High allergy baby food
Baby Food Allergies: Identifying and Preventing Them
Written by Gina Shaw
In this Article
- Start Gradually to Identify Any Food Allergies
- Babies and Allergies: The Top 8 Allergenic Foods
- Food Allergy Symptoms to Watch for in Your Baby
- Severe Food Allergy Symptoms: When to Call 911
- Dealing With Mild Food Allergies in Baby
- The Family Food-Allergy Connection
- Protecting Baby Against Food Allergies: Easy Does It
Starting to feed a baby solid foods is an exciting milestone for parents. However, it comes with a lot of questions and concerns, especially about food allergies. What foods are most likely to cause allergies in babies? How do you avoid them?
Emerging research has shown that introducing multiple foods together is safe, and may help the immune system have a lower risk of developing food allergies, but more studies are needed. Check with your doctor for what’s best for your baby.
Start Gradually to Identify Any Food Allergies
It’s most important to introduce a baby to new foods gradually, one at a time, in case of food allergies. If not, a parent may have trouble tying an allergy to a specific new food. For example, if you give your baby three new foods over the course of a day and they develop an allergic reaction, you won’t know which of the foods provoked it.
The type of food or the order in which food is introduced is not much of a concern, as long as the foods you are offering are healthy and well-balanced for the baby. Each time you offer a new food, you should wait three to five days before adding another new item to the menu. Don’t eliminate the other foods your baby is eating during that time; you already know these are safe because the child has not had any food reactions up until now. Just don’t add anything else new.
Babies and Allergies: The Top 8 Allergenic Foods
With any new food, you’ll want to be on the lookout for any allergic reactions. There are more than 160 allergenic foods; certain foods may be more allergenic than others. The following eight foods and food groups are known to possibly cause problems with allergic reactions possibly up to 90% of the time.
There are more than 160 allergenic foods; certain foods may be more allergenic than others. The following eight foods and food groups are known to possibly cause problems with allergic reactions possibly up to 90% of the time.
- Cow's milk
- Eggs
- Peanuts
- Tree nuts (such as walnuts or almonds)
- Fish
- Shellfish
- Soy
- Wheat
New nutrition guidelines from the American Academy of Pediatrics say it's okay to introduce these allergy-causing foods when your baby is ready to eat solids. There is no evidence that waiting until the baby is older prevents food allergy. If you believe your baby has an allergic reaction to a food, such as diarrhea, rash, or vomiting, talk with your child's doctor about the best choices for the diet.
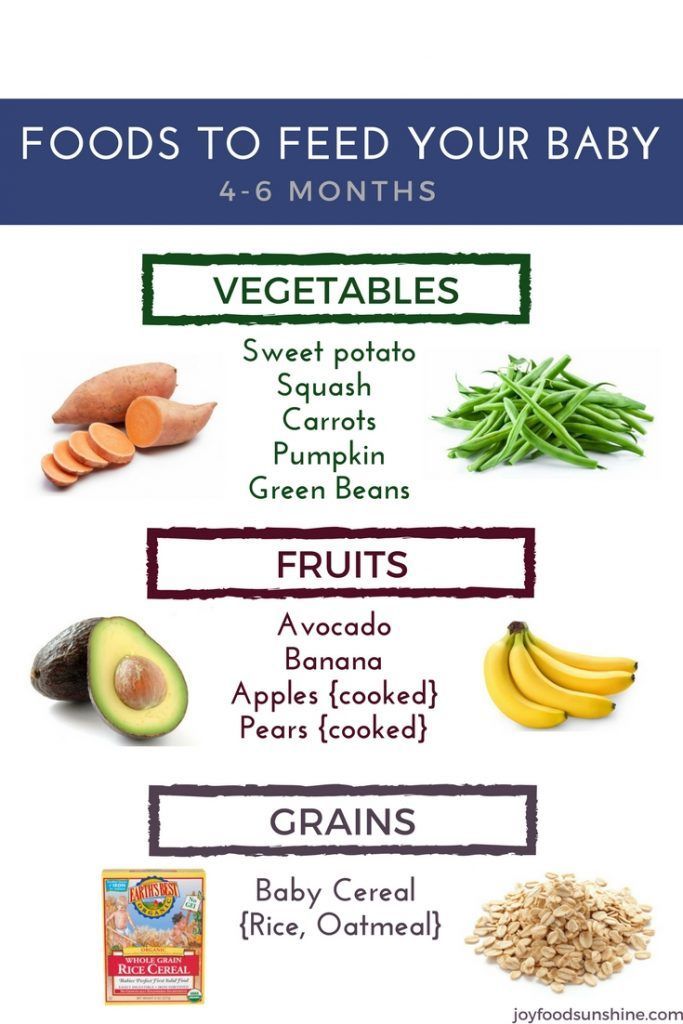
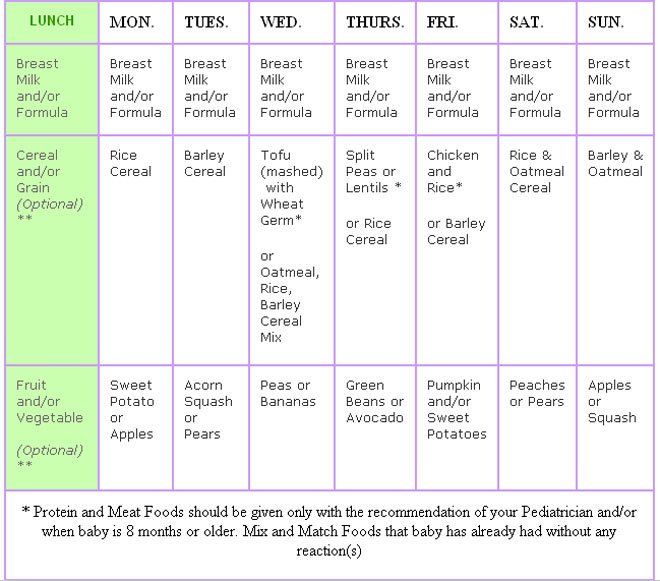
Within a few months of starting solid foods, your baby's daily diet should include a variety of foods, such as breast milk, formula, or both; meats; cereal; vegetables; fruits; eggs; and fish.
