Gavage feeding baby
Feeding in the NICU
9/21/2014
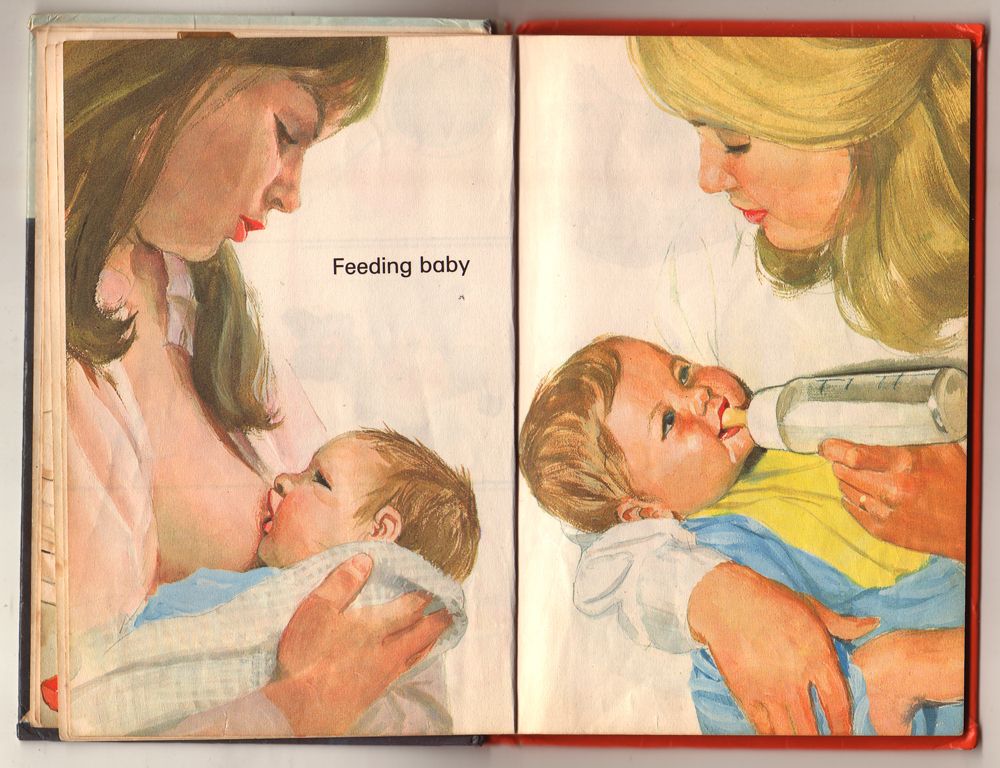
Most parents aren’t expecting a stint in the neonatal intensive care unit (NICU) when they welcome their new baby into the world so it isn’t an experience that parents typically prepare for. Well thought out plans like how to feed your baby may have to be altered, but you do have options in the NICU. The following article is a guide to feeding in the NICU, including some of the difficult situations that parents and babies encounter depending on the baby’s level of maturity. Please reach out to your trusted health care professionals for more information and support.
Overview Feeding in the NICU
Babies in the NICU often have feeding difficulties because the activity requires many different body systems, which often are not fully developed. Keep in mind that you may have many steps forward and some steps back in success with feeding; do not be discouraged by this.
Speech Therapy
Some NICUs use speech therapists to aid with feeding therapy. At some point, the speech therapist will evaluate every infant that is admitted to the NICU to determine whether there will be feeding difficulties. According to a speech therapist, Lee Ann Damian, from Dayton Children’s Hospital “The baby’s ability to feed and gain weight is not only a survival issue, but is one of the main factors in determining how quickly that baby can go home. The sooner we can get the baby happy and comfortable with feeding, the better it will be for the entire family.”
IV Therapy
Upon arriving at the NICU, baby will often be too sick or even too small to bottle or breastfeed. In this case, your baby’s medical team will insert a small catheter (IV) in one of three ways -- PICC lines, peripheral IV, and Umbilical Artery Catheter. The medical team will sometimes ask you to leave the NICU unit during this insertion to better concentrate. This therapy is used to deliver fluids and medications, which baby will eventually be weaned off of.
This therapy is used to deliver fluids and medications, which baby will eventually be weaned off of.
Gavage Feeding
A gavage must be used for feeding of babies who are smaller or too sick to be fed by bottle or breast. A small tube will be guided through the baby’s mouth or nose into the stomach and through this tube a small amount of breast milk or formula will be trickled into baby’s stomach. Inserting this tube will cause some discomfort, but after it is in place it can be left there for up to 7 days before needing to be changed. A pacifier will often be given while gavage feeding in order to strengthen your baby’s suckling. At about 32-34 weeks of age your baby should be strong enough to start transitioning into bottle or breastfeeding.
Breastfeeding in the NICU
It is important to make your baby’s medical team aware of your desire to breastfeed. A collaborative effort between the mother, nurses, and lactation consultants is required for a mother to be successful with breastfeeding their NICU baby. To heighten the chance of successful breastfeeding, the baby’s mother should start pumping immediately after birth and frequently (about every 2 hours or so). The mother should make sure to pump until the breast is empty of milk, including the hind milk that is high in milk fat and essential to baby’s nutritional needs. Do not be discouraged if you are producing a small amount of milk at first. It is important to be persistent during this process. Every mother is going to produce breast milk differently.
To heighten the chance of successful breastfeeding, the baby’s mother should start pumping immediately after birth and frequently (about every 2 hours or so). The mother should make sure to pump until the breast is empty of milk, including the hind milk that is high in milk fat and essential to baby’s nutritional needs. Do not be discouraged if you are producing a small amount of milk at first. It is important to be persistent during this process. Every mother is going to produce breast milk differently.
