Feeding newborn baby breastmilk and formula
How to Feed a Combination of Breast Milk and Formula
This guide was originally published on May 5, 2019 in NYT Parenting.
When I was a new mother, I heard so much about the advantages of breastfeeding over formula feeding that it felt like my only options were either breast milk or formula. So much so that it seemed like a revelation when I finally realized I could do both at the same time.
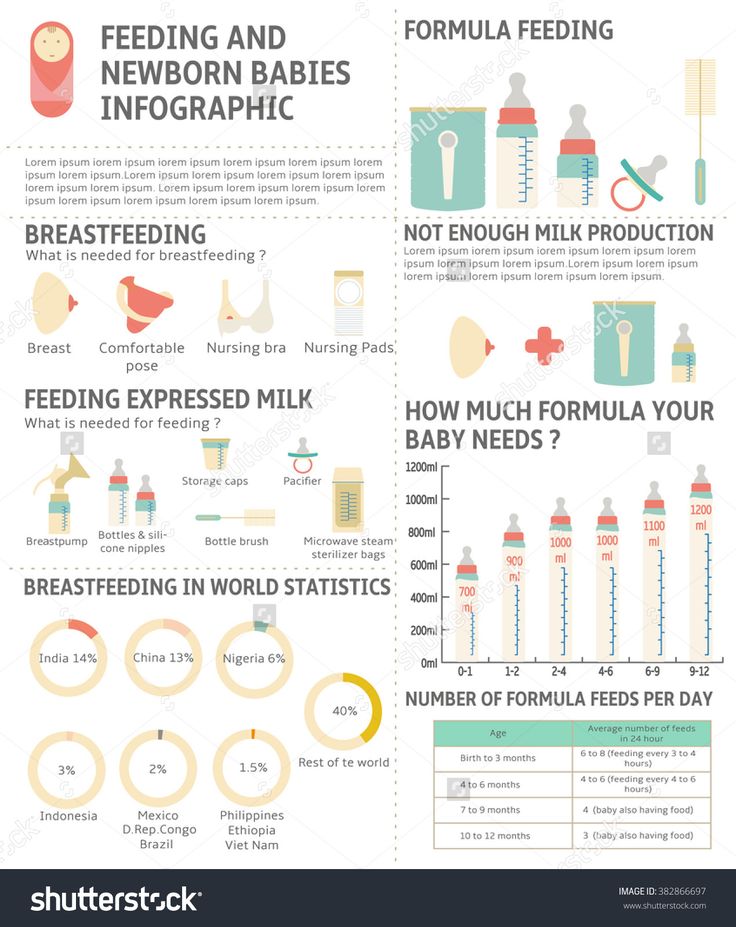
I was not alone in this realization, of course. Many women successfully combination feed — a practice that involves giving babies formula in addition to breast milk. According to the Centers for Disease Control and Prevention, one out of three breastfeeding mothers in the United States supplements her breast milk with formula by the time her baby reaches 6 months of age.
Many women find that their babies switch between breast and bottle and between breast milk and formula with ease. For others, there are hiccups along the way.
To help you get started combination feeding and manage any potential problems, I reviewed the published data and spoke with several experts, including Dr. Marianne Neifert, M.D., a pediatrician practicing in Denver; Freda Rosenfeld, a board-certified lactation consultant based in Brooklyn, N.Y.; and Dr. Michael Kramer, M.D., a professor of pediatrics at McGill University in Montreal.
[Read our guide on breastfeeding during the first two weeks of life]
What to do:
- Introduce a bottle early, but not too early.
- Start slowly, use the right nipple, relax and enlist help.
- Do not force your baby to bottle feed.
- When dealing with bottle refusal, be patient.
- Prevent uncomfortable engorgement, leaking and clogged ducts.
- Maintain your milk supply while giving formula.
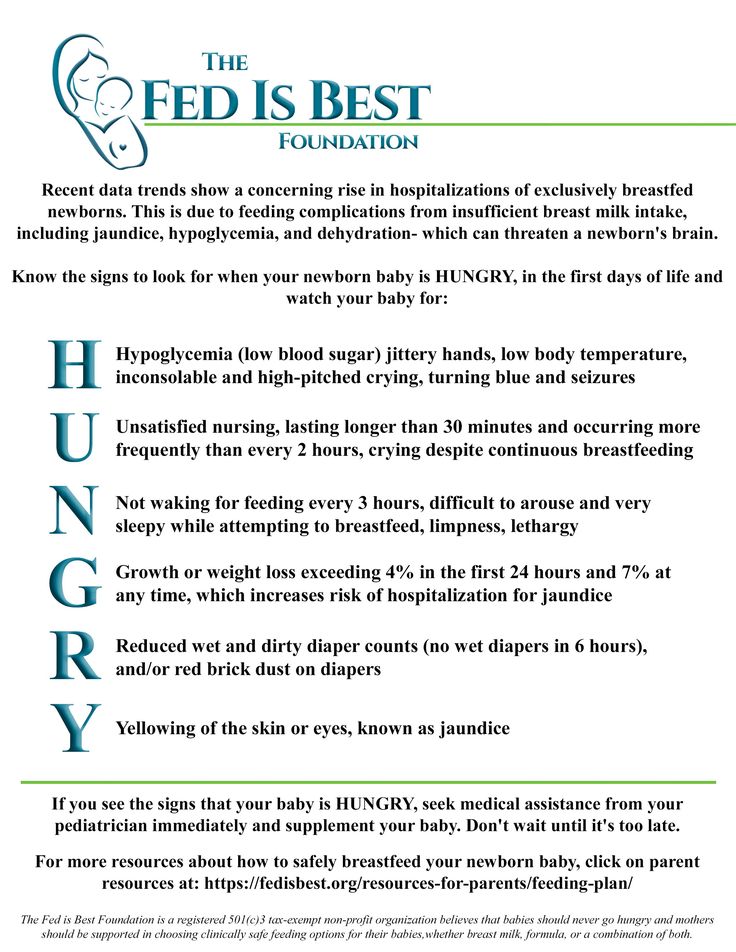
- Choose an iron-fortified formula.
The sweet spot for introducing bottles for full term babies is usually “between 2 and 6 weeks of age,” said Rosenfeld. If you do it before you and your baby are “in a groove with breastfeeding,” she warned, your baby may learn to prefer the faster, easier flow from the bottle and lose interest in the breast.
But even more important than age, according to Dr. Neifert, is whether “your baby is latching well, getting full feeds at the breast and gaining well.” Some babies get the hang of nursing sooner than others.
