Food allergy test for babies
How Doctors Test Your Child for Food Allergies – Lil Mixins
Now reading: How Doctors Test Your Child for Food Allergies
Feeding your baby new foods is an exciting milestone for any parent. But with new foods comes the worry of food allergies. Here’s what you should know about testing your child for food allergies.
When to Get Food Allergy Testing
The only time you should get your child tested for food allergies is when they have shown a reaction to a food. If your child seems to develop hives, stomach pain, itchiness, or eczema after eating a particular food, you should contact your pediatrician, who will most likely suggest testing for an allergy to that food.
The exception is if your baby has an allergy that is strongly linked to another allergy. For example, most people with walnut allergy have a pecan allergy. A child who has reacted to walnuts may get tested for sensitivity to other tree nuts.
You should not, in general, test for allergies to foods your child is not reacting to or has never eaten. Here’s why.
The only true test of a food allergy is an oral food challenge.
Skin prick tests and blood tests look for sensitivity to food, or signs that the immune system has created alarm bells (antibodies) for that food. Sensitization is not an allergy.
Sensitization means your baby’s body has flagged a particular food as potentially dangerous. Having antibodies does not prove that their body will react to that food.
For example, in one study, 86% of patients with a sensitivity to tree nuts passed an oral food challenge and went on to eat tree nuts normally. They were sensitized, but didn’t actually have a tree nut allergy.
This is why you shouldn’t have your baby tested for a food they’ve never eaten or haven’t had a problem with. Most allergists will even refuse to do so.
Skin prick tests and blood tests cause many parents to fear foods that their child may not actually have an issue with. They see a result indicating their baby’s immune system is sensitized to a food (remember, not allergic), and decide that they should avoid that food forever.
They see a result indicating their baby’s immune system is sensitized to a food (remember, not allergic), and decide that they should avoid that food forever.
As a parent, there’s a strong urge to “just test them for everything,” but you should resist this because you will likely end up scared of foods that your child can eat just fine.
Any good allergist will tell you that the only true test of a food allergy is an oral food challenge. You eat the food, and wait to see if there is a reaction. If you react, you have a food allergy. If you have no symptoms, you do not have a food allergy to that food.
So why is skin prick or blood testing ever done?
- Food allergy symptoms in babies are way more mild than in older children and adults. Hives can often come from a cold virus or something else. If a child has had food allergy-like symptoms in the past, skin or blood testing can be a good way to confirm if it was truly an allergic reaction.
- Before doing a food challenge, skin or blood testing can help predict the probability of passing the food challenge.
 Failing an oral food challenge, meaning that the child has a reaction, can be scary for a child and their parents. If the probability of an allergy is really low, it’s worth doing a food challenge. If the numbers are really high, and there’s been some past event that made you suspect a food allergy, it may be smarter to avoid a food challenge and an unnecessary reaction just to prove it.
Failing an oral food challenge, meaning that the child has a reaction, can be scary for a child and their parents. If the probability of an allergy is really low, it’s worth doing a food challenge. If the numbers are really high, and there’s been some past event that made you suspect a food allergy, it may be smarter to avoid a food challenge and an unnecessary reaction just to prove it. - If a child had a proven food allergy, comparing the results of skin testing and blood testing over time can help an allergist see if the child is naturally outgrowing the allergy.
- If a child is showing some symptoms, like belly pain all day, testing can help differentiate a food intolerance from a food allergy. You may still avoid foods that you are intolerant to, but you do not need to carry an epi-pen.
The goal of food allergy testing should be to find foods that your baby is NOT allergic to, so that your baby does not unnecessarily avoid foods.
What to Expect with Skin Prick and Blood Testing
In skin prick testing, the doctor will place a drop of liquid containing the allergenic protein on the skin and then push down to prick through the top layer of skin. If your baby’s body already has the antibody for that particular food or pollen, you’ll see a red puffy welt (called wheals) start to appear around that prick within fifteen minutes. Your doctor will look for these wheals and measure their size to determine the likelihood of a true allergy. Then they’ll wipe the area clean and apply a cortisone cream to stop any itching.
If your baby’s body already has the antibody for that particular food or pollen, you’ll see a red puffy welt (called wheals) start to appear around that prick within fifteen minutes. Your doctor will look for these wheals and measure their size to determine the likelihood of a true allergy. Then they’ll wipe the area clean and apply a cortisone cream to stop any itching.
Our son's first skin prick test at the doctor's office
For blood testing, a tube of blood is taken using a needle. The blood is sent to a lab where food and pollen proteins are put into the blood sample, and the amount of antibodies that show up are counted.
Blood testing gives you a result for each food or pollen protein from 0-100. Higher scores in general mean a higher probability of a true allergy to that protein.
However, you should not interpret the results without consulting a doctor. Different levels mean different things for each allergen, and it is really common to see high numbers all around in children who also have eczema, asthma, or seasonal allergies.
We saw this with our son when he was first diagnosed and his eczema was not controlled. When the test was repeated a year later, all the values went down a LOT.
The printout showing our son's IgE blood test results
Oral Food Challenges
A doctor-supervised oral food challenge is the one definitive test of a food allergy. Food challenges, like skin prick and blood testing, are used to make sure someone is NOT allergic. If your doctor is fairly sure that your child has a food allergy, they will not do a food challenge to prove it.
Oral food challenges are often done to see if a child can eat some versions of a food, like baked egg or baked milk, which can open up eating options. Food challenges are also done when it seems like your child has outgrown a food allergy.
