Feeding tube baby clothes
G Tube Clothing - Etsy.de
Etsy is no longer supporting older versions of your web browser in order to ensure that user data remains secure. Please update to the latest version.
Take full advantage of our site features by enabling JavaScript.
Find something memorable, join a community doing good.
( 480 relevant results, with Ads Sellers looking to grow their business and reach more interested buyers can use Etsy’s advertising platform to promote their items. You’ll see ad results based on factors like relevancy, and the amount sellers pay per click. Learn more. )
Products – Starberry Kids
Products – Starberry KidsAdaptive Clothing All White Feeding Tube Onesie
starberrykids
Regular price $22. 95
All White Feeding Tube Onesie (three pack) Buy More and Save
Starberry Kids
Regular price $59.95
Apple Green G Feeding Tube Onesie
starberrykids
Regular price $23.95
Awesome Kid Boys Blue/Red Feeding Tube Onesie
starberrykids
Regular price $26. 75
75
Awesome Kid Girls Pink/Green Feeding Tube Onesie
starberrykids
Regular price $26.75
Ballpark Feeding Tube Onesie
starberrykids
Regular price $24.75
Blue Feeding tube Onesie
Starberry Kids
Regular price $23. 95
95
Bubble Confetti Feeding Tube Onesie
starberrykids
Regular price $24.75
Cheerleader Feeding Tube Onesie
starberrykids
Regular price $24.75
Cool Grey Feeding Tube Onesie
starberrykids
Regular price $23. 95
95
Double Heart Feeding Tube Onesie
starberrykids
Regular price $24.75
Fighter Feeding Tube Onesie
starberrykids
Regular price $26.75
Hole-In-One Feeding Tube Onesie
starberrykids
Regular price $24. 75
75
Home Of The Brave Feeding Tube Onesie
starberrykids
From $23.75
Lavender and White Two Pack Feeding tube Onesie
Starberry Kids
Regular price $48.95
Nobody's Perfect Feeding Tube Onesie
starberrykids
From $23.75
Pink Feeding Tube Onesie
Starberry Kids
Regular price $23. 95
95
Tie-Dye FeedingTube Onesie
starberrykids
Regular price $24.75
Two Pack Animal Print Feeding Tube Onesie (beige, grey, oatmeal)
Starberry Kids
Regular price $48.95
Vehicle Print Feeding Tube Onesie
starberrykids
Regular price $24. 75
75
EVITA - charitable foundation
30.03.2021
20 most frequently asked questions about gastrostomy care and treatment of complications
Question 1. What is a gastrostomy and gastrostomy tube?
Gastrostomy is an artificial opening that connects the anterior abdominal wall to the stomach.
Gastrostomy tube is a medical device that is inserted into the gastrostomy canal and allows the introduction of food and drugs directly into the stomach.
Question 2. Why is a gastrostomy needed?
A gastrostomy is needed to feed or administer drugs directly through an opening (stoma) in the abdominal wall directly into the stomach. L Many children in need of palliative care have a potential risk of choking or reflux of food into the lungs (aspiration) when fed by mouth. Often they cannot eat at all in the usual way (through the mouth) and need special tubes (nasogastric tube, gastrostomy tube, etc. ). Many of the disabled children have not only swallowing problems, but also poor appetite, and therefore suffer from malnutrition and growth disorders, as they do not receive the right amount of nutrients and calories. This also affects the immunity of the child: he often suffers from colds.
). Many of the disabled children have not only swallowing problems, but also poor appetite, and therefore suffer from malnutrition and growth disorders, as they do not receive the right amount of nutrients and calories. This also affects the immunity of the child: he often suffers from colds.
Question 3. Why is a nasogastric tube not recommended for more than 4–8 weeks in palliative patients?
If the use of a nasogastric tube is foreseen for a long period (more than 1-2 months), it is necessary to consider the possibility and feasibility of installing a gastrostomy tube. In addition to medical indications, it also has an aesthetic component - the gastrostomy tube is hidden under clothing, which allows the patient and family to be more socialized.
Prolonged use of a nasogastric tube may lead to the following complications: bedsores; infections of the paranasal sinuses, eyes, ear from the side of the probe; reflux of stomach contents into the esophagus, oral cavity and lungs due to a partially open esophageal-gastric opening, aspiration pneumonia. In addition, a hard probe can permanently injure the mucosa and even cause erosive and ulcerative changes or gastric bleeding.