Breastfeeding in the NICU requires an enormous amount of patience. Preemies and sick babies take a long amount of time to learn the coordination of suckling, breathing, and swallowing. A popular method to start the breastfeeding process is Kangaroo Care, a method that involves skin-to-skin contact. During this process, the baby, clothed only in a diaper, will be snuggled up to your bare chest. This can be done by either the mother or father for several hours a day. Kangaroo Care has many benefits, including heart rate stabilization, increased weight gain, and will lead to a better chance to breastfeed. Parents feel some additional benefits from Kangaroo Care, such as increased sense of control, increased milk production, bonding, etc. Another helpful method is to introduce a pacifier dipped in breast milk. This helps promote suckling.
Parents feel some additional benefits from Kangaroo Care, such as increased sense of control, increased milk production, bonding, etc. Another helpful method is to introduce a pacifier dipped in breast milk. This helps promote suckling.
Kangaroo Care creates more opportunity for baby to “go to the breast.” This is a time for the baby to explore and smell mother’s nipple. It is important to pump before going on to this step so there will not be too much milk. Remember it takes the coordination of suckling, breathing, and swallowing on your baby’s part to be successful so it is central to be very patient.
Formula Feeding in the NICU
Although formula feeding might not have been your first option, your baby can thrive with this method too. There are many formula options and your NICU team will assist with picking the one best suited for your baby’s needs.
Although your baby’s time in the NICU will most likely include some challenges with feeding, there are many methods (many not included within this article) and skilled professionals to help you and your baby overcome them.
Resources
Feeding Matters mission is to bring pediatric feeding struggles to the forefront so infants and children are identified early, families' voices are heard, and medical professionals are equipped to deliver collaborative care. Feeding Matters overcome the complex issues of pediatric feeding struggles through our five mission pillars: Education, Advocacy, Research, Treatment, and Support.
Oley Foundation enriches the lives of those requiring home intravenous and tube feeding through education, outreach, and networking.Feeding Matters brings pediatric feeding struggles to the forefront so infants and children are identified early, families' voices are heard, and medical professionals are equipped to deliver collaborative care.
La Leche League supports mothers worldwide to breastfeed through mother-to-mother support, encouragement, information, and education
Feeding Tube Awareness Foundation dedicated to providing parents and caregivers with the information needed for day-to-day life with a child who is tube-fed.
Women, Infants and Children (WIC) provides Federal grants to States for supplemental foods, health care referrals, and nutrition education for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women, and to infants and children up to age five who are found to be at nutritional risk.
GI Kids provides easy to understand information about the treatment and management of these pediatric digestive conditions for children and parents
Hand to Hold provides comprehensive navigation resources and support programs to parents of preemies, babies born with special health care needs and those who have experienced a loss due to these or other complications.
United States Breastfeeding Committe (USBC): The mission of USBC is to improve the Nation's health by working collaboratively to protect, promote, and support breastfeeding.
WIC The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides Federal grants to States for supplemental foods, health care referrals, and nutrition education for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women, and to infants and children up to age five who are found to be at nutritional risk.
PLEASE NOTE: The contents of this article is for informational purposes only. Nothing contained in this article should be considered or used as a substitute for professional medical or mental health advice, diagnosis, or treatment.
References
"How to Feed your NICU Baby." Bay State Health. N.p., n.d. Web. 14 Sept. 2014. <http://baystatehealth.com/Baystate/Main+
"In the NICU." Feeding your baby in the NICU. N.p., 1 Aug. 2014. Web. 14 Sept. 2014. <http://www.marchofdimes.org/baby/feeding-your-baby-in-the-nicu.aspx>.
"Meeting the Challenges of Breast-Feeding in the NICU." Pregnancy.org. N.p., n.d. Web. 14 Sept. 2014. <http://www.pregnancy.org/article/meeting-challenges-breast-feeding-nicu>.
"NICU Feeding Baby Steps." The Chester County Hospital. N.p., n.d. Web. 14 Sept. 2014. <http://www.chestercountyhospital.org/cchpage.asp?p=1424>.
"Pediatric Dysphagia." : Overview. Web. 14 Sept. 2014. http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934965§ion=Assessment.
Web. 14 Sept. 2014. http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934965§ion=Assessment.
"Speech therapy in the NICU: Key to babies' survival." Speech therapy for premature newborns : The Children's Medical Center of Dayton. Web. 14 Sept. 2014. http://www.childrensdayton.org
Transitioning from gavage to full oral feeds in premature infants: When should we discontinue the nasogastric tube?
Transitioning from gavage to full oral feeds in premature infants: When should we discontinue the nasogastric tube?
Download PDF
Your article has downloaded
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
Download PDF
- Article
- Published:
- Sreekanth Viswanathan ORCID: orcid.
 org/0000-0002-1367-91341,2 &
org/0000-0002-1367-91341,2 & - Sudarshan Jadcherla1,2
Journal of Perinatology volume 39, pages 1257–1262 (2019)Cite this article
-
7512 Accesses
-
7 Citations
-
Metrics details
Subjects
- Motility disorders
- Outcomes research
Abstract
Background
The optimal timing for discontinuation of nasogastric (NG) tube in premature infants transitioning to oral feeding is not known.
Objective
To determine whether early removal of NG-tube is appropriate in low-risk premature infants.
Methods
Prospectively collected data of premature infants started on oral feeds at ≤34 weeks gestation were reviewed. Infants were categorized into ‘early’ or ‘late’ NG-removal groups based on the proportion of oral intake in the preceding 2-days, i.e., 60–79% or 80–100% of the total volume, respectively.