Food Allergy Symptoms to Watch for in Your Baby
Food allergy symptoms usually appear very soon after the food is eaten -- within a few minutes to a couple of hours. If you’re introducing a new food to your baby, keep an eye out for these symptoms:
If you’re introducing a new food to your baby, keep an eye out for these symptoms:
- Hives or welts
- Flushed skin or rash
- Face, tongue, or lip swelling
- Vomiting and/or diarrhea
- Coughing or wheezing
- Difficulty breathing
- Loss of consciousness
Severe Food Allergy Symptoms: When to Call 911
Severe allergic reactions can be fatal very quickly. If your baby is having trouble breathing/wheezing, has swelling on their face/lips, or develops severe vomiting or diarrhea after eating, immediately call 911. You can inform your pediatrician at a later time.
Dealing With Mild Food Allergies in Baby
If you see mild symptoms, such as hives or a rash, contact your pediatrician for further evaluation. The doctor might refer you to an allergist (allergy specialist doctor), who will ask more questions and do a physical exam. The allergies may order diagnostic tests such as:
- A skin test. This test involves placing liquid extracts of food allergens on your child's forearm or back, pricking the skin, and waiting to see if reddish raised spots form within 15 minutes.
 A positive test to a food only shows that your child might be sensitive to that food.
A positive test to a food only shows that your child might be sensitive to that food. - Blood tests to check the blood for IgE antibodies to specific foods
Remember, just because a baby’s initial allergic reaction to a new food may be mild, it may get worse upon following exposures. Talk to your pediatrician about any food allergy symptoms in your baby.
Some allergies go away with time. Egg and milk allergies often go away as children get older, but peanut, tree nut, and shellfish allergies tend to persist. That said, research shows that in the case of peanut allergies, peanut immunotherapy drops administered under the tongue are safe and effective as treatment for peanut allergy, even in children as young as 1. They were also found to help significantly desensitize the patients to peanuts.
The Family Food-Allergy Connection
If there is a family food allergies, your baby has an increased risk of also developing allergies, although it is not a certainty. If you have the allergies, the odds are 50-50 for them to have them as well.
If you have the allergies, the odds are 50-50 for them to have them as well.
It’s best to introduce the 8 allergens gradually, at one-to-two week intervals over time so that you can recognize if an allergy develops.
Protecting Baby Against Food Allergies: Easy Does It
In a reversal of earlier policy, the American Academy of Pediatrics is now recommending that potential allergens be introduced to your infant earlier rather than later. In doing so, the move may actually help prevent them from developing allergies to those foods.
Breastfeeding you baby for 4-6 months is the best way to prevent a milk allergy. Remember that breast milk or formula is higher in nutrition. When you begin to introduce whole milk, you should do so under a doctor’s supervision. Yogurt and soft cheeses are fine, because the proteins in these dairy products are broken down and less likely to cause tummy trouble.
The AAP now advises that, in the case of infants who are at high risk of allergies, peanuts should be introduced between 4-6 months. Infants at highest risk of developing peanut allergies are those with eczema or egg allergies or both. It was originally believed that introducing your baby to the foods when they are older might make any reactions more manageable.
Infants at highest risk of developing peanut allergies are those with eczema or egg allergies or both. It was originally believed that introducing your baby to the foods when they are older might make any reactions more manageable.
Other potential allergens such as tree nuts and fish should be introduced over a period of time as you introduce your baby to solid foods, between 6 and 9 months
You should wait until at least age 1 (some experts say age 2) to introduce honey, which can cause a potentially serious disease called infant botulism. Ask your pediatrician for guidance.
Baby Food Allergies: Identifying and Preventing Them
Written by Gina Shaw
In this Article
- Start Gradually to Identify Any Food Allergies
- Babies and Allergies: The Top 8 Allergenic Foods
- Food Allergy Symptoms to Watch for in Your Baby
- Severe Food Allergy Symptoms: When to Call 911
- Dealing With Mild Food Allergies in Baby
- The Family Food-Allergy Connection
- Protecting Baby Against Food Allergies: Easy Does It
Starting to feed a baby solid foods is an exciting milestone for parents. However, it comes with a lot of questions and concerns, especially about food allergies. What foods are most likely to cause allergies in babies? How do you avoid them?
However, it comes with a lot of questions and concerns, especially about food allergies. What foods are most likely to cause allergies in babies? How do you avoid them?
Emerging research has shown that introducing multiple foods together is safe, and may help the immune system have a lower risk of developing food allergies, but more studies are needed. Check with your doctor for what’s best for your baby.
Start Gradually to Identify Any Food Allergies
It’s most important to introduce a baby to new foods gradually, one at a time, in case of food allergies. If not, a parent may have trouble tying an allergy to a specific new food. For example, if you give your baby three new foods over the course of a day and they develop an allergic reaction, you won’t know which of the foods provoked it.
The type of food or the order in which food is introduced is not much of a concern, as long as the foods you are offering are healthy and well-balanced for the baby. Each time you offer a new food, you should wait three to five days before adding another new item to the menu. Don’t eliminate the other foods your baby is eating during that time; you already know these are safe because the child has not had any food reactions up until now. Just don’t add anything else new.
Don’t eliminate the other foods your baby is eating during that time; you already know these are safe because the child has not had any food reactions up until now. Just don’t add anything else new.
Babies and Allergies: The Top 8 Allergenic Foods
With any new food, you’ll want to be on the lookout for any allergic reactions. There are more than 160 allergenic foods; certain foods may be more allergenic than others. The following eight foods and food groups are known to possibly cause problems with allergic reactions possibly up to 90% of the time.