To do a food challenge safely, you will go to the doctor’s office and your child will eat a teensy amount of the food to start. Every 20 minutes or so, the doctor will check for any signs of a reaction and then have your child eat a larger amount of that food.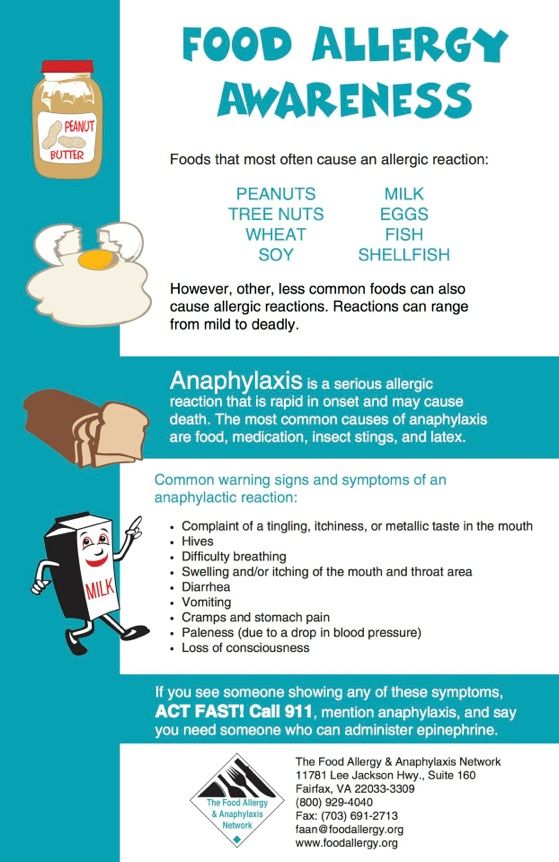 After about 2 hours, your child will have eaten a full serving of the food. This process takes four hours, so come prepared!
After about 2 hours, your child will have eaten a full serving of the food. This process takes four hours, so come prepared!
Our son doing his oral food challenge with syrup covered french toast
Once your child has eaten a full serving of the food and shown no reaction for 2 hours, they can be cleared as not having that allergy.
While this process sounds simple, it is important to do this at a doctor’s office, so that you will have help nearby if a reaction does happen.
Conducting oral food challenges is important because many people end up changing their lives and avoiding foods they aren’t actually allergic to. When a blood test or a skin prick test shows a lower probability of a true allergy, an oral food challenge can bring peace of mind.
What About Home Food Allergy Test Kits?
These days, because my search history is all about food allergies, I see a lot of advertisements online for home-based food allergy or food intolerance screening tests.
None of these diagnostic tests have been cleared by the FDA. That means that they have never created and presented data showing that their tests work. Acupuncture, hair/urine testing, and any other such testing you may have heard of has also never proven itself with a real clinical study. These clinical studies are not particularly difficult to do, so they would get FDA approval if they could.
When it comes to food allergies, it's important to focus on proven testing methods because you do not want to hurt your child accidentally.
ConclusionHopefully this introduction to food allergy testing will be useful to you. If you have any further questions, definitely reach out to your child's pediatrician to get specific answers by a trained medical professional.
Remember that food allergy testing doesn't have to be stressful, and with proper care and management, you will pull through this uncertain period, just like we did.
When to Test Your Newborn for Food Allergies
A lot of parents get excited when they start to feed their child solid foods. It will be fun, adventurous and all around hysterical. You’ve seen the viral videos of babies eating lemons that make us all bend over laughing. Or how about the kid that discovered bacon and experienced his first love?
It will be fun, adventurous and all around hysterical. You’ve seen the viral videos of babies eating lemons that make us all bend over laughing. Or how about the kid that discovered bacon and experienced his first love?
The point is… introducing solids is fun.
But when will you know when the time is right?
The American Academy of Pediatrics says that between the ages of 4 and 6 months is the optimal time to begin introducing solid foods. This is when babies start showing signs of readiness, which means that their bodies are ready. Some of these signs include sitting up with support, having control of their head and neck movements, showing interest in what you’re eating and no longer having the reflex of pushing food out of his or her mouth.
It’s important to start incorporating solid foods at this time because otherwise, your baby will get overly accustomed to liquids and loose the interest of learning how to eat solids.
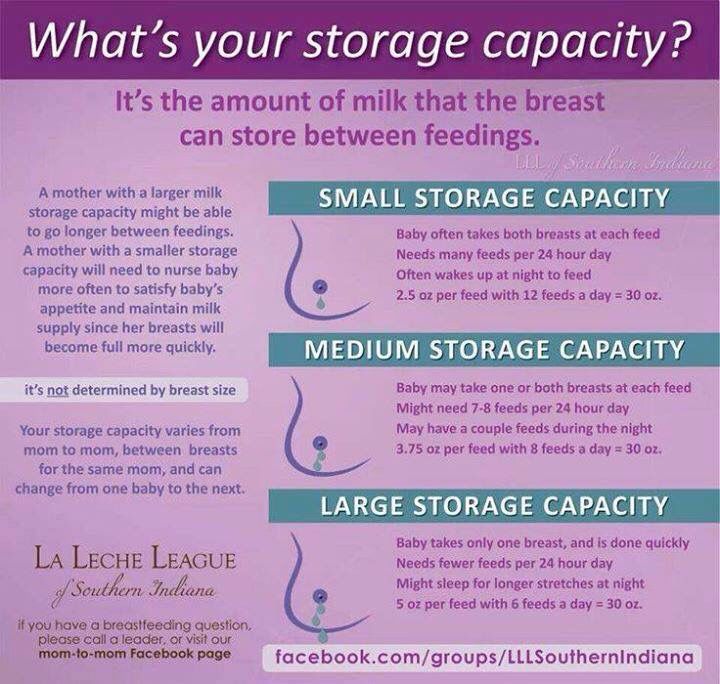
When it’s time to start introducing solid foods, it means it’s also time to start testing your newborn for food allergies. The two go hand-in-hand. However, you’re introducing new foods, continue to breastfeed for other meals. This will help reduce the chances of food allergies due to the immune properties in the breast milk.