Once your baby is nursing effectively and gaining weight, however, don’t wait too much longer before introducing the bottle because the baby might reject it. Babies’ sucking reflexes typically start fading at around 6 to 8 weeks, so it’s best to introduce a bottle before this reflex has faded so your baby reflexively sucks on the bottle nipple.
Start by offering bottles filled with just a half ounce or so (of breastmilk or formula).
If your baby has been exclusively breastfed, Rosenfeld recommended starting with a wide, slow flow nipple that mimics the shape and flow of your own nipples, decreasing the chance that your baby will find it easier to get milk from a bottle than the breast.
A baby older than 3 months, however, may become frustrated with a slow flow bottle, especially if mom’s breasts have a fast flow, Rosenfeld warned. In that case, she recommended trying a faster flow nipple.
In that case, she recommended trying a faster flow nipple.
To ensure that baby is happy, relaxed and not too hungry, offer a bottle one to two hours after your baby’s last feeding. Crying is a late sign of hunger, and a hungry baby is easily frustrated.
If you are the first to offer the bottle, your baby may refuse and insist on nursing. (She knows who has the good stuff, after all.) Instead, ask your partner or another familiar caregiver to offer the first few bottles, if you can. This will not only help your baby get used to bottle feeding, but will help establish a feeding relationship with your partner (if you have one), too.
Whomever is giving the bottle should try to relax and follow your baby’s cues. Babies sense stress and may reject a bottle if the person offering it seems anxious.
If your baby refuses the bottle at first, do not force him to drink. Wait and try again later, an hour or two after their next feeding. Some studies have linked early overfeeding with an increased risk of later obesity.
“For most healthy, full-term infants, parents can look to their baby rather than the clock for hunger cues,” according to a webpage from the American Academy of Pediatrics. “This is called feeding on demand, or responsive feeding.”
When bottle feeding, watch for signs your baby has had enough: turning away, pushing away the bottle, spitting out milk, chewing on the nipple, gagging or falling asleep. (This video from the A.A.P. describes these signs in detail.)
Unlike breast milk, leftover formula in a bottle your baby has drunk from cannot be saved. Check out this A.A.P. guide to safely preparing formula.
Rarely, a breastfed baby will prove shockingly tenacious in refusing to take milk from a bottle. If after trying all of the above techniques your baby is still rejecting the bottle, or if your baby begins refusing the bottle after taking it previously, you can also try:
Distracting the baby. Try giving the bottle when your baby is calm and a little distracted, for example, by offering a bottle while taking a walk outside.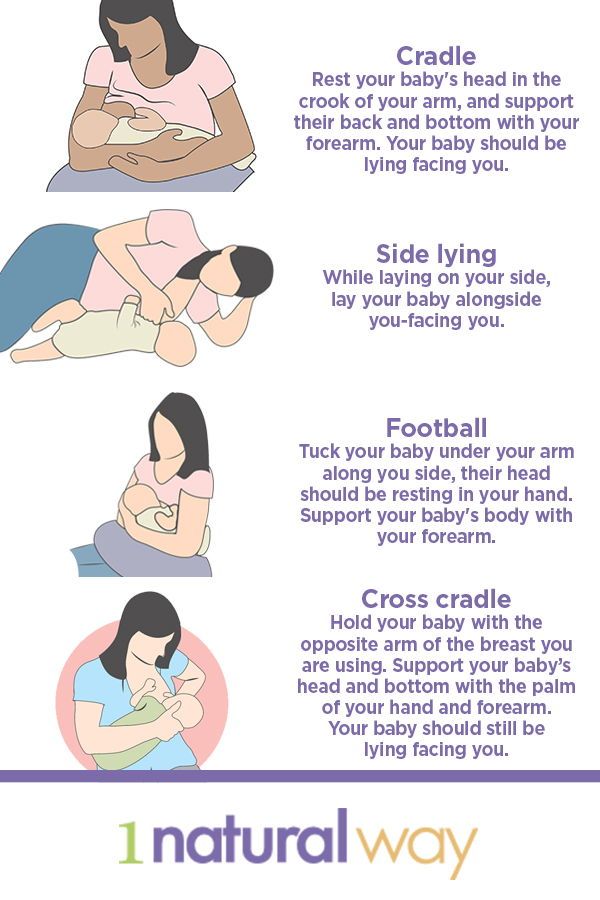
Heating things up. Try warming the milk and the bottle nipple, to make the experience more similar to feeding at your breast.
Offering a taste. Using a syringe, try dribbling a little milk into your baby’s mouth and then giving her the bottle. This helps trigger her drive to suck on the bottle.
Using music as a feeding cue. Rosenfeld recommended playing the same music while nursing and bottle feeding. This cues your baby that it’s time to eat.
Bypassing the bottle. If your baby is 6 months or older, try circumventing the bottle and weaning directly onto a cup.
When you start introducing formula, your breast milk production will take a few days to adjust to the reduced demand. In the interim, your breasts may become uncomfortably engorged, which can lead to embarrassing leakage, clogged ducts or even mastitis — a painful infection of the breast tissue.
Thus experts generally advise introducing formula slowly, gradually replacing breastfeeding sessions with formula feeding.
One method is to replace one nursing session per week with a formula feeding session. Start by giving your baby one bottle of formula at around the same time each day. This will train your body to stop producing milk at that time.
Another way to start introducing formula, according to the National Childbirth Trust, a nonprofit based in Britain, is the “top it off” method, which involves giving a small amount of formula (half an ounce to an ounce) after a nursing session. The extra nourishment will make your baby feel more full, extending the time until your next nursing session and gradually reducing the amount of milk you produce at that time.
If your breasts still become engorged, “you can relieve some of the pressure by pumping or hand expressing a little milk, but only until you feel relief,” said Dr. Neifert. She warned against “draining your breasts completely, as that signals to your breasts to continue to produce milk.”