Results
In total 50 infants in early group vs. 43 in late group. Both groups had similar oral intake and weight change in the subsequent 2-days post-NG removal. The days from NG-removal to target oral volume, and to hospital discharge trended shorter in early vs. late group.
Conclusions
Discontinuing NG-tube when the oral feeding competency reaches ~75% of prescribed feeding volume is safe and appropriate in low-risk premature infants.
Introduction
Successful transition from full gavage to independent oral feedings is a criterion of hospital discharge in premature infants [1]. Delay in achieving full oral feeding milestone is one of the main reasons for delays in hospital discharge [2,3,4], and adverse neurodevelopmental outcome in premature infants [5]. During this period of functional immaturity of coordinating sucking, swallowing, and breathing [6], many premature infants require enteral feeding, usually by a nasogastric (NG) tube, until they achieve adequate oral feeding skills. The optimal timing for discontinuation of NG tube feeding in premature infants transitioning to oral feeding is not known, and thus associated with practice variation.
Some of the cue-based oral feeding protocols suggest to keep the NG feeding tube until the infant have appropriate weight gain for 48 hours without supplementation by NG tube [7,8,9]. However, having a NG tube is not without problems. In presence of NG tube especially with size >5F, premature infants have increased nasal airway resistance [10, 11], and reduced tidal volume and minute ventilation during sucking, which can affect their oral feeding performance [12]. Its presence can potentially increase the gastroesophageal reflux (GER) events depending on the size of NG tube [13, 14]. Use of NG tube is also associated with significant nutrient loss, especially fat, fat soluble vitamins, and minerals because fat adheres to tubing surfaces [15], and is a potential source of infection as it is easily colonized by pathogenic bacteria/fungi [16].
In presence of NG tube especially with size >5F, premature infants have increased nasal airway resistance [10, 11], and reduced tidal volume and minute ventilation during sucking, which can affect their oral feeding performance [12]. Its presence can potentially increase the gastroesophageal reflux (GER) events depending on the size of NG tube [13, 14]. Use of NG tube is also associated with significant nutrient loss, especially fat, fat soluble vitamins, and minerals because fat adheres to tubing surfaces [15], and is a potential source of infection as it is easily colonized by pathogenic bacteria/fungi [16].
If earlier removal of NG tube is safe and feasible, it can potentially reduce these complications and length of hospital stay in premature infants. Our study objective was to determine whether early removal of NG tube is safe and appropriate in relatively low-risk premature infants transitioning to oral feeding. We hypothesize that earlier removal of NG tube would lead to earlier transition to independent oral feeding resulting in decreased length of hospital stay.
Methods
The study was conducted at the all-referral level IV neonatal intensive care unit (NICU) at Nationwide Children’s Hospital, Columbus, Ohio. As part of an ongoing quality improvement (SIMPLE feeding initiatives) [17], focused on prevention and early identification of feeding related problems in premature infants, data of all infants admitted at ≤34 weeks’ post-menstrual age (PMA) were collected prospectively. NG tube sizes 6.5F or 8.0F was used for enteral feeding and feedings were typically given intermittently over 10–30min every 3 h. There was no unit guideline regarding the timing of NG tube removal during the study period from Jan 2011 to Dec 2017. In general, the decision to remove NG tube occurs when the oral feeding volume reaches 60–100% of prescribed enteral feeding depending on the individual provider comfort level.
To meet the objective of this study, SIMPLE feeding program database was reviewed for ‘low-risk’ premature infants which we defined as infants born ≤32 weeks’ gestation and had started on cue based oral feeds at ≤34 weeks’ PMA. Infants on invasive respiratory support (>2L of nasal cannula support, CPAP or ventilator support), gastrointestinal surgical conditions, intraventricular hemorrhage > grade 2, and major congenital anomalies were excluded. Among eligible infants, the day of NG tube removal was recorded and the percentage of oral feeding volume (OFV) in the preceding two days of NG tube removal was calculated from the electronic medical records. Infants were categorized into ‘early’ and ‘late’ NG removal groups. In early group, NG tube was removed when the mean OFV was between 60–79% of prescribed feeding volume in the preceding 2 days, while in late group, it occurred at 80–100%. Infants with mean OFV less than 60% in the preceding 2 days of NG removal were excluded considering their relatively quicker progression and more mature oral feeding skills. For both groups, characteristics before and at NG removal were collected from the SIMPLE feeding program database and electronic medical records. The clinical outcomes including time from NG removal to reach the target full oral feeding volume (ability to take PO of all prescribed enteral feeding volume, which generally ranges from 130 to 150 ml/kg) and to NICU discharge, and growth metrics were compared between the two groups.
Infants on invasive respiratory support (>2L of nasal cannula support, CPAP or ventilator support), gastrointestinal surgical conditions, intraventricular hemorrhage > grade 2, and major congenital anomalies were excluded. Among eligible infants, the day of NG tube removal was recorded and the percentage of oral feeding volume (OFV) in the preceding two days of NG tube removal was calculated from the electronic medical records. Infants were categorized into ‘early’ and ‘late’ NG removal groups. In early group, NG tube was removed when the mean OFV was between 60–79% of prescribed feeding volume in the preceding 2 days, while in late group, it occurred at 80–100%. Infants with mean OFV less than 60% in the preceding 2 days of NG removal were excluded considering their relatively quicker progression and more mature oral feeding skills. For both groups, characteristics before and at NG removal were collected from the SIMPLE feeding program database and electronic medical records. The clinical outcomes including time from NG removal to reach the target full oral feeding volume (ability to take PO of all prescribed enteral feeding volume, which generally ranges from 130 to 150 ml/kg) and to NICU discharge, and growth metrics were compared between the two groups. OFV in infants who are on direct breast feeding was considered as 150 ml/kg after the NG removal. The project was approved by the Nationwide Children’s Hospital Institutional Review Board.