In addition, a hard probe can permanently injure the mucosa and even cause erosive and ulcerative changes or gastric bleeding.
Question 4. Are there any contraindications for gastrostomy?
Yes. In some cases, the application of a gastrostomy opening is not possible, for example, with severe ascites, peritoneal dialysis, severe portal hypertension, severe hepato- or splenomegaly, high obesity, anatomical defects as a result of a previous operation or inflammation, etc.
Question 5. What are types of gastrostomy tubes?
There are two main types of gastrostomy tubes: percutaneous endoscopic, and balloon (long and low profile). Different children fit different tubes. This depends on the length of time the child will have the gastrostomy tube, the doctor's recommendations, and whether the tube is suitable for the child and family.
The advantage of balloon gastrostomy tubes is that anesthesia is usually given only once, during the initial tube insertion. When it is replaced, general anesthesia and hospitalization are not needed.
When it is replaced, general anesthesia and hospitalization are not needed.
Question 6. How is a gastrostomy tube placed?
Gastrostomy tubes are currently placed using minimally invasive procedures that take 15-20 minutes.
Question 7. How is the gastrostomy tube changed?
PEG installation and replacement require general anesthesia and hospitalization in the clinic. The balloon gastrostomy can be changed without anesthesia at home, which is extremely important for palliative patients. On average, balloon gastrostomy is recommended to be changed every 4-6 months, PEG can be replaced after 1.5-2 years.
Question 8. Can there be problems with the gastrostomy tube?
Yes, there may occasionally be problems with the gastrostomy site (gastric leakage, infection, granulation) or the gastrostomy tube (blockage, disposition/outlet of the tube). In most cases, problems arise due to non-compliance with the rules of care or manufacturer's recommendations.
Question 9. How do I take care of my gastrostomy?
- Wash the skin around the stoma (gastrostomy opening) and under the external fixation device or tube cover (if it is a low-profile gastrostomy) daily with warm soapy water. You can also take a regular bath or shower, but the new tube should not be submerged in water for three weeks after surgery. After showering, make sure the area around your stoma is thoroughly dried. Do not dust it with talcum powder. As prescribed by a doctor, in addition to treatment with soap and water, you can use a solution of an alcohol-free antiseptic (for example, miramistin, octenisept, etc.).
- To prevent blockage, the gastrostomy tube should be flushed with water before and after each feeding and drug administration. Flush the tubing with a bolus of at least 20 to 40 ml of water (10 ml in neonates if there is no fluid restriction).
- After the stoma is fully formed, rotate the gastrostomy tube 360 degrees every day to avoid buildup of granulation tissue around the stoma.

- Check daily that the tube is not “drowned” and that the external fixation device is correctly positioned (approximately 2–5 mm from the skin surface). To do this, daily evaluate the depth of the tube by external marks.
- After processing the gastrostomy opening and the tube itself, daily carefully check whether the internal fixator or balloon rests against the anterior abdominal wall (you can gently pull it towards you until it stops), and then lower the external fixator to the desired mark.
— The external fixation device must not be moved for two weeks after surgery to allow the tube to fit properly. If during this time there is compression and discomfort, report it to specialists.
- When some gastrostomy is placed, additional clips are applied for gastropexy (fixation of the stomach to the anterior abdominal wall to prevent reflux). The duration of the clips is determined by the surgeon, then they either fall off on their own, or the doctor removes them. If during this time there is compression, discomfort, redness - inform the specialist. If you find that the gastrostomy tube is buried deep in the stomach, do not pull it up yourself, inform the specialists.
If during this time there is compression, discomfort, redness - inform the specialist. If you find that the gastrostomy tube is buried deep in the stomach, do not pull it up yourself, inform the specialists.
5. Do not use occlusive dressings over the gastrostomy as they can promote the development of pressure sores and granulations on the skin, as well as an increase in the number of bacteria. Check the area around your stoma for irritation, redness, or swelling. If they appear, you need to consult a specialist.