[How to keep pumping when you return to work]
If you wish to maintain your milk supply while giving formula, you may need to breastfeed or pump frequently, up to 8 to 12 times per day.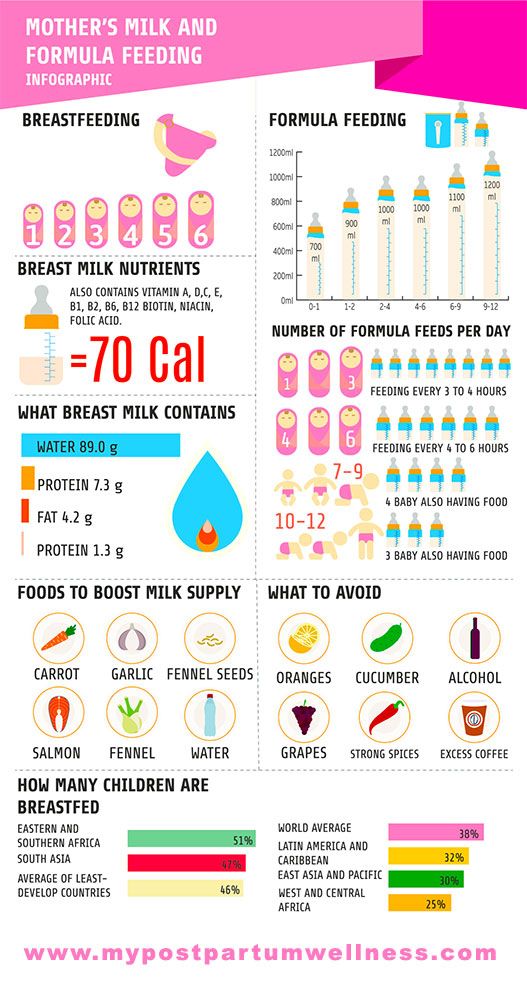 The exact number of times will depend on your breasts’ storage capacity and the age of your baby.
The exact number of times will depend on your breasts’ storage capacity and the age of your baby.
According to the N.C.T., if your baby is older — around 8 or 9 months — you can usually maintain your breastmilk supply alongside formula feeding, as long as you breastfeed every day.
The Department of Agriculture has tips for maintaining your milk supply while introducing formula.
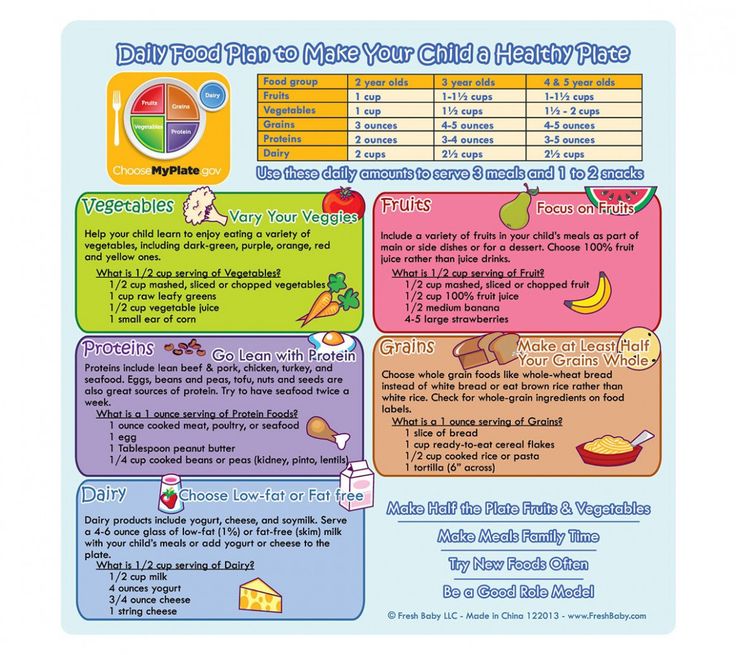
For healthy, full term babies who are partially breastfed, the A.A.P. recommends a cow’s milk-based formula that is iron-fortified. (Low-iron formulas raise your baby’s risk of anemia.)
Infants younger than 1 year should never receive regular cow’s milk or any other milk in place of formula or breast milk. Cow’s milk does not contain the proper balance of nutrients your growing baby needs.
A few babies, such as those with lactose intolerance, severe reflux or milk allergies may need a special formula. Talk with your baby’s pediatrician if you think your baby needs one.
If you need more help choosing a formula, consult The Wirecutter’s Guide to the Best Baby Formula. (The Wirecutter is a New York Times company that does rigorous product reviews.)
(The Wirecutter is a New York Times company that does rigorous product reviews.)
To breastfeed effectively, babies must open their mouth wide, latch on to the breast and then coordinate a suck, swallow and breath sequence. Bottle feeding, by contrast, provides a continuous flow of milk; instead of working to extract the milk, babies only need to pause the flow of milk in order to breathe.
Because of these differences, some babies will develop a strong preference for the bottle or, less often, for the breast.
Nipple confusion. Women sometimes receive dire warnings that artificial nipples, including pacifiers, can lead to nipple confusion — or an inability to latch on to the breast and effectively extract milk.
“ … these concerns [over nipple confusion] can cause significant stress for new mothers who are struggling with breastfeeding,” Dr. Chad Hayes, M.D., a pediatrician practicing in Charleston, S.C., wrote on his blog.
For example, La Leche League, a nonprofit focused on breastfeeding advocacy, warns that many mothers have “noticed a change in her baby’s sucking patterns after introducing a bottle or a dummy [pacifier]. Her baby may struggle and cry, find it difficult to latch on, or simply nurse ineffectively at the breast.”
Her baby may struggle and cry, find it difficult to latch on, or simply nurse ineffectively at the breast.”
Fortunately, according to Dr. Hayes, these fears are overblown. A recent meta-analysis of randomized controlled trials, for instance, found that among full-term babies, bottle feeding and pacifier use had no apparent impact on the duration of breastfeeding. After reviewing the research, Hayes concluded that “nipple confusion doesn’t seem to play a huge role in infant feeding.”
(Among preterm babies who, for health reasons, often need to start on bottles before breastfeeding is established, bottle feeding has been linked with a slightly shorter duration of exclusive breastfeeding.)
Flow preference. While true nipple confusion is rare, a more common cause of a baby fussing at the breast or refusing to latch is flow preference.
Flow preference occurs when your baby can still breastfeed effectively but prefers the fast, easy flow of milk from a bottle.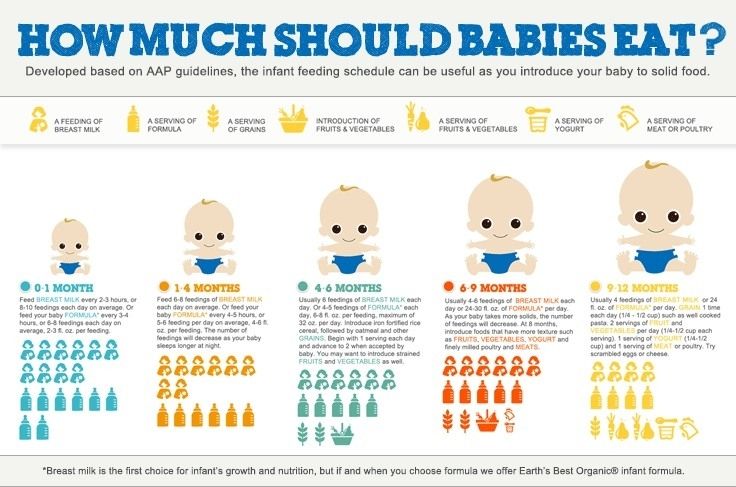 Babies who prefer bottles may fuss, cry or push you away when you try to nurse. Some babies may temporarily refuse to nurse at all, going on a nursing strike.