- Cow's milk
- Eggs
- Peanuts
- Tree nuts (such as walnuts or almonds)
- Fish
- Shellfish
- Soy
- Wheat
New nutrition guidelines from the American Academy of Pediatrics say it's okay to introduce these allergy-causing foods when your baby is ready to eat solids. There is no evidence that waiting until the baby is older prevents food allergy. If you believe your baby has an allergic reaction to a food, such as diarrhea, rash, or vomiting, talk with your child's doctor about the best choices for the diet.
Within a few months of starting solid foods, your baby's daily diet should include a variety of foods, such as breast milk, formula, or both; meats; cereal; vegetables; fruits; eggs; and fish.
Food Allergy Symptoms to Watch for in Your Baby
Food allergy symptoms usually appear very soon after the food is eaten -- within a few minutes to a couple of hours. If you’re introducing a new food to your baby, keep an eye out for these symptoms:
- Hives or welts
- Flushed skin or rash
- Face, tongue, or lip swelling
- Vomiting and/or diarrhea
- Coughing or wheezing
- Difficulty breathing
- Loss of consciousness
Severe Food Allergy Symptoms: When to Call 911
Severe allergic reactions can be fatal very quickly. If your baby is having trouble breathing/wheezing, has swelling on their face/lips, or develops severe vomiting or diarrhea after eating, immediately call 911. You can inform your pediatrician at a later time.
Dealing With Mild Food Allergies in Baby
If you see mild symptoms, such as hives or a rash, contact your pediatrician for further evaluation. The doctor might refer you to an allergist (allergy specialist doctor), who will ask more questions and do a physical exam. The allergies may order diagnostic tests such as:
- A skin test. This test involves placing liquid extracts of food allergens on your child's forearm or back, pricking the skin, and waiting to see if reddish raised spots form within 15 minutes. A positive test to a food only shows that your child might be sensitive to that food.
- Blood tests to check the blood for IgE antibodies to specific foods
Remember, just because a baby’s initial allergic reaction to a new food may be mild, it may get worse upon following exposures. Talk to your pediatrician about any food allergy symptoms in your baby.
Some allergies go away with time. Egg and milk allergies often go away as children get older, but peanut, tree nut, and shellfish allergies tend to persist.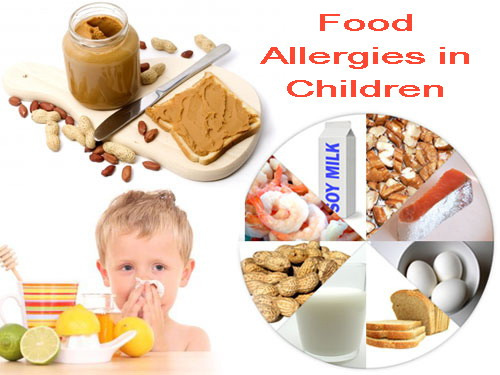 That said, research shows that in the case of peanut allergies, peanut immunotherapy drops administered under the tongue are safe and effective as treatment for peanut allergy, even in children as young as 1. They were also found to help significantly desensitize the patients to peanuts.
That said, research shows that in the case of peanut allergies, peanut immunotherapy drops administered under the tongue are safe and effective as treatment for peanut allergy, even in children as young as 1. They were also found to help significantly desensitize the patients to peanuts.
The Family Food-Allergy Connection
If there is a family food allergies, your baby has an increased risk of also developing allergies, although it is not a certainty. If you have the allergies, the odds are 50-50 for them to have them as well.
It’s best to introduce the 8 allergens gradually, at one-to-two week intervals over time so that you can recognize if an allergy develops.
Protecting Baby Against Food Allergies: Easy Does It
In a reversal of earlier policy, the American Academy of Pediatrics is now recommending that potential allergens be introduced to your infant earlier rather than later. In doing so, the move may actually help prevent them from developing allergies to those foods.
Breastfeeding you baby for 4-6 months is the best way to prevent a milk allergy. Remember that breast milk or formula is higher in nutrition. When you begin to introduce whole milk, you should do so under a doctor’s supervision. Yogurt and soft cheeses are fine, because the proteins in these dairy products are broken down and less likely to cause tummy trouble.
The AAP now advises that, in the case of infants who are at high risk of allergies, peanuts should be introduced between 4-6 months. Infants at highest risk of developing peanut allergies are those with eczema or egg allergies or both. It was originally believed that introducing your baby to the foods when they are older might make any reactions more manageable.
Other potential allergens such as tree nuts and fish should be introduced over a period of time as you introduce your baby to solid foods, between 6 and 9 months
You should wait until at least age 1 (some experts say age 2) to introduce honey, which can cause a potentially serious disease called infant botulism. Ask your pediatrician for guidance.
Ask your pediatrician for guidance.
Therapeutic nutrition of children of the first year of life suffering from food allergies | #06/02
In recent years, pathologies caused by food intolerance, especially allergy to protein components of food, have acquired a large proportion in the structure of morbidity in young children. Almost any product used in a child's diet can cause the development of allergic and pseudo-allergic reactions, the frequency of which depends on the nature of the product and its individual tolerance.
The program of dietary treatment developed by us for patients with food allergies provides for the earliest possible detection of causally significant allergens, the justification and timely appointment of an elimination hypoallergenic diet. Therapeutic diets are built taking into account the age and nutritional status of the child, the period of the disease, the results of allergological testing, the characteristics of the functional state of the gastrointestinal tract, and comorbidities [1].
For the diagnosis of food hypersensitivity in the acute period of the disease, the main, most accessible studies that allow the determination of IgE-specific antibodies remain immunological (RAST, MAST, ELISA) conducted "in vitro". Tests such as skin tests (prick tests) in young children, especially in the first year of life, can be extremely difficult to properly perform and evaluate; The double-blind, placebo-controlled test, the “gold standard” for diagnosing food allergies, is certainly accurate, but technically complex and can only be performed in scientific clinical centers [2, 3].