The two go hand-in-hand. However, you’re introducing new foods, continue to breastfeed for other meals. This will help reduce the chances of food allergies due to the immune properties in the breast milk.
Common Allergenic Foods
Before you begin testing your newborn for allergies, here is a list of the most common allergenic foods. It’s great to keep this in mind when you start feeding your baby solids in order to keep a watchful eye out for any symptoms. Read more information on these common food allergens here.
- Milk
- Eggs
- Peanuts
- Tree nuts
- Fish
- Shellfish
- Soy
- Wheat
How to Test Your Newborn
While the time may have come to start testing your newborn, there’s a lot of conflicting information on how to actually do it. Luckily, we’ve put together our best tips for seamlessly testing your newborn below.
Introduce Solid Foods Gradually
Feeding your baby solids is fun.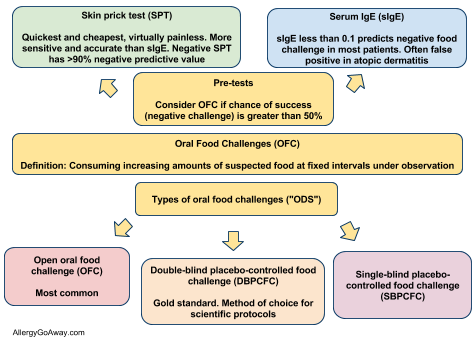 You get to see their reactions to certain foods and find out what they like and dislike. It’s one more milestone for parents to check off their lists. However, introducing solids should be done carefully.
You get to see their reactions to certain foods and find out what they like and dislike. It’s one more milestone for parents to check off their lists. However, introducing solids should be done carefully.
When you do decide to start introducing solid foods to your newborn, make sure that you take your time. While it is tempting to let your child try a little bit of this and a little bit of that, it has the potential to cause complications. This is because introducing solids is essentially how you test for allergens.
For this reason, doctors recommend introducing babies to new foods one at a time. This way, if an allergic reaction does occur, you’ll be able to exactly pinpoint which food it was that caused the reaction.
If you give your child a few new solid foods over the course of the day and something goes wrong, you won’t be able to determine exactly which of the foods caused it and you’ll need to do further tests to be sure.
Don’t stress too much about the order of foods you introduce.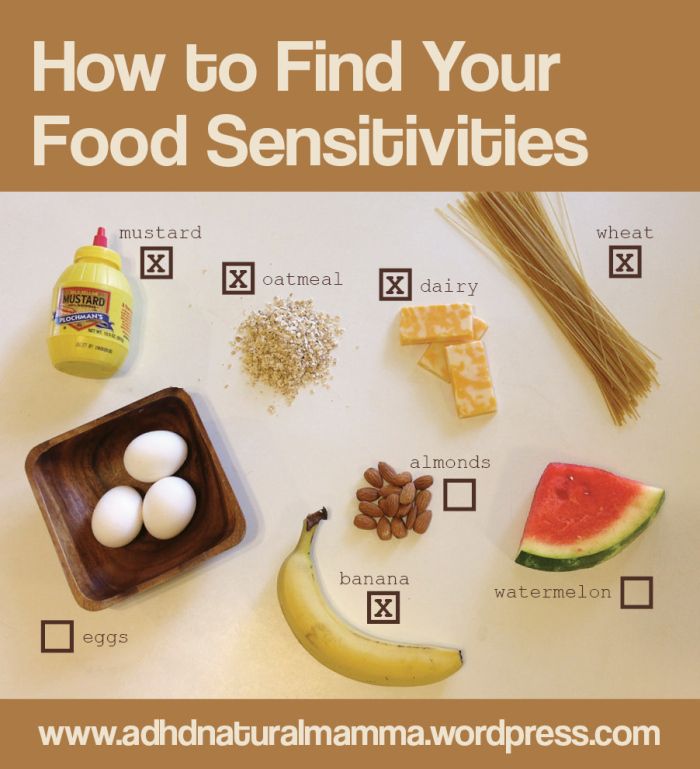 As long as the foods are healthy, then things will go fine. As a general rule of thumb, the Mayo Clinic recommends single-ingredient foods with no added sugar or salt.
As long as the foods are healthy, then things will go fine. As a general rule of thumb, the Mayo Clinic recommends single-ingredient foods with no added sugar or salt.
Additionally, it is recommended that every time you introduce a new food, you wait a few days before introducing more1. This is because some foods may have an extended reaction time. Which leads us to our next point…
Keep a Close Eye Out for Baby Food Allergy Symptoms
As you start introducing new foods, it’s important to make sure that you are keeping a close eye out for symptoms of allergies. Most reactions occur soon (even immediately) after the food is eaten, but will also extend hours post consumption.
Make sure that you are aware of the following food allergen symptoms so that you will react quickly.
- Hives or welts, which can occur on the face or on the body
- Rash or flushed skin
- Any swelling of the face, tongue or lips
- Vomiting
- Diarrhea
- Coughing or continual wheezing
- Any difficulty breathing
- A sudden loss of consciousness
In order to ensure the safety of your child, make sure that you pay close attention to these symptoms.
Severe Reactions
If your baby is having any difficulty breathing, high levels of swelling or severe vomiting and/or diarrhea, call 911 immediately. It is more important to get immediate medical attention than it is to contact your pediatrician first.