Babies who prefer bottles may fuss, cry or push you away when you try to nurse. Some babies may temporarily refuse to nurse at all, going on a nursing strike.
If this happens, La Leche League recommended hand expressing a bit before trying to latch your baby onto your breast. This helps to reduce engorgement and to get the milk flowing, so that your baby is rewarded with milk immediately after latching. The Australian Breastfeeding Association also offers several tips for handling breast refusal.
If your baby is still resisting breastfeeding, Rosenfeld recommended taking a bottle holiday for at least a week. When you reintroduce the bottle, you can try paced bottle feeding, a method of giving bottles designed to emulate breastfeeding. It involves sitting your baby upright or only slightly reclined, holding the bottle horizontally so your baby has to suck to extract milk from the bottle, and allowing for frequent pauses between gulps of milk.
If you are having persistent problems getting your baby to latch or to breastfeed effectively, seek outside help. The United States Lactation Consultant Association website can help you find a board-certified lactation consultant near you.
The United States Lactation Consultant Association website can help you find a board-certified lactation consultant near you.
The A.A.P. recommends that women breastfeed exclusively for about the first six months of life, and then continue breastfeeding while giving solid foods for at least a year.
Exclusive breastfeeding for six months — without additional solids or formula — provides the strongest protection against gastrointestinal and respiratory infections during infancy. But partial breastfeeding does still provide some protections against diarrhea, ear infections, Sudden Infant Death Syndrome and respiratory infections like pneumonia.
Note though, that “this protection against infection lasts only as long as you are breastfeeding,” said Dr. Kramer.
Some studies also suggest that breastfeeding can confer additional lifelong protection against obesity, eczema, asthma and allergies, as well as a slight boost in I.Q., though many of the studies showing these long-term benefits “have major methodological issues,” according to the A. A.P.
A.P.
Women sometimes hear that just one drop of formula will change a baby’s microbiome — the mélange of bacteria, fungi, and other microscopic bugs that line the skin and gastrointestinal system. Such changes, they are warned, may have lifelong consequences for their babies’ immune and metabolic health.
While formula-fed babies do have a different balance of bacteria in their gut microbiome, said Dr. Kramer, “we still do not know how this relates to later health.” And, Dr. Kramer added, many things, such as antibiotics, how they were born and the types of foods they eat, can also alter the microbiome.
Some popular breastfeeding websites also warn that using formula can “shorten the breastfeeding relationship.”
But this depends on your situation. I and many of my mom friends found that giving some formula helped us sustain breastfeeding by lessening its logistical, physical and emotional demands.
Cutting down on breastfeeding may cause your breasts to become engorged with milk, which can lead to clogged milk ducts.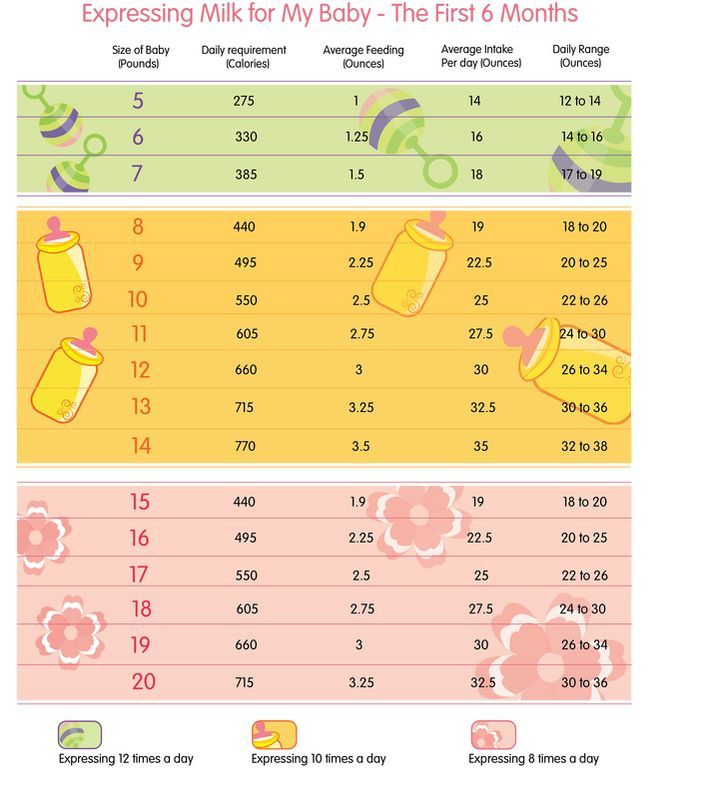 You may notice a hard, red and tender lump on your breast that feels warm to the touch. A clogged duct will often occur only in one breast.
You may notice a hard, red and tender lump on your breast that feels warm to the touch. A clogged duct will often occur only in one breast.
To help clear the duct, nurse and pump frequently to keep your breast from becoming full of milk. Massaging your breast and applying warm compresses while nursing or pumping may also help the duct clear and ease discomfort.
If you also develop shivers, chills or other flu-like symptoms, you may have mastitis, a serious infection of the breast tissue. Mastitis can come on suddenly and cause you to feel weak and achy. If you think you may have mastitis, contact your doctor right away; you may need antibiotics.
Amy Kiefer, Ph.D., is a freelance science writer and mother of three who blogs on pregnancy and breastfeeding for Expecting Science.
How to combine breast and bottle feeding
It can take several weeks for you and your baby to feel happy and confident with breastfeeding.
Once you've both got the hang of it, it's usually possible to offer your baby bottles of expressed milk or formula alongside breastfeeding.
This is sometimes called mixed or combination feeding.
Why combine breast and bottle?