Our studies have shown that in children of the first year of life suffering from atopic dermatitis, hypersensitivity to proteins of cow's milk (85%), banana (81%), chicken egg (62%), gluten (53%) is most often detected. Less common is sensitization to buckwheat proteins (48%), potatoes (26%), soybeans (26%), and even less often to corn proteins (12%), various types of meat (0-3%). It should be noted that the majority of children (76%) have polyvalent sensitization, i.e. allergy to three or more food proteins [4].
It should be noted that the majority of children (76%) have polyvalent sensitization, i.e. allergy to three or more food proteins [4].
An important component of the complex treatment of children suffering from food allergies is diet therapy [5].
Children of the first year of life need to make individual elimination diets (dairy-free, agliadin, with the exception of certain complementary foods, etc.). Patients older than a year for the duration of the survey (7-10 days) are prescribed a non-specific hypoallergenic diet, then an individual hypoallergenic diet.
In the acute period of the disease, the diet should be as strict as possible and provide, on the one hand, the elimination of products with high sensitizing activity, the exclusion or restriction of causally significant and cross-reacting allergens, and on the other hand, an adequate replacement of the eliminated products with natural or specialized products or mixtures. In the remission phase, the diet is gradually expanded due to previously excluded foods and dishes. At the same time, regardless of the period of illness, the diet should provide the physiological needs of children for basic nutrients, energy, vitamins, mineral salts, and microelements [6].
At the same time, regardless of the period of illness, the diet should provide the physiological needs of children for basic nutrients, energy, vitamins, mineral salts, and microelements [6].
Breastfed children should be breastfed for as long as possible, prescribing a hypoallergenic diet to the mother, which is used throughout the lactation period and provides for the elimination of products with increased sensitizing activity, as well as products and dishes containing extractives and essential oils ( meat, chicken, fish and mushroom broths, hot spices, garlic, radish, radish, raw onion, etc.). Dairy products are allowed only in the form of fermented milk drinks, sour cream and mild cheese. The amount of cereals and pasta, wheat bread, sugar is reduced by 20-25%, salt - by 30%.
As noted above, cow's milk proteins are often the cause of the development of food allergies in children of the first year of life. This product contains about 15-20 antigens, of which the most allergenic are b-lactoglobulin, casein, a-lactoalbumin, bovine serum albumin. It is known that in the first year of life, allergy to cow's milk proteins occurs in 0.5-1.5% of children who are breastfed, and in 2-5% of children who are formula-fed. Among patients with atopic dermatitis 85-90% of children are allergic to cow's milk proteins [1, 3].
It is known that in the first year of life, allergy to cow's milk proteins occurs in 0.5-1.5% of children who are breastfed, and in 2-5% of children who are formula-fed. Among patients with atopic dermatitis 85-90% of children are allergic to cow's milk proteins [1, 3].
Currently, the consumer market has a wide range of therapeutic mixtures that can be used in the nutrition of children with milk allergies. The doctor has the opportunity to choose the necessary mixture in accordance with the age of the child, the period of the disease, the degree of sensitization to cow's milk proteins (Table 1).
Children with low sensitivity to cow's milk proteins, as a rule, tolerate fermented milk formulas well: adapted (Agusha 1, Nan fermented milk) and partially adapted (Agusha 2, Bifilin), and such products based on partially hydrolyzed milk protein: Humana GA1, Humana GA2 , Frisopep, Hipp GA (Table 2 and Table 3). In the diet of children older than 7 months, non-adapted fermented milk products (kefir, biokefir, Biolact, Narine, Acidolact, etc. ) can be used in the amount of one feeding.
) can be used in the amount of one feeding.
In the absence of a positive effect from the use of fermented milk products in the nutrition of children with an average sensitivity to cow's milk proteins, specialized mixtures based on soy protein isolate can be used: Humana SL, Alsoy, Nutrilak-soy, Nutri-soy, Soy-Samp, Frisovoy, as well as mixtures Suprolact and Supromilk produced in children's dairy kitchens (Table 4). These products are enriched with a vitamin-mineral complex and microelements in accordance with the physiological needs of children of the first year of life, do not contain milk protein, lactose, gluten. A positive effect should be expected no earlier than 3-4 weeks from the start of their use. The duration of the use of soy mixtures depends on the timing of achieving clinical and laboratory remission and can range from 3 to 9months or more.
However, it is known that 20-25% of children have allergic reactions to soy mixtures. The most common reason for their development is the rapid (within 1-2 days) introduction of these products, as well as the age of children (mainly the first six months of life) [7]. In such cases, the use of specialized hypoallergenic therapeutic mixtures prepared on the basis of milk protein hydrolysates with a high degree of hydrolysis is indicated: Alfare, Nutramigen, Pepti TSC, Peptidi-Tutteli (Table 3). When using these products in most patients (89-93%) it is possible to achieve positive dynamics on the part of skin, gastrointestinal and respiratory manifestations of food allergy after 2-3 weeks from the start of their use, and clinical remission is achieved after another 2-4 months.
In such cases, the use of specialized hypoallergenic therapeutic mixtures prepared on the basis of milk protein hydrolysates with a high degree of hydrolysis is indicated: Alfare, Nutramigen, Pepti TSC, Peptidi-Tutteli (Table 3). When using these products in most patients (89-93%) it is possible to achieve positive dynamics on the part of skin, gastrointestinal and respiratory manifestations of food allergy after 2-3 weeks from the start of their use, and clinical remission is achieved after another 2-4 months.
During the period of remission, hypoallergenic, dairy-free diets are expanded through the introduction of fermented milk products and mixtures based on partial protein hydrolysates. Children older than a year are trying to add diluted dry milk to cereals and cottage cheese. The expansion of the diet is carried out carefully and gradually under the control of the general condition of the child, clinical and immunological parameters with the obligatory registration of allergic reactions that have arisen in the food diary.