OFV in infants who are on direct breast feeding was considered as 150 ml/kg after the NG removal. The project was approved by the Nationwide Children’s Hospital Institutional Review Board.
Statistics
Appropriate bivariate analysis was performed to identify the unadjusted differences between the cases and controls. Student’s t-test was used for parametric continuous variables, and the Mann–Whitney U test was used for nonparametric continuous variables. Chi-square tests and Fisher exact tests were used for categorical variables. All quantitative data were expressed as the mean ± standard deviation (SD), or median with inter-quartile range. A p ≤ 0.05 was considered to be statistically significant. The statistical software IBM SPSS Statistics version 23 (SPSS, Chicago, IL) was used for the statistical analysis of the data.
Results
Of the 93 eligible infants during the study period, 50 infants were in early NG removal group, the rest 43 were in late NG removal group. Early group had similar perinatal and birth characteristics, compared to the late group except that late group were exposed to more number of CPAP days (Table 1). At NG tube removal, early group had similar corrected gestational age, and body weight compared to the late group (Table 1). Early group had similar direct breast feeding rate at NG removal compared to late group (30.0 vs. 16.3%, p = 0.12). The mean OFV % in the preceding two days of NG removal was 72.3 ± 5.8 in the early group vs. 87.3 ± 4.0 in the late group (p < 0.001). The oral feeding volume and weight change in the subsequent two days after NG removal were similar in both groups (Fig. 1, Table 2). Supplemental oxygen use at initial oral feeding, at NG tube removal, at 36 weeks’ gestation, and at NICU discharge were similar in both groups. Majority of the infants reached full oral target volume before discharge (90% in early vs. 88.4 in late group, p = 0.80). Early group showed a trend for lower number of days from the NG removal to reach oral target volume (median days of 2.
Early group had similar perinatal and birth characteristics, compared to the late group except that late group were exposed to more number of CPAP days (Table 1). At NG tube removal, early group had similar corrected gestational age, and body weight compared to the late group (Table 1). Early group had similar direct breast feeding rate at NG removal compared to late group (30.0 vs. 16.3%, p = 0.12). The mean OFV % in the preceding two days of NG removal was 72.3 ± 5.8 in the early group vs. 87.3 ± 4.0 in the late group (p < 0.001). The oral feeding volume and weight change in the subsequent two days after NG removal were similar in both groups (Fig. 1, Table 2). Supplemental oxygen use at initial oral feeding, at NG tube removal, at 36 weeks’ gestation, and at NICU discharge were similar in both groups. Majority of the infants reached full oral target volume before discharge (90% in early vs. 88.4 in late group, p = 0.80). Early group showed a trend for lower number of days from the NG removal to reach oral target volume (median days of 2.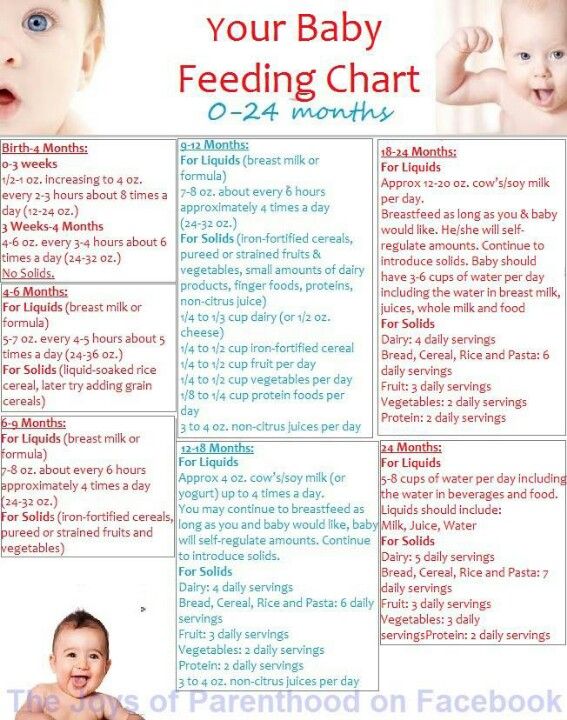 0 vs 2.5, p = 0.13, mean days 2.4 ± 1.9 vs. 4.4 ± 5.8, p = 0.051), and to NICU discharge (mean days of 10.9 vs. 13.5, p = 0.21), compared to late group. None required replacing NG tube in both groups, and none required tube feeding at discharge. The NICU discharge outcomes including BPD (oxygen requirement at 36 week PMA), length of hospital stay (LOHS), OFV, and discharge weight were similar in both groups (Table 2). A subgroup analysis of infants born ≤28 weeks and >29 weeks also did not show differences between early and late groups (Table 3).
0 vs 2.5, p = 0.13, mean days 2.4 ± 1.9 vs. 4.4 ± 5.8, p = 0.051), and to NICU discharge (mean days of 10.9 vs. 13.5, p = 0.21), compared to late group. None required replacing NG tube in both groups, and none required tube feeding at discharge. The NICU discharge outcomes including BPD (oxygen requirement at 36 week PMA), length of hospital stay (LOHS), OFV, and discharge weight were similar in both groups (Table 2). A subgroup analysis of infants born ≤28 weeks and >29 weeks also did not show differences between early and late groups (Table 3).
