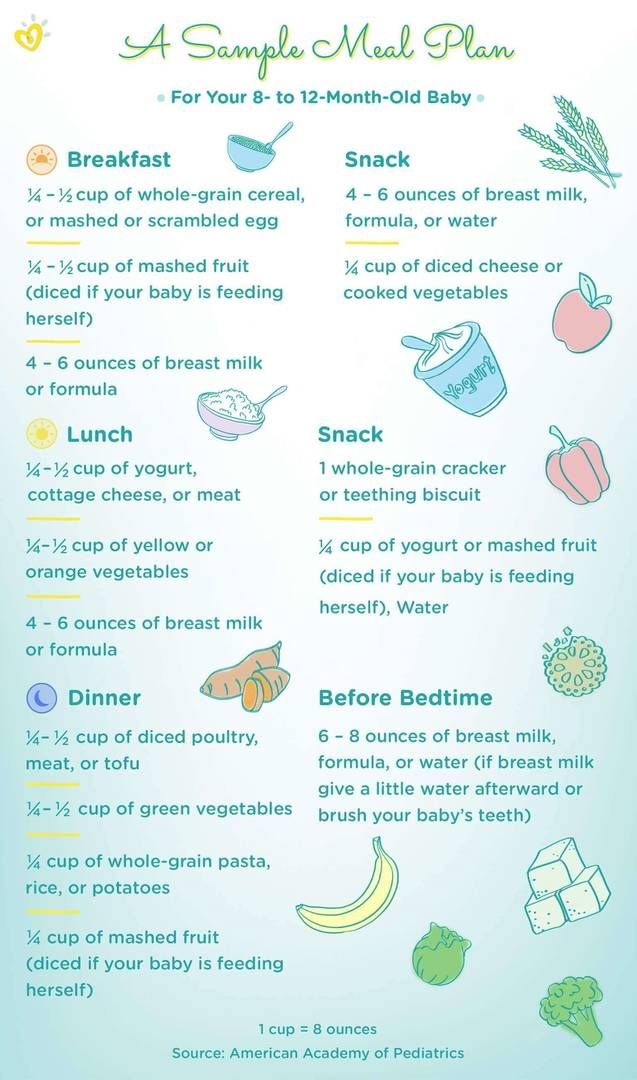
According to the presented recommendations, the daily ration of children from one to three years old should be divided into five meals - three main and two additional. It should include milk porridge, fruits, vegetable salads, dairy and sour-milk products, meat and fish dishes, vegetable oil, bread, and infant formula. “Now we all know that our diet is characterized by micronutrient deficiencies. Even if we and our children receive very high-quality, expensive products, it still remains. But mixtures specially designed for this age contain less protein, deficient vitamins and prebiotics, are not widely used, ”Tatyana Borovik, head of the healthy and sick child nutrition department at the Scientific Center for Children's Health, explained the recommendations for using mixtures. nine0003
According to her, the next step in the implementation of the program will be work with parents, they will develop recommendations on children's nutrition, and publish information materials.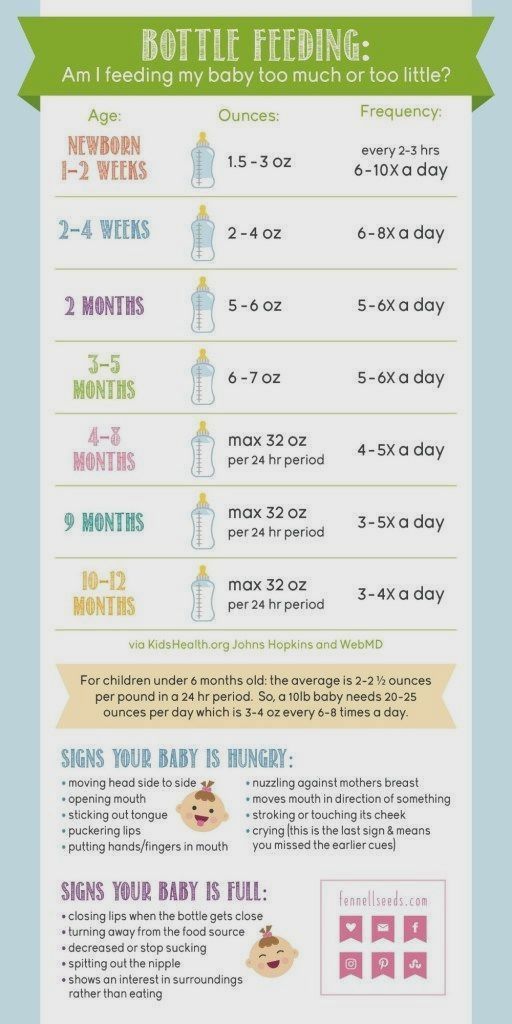 Irina Zakharova, Head of the Department of Pediatrics at the Russian Medical Academy of Postgraduate Education, said that in the course of the research, more than 90% of the parents surveyed stated that they were interested in the issue of children's nutrition, 80% were satisfied with the recommendations provided by pediatricians on nutrition, but only 45% followed them. nine0003
Irina Zakharova, Head of the Department of Pediatrics at the Russian Medical Academy of Postgraduate Education, said that in the course of the research, more than 90% of the parents surveyed stated that they were interested in the issue of children's nutrition, 80% were satisfied with the recommendations provided by pediatricians on nutrition, but only 45% followed them. nine0003
Valeria Mishina
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information nine0003
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not yet enough scientific evidence on this, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding. nine0003
There is not yet enough scientific evidence on this, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding. nine0003
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after birth. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How to feed your baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs. nine0003
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 The Calma Smart Soother was developed with input from breastfeeding experts at the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. nine0027 4 Preservation of natural sucking skills allows the baby to easily transition from breast to bottle and back.
2.3 The Calma Smart Soother was developed with input from breastfeeding experts at the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. nine0027 4 Preservation of natural sucking skills allows the baby to easily transition from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly. nine0003
nine0003
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children. nine0003
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible. nine0003
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature. nine0003
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding. nine0003
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much expressed milk should I give my baby? nine0025
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your breast pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk. nine0003
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, they will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast. nine0003
In general, in these cases, they say that the child confuses the nipple with the breast. nine0003
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a teat, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist. nine0003
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." Zh Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only.