At present, due to the wide choice of therapeutic mixtures, the timing of the appointment of complementary foods for children with food allergies practically does not differ from those in healthy children (Table 5 and Table 6). At the same time, it is necessary to take into account the individual tolerance of products [5, 6, 8].
The first complementary food - vegetable puree - is prescribed at 4.5-5 months. It can include zucchini, squash, cauliflower, white and Brussels sprouts, light-colored pumpkin, potatoes and other green or white vegetables. For the preparation of puree, both natural (including frozen) vegetables and canned vegetables for baby food from the above vegetables can be used.
The second complementary food - dairy-free porridge - is included in the diet of children from 5 months. It can be buckwheat, corn, rice, oatmeal. Hypoallergenic oatmeal, buckwheat, and corn porridges from the Heinz company, which have been tested at the National Health Center of the Russian Academy of Medical Sciences, have proven themselves well. Preference should be given to dairy-free cereals for baby food of industrial production, which are prepared from environmentally friendly raw materials, enriched with vitamins, mineral salts (including iron) and do not require cooking. Porridges are cooked on water or with the addition of a specialized mixture (based on soy or hydrolyzate).
Preference should be given to dairy-free cereals for baby food of industrial production, which are prepared from environmentally friendly raw materials, enriched with vitamins, mineral salts (including iron) and do not require cooking. Porridges are cooked on water or with the addition of a specialized mixture (based on soy or hydrolyzate).
In order to correct the protein part of the diet, meat puree is introduced into the child's diet from 5.5-6 months. In case of intolerance to beef, which has antigenic affinity for cow's milk proteins, it is recommended to use lean pork, rabbit meat, turkey, as well as specialized children's canned meat from horsemeat "Humpbacked Horse", pork "Pork Puree", a combination of these products "Cheburashka", as well as other domestic and foreign analogues.
As a third complementary food (from 8-9months) you can introduce a second vegetable or vegetable-cereal dish (zucchini with corn grits, cauliflower with buckwheat) into the diet, thus achieving some restriction of dairy products.
From fruits, preference is given to apples of green and white color (Antonov, Simirenko, white filling). Taking into account individual tolerance, pears, white and red currants, yellow and red cherries, yellow plums are used. Boiling and baking fruits somewhat reduces their allergenicity.
Eggs, fish, cottage cheese are completely excluded from the diets of children with food allergies.
It should be noted that the timing of the appointment of an elimination hypoallergenic diet, as a rule, is individual. The effect of diet therapy depends not only on the severity of therapeutic nutrition, but also on the severity of atopy.
For literature inquiries, contact the editor
FOOD, CHILDREN, ALLERGIES | Science and life
The rapid development of civilization has brought us more than one misfortune. "Food allergy" - many, when they hear this diagnosis, say: still, because what a muck you have to feed your children. Nitrates, dyes, modified products. But we will talk about something else: the products are good, and the body responds to them with reddening of the skin and a rash. As a rule, an allergic reaction is caused by food that is unusual, say, for the inhabitants of the Central Russian Upland - sea fish and shrimps, oranges and chocolate, nuts and spices. Although traditional milk, wheat and honey can cause allergies. It is not yet possible to establish the exact causes of the growing "coma" of allergic reactions. But you can stop its growth through proper nutrition.
Nitrates, dyes, modified products. But we will talk about something else: the products are good, and the body responds to them with reddening of the skin and a rash. As a rule, an allergic reaction is caused by food that is unusual, say, for the inhabitants of the Central Russian Upland - sea fish and shrimps, oranges and chocolate, nuts and spices. Although traditional milk, wheat and honey can cause allergies. It is not yet possible to establish the exact causes of the growing "coma" of allergic reactions. But you can stop its growth through proper nutrition.
Science and life // Illustrations
In allergy, the formation of an antigen-antibody complex causes the release of biologically active substances (BAS) - allergy mediators.
When preparing hypoallergenic diets for lactating women, it is necessary to ensure their high biological and nutritional value, sufficient content of vitamins, minerals and trace elements.
The division given in the table is conditional: regional, national, family and other peculiarities of children's nutrition are of great importance.
Highly allergenic foods include bright red and orange fruits and berries. Give your child green and yellow apples as complementary foods.
Science and life // Illustrations
Cross-reactions of pollen allergens, food products and phytopreparations ›
View full size
Many people suffer from hypersensitivity to food, but it is not always an allergy. Food intolerance is often caused by diseases of the gastrointestinal tract, insufficient activity of food enzymes, psychogenic aversion to certain foods, and other reasons. None of these cases involved an immune mechanism.
In the case of a true food allergy, the immune system perceives certain proteins not as useful food components, but as something alien, harmful to the body and develops protective antibodies against them. Proteins usually cause an allergic reaction, but sometimes other substances contained in food products act as allergens. When an allergen first enters the body, sensitization occurs - the immune system remembers it as a "stranger". And with any subsequent use of the product, an allergic reaction develops.
And with any subsequent use of the product, an allergic reaction develops.
Manifestations of food allergies most often occur in early childhood and persist throughout life. Usually the skin reacts first: redness, itching, swelling appear. But there may also be abdominal pain, nausea, vomiting, intestinal upset (diarrhea, flatulence - increased gas formation, constipation). In addition, headache, irritability, nasal congestion, difficulty breathing up to an attack of suffocation and, as an extreme degree of severity, anaphylactic shock are not uncommon. It is important to know: an attack of a true allergy occurs even when the allergen enters the body in the smallest amount.
ONE IS POSSIBLE, THE OTHER IS NO
And now let's figure out the reason for this "injustice": why is it possible for one, and not for the other? We are all very different - not only our appearance is unique, but also biochemical processes, and how our body reacts to a new food component. And yet science establishes some patterns.
And yet science establishes some patterns.
In the twentieth century, the external manifestations of allergies were called diathesis. In Greek it means "inclination". Addiction here is an abnormal reaction of the organism. If earlier this situation was stated, now it can be quantified: when analyzing blood, a specific (immune) protein is found in it, and the severity of the allergy can be determined by its quantity.