You may want to combine breastfeeding with bottle feeding if you:
- are breastfeeding and want to use a bottle to offer your baby some expressed breast milk
- want to breastfeed for some of your baby's feeds, but give bottles of formula for 1 or more feeds
- are bottle feeding your baby and want to start breastfeeding
- need to leave your baby and want to make sure they have some milk while you're away
Introducing formula feeds can affect the amount of breast milk you produce. There is also a small amount of evidence to show babies may not breastfeed as well because they learn to use a different kind of sucking action at the bottle than at the breast.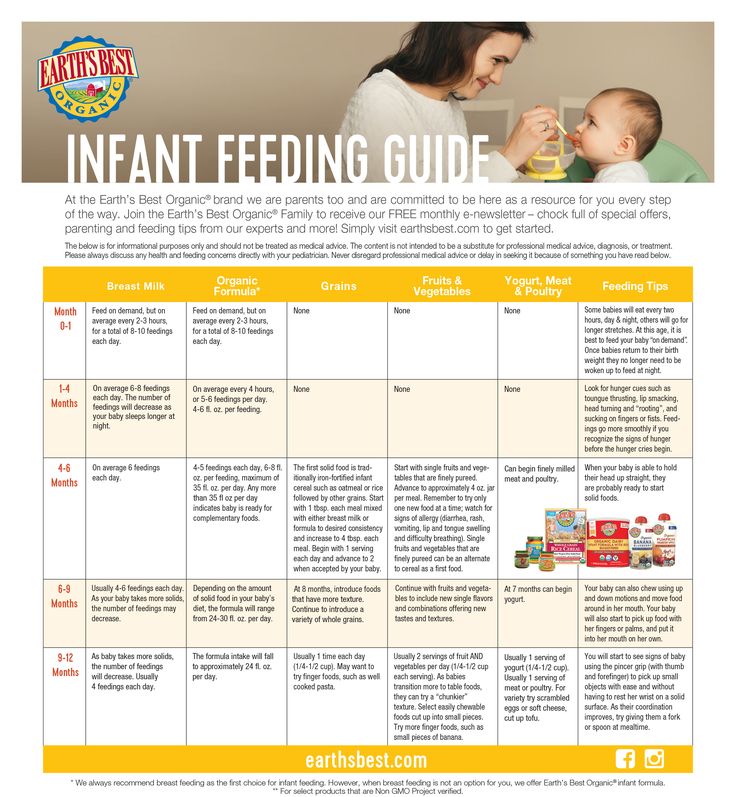
Introducing formula feeds
If you're combining breastfeeding with formula feeds both you and your baby can carry on enjoying the benefits of breastfeeding.
If you choose to introduce infant formula:
- it's best to do it gradually to give your body time to reduce the amount of milk it makes – this helps lower your chance of getting uncomfortable, swollen breasts, or mastitis
- if you're going back to work, start a few weeks beforehand to give both of you time to readjust
- if your baby is 6 months old or more and can drink milk from a cup, you may not need to introduce a bottle at all
For more information, see drinks and cups for babies.
Giving your baby their first bottle
It may take a while for a breastfed baby to get the hang of bottle feeding.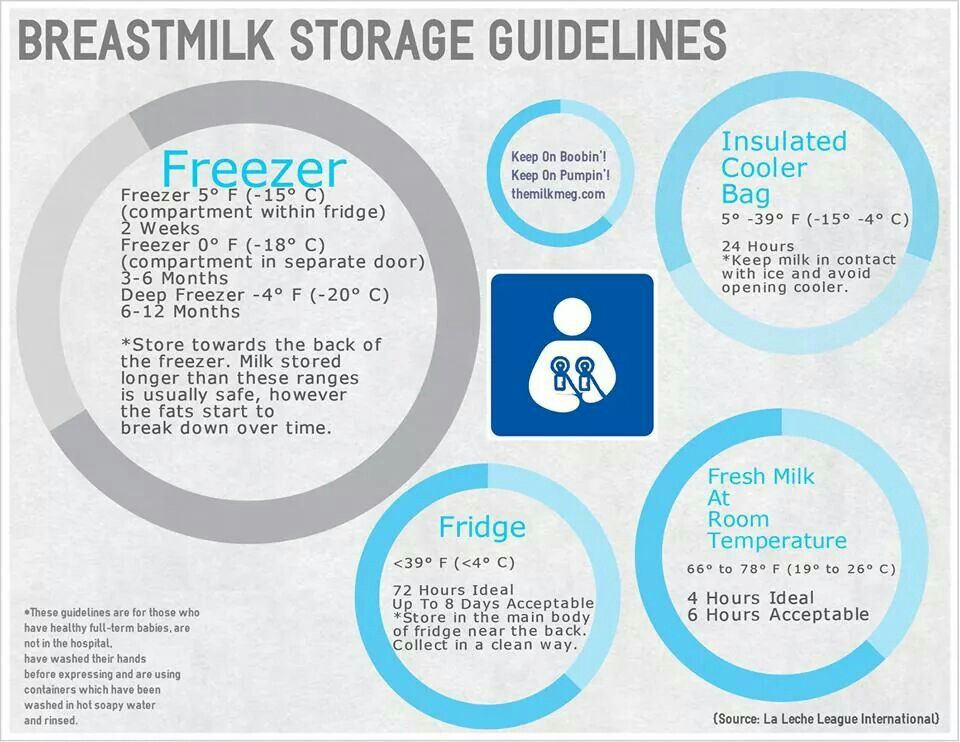
- it usually helps to give the first few bottles when your baby is happy and relaxed – not when they're very hungry
- it may help if someone else gives the first bottle feeds, so that your baby is not near you and smelling your breast milk
- you might want to try using a different position for bottle and breastfeeding
See more advice on how to bottle feed.
Breastfeeding more and giving fewer bottles
If you want to start breastfeeding more and give your baby fewer bottles, it's a good idea to ask your midwife, health visitor or breastfeeding supporter for support.
These tips may help too:
- Hold and cuddle your baby as much as possible, ideally skin to skin. This will encourage your body to make milk and your baby to feed.

- Express your breast milk regularly. Expressing releases the hormone prolactin, which stimulates your breasts to make milk. About 8 times a day, including once at night is ideal. It may be easier to express by hand to begin with – your midwife, health visitor or breastfeeding supporter can show you how.
- Try bottlefeeding while holding your baby skin to skin and close to your breasts.
- If your baby is latching on, feed often. Do not worry if your baby does not feed for long to begin with. See tips on how to get your baby properly positioned and attached.
- Choose times when your baby is relaxed, alert and not too hungry, and do not force your baby to stay at the breast.
- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid (supplementer).
 A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast. This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast. This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
See more tips on boosting your milk supply.