These types of symptoms indicate that your child is having a severe allergic reaction and you should take extra precaution to make sure that your child avoids these as they continue to grow.
Mild Reactions
A rash isn’t as serious as difficulty breathing, so don’t freak out! If mild allergic reactions occur simply give your pediatrician a call. They will walk you through the steps for how to manage these reactions.
If you find a mild reaction in a food, it’s best to completely avoid it for now. Allergens will increase in severity over time, remain the same or completely disappear. Talk to your pediatrician for more information
Only Introduce New Foods at Home
After reading about the symptoms, we’re sure you understand why we recommend only introducing new foods at home. This makes things much more manageable if an allergic reaction occurs.
This makes things much more manageable if an allergic reaction occurs.
Plus, who wants to deal with the stress of baby’s first allergic reaction while out at a restaurant? We doubt many people do.
If you want to be especially careful, consider having a child-safe oral antihistamine around. Talk to your pediatrician to find one that will work best for you and your child.
Be Especially Careful When Introducing Peanut Products
Serious food allergies are dangerous and will change the way you and your family eat. Since the most common serious allergen is peanuts, be overly cautious when introducing it to your child.
This doesn’t mean hold off on introducing peanuts though. In fact, there’s currently research that states that introducing younger children to peanuts, as early as 4 months old, can actually reduce the risk of developing an allergy.
Here’s a great article with tips for safely incorporating peanuts into your baby’s diet.
See an Allergist
When you are allergic to something, your body develops antibodies as a layer of protection.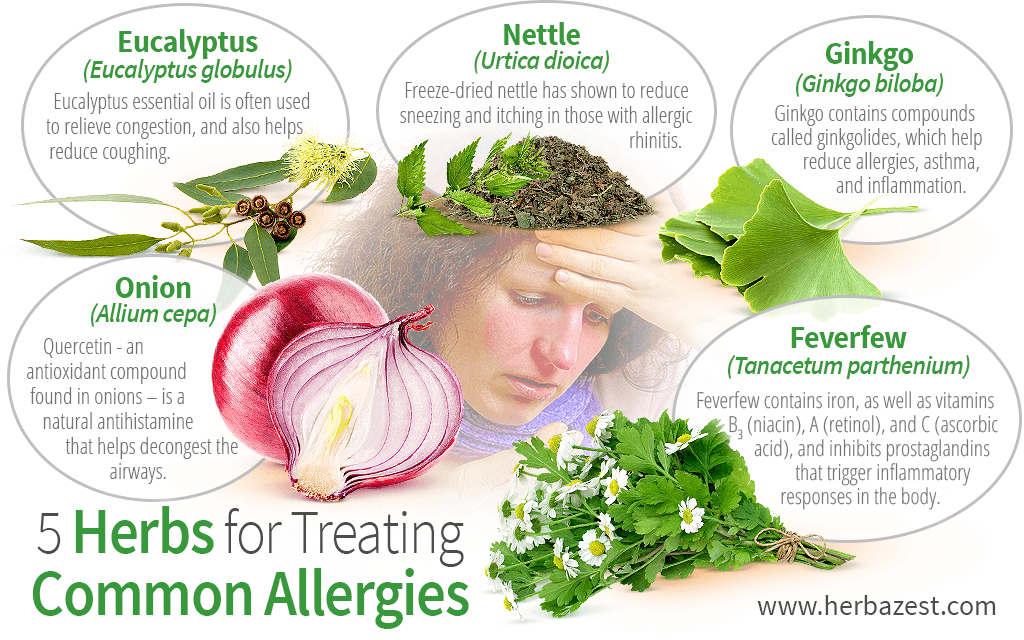 When these antibodies come in contact with the allergen, there are chemicals released to warn your body. These chemicals are what cause food allergy symptoms.
When these antibodies come in contact with the allergen, there are chemicals released to warn your body. These chemicals are what cause food allergy symptoms.
If you find that your baby has one or more positive symptoms of allergic reactions, it’s a good idea to take them into an allergist. At their office, an allergist may recommend either doing a blood test, a skin prick test or both.
A blood test measures the amount of antibodies that your body contains for specific allergens6. A skin test is an alternative way to test allergens but will cause more discomfort for newborns over a longer period of time.
Take Precautions
There are a few precautions to keep in mind when you begin testing your newborn for allergies. The following things are not appropriate for babies and should be avoided until the reach a certain age:
- No cow’s milk before reaching age 1.
- Do not give your infant honey – it causes a serious illness called infant botulism. Wait until at least 1 year, maybe even 2 years to be on the safe side.

- Always cut up the food your giving your newborn into small pieces that have zero risk of choking.
- Avoid hard foods like nuts, popcorn and candy.
The Difference Between Intolerance and an Allergy
One thing to note is that there is a difference between an allergy to foods and intolerance to foods. An allergy is your immune system’s first line of defensive. It indicates that there is something, usually a protein, in the food that will cause either respiratory or gastrointestinal problems.
There may be an underlying factor causing the allergens, but that is easier to test when your baby grows older.
Intolerance to food is more of a metabolic response – unrelated to the immune system. It usually involves enzymes and chemical reactions that any given body has a hard time processing. Talk to your pediatrician to learn more about these differences and what they mean for your baby.
Conclusion
When your newborn begins to show signs of curiosity toward solid foods, it’s time to start testing them for allergies. Remember, start slow and always introduce new foods in a place that you’re comfortable in. If you have any genetic predispositions to allergies, be cautious and ready for reactions. It can be handy to keep a child-friendly antihistamine ready just in case, and remember to always call 911 before your pediatrician in case of severe reactions. If you’re looking for more great pregnancy tips, info, and product reviews head over to our website. As always, through the Affordable Care Act you are eligible to receive a breast pump from Byram Healthcare at no additional cost.