Predisposition to food allergies is often inherited. A hereditary relationship has been established in 50-70% of cases of allergic manifestations. An allergy to food products can form in a baby even in the womb with malnutrition of the expectant mother, as well as during breastfeeding. This is facilitated by overeating foods that have a pronounced allergenicity (fish, seafood, eggs, nuts, citrus fruits, chocolate, etc.). Transmission of the allergen to the fetus can occur in utero through the amniotic fluid when swallowed by the fetus or through its skin (it is very permeable).
In the immature body of premature babies, food allergies develop more often. The early transfer of the child to artificial feeding is also critical. Food allergies can be caused by improper introduction of complementary foods, inconsistency of food ingredients with the weight and age of the child. Do not overfeed your baby and introduce foods that have highly allergenic properties into the diet. The risk of developing allergies is higher if the child has an inflammatory disease. It is necessary to pay attention to the inadmissibility of the early use of medicines, especially antibiotics (the instructions for use of most drugs indicate whether they can be taken during pregnancy and lactation). Here is the last rule, expectant mothers often observe, but they don’t remember that during pregnancy you shouldn’t lean on chocolate. Especially if the mother herself had, as they used to say, "New Year's diathesis" - a reaction to tangerines and sweets eaten in excess during the holidays. So even in the womb, the child's body is subjected to sensitization.
So even in the womb, the child's body is subjected to sensitization.
SOMETIMES GOOD AND DANGEROUS FOOD
What in ordinary products can become dangerous? Most often, proteins of animal and vegetable origin become allergens, less often polypeptides - fragments of proteins. Some low molecular weight substances, in themselves not dangerous, turn into allergens by attaching to a certain protein. With a normal diet during the day, a person receives about 120 potential allergens. Milk, fish, eggs, animal and poultry meat, nuts, legumes, grains, vegetables and fruits - all of these common foods contain substances that can cause allergies.
Food allergens can change their antigenic properties during heat treatment in the direction of both their weakening and strengthening. But more often pasteurization, sterilization, freezing, pickling or salting products have little effect on the severity of allergenic properties. If the expectant mother is allergic to eggs, then she needs to limit the use of buns, mayonnaise, and cakes.
ALLERGY PORTRAIT
In each childhood, food allergies have different clinical manifestations. When breastfeeding, if the mother follows the diet, food allergies rarely develop in a child under 6 months old. Its very first manifestation is atopic dermatitis. It is first expressed in itching and redness of the skin around the mouth or around the anus of the child, in persistent diaper rash with careful care of his skin. Not only the skin responds to the onset of the allergen. With its further introduction, the whole body reacts: regurgitation, vomiting, frequent loose stools with mucus, bloating like intestinal colic and further skin damage may appear. Children often refuse food.
Small bubbles pour out on the skin, which quickly merge, burst with the development of weeping and further formation of crusts. Localization of skin lesions can be different, but more often it all starts with the face, neck. As the child grows, allergies can become chronic. The area of skin lesions increases, areas of redness appear with fuzzy boundaries and rashes, accompanied by itching, peeling, scratching. The child becomes irritable, whiny, sleeps poorly, often refuses food. In the older age group in children with food allergies, skin manifestations can be urticaria, as well as angioedema angioedema.
The child becomes irritable, whiny, sleeps poorly, often refuses food. In the older age group in children with food allergies, skin manifestations can be urticaria, as well as angioedema angioedema.
Attentive parents quickly notice the connection between clinical manifestations and the introduction of a new product into the child's diet. But it happens that it is quite difficult to identify the allergen, then an allergist-immunologist comes to the aid of parents. He examines the child, noting the characteristic manifestations on the skin, mucous membranes, checks the safety of nasal breathing, examines the activity of all organs and systems. With its help, a family history is carefully collected and analyzed, the mother's diet is examined, the correctness and timeliness of the introduction of complementary foods and the composition of the mixtures used to supplement the child. In difficult cases, diagnostic tests are performed.
WHAT YOU CAN DO FOR YOUR CHILD
How do you determine what your child can and cannot eat? The most acceptable for children is an elimination test (from the Latin elimino - I take it out of the threshold, I delete it) test, when the suspected product is excluded from the diet for 1-2 weeks. Improvement in skin condition or disappearance of symptoms is a sign of his "guilt". Repeated use of a "suspect" food with a true food allergy will again evoke a past reaction. But it happens that in this way it is not possible to identify allergenic products, especially if there are several of them. Skin tests with allergens in young children are not performed, as children are afraid of such manipulations. And conducting provocative tests can cause serious complications. The doctor comes to the aid of laboratory diagnostics with a study of the patient's blood. Special diagnostic tests have been developed to detect the presence of specific antibodies in the patient's blood in allergic diseases. In practical medicine, enzyme-linked immunosorbent assay (ELISA), radioallergosorbent test (RAST), multiple allergosorbent test (MAST), immunochemiluminescent method, etc. are commonly used. The advantage of these tests lies in their informativeness and complete safety for the patient.
Improvement in skin condition or disappearance of symptoms is a sign of his "guilt". Repeated use of a "suspect" food with a true food allergy will again evoke a past reaction. But it happens that in this way it is not possible to identify allergenic products, especially if there are several of them. Skin tests with allergens in young children are not performed, as children are afraid of such manipulations. And conducting provocative tests can cause serious complications. The doctor comes to the aid of laboratory diagnostics with a study of the patient's blood. Special diagnostic tests have been developed to detect the presence of specific antibodies in the patient's blood in allergic diseases. In practical medicine, enzyme-linked immunosorbent assay (ELISA), radioallergosorbent test (RAST), multiple allergosorbent test (MAST), immunochemiluminescent method, etc. are commonly used. The advantage of these tests lies in their informativeness and complete safety for the patient.