Help and support with mixed feeding
If you have any questions or concerns about combining breast and bottle feeding:
- talk to your midwife, health visitor or breastfeeding supporter
- call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm, every day)
- find breastfeeding support near you
Video: why combine breast and bottle feeding?
In this video, 3 mothers discuss ways to combine breast and bottle feeding.
Media last reviewed: 14 March 2023
Media review due: 14 March 2026
Page last reviewed: 30 March 2023
Next review due: 30 March 2026
Breast milk and formula: what do they have in common?
1 Cribb VL et al. Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B. , "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
, "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity." Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . - Hassiot F. et al.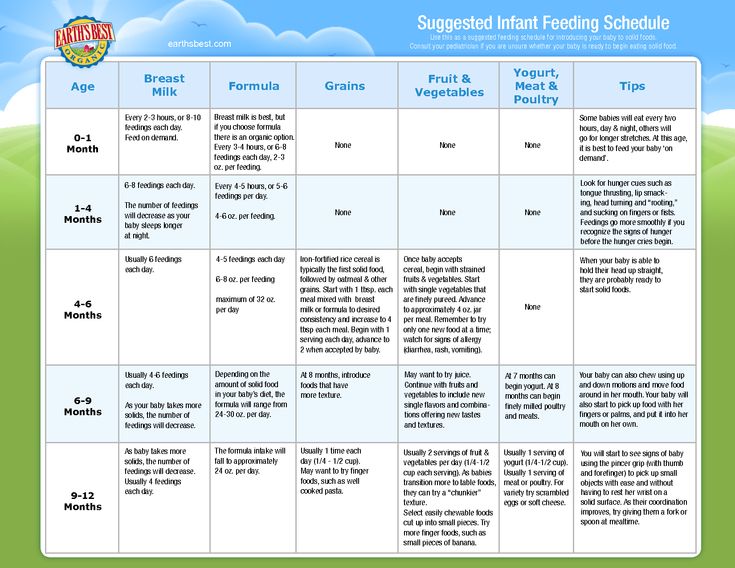 , "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
, "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86.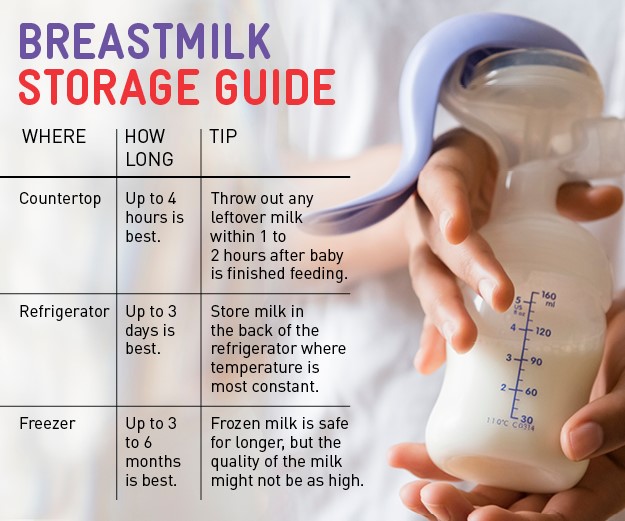 - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
- Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health. " Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
" Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr .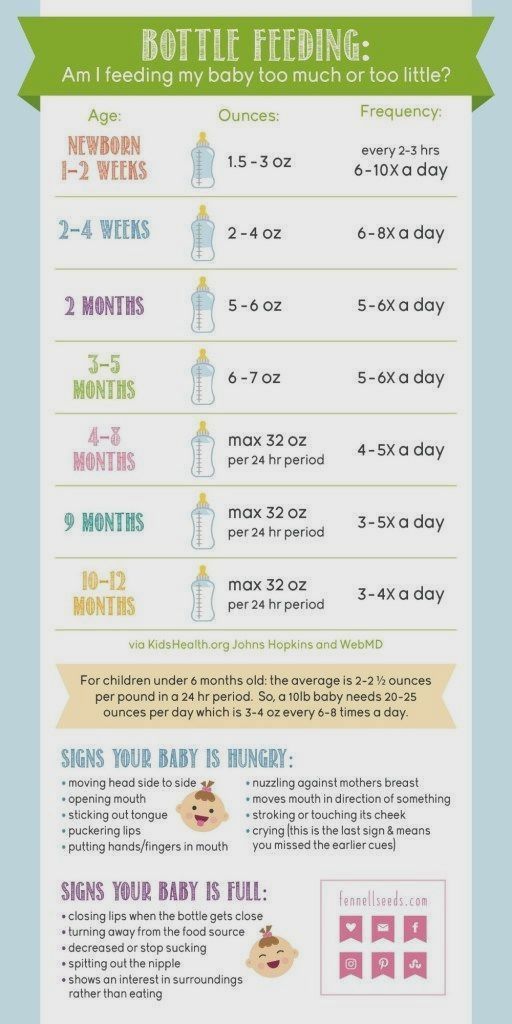 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263. - Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr . 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review. " JAMA Pediatrician. 2015;169(6):e151025.
" JAMA Pediatrician. 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatric. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas G Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration. " G Perinat Neonatal Nurs. 2007;21(3):200-206.
" G Perinat Neonatal Nurs. 2007;21(3):200-206.
33 Menella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics . 2001;107(6): E 88. - Menella J.A. et al., Prenatal and Postnatal Taste and Smell Recognition in Children. Pediatrix (Pediatrics). 2001;107(6):e88.
34 Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance. Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
Rules for mixed feeding - how to maintain lactation, choose a mixture and other questions.
— Polina Aleksandrovna, what is mixed feeding of newborns?
— With mixed feeding, the baby receives breast milk and milk formula in different proportions.
— When does the pediatrician recommend mixed feeding?
— The reasons why a pediatrician partially replaces natural nutrition with formula can be divided into three groups.
- Mother's lack of milk. Low lactation can lead to weight loss in a baby. With a pronounced lack of weight, additional nutrition is needed.
- Functional disorders in a child. For constipation, regurgitation, allergic reactions and other conditions, a therapeutic mixture is prescribed.
- Mom is away for feeding time. If there is no milk bank and it is impossible to form it, supplementary feeding is given.
— Some mothers refuse to breastfeed because of bad environment. Does the environment really affect the quality of breastfeeding?
— It cannot be said that the environment affects the quantity and quality of women's milk. Milk is filtered from the mother's blood. Blood passes through the vessels of the mammary gland and brings useful substances into breast milk, they are no longer taken from anywhere. At the same time, harmful substances from the environment are not allowed to enter the milk.