6. If a balloon gastrostomy tube is available, check and/or change the balloon water weekly using sterile water (in the hospital) or chilled boiled water (at home). The volume of fluid must be checked each time with that indicated in the instructions for this gastrostomy tube. The gastrostomy tube should be changed on average every 4 to 6 months according to the manufacturer's instructions. If the gastrostomy is recent, do not manipulate the gastrostomy tube balloon for 2 to 3 weeks after surgery to keep the stomach in close contact with the abdominal wall. Do not fill the balloon with other solutions (saline, furacilin, etc.). Only sterile (boiled) water can be used.
Do not fill the balloon with other solutions (saline, furacilin, etc.). Only sterile (boiled) water can be used.
Question 10. Is it necessary to take care of the oral cavity if the child is fed through a gastrostomy?
Yes. Oral hygiene should be mandatory, even if the child does not eat through the mouth. Teeth should be brushed twice a day. If necessary, use artificial saliva or mouthwash. If oral nutrition is reduced or not taken at all, plaque can quickly form on the teeth. Poor oral hygiene causes pain and contributes to the development or maintenance of infection and inflammation in the nasopharynx and upper respiratory tract.
Question 11. How to treat the skin around the gastrostomy opening?
The skin is wiped with boiled water, dried and then irrigated with a spray of a local antiseptic such as Miramistin. In some cases, if necessary, a single layer of non-woven cloth can be applied. Gauze pads should not be used. The gastrostomy must “breathe” freely, it must not be sealed with a layer of napkins and a band-aid, as this can lead to pressure sores, infection and granulation. Hydrogen peroxide is not used to treat the skin around the gastrostomy, as it may promote the development of granulations.
The gastrostomy must “breathe” freely, it must not be sealed with a layer of napkins and a band-aid, as this can lead to pressure sores, infection and granulation. Hydrogen peroxide is not used to treat the skin around the gastrostomy, as it may promote the development of granulations.
Question 12. How to feed through a gastrostomy tube?
- Before feeding.
- Examine and listen to the child, check if everything is in order, inspect the site of the gastrostomy for infection and / or leakage of gastric juice through a hole in the skin; inspect the gastrostomy itself, its integrity.
- Prepare the tray (clean the tray with an alcohol antiseptic or alcohol wipe, place only disposable or sterile items on it, gastrostomy flush).
- Check the nutrition: whether it is appropriate for this child, the integrity of the package, the expiration date, the correct volume, the correct time of intake, the temperature (the food should be at room temperature or body temperature).
- Position your baby in the correct feeding position (upper torso should be at least 30-45 degrees to aid digestion and reduce the chance of reflux). method (jet, "gravity", through a pump / syringe pump) - Check the functioning of the gastrostomy (attach the syringe to the gastrostomy and slowly pull the plunger back until the contents of the stomach show; after placing the gastrostomy for three months, it is necessary to check the pH of the stomach daily before feeding using litmus paper)
- Clean the gastrostomy tube and tube with an antiseptic (clean all parts of the gastrostomy tube and connections before each feeding - they are most likely to become infected). Allow antiseptic to dry before attaching syringe, connector, etc.
- During feeding.
– Feeding by any means should last at least 15-20 minutes, it is physiological and is the prevention of reflux of stomach contents into the esophagus and lungs.
- Do not leave your baby alone while feeding, listen to him and talk to him. If you experience coughing or abdominal discomfort during feeding, stop feeding.
If you experience coughing or abdominal discomfort during feeding, stop feeding.
– Remember that feeding in the circle of family members, at the common table is a good socialization of the child.
- Syringe or bolus feeding is not recommended.
- Gravity feeding - minimum 20 minutes. The feed rate can be adjusted as with communicating vessels - by raising or lowering the syringe with food (water).
— Before feeding, flush the gastrostomy tube and fill with chilled boiled water. After connecting the powered syringe, make sure that the water does not drain faster than the power will flow. After feeding, flush the gastrostomy tube with cool water.
- Feeding with pumps (enteromats, syringe pumps) is carried out according to the rules listed above. Pumps can be stationary and portable, saving staff time when used in the clinic. The portable pump gives greater mobility to the family and the patient.
- After feeding.