Remember, start slow and always introduce new foods in a place that you’re comfortable in. If you have any genetic predispositions to allergies, be cautious and ready for reactions. It can be handy to keep a child-friendly antihistamine ready just in case, and remember to always call 911 before your pediatrician in case of severe reactions. If you’re looking for more great pregnancy tips, info, and product reviews head over to our website. As always, through the Affordable Care Act you are eligible to receive a breast pump from Byram Healthcare at no additional cost.
Have any fun stories or words of caution about when you introduced your baby to solids for the first time? Leave a comment on our Facebook page today!
Allergy to food, find out the prices for a set of tests and take it in Moscow
Synonyms: Blood test for food allergy.
Food allergy: Allergy blood test: allergies to foods; Food blood allergy test.
Profile composition:
No.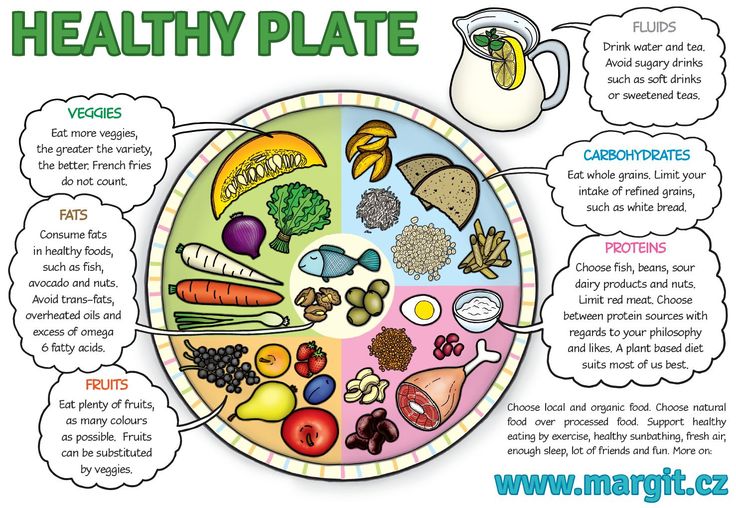 67 IgE total (Immunoglobulin E total, IgE total)
67 IgE total (Immunoglobulin E total, IgE total)
No. 998 Orange, IgE (Orange, IgE, F33)
No. 611 Peanut, Ig0105)
№ 636 Grapefruit, IgE (Grapefruit, IgE, F209)
Ref. 608 Cow's milk, IgE (Milk, IgE, F2)
Ref. 614 Crabs, IgE (Crab, IgE, F23)
Ref. IgE (Lemon, IgE, F208)
No. 617 Carrot, IgE (Carrot, IgE, F31)
No. 632 Baker's Yeast, IgE (Baker's Yeast, IgE, F45)
No. 610 Wheat flour, IgE (Wheat, IgE , F4)
Ref. 619 Celery, IgE (Celery, IgE, F85)
Ref. 612 Soybeans, IgE (Soybean, IgE, F14)
Ref.0005
No. 609 Cod, IgE (Codfish, IgE, F3)
No. 613 Hazelnut, IgE (Hazelnut, IgE, F17)
No. 633 Chocolate, IgE (Chocolate, IgE, F105)
Egg white, IgE No. 607 (Egg White, IgE, F1)
No. 618 Egg yolk, IgE (Egg Yolk, IgE, F75)
Brief description of the Food Allergy study
According to the World Health Organization (WHO), manifestations of food allergy occur an average of 2.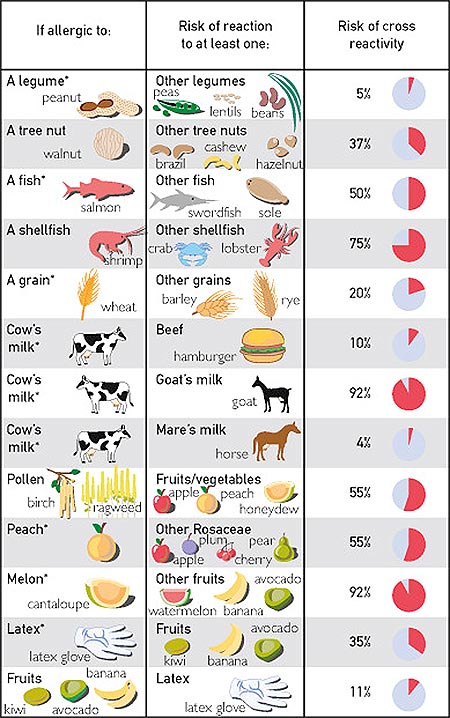 5% of the population.
5% of the population.