Due to poor ecology, the mother may be deficient in trace elements, and then the quality of milk will decrease.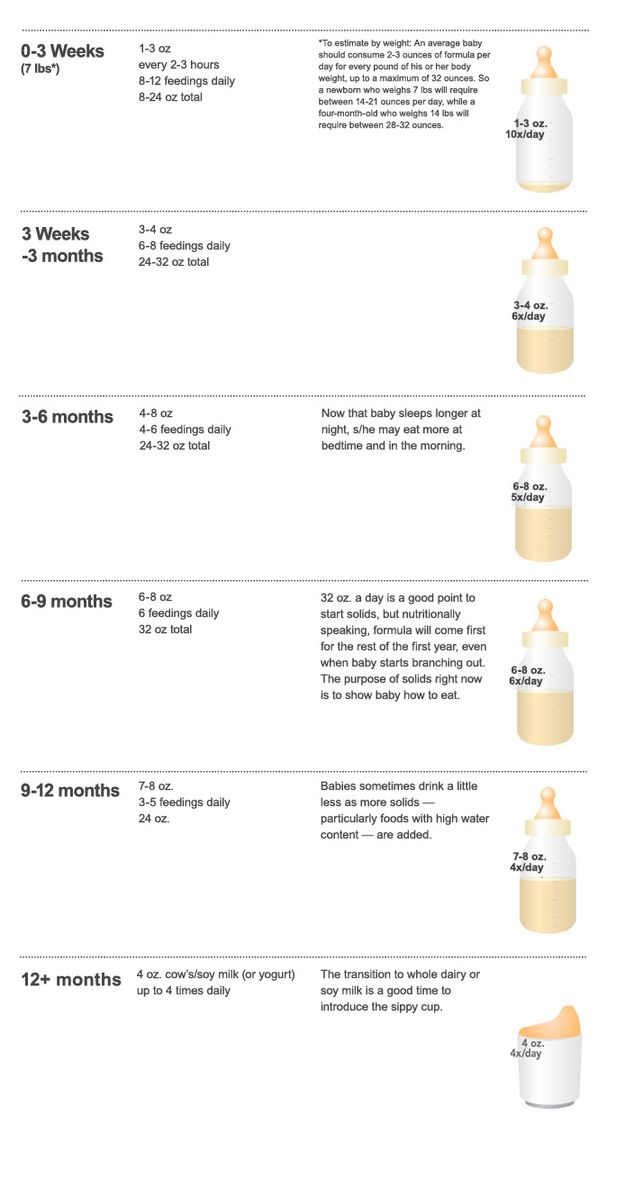 However, doctors are usually aware of the mother's deficiency conditions, since she had blood tests during pregnancy, and they correct them with nutrition or drugs.
However, doctors are usually aware of the mother's deficiency conditions, since she had blood tests during pregnancy, and they correct them with nutrition or drugs.
— Polina Alexandrovna, another fear — mothers are afraid that milk will be lost during mixed feeding.
- This can become a reality if mixed feeding is not rationally approached. True hypogalactia is extremely rare, it is 1-2% in the female population. The body of a woman produces a sufficient amount of milk on the principle of "supply - demand". If the mother begins to increase the volume of the mixture, then the amount of milk in the breast really decreases. The baby will not suck more milk from the breast when he receives an increasing portion of the mixture.
— Will a mixed-fed baby have stomach ache?
- There is no specific link between infant formula and abdominal pain. Yes, when formula is introduced, stools may change. But this does not mean that there will be discomfort for the child. The stool becomes more dense, acquires a greenish tint (it has a yellowish color when breastfed) - this is the norm, which should not be feared.
The stool becomes more dense, acquires a greenish tint (it has a yellowish color when breastfed) - this is the norm, which should not be feared.
Liquid stools with mixed feeding are formed for various reasons:
- the baby receives special formula;
- mom went too far with the amount of mixture;
- with intolerance to the components of the milk mixture.
For symptoms that bother the baby and mother, you need to see a doctor.
— How does mixed feeding affect the child's immunity?
— The immunity of infants develops independently of the type of feeding. But mother's milk contains antibodies and beneficial substances that enhance the immunity of the baby. With a reduced proportion of breast milk on mixed feeding of these substances, the child will receive less than on breastfeeding. But this does not apply to the formation of immunity, and the child's immunity will not suffer from mixed feeding.
— Polina Alexandrovna, how to maintain lactation with mixed feeding?
- In order to keep breastfeeding, you do not need to give formula more than necessary. The doctor determines the amount of supplementary feeding, and you should not independently increase its volume.
The doctor determines the amount of supplementary feeding, and you should not independently increase its volume.
Try to breastfeed more often, breastfeed first and then formula. With the help of a breast pump, you can express after bottle feeding. The goal is not to express a large amount of milk, but to stimulate the nipple, as if applying to the breast, and send a signal to the brain that the baby needs more milk. More milk will come next time.
Table. Mixed feeding of newborns - pros and cons
— Can I choose my own formula for mixed feeding?
- I do not recommend choosing food for the child on your own. With mixed feeding of an infant, it is important to determine not only the type of mixture, but also the nature of supplementary feeding. How much to supplement, so as not to overfeed or leave the baby hungry, so as not to lose breast milk? Should I supplement each time or alternate between breast and bottle feeding, should I formula feed at night? There are many questions. Therefore, even if the mother has made a choice in favor of a certain mixture, she should consult a doctor about the appropriateness of its use and ask how and how much to give the mixture.
Therefore, even if the mother has made a choice in favor of a certain mixture, she should consult a doctor about the appropriateness of its use and ask how and how much to give the mixture.
See also
- "How to choose the right infant formula"
How to switch to mixed feeding
- It all depends on the chosen scheme of mixed feeding and the method of supplementary feeding.
- How to calculate the amount of formula for mixed feeding?
— You need to start from how much the child should eat per day. The daily amount of food is divided by the frequency of feedings to determine the amount of food at one time.
- Checkweighing determines how much breastmilk the baby eats and how much the baby is undernourished. He makes up the difference with a mixture.
- Although the formula is usually diluted at a ratio of 1 scoop per 30 ml, supplementation will not necessarily be a multiple of 30.
 If 40 ml is needed for supplementation, mom prepares 60 ml and only gives 40 ml of them. It is not necessary to give food beyond measure so that lactation does not fade away - when you offer the baby more formula, he asks for less breast milk.
If 40 ml is needed for supplementation, mom prepares 60 ml and only gives 40 ml of them. It is not necessary to give food beyond measure so that lactation does not fade away - when you offer the baby more formula, he asks for less breast milk.