- SLOWLY rinse the gastrostomy tube with cooled boiled water blast.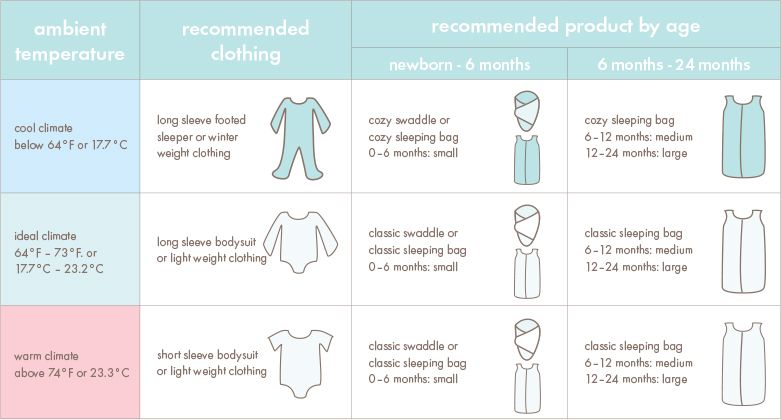
- Close the clip (for long gastrostomy tubes), then remove the syringe and stopper the tube outlet. For a low-profile gastrostomy, close the tubing clamp, disconnect the syringe, disconnect the tubing, close the gastrostomy valve.
- Make sure the child is comfortable and the skin around the gastrostomy tube and clothes are dry.
- In some children, the gastrostomy tube may only be used to administer certain drugs or formulas. If a child has a gastrostomy tube, this does not mean that it is completely contraindicated for him to eat through the mouth. In some children (in agreement with the doctor), a mixed diet may be maintained, for example, solid food - through the mouth, liquids - through the gastrostomy.
- If the child no longer needs a gastrostomy tube, the tube is removed. In this case, the opening of the gastrostomy can either completely close spontaneously (usually within a week), or it is sutured if this does not happen within a month.

Question 13. How do I administer drugs through the gastrostomy?
Do not add medicine directly to food. Consult with patients with fluid restrictions as it may be necessary to reduce flush volumes before and after medication. Decide if the drug can be given through the gastrostomy tube (sometimes crushed drugs do not work as expected or can lead to blockage of the tube).
Some preparations (eg slow-release preparations) must not be ground.
Liquids or dissolvable tablets are the preferred dosage forms for administration through a tube.
Many injectable drugs can be given through the gastrostomy tube.
Step-by-step instructions
- Check with your doctor if you need to take a break after feeding before administering medication.
- Collect necessary medicines and equipment, such as syringes, pestle and mortar.
- Prepare each medicine separately. Never mix medicines without your doctor's approval.
- Stop feeding and flush the tube with at least 30 ml of water for children over two years of age and adolescents, for children under two years of age 10-20 ml (check with your doctor).
- Dispersible tablets: dissolve in 10-15 ml of water, insert into the tube. – Liquids: shake, dilute a viscous liquid immediately before administration in an equal amount of water, enter into the tube.
– Tablets: crush the tablets using a pestle and mortar. Mix with 10-15 ml of water and inject into the tube.
- Capsules: open the capsules, pour the medicine into the medicine container. Mix with 10-15 ml of water and inject into the tube.
– After each medication, rinse the grinder, draw water (10-15 ml) into the used syringe and pour into the tubing. This way you will ensure that the entire dose is delivered.
- If more than one medication is to be administered, ensure that you flush at least 10 ml of water between 2 medications to clear the tube. After administering the last medication, flush the tube with at least 30 ml of water.
- Do I need to take a break before resuming feeding? Check with your doctor.
- Resume feeding.
Question 14. What should I do if the gastrostomy is blocked?
For partial blockage, flush with warm boiled water. If it doesn’t help - soda water, Coca-Cola or freshly squeezed pineapple juice (exposure in a tube - 20 minutes). With complete or partial blockage (if previous methods are ineffective) - pancreatin (dilute in water and inject into the tube by 30–90 minutes).
If it is not possible to unlock it, replace the gastrostomy.
For prevention, rinse with water before and after feeding in a volume of 20-40 ml (minimum volume of 10 ml is suitable for all ages).
For prophylaxis, use forms of drugs that do not "clog" the tube.