DIET
After identifying the cause of the food allergy, a diet is drawn up that excludes the use of the “guilty” product. This is the first and main step in the treatment of food allergies. Back in 1998, it was shown that the frequency of food allergy in children in the first 5 years of life is more than 6 times higher than other forms of allergy, such as inhalation to plant pollen or household allergens. Moreover, up to 30% of children with a proven immune mechanism of food allergy become more tolerant (able to tolerate) food by the age of three, and by the age of 12 this figure reaches 53% if reasonable individual hypoallergenic ("hypo" - low) diets are followed. Here is evidence that even genetically determined allergic manifestations can be avoided by eliminating contact with allergens. In cases where a food allergy develops in relation to infrequently consumed foods, such as strawberries, chocolate, crabs, the only effective method of treatment is the complete elimination of a particular food product and any others in which this product is included, even in the smallest quantities. The situation is more complicated with allergies to basic foods.
This is the first and main step in the treatment of food allergies. Back in 1998, it was shown that the frequency of food allergy in children in the first 5 years of life is more than 6 times higher than other forms of allergy, such as inhalation to plant pollen or household allergens. Moreover, up to 30% of children with a proven immune mechanism of food allergy become more tolerant (able to tolerate) food by the age of three, and by the age of 12 this figure reaches 53% if reasonable individual hypoallergenic ("hypo" - low) diets are followed. Here is evidence that even genetically determined allergic manifestations can be avoided by eliminating contact with allergens. In cases where a food allergy develops in relation to infrequently consumed foods, such as strawberries, chocolate, crabs, the only effective method of treatment is the complete elimination of a particular food product and any others in which this product is included, even in the smallest quantities. The situation is more complicated with allergies to basic foods. They can be excluded only with proven allergies, with a mandatory replacement with another product of similar calorie content and with the same protein content, but not causing allergic reactions.
They can be excluded only with proven allergies, with a mandatory replacement with another product of similar calorie content and with the same protein content, but not causing allergic reactions.
MILK FORMULA
An infant receiving formula milk does not have a variety of nutrition, and if an allergy to milk, more often cow's milk, occurs, it is excluded from the diet. In such cases, the child is transferred to hypoallergenic mixtures. Food should be selected with great responsibility. For the growth and development of the child, nutrients (proteins, fats and carbohydrates), vitamins and microelements are needed, which must be supplied to the body in sufficient and properly balanced amounts. It is best to use baby food based on protein hydrolysates. Soy-based baby food (soy milk) is currently recommended with great caution due to the high likelihood of developing an allergy to soy protein and is prescribed if a child is found to be deficient in the enzyme for digesting lactose - milk sugar.
Formulated infant formula based on milk protein hydrolysates contains already digested (hydrolysed) proteins. Allergic reactions to them practically do not occur. The disadvantages of these mixtures are not very pleasant smell and color, leading to a change in color and consistency of baby feces to greenish and liquid, as well as their relatively high cost. But with food allergies, they become a saving substitute for intolerant milk. An example is the mixtures of the Dutch company Nutricia, a leader in the creation of mixtures for baby and medical nutrition. But there are products from other companies as well. The right choice will be made by the allergist.
Each jar indicates how to prepare baby food for a child depending on age, and a recipe for preparing a mixture is given, which is simple and consists in combining boiled water and powder in certain proportions.
Recent studies have shown that in many cases of food allergy, it is effective to replace cow's milk with goat's, which is due to the peculiarities of the physicochemical structure of its proteins. At present, products based on goat's milk have been developed for use not only as a substitute for women's milk, but also for cow's milk intolerance.
At present, products based on goat's milk have been developed for use not only as a substitute for women's milk, but also for cow's milk intolerance.
These goat-based breast milk substitutes are manufactured by Enfagroup Nutritional. In order to normalize the microflora and prevent constipation, these mixtures are additionally supplemented with prebiotics, compounds that restore the intestinal flora. Proteins have been added to the substitutes to improve the processes of brain maturation and the development of intelligence in an infant. In addition, these mixtures are enriched with an antioxidant complex containing selenium, beta-carotene, vitamin D3, taurine, inositol and choline, which enhances the child's body's resistance to various adverse environmental influences.
SUPPLEMENTING FOOD
After six months, not only with artificial, but also with breastfeeding, an insufficient amount of nutrients enters the body of a child with milk or milk mixtures for full growth and development. From this time on, it is recommended to introduce more solid food - complementary foods - into the diet. At first, it should be vegetable and fruit purees. At the same time, the child receives not only all the substances necessary for growth, but also new skills - he learns to chew and taste food. For children with a high likelihood of developing allergies, complementary foods are introduced carefully under the supervision of a pediatrician, one product per week and in small quantities. They start with foods that rarely cause allergies, such as fermented milk products, vegetable purees, cereals. When choosing a diet therapy, it must be remembered that the appointment of kefir for children with hypersensitivity to cow's milk proteins is unacceptable. Kefir has a high protein content (2.8 g per 100 ml), which increases the load on the urinary system of the child, and also causes microbleeding from the gastrointestinal tract. A new product is not introduced into the diet if the child is not completely healthy when teeth are cut, during vaccination.
From this time on, it is recommended to introduce more solid food - complementary foods - into the diet. At first, it should be vegetable and fruit purees. At the same time, the child receives not only all the substances necessary for growth, but also new skills - he learns to chew and taste food. For children with a high likelihood of developing allergies, complementary foods are introduced carefully under the supervision of a pediatrician, one product per week and in small quantities. They start with foods that rarely cause allergies, such as fermented milk products, vegetable purees, cereals. When choosing a diet therapy, it must be remembered that the appointment of kefir for children with hypersensitivity to cow's milk proteins is unacceptable. Kefir has a high protein content (2.8 g per 100 ml), which increases the load on the urinary system of the child, and also causes microbleeding from the gastrointestinal tract. A new product is not introduced into the diet if the child is not completely healthy when teeth are cut, during vaccination. To be able to track the appearance of an allergic reaction, it is recommended to introduce a new product in the morning feeding, and not in the evening, especially at night. When prescribing an elimination diet, it is also necessary to exclude products that have cross-reactions with a food allergen: cow's milk - beef; tree pollen - apples, cherries, apricots, nuts; pollen of cereals - cereals, flour and flour products; eggs - the meat of various birds; quinoa pollen - beets, spinach, etc. If no improvement is observed within 10 days of the elimination diet, the list of recommended foods should be reviewed. Finding the "guilty" product is easier if parents keep a food diary, where they enter all the foods the child consumes, indicate the time of admission, the child's well-being during the day, and the time of onset of symptoms. The symptoms must be described in detail. All this information must be reported to the allergist-immunologist for careful selection of an individual hypoallergenic diet.