Full size table
Fig. 1Percentage of oral feeding volume (OFV) in early vs. late nasogastic tube removal groups
Full size image
Table 2 Outcomes after NG tube removal and at NICU discharge in early and late NG removal groupsFull size table
Table 3 Subgroup analysis stratified by GA (GA ≤ 28 vs. >29 weeks) of characteristics in the early and late NG removal groups
>29 weeks) of characteristics in the early and late NG removal groupsFull size table
Discussion
The purpose of this study was to determine whether early removal of NG tube is safe and appropriate in relatively low-risk premature infants transitioning to oral feeding. By using a prospectively collected clinical database of premature infants enrolled in the SIMPLE feeding program at our all-referral NICU, our study suggests that discontinuing NG tube when the oral feeding competency reaches ~75% of prescribed enteral feeding volume in the preceding two days is safe and appropriate in low-risk premature infants. The practice of keeping the NG tube until these infants reach their full targeted oral feeding volume is not associated with any significant clinical benefits.
In routine clinical practice, the decision to remove the NG tube is often based on the oral feeding performance of infants in the preceding days. The relationship between chronological age and functional maturity of the oral feeding skills is no t always linear, and is often influenced by growth metrics and associated co-morbidities [18]. Because of the positive association between postnatal growth and neurodevelopmental outcomes [19], potential for faltering growth with early NG tube removal is often a concern among neonatal providers. However, our data of relatively stable low-risk premature infants who have made steady oral feeding progression suggest that discontinuing NG tube when the OFV reaches about ¾ of the prescribed enteral feeding volume was not associated with significant reduction in time to achieve targeted oral feeding volume or subsequent postnatal growth until NICU discharge. Even though the late group infants were exposed to more number of CPAP days suggesting more severe early lung disease, the use of supplemental oxygen need during the oral feeding period, at 36 weeks, and at hospital discharge were similar between the two groups. Similar to our study, Fucile et al. [20], reported that setbacks in oral feeding progression are least likely to occur when the oral feeding attempt frequency reaches 6–8/day vs.
Because of the positive association between postnatal growth and neurodevelopmental outcomes [19], potential for faltering growth with early NG tube removal is often a concern among neonatal providers. However, our data of relatively stable low-risk premature infants who have made steady oral feeding progression suggest that discontinuing NG tube when the OFV reaches about ¾ of the prescribed enteral feeding volume was not associated with significant reduction in time to achieve targeted oral feeding volume or subsequent postnatal growth until NICU discharge. Even though the late group infants were exposed to more number of CPAP days suggesting more severe early lung disease, the use of supplemental oxygen need during the oral feeding period, at 36 weeks, and at hospital discharge were similar between the two groups. Similar to our study, Fucile et al. [20], reported that setbacks in oral feeding progression are least likely to occur when the oral feeding attempt frequency reaches 6–8/day vs. 1–2 or 3–5 per day. In our center, we generally consider hospital discharge, once infant is 48h off-NG tube feeding if there are no other medical or social reasons. However, infants in both our study groups were discharged from the NICU about 11–13 days after the NG tube removal. This suggests that attaining oral feeding competency is not the only reason that was delaying NICU discharge in our study population. Considering our NICU being an all-referral center, the complexity of referred infants’ initial NICU course, incidence of clinical BPD at 36 weeks PMA in about 1/3 of study infants, and other unmeasured medical and social variables may have affected the timing of NICU discharge. However, considering our specific inclusion and exclusion criteria and that all our study patients were started on oral feeding ≤34 weeks’ PMA suggest that our study cohort represents the relatively low-risk premature infants in a contemporary academic NICU hospital setting. Though the described approach and conclusions are limited to the select inclusions and exclusions of our study population, we believe, these findings may be relevant to most level-II NICUs or step-down units where the majority of such low-risk premature infants are admitted.
1–2 or 3–5 per day. In our center, we generally consider hospital discharge, once infant is 48h off-NG tube feeding if there are no other medical or social reasons. However, infants in both our study groups were discharged from the NICU about 11–13 days after the NG tube removal. This suggests that attaining oral feeding competency is not the only reason that was delaying NICU discharge in our study population. Considering our NICU being an all-referral center, the complexity of referred infants’ initial NICU course, incidence of clinical BPD at 36 weeks PMA in about 1/3 of study infants, and other unmeasured medical and social variables may have affected the timing of NICU discharge. However, considering our specific inclusion and exclusion criteria and that all our study patients were started on oral feeding ≤34 weeks’ PMA suggest that our study cohort represents the relatively low-risk premature infants in a contemporary academic NICU hospital setting. Though the described approach and conclusions are limited to the select inclusions and exclusions of our study population, we believe, these findings may be relevant to most level-II NICUs or step-down units where the majority of such low-risk premature infants are admitted.
This study was observational single-center study; consist of a heterogeneous group of relatively stable premature infants born at different gestational ages, but appropriate PMA for oral feeding initiation and maintenance. The primary outcome of the study (Days from NG removal to target full oral feeds, median days of 2.0 vs. 2.5, p = 0.13, mean days 2.4 ± 1.9 vs. 4.4 ± 5.8, p = 0.051) showed a trend for lower number of days in the early group, compared to the late group. Assuming parametric distribution of the variable, the difference between the groups has a small to medium effect size of 0.46. With this effect size, a statistically significant difference in days from NG removal to target full oral feeds between the two groups can be obtained from a sample size of 148 (74 in each group) with 80% power (α = 0.05, β = 0.20). The decision to remove NG tube was not based on a standardized unit practice, but was based on the individual provider discretion, which can be a limitation in that it adds to the subjectivity in approaches. Variability in individual views among a large number of NICU providers potentially may have influenced the study group determination and the outcomes observed. Generalization of these findings to premature infants with significant comorbidities or anomalies must be applied with caution, as our study participants did not include such patients.