If a blockage occurs, do not worry, as this will not harm the child's health. If you need to administer drugs that are required for regular intake (for example, anticonvulsants), consult your doctor. Temporarily they can be given to the child through a nasogastric tube, rectally, etc.
Temporarily they can be given to the child through a nasogastric tube, rectally, etc.
Question 15. What should I do if the skin around the gastrostomy is inflamed?
Inflammation may result from bacterial or fungal infections. For superficial infections, a cream/ointment with bactericidal antibiotics (eg, neomycin, bacitracin). If necessary, an antifungal drug is added. For deep infection, systemic antibiotics +/- antifungal drugs (by mouth).
Signs of infection : erythema, edema, soreness, purulent discharge, bad smell, fever (one or a combination of symptoms may occur). A swab for flora and sensitivity to antibiotics is required. It is necessary to differentiate with granulation.
Wash stoma with soap and water before applying creams/ointments. Keep your stoma open and breathable (do not cover).
Question 16. What to do with granulations?
Treat. Use an ointment with a steroid hormone (for example, betamethasone - akriderm, beloderm, celestoderm, betliben, etc. ) or combined with a hormone, antibiotic and antifungal drug (for example, triderm, canison plus, akriderm GK, etc.). How to use: carefully wash the granulation with cool boiled water, dry it. Then treat with an alcohol-free antiseptic (for example, Miramistin), wait for it to dry. Then generously apply betamethasone ointment with a cotton swab to the edges of the gastrostomy and granulation. If necessary, place a thin non-woven cloth between the granulation and the external fixator of the gastrostomy tube. Do not tape. Repeat the procedure 2 times a day, the course of treatment is at least 10-14 days.
) or combined with a hormone, antibiotic and antifungal drug (for example, triderm, canison plus, akriderm GK, etc.). How to use: carefully wash the granulation with cool boiled water, dry it. Then treat with an alcohol-free antiseptic (for example, Miramistin), wait for it to dry. Then generously apply betamethasone ointment with a cotton swab to the edges of the gastrostomy and granulation. If necessary, place a thin non-woven cloth between the granulation and the external fixator of the gastrostomy tube. Do not tape. Repeat the procedure 2 times a day, the course of treatment is at least 10-14 days.
If the granulation becomes infected (purulent discharge appears) - treat with an antibiotic ointment for the first 3 days (apply 2 times a day), and then use a combined ointment with a hormone, an antibiotic and an antifungal drug.
Signs of granulation
- pink-red pimply edging, "plus-tissue", mucous discharge, sometimes - bleeding.
Question 17. What should I do if I have a gastrostomy leak?
Check external attachment, depth and correct standing, and integrity of gastrostomy tube. Check the condition of the cylinder and its filling (if any). Check the volume of the stomach - if necessary, remove excess air with a syringe before feeding. Eliminate pressure on the stomach from the outside, including constipation. In case of leakage associated with a violation of the integrity of the gastrostomy or a discrepancy between the diameter of the gastrostomy and the diameter of the tube, the gastrostomy tube should be replaced. Find the optimal position of the child during feeding to improve gastric emptying, reduce its volume and pressure during the introduction of food.
Leakage is common for 3 to 4 weeks after gastrostomy placement until a skin canal has formed. Routine hygienic care is carried out. Barrier creams and ointments with zinc oxide are used to prevent or treat skin maceration.
- In case of decreased gastric motility or hypersecretion of the stomach, drugs such as prokinetics and antacids are prescribed.
— Leakage may occur with gastrostomy infection (see question 15 for care and treatment).
— If all the above methods do not solve the problem, try switching the child from bolus feeding to continuous feeding. If the problem does not go away with continuous feeding, you need to reduce the feed rate of the mixture.
Question 18. What if the gastrostomy tube is completely out of the stomach?
If you have a balloon gastrostomy tube, you need to have a spare so you can insert a new one right away. If a new one is not available, insert and bandage an old one, or a Foley catheter (size 12), or a suction catheter to prevent obstruction of the gastrostomy port, call a physician immediately to replace with a new one.
- Be aware that the hole can close quickly. Depending on various factors and individual characteristics of the organism, the gastrostomy begins to close after 1-2 hours and in most cases completely closes after 4-6 hours.
Question 19. Are there advantages to low profile gastrostomy?