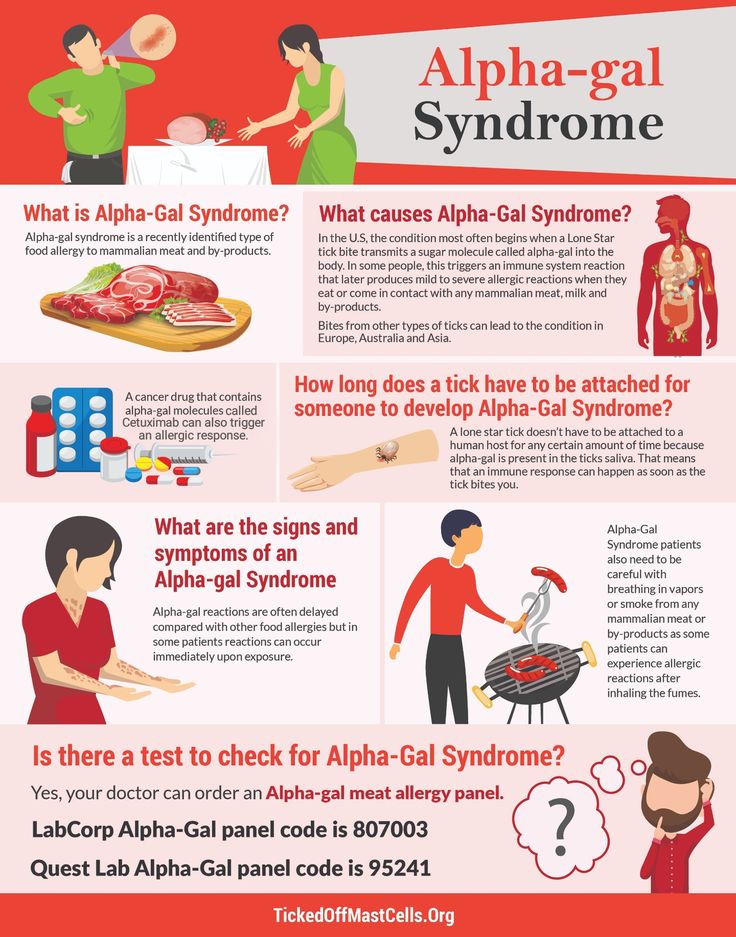
Food allergies are directly caused by antigens in foods. Antigens are substances that, when they enter the human body, are recognized as foreign and cause an immune response in the form of an allergic reaction. The so-called "Big Eight" foods that most commonly cause allergic reactions include cow's milk, chicken eggs, peanuts and tree nuts, wheat, soy, fish and seafood. At the last congress of the European Association of Allergists and Clinical Immunologists (EAACI 2020), held in June 2020 in London (UK), fourteen allergens were discussed, sesame, celery, sulfites, mustard, soy and lupine were added to the standard eight. These foods are the most common cause of food allergies. This type of allergy is more common in children than in adults, and some children outgrow food allergies as they get older.
Food allergies are characterized by lethargy, diarrhea, vomiting, and skin symptoms such as urticaria, atopic dermatitis, oral allergy syndrome (itching, slight swelling of the mouth). A life-threatening reaction includes anaphylaxis, a condition in which a few minutes or hours after contact with an allergen, blood pressure suddenly decreases, which leads to circulatory failure and, as a result, inadequate saturation of organs and tissues with oxygen (“oxygen starvation”). Typical symptoms: tinnitus, weakness, dizziness, nausea, abdominal pain, urticaria with severe itching, swelling of the lips, tongue, uvula, difficulty breathing, cough, changes in heart rate, loss of consciousness. In case of anaphylaxis, an ambulance should be called immediately.
A life-threatening reaction includes anaphylaxis, a condition in which a few minutes or hours after contact with an allergen, blood pressure suddenly decreases, which leads to circulatory failure and, as a result, inadequate saturation of organs and tissues with oxygen (“oxygen starvation”). Typical symptoms: tinnitus, weakness, dizziness, nausea, abdominal pain, urticaria with severe itching, swelling of the lips, tongue, uvula, difficulty breathing, cough, changes in heart rate, loss of consciousness. In case of anaphylaxis, an ambulance should be called immediately.
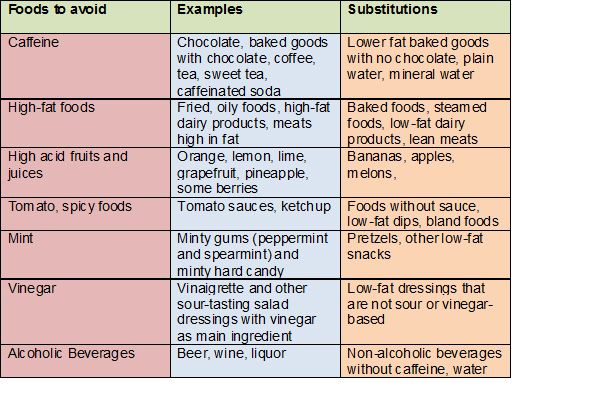
One of the most effective ways to fight allergies is a hypoallergenic diet. Accurate diagnosis of a food allergy is extremely important for the selection of an elimination diet with the exclusion of a causally significant food allergen. It is quite difficult to develop a competent nutrition algorithm on your own. Therefore, for the treatment of food allergies and the preparation of an optimal diet, you should contact specialists.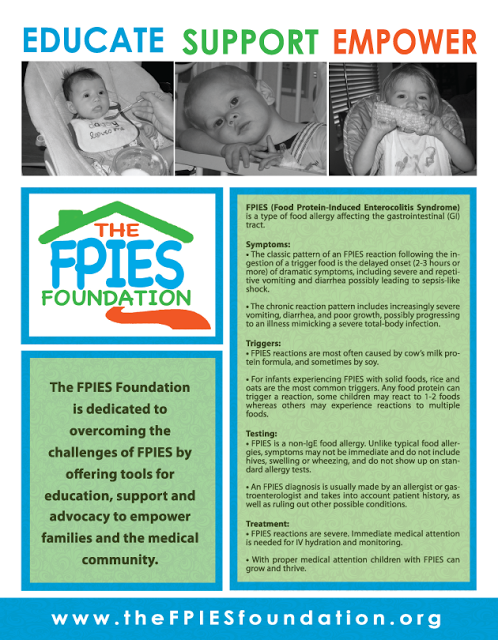 An allergist-immunologist will help you choose a diet taking into account the characteristics and taste preferences.
An allergist-immunologist will help you choose a diet taking into account the characteristics and taste preferences.