Variability in individual views among a large number of NICU providers potentially may have influenced the study group determination and the outcomes observed. Generalization of these findings to premature infants with significant comorbidities or anomalies must be applied with caution, as our study participants did not include such patients.
In summary, lack of consensus regarding the timing of NG tube removal in relation to oral feeding competency in premature infants can be associated with practice variation among individual providers. Our study suggests that discontinuing NG tube when the oral feeding competency reaches ~75% of prescribed enteral feeding volume in the preceding two days is safe and appropriate in stable low-risk premature infants. Keeping NG tube longer is not associated with any additional clinical benefits. As there is no harm in discontinuing NG tube at ~75% oral feeding competency, as evidenced by similarities in growth and LOHS, at least in monitored clinical settings, this practice can be safe and may have potential benefits in lowering resource utilization, potentially reduce the length of hospitalization, increase opportunities for parent participation, all resulting in cutting down the healthcare costs.
References
Newborn AAoPCoFa. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Article Google Scholar
Jadcherla SR, Wang M, Vijayapal AS, Leuthner SR. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol. 2010;30:201–8.
Article CAS Google Scholar
Pickler RH, Reyna BA, Wetzel PA, Lewis M. Effect of four approaches to oral feeding progression on clinical outcomes in preterm infants. Nurs Res Pract. 2015;2015:716828.
PubMed PubMed Central Google Scholar
Walsh MC, Bell EF, Kandefer S, Saha S, Carlo WA, D’angio CT, et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants.
 Pedia Res. 2017;82:297–304.
Pedia Res. 2017;82:297–304.Article Google Scholar
Lainwala S, Kosyakova N, Power K, Hussain N, Moore JE, Hagadorn JI, et al. Delayed achievement of oral feedings is associated with adverse neurodevelopmental outcomes at 18 to 26 months follow-up in preterm infants. Am J Perinatol. 2019. https://doi.org/10.1055/s-0039-1681059. [Epub ahead of print]
Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92:721–7.
Article CAS Google Scholar
Kirk AT, Alder SC, King JD. Cue-based oral feeding clinical pathway results in earlier attainment of full oral feeding in premature infants. J Perinatol. 2007;27:572–8.
Article CAS Google Scholar
Kamitsuka MD, Nervik PA, Nielsen SL, Clark RH.
 Incidence of nasogastric and gastrostomy tube at discharge is reduced after implementing an oral feeding protocol in premature (< 30 weeks) infants. Am J Perinatol. 2017;34:606–13.
Incidence of nasogastric and gastrostomy tube at discharge is reduced after implementing an oral feeding protocol in premature (< 30 weeks) infants. Am J Perinatol. 2017;34:606–13.Article Google Scholar
Davidson E, Hinton D, Ryan-Wenger N, Jadcherla S. Quality improvement study of effectiveness of cue-based feeding in infants with bronchopulmonary dysplasia in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2013;42:629–40.
Article Google Scholar
Greenspan JS, Wolfson MR, Holt WJ, Shaffer TH. Neonatal gastric intubation: differential respiratory effects between nasogastric and orogastric tubes. Pedia Pulmonol. 1990;8:254–8.
Article CAS Google Scholar
Bohnhorst B, Cech K, Peter C, Doerdelmann M. Oral versus nasal route for placing feeding tubes: no effect on hypoxemia and bradycardia in infants with apnea of prematurity.
 Neonatology. 2010;98:143–9.
Neonatology. 2010;98:143–9.Article Google Scholar
Shiao SY, Youngblut JM, Anderson GC, DiFiore JM, Martin RJ. Nasogastric tube placement: effects on breathing and sucking in very-low-birth-weight infants. Nurs Res. 1995;44:82–88.
CAS PubMed Google Scholar
Peter CS, Wiechers C, Bohnhorst B, Silny J, Poets CF. Influence of nasogastric tubes on gastroesophageal reflux in preterm infants: a multiple intraluminal impedance study. J Pediatr. 2002;141:277–9.
Article Google Scholar
Murthy SV, Funderburk A, Abraham S, Epstein M, DiPalma J, Aghai ZH. Nasogastric feeding tubes may not contribute to gastroesophageal reflux in preterm infants. Am J Perinatol. 2018;35:643–7.
Article Google Scholar
Rogers SP, Hicks PD, Hamzo M, Veit LE, Abrams SA. Continuous feedings of fortified human milk lead to nutrient losses of fat, calcium and phosphorous. Nutrients. 2010;2:230–40.
Article CAS Google Scholar
Petersen SM, Greisen G, Krogfelt KA. Nasogastric feeding tubes from a neonatal department yield high concentrations of potentially pathogenic bacteria- even 1 d after insertion. Pediatr Res. 2016;80:395–400.
Article Google Scholar
Jadcherla SR, Dail J, Malkar MB, McClead R, Kelleher K, Nelin L. Impact of process optimization and quality improvement measures on neonatal feeding outcomes at an all-referral neonatal intensive care unit. JPEN J Parent Enter Nutr. 2016;40:646–55.
Article Google Scholar
Lau C. Development of infant oral feeding skills: what do we know? Am J Clin Nutr.
 2016;103:616S–621S.
2016;103:616S–621S.Article CAS Google Scholar
Latal-Hajnal B, von Siebenthal K, Kovari H, Bucher HU, Largo RH. Postnatal growth in VLBW infants: significant association with neurodevelopmental outcome. J Pediatr. 2003;143:163–70.