Yes. The quality of life is improved, since the tube is small and invisible under clothing, no additional adhesive is needed. The highly secure port cover prevents spontaneous tube opening and leakage. The anti-reflux valve prevents backflow of contents from the stomach. Improved air circulation around the stoma.
The child cannot accidentally pull out the tube from himself or from the one who has it, because there is no long “tail”. It is better to give preference to "atraumatic" tubes, in which the distal tip of the tube does not extend beyond the balloon ("drowned"), which prevents irritation of the opposite wall of the stomach, and the conical shape of the distal tip of the tube ensures easy insertion.
The material of which the tube is made must be hypoallergenic. Preference is generally given to medical silicone that does not contain latex, diethylhexyl phthalate and other substances that cause allergies and other undesirable reactions. A radio-opaque coating along the entire length of the tube allows for fluoroscopic imaging.
A radio-opaque coating along the entire length of the tube allows for fluoroscopic imaging.
Question 20. What literature and Internet sources exist on the gastrostomy?
- Gastrostomy care in pediatric palliative care. – http://www.youtube.com/watch?v=wcu5K1Vcca4
- How to administer drugs through a gastrostomy. – http://www.youtube.com/watch?v=veVpW2DYCcc
- Percutaneous endoscopic gastrostomy. – http://www.youtube.com/watch?v=atQGkK0zW2s
- Balloon low profile gastrostomy tube. – Care, feeding, replacement, general problems (leakage, infections, granulation): http://www.youtube.com/watch?v=B4tKh51XJ6Y
- Care, feeding, replacement, granulation: http://www.youtube.com/watch?v=A5TLBEzulcE
- Treatment of the gastrostomy area: http://www.youtube.com/watch?v=S75imEdB3YU
GASTROSTOMA in palliative pediatrics: 20 questions and answers on the care and treatment of complications (Edited by Candidate of Medical Sciences, Associate Professor Savva N. N)
N)
http://www.rcpcf.ru/wp-content/uploads /2014/08/Brochure_Gastrostoma_site.pdf
Everything you need to know – Covey
Your first step as a parent of a tube-fed baby: Don't panic - you can handle it. Next, get to know this super-important tool designed to keep your child healthy and prosperous.
Did your pediatrician suggest a feeding tube for your baby? If you are experiencing a storm of emotions - from sadness, anxiety to complete panic - you are not alone. Nearly 200,000 American children use feeding tubes to meet some or all of their nutritional needs.
This means that more than a few other parents know how you feel.
“Tube feeding can be traumatic,” explains Gary Noritz, MD, pediatrician and Comprehensive Care Program Manager at Nationwide Children's Hospital in Columbus, Ohio. “Many parents may think that they did something wrong when their child has problems with eating or feeding, but this is not the case. The feeding tube is just a tool that we use to ensure that the baby is well fed. We can use it as long as we need it."
The feeding tube is just a tool that we use to ensure that the baby is well fed. We can use it as long as we need it."
Overloaded? Take a deep breath. “You may need to learn a little,” says Dr. Noritz. "But a feeding tube can help your baby grow and thrive."
Here's a guide to help you get started.
Contents
Why might my baby need tube feeding?
According to the Feeding Tube Awareness Foundation, there are over 300 conditions that may require tube feeding for children. "There are several reasons why children may have difficulty swallowing food," explains Julie Sunville, MD, pediatric gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire. “One of the main reasons is preterm birth, but sometimes anatomical differences can also interfere with the ability to feed. There may also be allergic diseases, genetic problems, or problems with the gastrointestinal tract.”
Dr. Sanville also notes that certain medical conditions, such as cystic fibrosis or cerebral palsy, may also warrant a feeding tube. Dr. Sunville adds, "Children with severe behavioral or mental health problems, such as sensory disturbances, severe anxiety, or avoidance of food restriction, may have difficulty feeding or refuse to feed at all."
Dr. Sunville adds, "Children with severe behavioral or mental health problems, such as sensory disturbances, severe anxiety, or avoidance of food restriction, may have difficulty feeding or refuse to feed at all."
In the end, no matter why your baby might need a feeding tube: It all comes down to math. "Children need to get more calories than they expend on a daily basis in order to gain adequate weight," explains Dr. Sunville.