— Is it possible to overfeed a newborn?
- It is always worthwhile to adequately assess lactation and add the amount of formula that the baby really needs. By weighing your baby before and after a feed, you will know how much breast milk he has eaten and how much formula to give him. Given this, the mother will not overfeed the baby.
— Polina Alexandrovna, what dish should I choose for mixed feeding?
- Baby utensils must have the following characteristics:
- material safety - it is confirmed by certificates;
- the possibility of processing high temperatures during sterilization and boiling;
- The right size nipple on the bottle - for the comfort of the baby at each age, a different flow rate of nutrition is needed.
In addition, choose a baby dishwashing detergent that rinses off well with water, and use a separate brush for greater hygiene and convenience.
— The rules for mixed feeding are not limited to formula. What role does mother's nutrition play in this process?
— Scientists have long found out that mother's diet does not affect the child one hundred percent. If the mother is not on a strict diet, does not use preservatives, dyes and heavy fried foods, eats varied, then her diet will not adversely affect the baby's condition. Therefore, the only limitation is a reasonable diet without harmful substances.
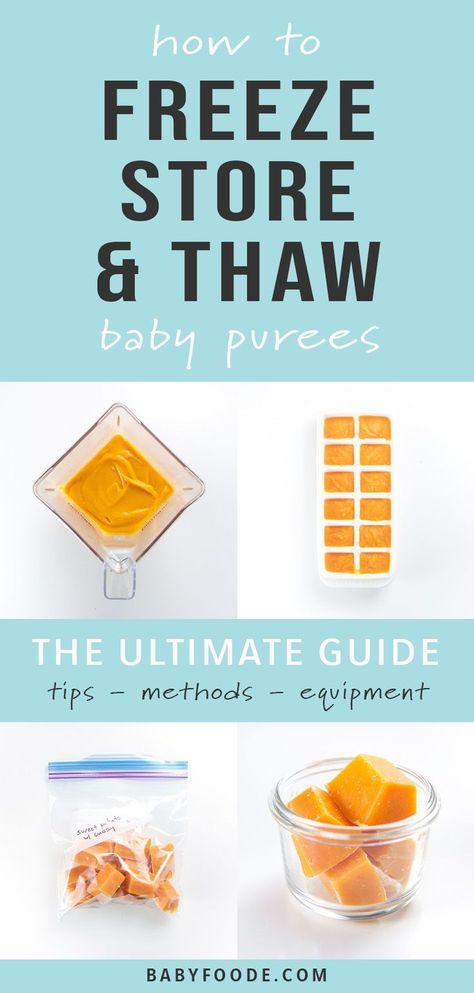
- How long does expressed breast milk last?
- Expressed milk can be stored in the refrigerator or frozen. Temperature and shelf life of expressed breast milk:
Expressed milk is stored in the refrigerator before freezing, and after cooling it is sent to the freezer. Frozen milk is thawed in the refrigerator and heated in a water bath to a comfortable temperature. You do not need to boil it in order to cool it down and give it to the child.
You do not need to boil it in order to cool it down and give it to the child.
Mixed Feeding Rules
— How to properly feed a child with mixed feeding?
- It is advisable to prepare the bottle in advance or pour water heated to the required temperature into it. After breastfeeding and control weighing, it remains to pour the required number of spoons of the mixture into a bottle of water and dilute it.
It is advisable to breastfeed and formula in one meal - first at the breast and immediately after the bottle. When formula feeding, it is best to hold the baby in your arms to maintain physical and emotional contact and minimize the difference for the baby between feeding breast milk and infant formula.
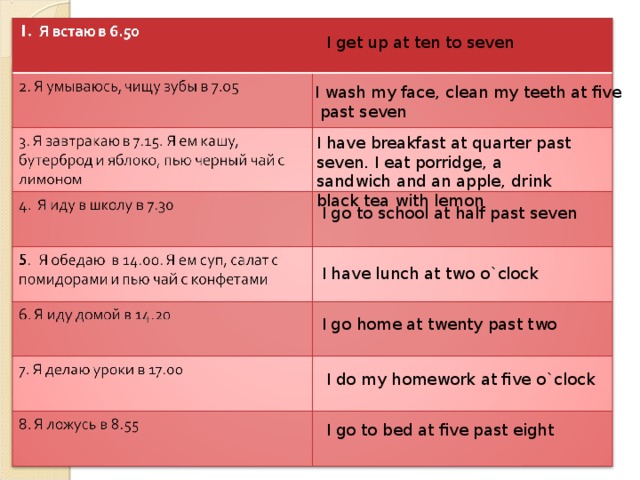
— Do I need a feeding schedule for mixed feeding?
— Yes, when formula appears in a child's diet, there is a need for a feeding regimen. The mixture is quite dense and leaves the baby's stomach 3-4 hours after feeding, so it is recommended to keep breaks between feedings for at least 3 hours on mixed feeding.
— How to feed the baby at night with mixed feeding?
— Everything is individual and depends on the amount of supplementary food. If the mother gives 10-20 ml of the mixture, you can not supplement it at night, at this time of the day the need for nutrition is lower. But if the volume of supplementary feeding is large enough, then it is required to supplement the child with a mixture even at night. The most important thing is to come to the required daily amount of food. In addition, to maintain lactation, it is important to put the baby to the breast from 3 am to 7 am: at this time, the hormone responsible for stimulating lactation is most active.
— Should I give my baby water when mixed feeding?
- It is necessary to focus on the amount of supplementary feeding:
- if you supplement 10-20 ml of the mixture - there is no urgent need for water;
- if supplementary feeding is 50% or more in the meal, you can supplement it.
 Enough 20-50 ml of water per day, depending on the volume of the mixture in the diet, the age of the child and external factors (such as temperature, dry air).
Enough 20-50 ml of water per day, depending on the volume of the mixture in the diet, the age of the child and external factors (such as temperature, dry air).
See also
- "How to give water for up to a year"
— When are goat milk formulas recommended for mixed feeding?
— Goat milk formula is recommended for supplementary feeding and replenishment of breast milk deficiency or as preventive nutrition for a healthy baby with allergies in relatives. With a proven allergy to cow protein, a therapeutic mixture is prescribed.
Infant formula for mixed feeding is selected by a specialist. In order for lactation not to decrease, the mixture is administered in the amount that the child really needs - not beyond the measure and not less than the norm, which is determined by the doctor. Do not forget to supplement your baby with water if the amount of mixture in the mixed-feeding diet is significant enough.
* Breast milk is the best food for babies.