Article Google Scholar
Fucile S, Phillips S, Bishop K, Jackson M, Yuzdepski T, Dow K. Identification of a pivotal period in the oral feeding progression of preterm infants. Am J Perinatol. 2019;36:530–6.
Article Google Scholar
Download references
Author information
Authors and Affiliations
Division of Neonatology, Department of Pediatrics, Nationwide Children’s Hospital, The Ohio State University College of Medicine, Columbus, OH, USA
Sreekanth Viswanathan & Sudarshan Jadcherla
Neonatal and Infant Feeding Disorders Research Program, Center for Perinatal Research, The Research Institute at Nationwide Children’s Hospital, Columbus, OH, USA
Sreekanth Viswanathan & Sudarshan Jadcherla
Authors
- Sreekanth Viswanathan
View author publications
You can also search for this author in PubMed Google Scholar
- Sudarshan Jadcherla
View author publications
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sreekanth Viswanathan.
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and Permissions
About this article
This article is cited by
-
Oral-feeding guidelines for preterm neonates in the NICU: a scoping review
- Lise Bakker
- Bianca Jackson
- Anna Miles
Journal of Perinatology (2021)
Download PDF
Associated Content
Collection
The Importance of Nutrition: From Fetuses to Adolescents
Bolus Feeding Using a Syringe)
Your child is discharged from the hospital with a nasogastric (NG) feeding tube in place. The tube is a thin, soft tube that is inserted into the baby's stomach through the nose. This tube delivers liquid food directly to the stomach. Before your baby was released from the hospital, you were shown how to feed with a nasogastric tube. This memo will help you remember the necessary procedure for feeding at home. You can also get help from a district nurse at your home.
The tube is a thin, soft tube that is inserted into the baby's stomach through the nose. This tube delivers liquid food directly to the stomach. Before your baby was released from the hospital, you were shown how to feed with a nasogastric tube. This memo will help you remember the necessary procedure for feeding at home. You can also get help from a district nurse at your home.
NOTE: There are many different types of nasogastric tubes, feeding syringes, and pumps. The appearance and function of the nasogastric tube and accessories prescribed for your child may differ from those shown and described below. Always follow the advice of your child's primary care physician or district nurse. Write down their phone numbers in case you need help. Also write down the phone number of the facility that supplies medical equipment for your child. In the future, you will need to order additional accessories that your child may need. Write down all the phone numbers you need in the spaces below.
Write down all the phone numbers you need in the spaces below.
Healthcare provider phone number: _________________________________________________________
Home health nurse phone number: _________________________________________________
Medical supply company phone number: ______________________
Types of feeding
-
Two types of feeding can be performed with a nasogastric tube:
-
bolus feeding. Several times a day, an amount of liquid food, commensurate with one meal, is fed through the tube. Bolus feeding is done with a syringe or pump;
-
continuous feeding. Liquid food drips slowly through the tube. Continuous power is supplied by a pump.
-
-
Your child may be prescribed one or both types of food.
 Detailed instructions for each type of food are given below.
Detailed instructions for each type of food are given below.
Syringe Bolus
Your child's doctor or district nurse will tell you how much liquid food to use with each bolus. You will also be told how many times a day to feed your baby. Record this information below.
How much to give at each feeding: _____________
Number of feedings per day (How often to feed): __________________________
Accessories
Actions
-
Wash your hands with soap and water.
-
Make sure the tube is in the stomach (as you were shown in the hospital). Be sure to perform this step BEFORE feeding begins.
-
Check liquid food label and expiration date. Never use jars (or bags) with food that have already expired.
 In this case, you must use a new jar (or bag) with food.
In this case, you must use a new jar (or bag) with food. -
Open the hole plug at the end of the food probe.
-
Remove the plunger of the feeding syringe.
-
Connect the feeding syringe to the feeding port of the probe.
-
Gently bend or squeeze the probe with one hand. While holding the tube bent or pinched, slowly draw the liquid food into the feeding syringe with your free hand. In this case, the food will not flow through the probe, which will allow you to measure its amount.
-
Fill the feeding syringe to the level prescribed by the child's healthcare provider.
-
The probe can now be released.
-
Hold the feeding syringe straight.
 In this case, the food will pass through the probe by gravity without additional pressure. Adjust the angle of the feeding syringe to control the rate of fluid flow.
In this case, the food will pass through the probe by gravity without additional pressure. Adjust the angle of the feeding syringe to control the rate of fluid flow. -
If the food flows too slowly or does not flow at all, insert the plunger into the syringe. Gently, lightly press the piston. This will remove any particles blocking or clogging the probe. Do not push the syringe plunger all the way or with force.
-
Refill the feeding syringe with food if necessary. Repeat the above steps until the child receives the prescribed amount of food.
-
After feeding, rinse the tube with water (as you were shown in the hospital).
-
Disconnect the feeding syringe.
-
Close the cap on the food inlet of the probe.

| AddiAdditional instructions:_________________________________________________________________________________ ________________________________________________________________________________________________ ________________________________________________________________________________________________ ________________________________________________________________________________________________ |
Call your doctor right away if you experience any of the following.
-
The child has trouble breathing.
-
Formation of redness, swelling (swelling), leakage (leakage), ulcers (sores) or suppuration (pus) on the skin in the area of the probe.

-
Presence of blood (blood) around the probe, in the child's stool or stomach contents.
-
Baby coughing (cough), shortness of breath (choke) or vomiting (vomit) while feeding.
-
Urebenka swollen (bloated abdomen) or hard abdomen (rigid abdomen) (abdomen hard with light pressure).