Is tube feeding forever?
Optional. Children with serious illnesses may need feeding tubes for life, but for others it is temporary, explains Dr. Noritz.
"For some children, the ability to eat improves over time," he explains. "Intensive feeding therapy can sometimes get them off the tubes and switch them to regular oral feeding." And other children may even develop a hybrid diet: they get part of the food through their mouths, and the rest through a tube.
How does the feeding tube work?
Feeding tubes come in several basic types: those that feed through the nose and those that are inserted through the abdomen. Both types inject liquid food from a bag or syringe directly into the baby's body through a tube that connects to a port called a "button".
Both types inject liquid food from a bag or syringe directly into the baby's body through a tube that connects to a port called a "button".
Although it sounds intimidating, tube feeding is actually quite simple and painless: You can hang the bag on a wall hook (or, for older children, in a specially designed backpack) while the pump delivers formula through the tube at a precisely calculated pace. Some babies feed every few hours, while others feed little by little, continuously throughout the day or at night.
Here's what you need to know about types of feeding tubes and placement of feeding tubes:
- Nasal tubes. They are introduced into the child's body through the nose, through the esophagus and into the stomach (NG tubes) or directly into the small intestine (ND or NJ tubes). They are used when your child needs short-term help getting nutrients or medicines into the body, such as after surgery. Your doctor will place these tubes during your outpatient visit.

- Gastric or gastronomic tubes. The most common types of feeding tubes, they are used when your baby needs help with feeding for a long time - at least three months. They are inserted into your child's abdomen and passed into the stomach (G or PEG tubes) or intestines (GJ or J tubes). Your child will go to the hospital for a short operation followed by close observation for a few days. Dr. Noritz admits that this moment can be stressful for the family. “Despite the fact that this is a routine procedure for doctors, we know that this is always a big event for parents.”
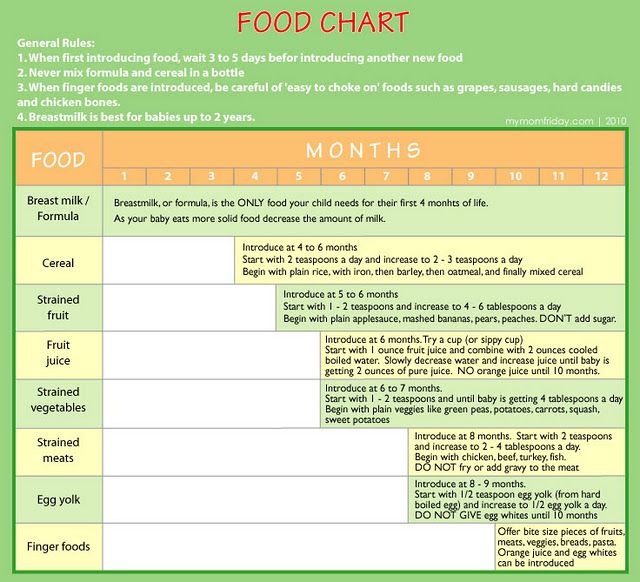
What food will my child get through the tube?
You will work with a doctor and dietitian to find the right food for your child. “For a baby,” explains Philomena Kersey, a registered pediatric dietitian with Dr. Sunville's team at Dartmouth Hitchcock, “we always want to use breast milk, at least in part. Or we will use conventional or specialty formula, such as the one made for a child with a food allergy or fat digestion problem. ”
”
It can be different for older kids, Kersey says. “We choose formula based on what the child can tolerate and what the underlying medical problem is – there are a lot of options.”
Kersey advises caution with homemade tube feeding formulas. “You have to be very careful about food safety,” she explains, noting that some homemade formulas expire earlier than store-bought ones. For some children, it may be difficult to meet all of their nutritional needs with homemade formula.” If you're thinking about mixing your own products, it's a good idea to consult a nutritionist."
How do I care for and clean my pipe?
Handling and administering food is easy, but requires some preparation.
“In a couple of weeks, cleaning your child's tube will become a daily routine,” says Dr. Sunville, noting that you will first learn how to care for the tube while your child is in the hospital by working with a baby doll with connected handset. You will then move on to handling your child's tube under the supervision of a nurse.