The specifics of the application of tests profile "Allergy to food"
With the help of laboratory diagnostics, you can find the allergen, eliminate it from the diet and thus protect yourself from unwanted reactions and their consequences.
Milk and its products are widely used in the food industry. Allergy to cow protein is common in young children. In adults, milk intolerance is more common, which indicates an enzymatic deficiency. The most common clinical manifestations of milk allergy can be skin manifestations (itchy rash, eczema, dermatitis), gastrointestinal symptoms (abdominal pain, vomiting, diarrhea, flatulence, constipation), and sometimes respiratory symptoms (cough, asthma attacks, rhinitis). If you are allergic to cow's milk, you can cross-react with beef.
Eggs also contain common allergens, with the most active allergenic component being albumin, which is part of the egg white. During cooking or frying, albumin disappears from the yolk, but remains in the protein. Like cow's milk protein, egg protein allergy develops in childhood. Products containing egg white should be excluded from the diet of an allergic person. Patients with egg allergy should also take medication and vaccinate with caution.
During cooking or frying, albumin disappears from the yolk, but remains in the protein. Like cow's milk protein, egg protein allergy develops in childhood. Products containing egg white should be excluded from the diet of an allergic person. Patients with egg allergy should also take medication and vaccinate with caution.
Cereals, as powerful allergens, can cause both food allergies and hay fever, that is, cause a reaction to cereal pollen. wheat has strong allergenic properties. Products containing wheat are widely distributed (wheat flour, starch, bran, cereals, pastries, pasta, sweets, beer, etc.). If you have an allergy, even inhaling wheat flour can cause an allergic reaction. Manifestations of wheat allergy can include gastrointestinal disorders, eczema, rhinitis, bronchial asthma, and even anaphylaxis.
Soya is widely used in the food industry and is a common cause of allergic reactions in adults and children. Soy can be found in confectionery, semi-finished meat products, medicines and cosmetics.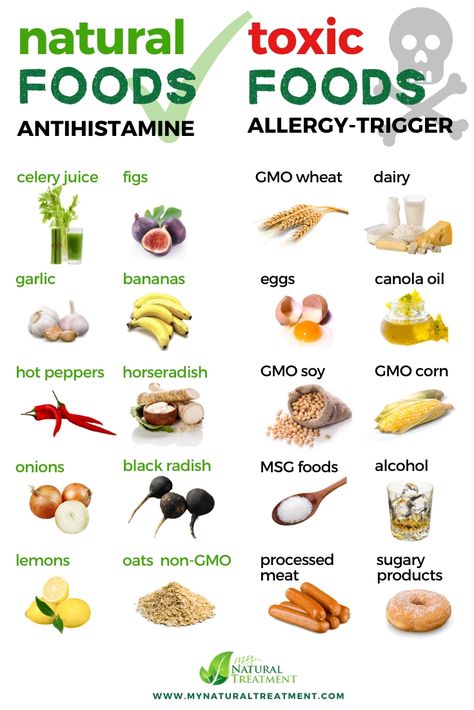 Soy is widely used as a filler, however this is often not listed on the packaging, instead it is usually written "plant protein filler". Cross-allergy to peanuts is possible. Children who are allergic to soy may develop an allergy to cow's milk.
Soy is widely used as a filler, however this is often not listed on the packaging, instead it is usually written "plant protein filler". Cross-allergy to peanuts is possible. Children who are allergic to soy may develop an allergy to cow's milk.
Peanuts and hazelnuts have pronounced allergenic properties and can cause the most severe cases of food allergies, up to anaphylaxis. May cause severe cases of food allergies. It is called "peanut-nut syndrome" or nut tree syndrome. Peanuts and hazelnuts are part of many culinary products: chocolate, liqueurs, cakes, muffins. Proteins of peanuts and nuts are thermostable and during heat treatment their allergenicity increases.
Carrots and celery are the most allergenic among umbelliferous crops, and tomato should be singled out among nightshade crops.
Orange, grapefruit, lemon - one of the most popular representatives of citrus fruits, they are sources of vitamins and a number of useful minerals, contain a significant amount of antioxidants and other biologically active substances. Allergy to citrus fruits is observed relatively often among other types of food allergic reactions. An allergic reaction is more often observed to one particular type of citrus fruits, and combined reactions to various representatives of citrus fruits are also possible.
Allergy to citrus fruits is observed relatively often among other types of food allergic reactions. An allergic reaction is more often observed to one particular type of citrus fruits, and combined reactions to various representatives of citrus fruits are also possible.
Allergy to crabs and shrimp is noted quite often, especially among residents of coastal areas. Many people with this type of allergy are sensitized only to this type of crustacean, but cross-allergy to other crustaceans (eg, lobster) and some types of fish can also occur. Allergy to fish protein is noted quite often. Despite this, most patients with this type of allergy are sensitized only to certain types of fish, in particular, to cod .
Baker's yeast is a single-celled microscopic fungus widely used in the production of bakery products, as well as in the field of scientific research and genetic engineering. Sensitization to yeast allergens may underlie allergic reactions to foods that contain yeast (eg bread, wine, and beer). Mushrooms are also important respiratory allergens. Allergy to baker's yeast can cause an allergic reaction to the hepatitis B vaccine because the recombinant hepatitis B surface antigen used in the vaccine is produced on baker's yeast, in the genetic material of which the gene responsible for the production of this protein is inserted.
Mushrooms are also important respiratory allergens. Allergy to baker's yeast can cause an allergic reaction to the hepatitis B vaccine because the recombinant hepatitis B surface antigen used in the vaccine is produced on baker's yeast, in the genetic material of which the gene responsible for the production of this protein is inserted.