-
Child diarrhea (diarrhea) or constipation (constipation).
-
Child temperature (fever) 38˚C ( 100.4° F) or higher.
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes no
Tell us more.

Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Enteral nutrition (tube feeding)
What is enteral nutrition?
Sometimes during treatment and recovery, children with cancer cannot get the calories and nutrients they need orally. Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Typically, the tube is inserted in two ways:
- Nasal (non-surgical)
- Through a small incision in the abdomen (surgical method)
Most commonly used are nasogastric tubes and gastrostomy tubes. But there are several types of enteral feeding tubes that differ in the method of insertion and location in the digestive tract.
Sometimes the patient is simply not able to eat enough calories or protein. There is no fault in this. It is important to help your child understand that nutritional support is not a punishment. Most children get used to the enteral feeding tube quickly. It is important that the child does not touch or pull the phone. Follow skin care instructions at the insertion site to avoid irritation or infection.
A nasogastric tube is inserted into the stomach or small intestine through the nose and throat.
Enteral feeding tube types
Enteral feeding tube connects to the stomach or small intestine. The location depends on how the patient tolerates the formula and how well their body is able to digest the nutrients. If possible, they try to place the probe in the stomach so that digestion occurs naturally.
There are 5 types of enteral feeding tubes:
Nasogastric Tube . A nasogastric tube is inserted into the stomach through the nose. It passes through the throat, esophagus and into the stomach.
Nasojejunal Probe . A nasojejunal tube is similar to a nasogastric tube but passes through the entire stomach into the small intestine.
Gastrostomy Tube (Gastrostomy Probe) . A gastrostomy tube is inserted through a small incision in the skin. The probe in this case passes through the wall of the abdominal cavity directly into the stomach.
Gastrojejunostomy tube (gastrojejunostomy probe) . The gastrojejunostomy tube is inserted into the stomach like a gastrostomy tube, but passes through the stomach into the small intestine.
Jejunostomy Probe . A jejunostomy tube is inserted through a small incision in the skin and passed through the abdominal wall into the small intestine.
Nasal tubes, including nasogastric and nasojejunal tubes, are generally used for short-term enteral feeding, usually not more than 6 weeks. The probe comes out of the nostril and is attached to the skin with adhesive tape. Nasogastric and nasojejunal tubes have a number of advantages, such as a low risk of infection and a simple insertion procedure. However, the probe must be attached to the face, and this worries some children. Other children may have problems with the nasogastric tube due to chemotherapy, which irritates the skin and mucous membranes.
Surgical insertion tubes - gastrostomy tube, gastrojejunostomy tube and jejunostomy tube - are used for longer periods of time or if a nasal tube cannot be placed in the child. The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
-
Insertion of nasogastric and nasojejunal tubes
-
Gastrostomy, gastrojejunostomy and jejunostomy insertion
After healing, the stoma usually does not hurt. The child can perform most daily activities.
Side effects of enteral nutrition
The most common side effects of enteral nutrition are nausea, vomiting, stomach cramps, diarrhoea, constipation and bloating.
There may be other side effects:
- Infection and irritation at the insertion site
- Probe misaligned or falling out
- Lung feeding formula
Most side effects can be avoided by following the care and nutrition instructions.
Feeding babies with tubes in place
The nutritionist is responsible for providing the baby with all the necessary nutrients. In children with cancer, an enteral feeding tube is often used in addition to what the child can eat normally. However, some patients have to enter all the nutrients through a tube.
The patient is prescribed a mixture containing:
- Calories
- Fluid
- Carbohydrates
- Fats
- Protein
- Vitamins and minerals
Standard formulas are suitable for many patients. For babies, it is preferable to use breast milk. Some children need special formulas that take into account their characteristics: the presence of allergies, diabetes or digestive problems.
It is very important for family members to work closely with a nutritionist. Nutritional needs may change due to changes in the child's health or side effects such as vomiting or diarrhea.
Types of enteral feeding
There are three types of enteral feeding - bolus, continuous and gravity.
Bolus feeding - large doses of the mixture are given to the patient by tube several times a day. This species is closest to the usual diet.
Continuous Power - Electronic pump delivers small doses of formula over several hours. Some children may need continuous feeding to reduce nausea and vomiting.
Gravity Feeding - A bag of formula is placed on the IV stand and a predetermined amount of formula is dripped through the tube at a slow rate. The duration of such nutrition depends on the needs of the patient.
Enteral feeding at home
Children can go home with a feeding tube. The doctors will ensure that family members know how to feed and care for the probe. Family members need to pay attention to the following issues:
- Weight gain or loss
- Vomiting or diarrhea
- Dehydration
- Infection
Formulas, Consumables, and Equipment Required:
- Formula: Most enteral formulas are sold ready-made.
 Some are available as a powder or liquid to mix with water.
Some are available as a powder or liquid to mix with water. - Syringe
- Adapter tube (if the child has a button tube for long-term enteral nutrition)
- Pump (with continuous power)
- Feeding formula bag with tubing (for continuous feeding)
- IV Stand (Gravity Feed)
General tips for enteral feeding at home:
- Always wash your hands with soap and water before feeding your baby.
- Make sure the baby's head is above the stomach.
- Throw away any ready-made or homemade formulas that have been opened and kept in the refrigerator for 24 hours or more.
- Store mixed formulations in the refrigerator and discard after 24 hours.
- Ready-to-use formulas do not need to be refrigerated.
- Do not empty the syringe completely during feeding.
- Wash the syringe (and transfer tube, if used) with warm water and dishwashing detergent after each use.
- Watch for signs of nausea, vomiting, bloating or irritability while feeding.