Chocolate is a product whose components (cocoa butter, cocoa powder, sugar) in case of individual intolerance can cause allergic reactions in the form of atopic dermatitis, urticaria, angioedema. However, more often allergens in chocolate are various additives and substitutes. These are soy, peanut, palm, coconut oils, peanuts, nuts, flavors, soy lecithin, wheat gluten, raisins, dried apricots. Milk is also added to chocolate, which is a common cause of allergies in children.
Why the Food Allergy study is carried out
The profile includes a set of allergens that will make it possible to navigate the main points of nutrition and allow you to regulate the composition of foods in the diet, taking into account the risk of developing allergic manifestations. However, it is important to remember that the results of laboratory diagnostics are not a diagnosis. A positive result can only indicate the presence of sensitization to the product, therefore, it is necessary to contact allergologists for a full consultation and preparation of an individual diet based on a survey, examination and laboratory diagnostic data.
However, it is important to remember that the results of laboratory diagnostics are not a diagnosis. A positive result can only indicate the presence of sensitization to the product, therefore, it is necessary to contact allergologists for a full consultation and preparation of an individual diet based on a survey, examination and laboratory diagnostic data.
Infant Food Allergen IgE, mix fx5: Egg white, Milk, Fish, Wheat, Peanut, Soybean - f1, f2, f3, f4, f13, f14)
Description
Method of determination Immunofluorescence assay (ImmunoCAP).
Test material Blood serum
Home visit available
Online check-in
Detection of specific IgE to six food allergens that most often cause allergies in children. Used for laboratory confirmation of IgE sensitization in skin/food allergy symptoms. The answer is general for the mixture.
Food allergies and atopic dermatitis/eczema are most common among young children. Sometimes the causal dependence of allergic-like manifestations on certain food allergens can be established by eliminating the suspected product and assessing the patient's condition after cessation of contact with him. For the same purposes, skin allergy tests and / or blood tests are used to detect specific IgE antibodies, confirming the presence of allergic sensitization to the corresponding allergens. This is important for making the right recommendations for monitoring the child's condition, determining (if necessary) appropriate treatment, and timely referral to an allergist for follow-up. Food allergies and atopic dermatitis in the first years of life and family predisposition are considered risk factors for the subsequent development of allergy to inhalant allergens (“allergic march”).
A test that detects the presence of specific IgE to a mixture of six common food allergens can be used in addition to clinical assessment to screen for suspected food allergies in children.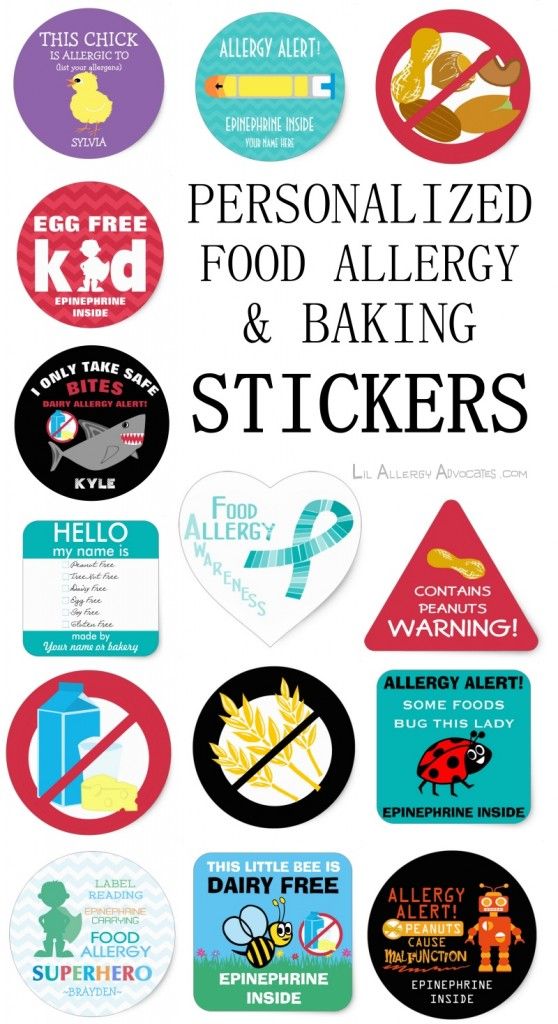 If the result of this study is positive, subsequent testing should be aimed at identifying specific causative allergens and based on the patient's history, taking into account the allergens with which he comes into contact.
If the result of this study is positive, subsequent testing should be aimed at identifying specific causative allergens and based on the patient's history, taking into account the allergens with which he comes into contact.
Preparation
Preferably 4 hours after the last meal, no requirement. Antihistamines do not affect the result. It is undesirable to conduct a study against the background of the use of glucocorticoid hormone preparations (you should consult with your allergist about the advisability of conducting a study or the conditions for canceling the corresponding drug).
Indications for use
in the presence of allergic-like symptoms (including skin, gastrointestinal) for the purpose of screening to confirm / exclude sensitization to common food allergens listed in the mixture, which most often cause food allergies in children.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: history, results of other examinations, etc.
The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: history, results of other examinations, etc.
Units: kU/l.
Limits of detection: 0.1-100 kU/l.
Reference values:
Interpretation of results
Increasing levels
- A result above the specified threshold confirms the presence of sensitization to one or more food allergens in the mixture, higher values indicate the level of sensitization. The causative allergen should be clarified by further testing. The diagnosis of allergy is established on the basis of clinical symptoms, taking into account the patient's history and examination results.
- False positive due to very high levels of total IgE.
Reduced levels
No sensitization to food allergens in the mixture.