To be able to track the appearance of an allergic reaction, it is recommended to introduce a new product in the morning feeding, and not in the evening, especially at night. When prescribing an elimination diet, it is also necessary to exclude products that have cross-reactions with a food allergen: cow's milk - beef; tree pollen - apples, cherries, apricots, nuts; pollen of cereals - cereals, flour and flour products; eggs - the meat of various birds; quinoa pollen - beets, spinach, etc. If no improvement is observed within 10 days of the elimination diet, the list of recommended foods should be reviewed. Finding the "guilty" product is easier if parents keep a food diary, where they enter all the foods the child consumes, indicate the time of admission, the child's well-being during the day, and the time of onset of symptoms. The symptoms must be described in detail. All this information must be reported to the allergist-immunologist for careful selection of an individual hypoallergenic diet.
If the symptoms of food allergies do not disappear, the doctor prescribes medications, taking into account the age of the child, the severity of the skin process and the speed of the regression of the disease. In the diary, you need to write down what remedies and how quickly they helped to eliminate the symptoms.
Dry air enhances skin manifestations, so in the apartment where the child lives, it is necessary to maintain sufficient air humidity.
As a child with a food allergy grows, he eats and drinks a lot more different foods than in the infant period. In addition, he can already eat on his own, and does not always do this in the presence of his parents. Therefore, it can be difficult to trace the relationship between the development of symptoms and the consumption of any particular food.
SEVERAL RULES OF CONDUCT FOR PARENTS
Just drawing up a daily menu, even with the help of a doctor, will not solve the problem of feeding children with food allergies, you must ensure that it is also respected.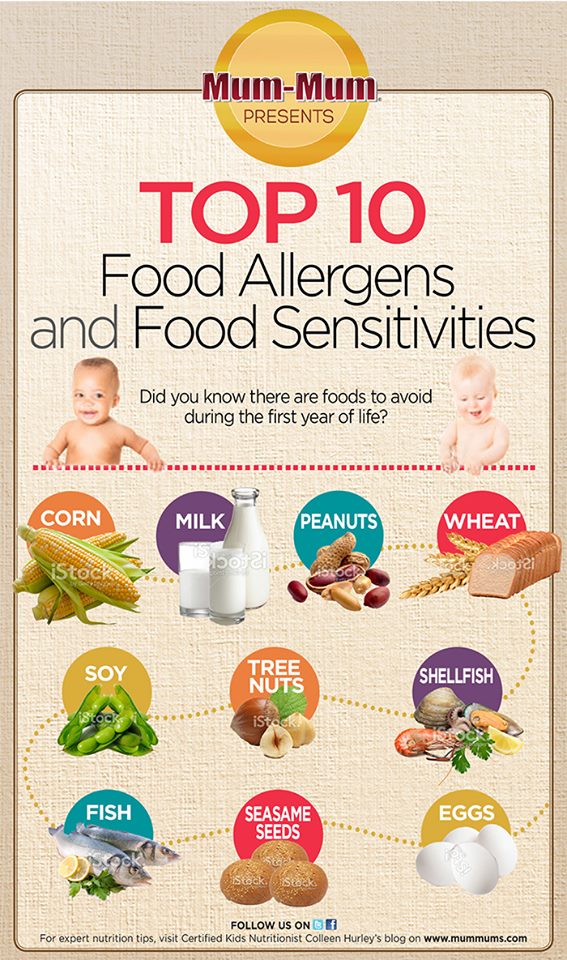
The child grows up, he understands better that after eating certain foods he becomes ill, he himself feels that something is wrong with him.
Try to explain to him in as much detail as possible what food is better not to eat. But you can’t foresee everything, there may be violations in the diet due to the use of an intolerable product in a hidden form (unknown filling, an integral part of the sauce, etc.). Be sure to have at home in a conspicuous place a list of products that are contraindicated for the child in order to exclude the possibility of feeding them out of forgetfulness or by an outsider if he is ignorant. It’s good to always have a supply of food in the house that the child tolerates well. When he goes to school or visits, you can give a well-tolerated product in a convenient package to replace the treat that is contraindicated for him. Living with food allergies is difficult for both the child and his parents, but we must try so that the disease does not interfere with the development of the child and his communication with peers, does not form in him a feeling of self-doubt, isolation. It is necessary to talk about this with children, and explain to close relatives and friends about food allergies. This will help to avoid excesses when someone “kind” thrusts a “forbidden fruit” into a child secretly from their parents and, bringing joy for a second, brings suffering for hours. Close contact with a knowledgeable allergist will help resolve the painful problem and eliminate the manifestations of food allergies.
It is necessary to talk about this with children, and explain to close relatives and friends about food allergies. This will help to avoid excesses when someone “kind” thrusts a “forbidden fruit” into a child secretly from their parents and, bringing joy for a second, brings suffering for hours. Close contact with a knowledgeable allergist will help resolve the painful problem and eliminate the manifestations of food allergies.
Older children are more likely than younger children to experience non-immune food intolerance reactions (pseudo-allergic reactions). They usually depend on the amount eaten. Food intolerance is also associated with dyes, preservatives, various thickeners, stabilizers, flavors and the like. When buying products, always look for labels that list these ingredients. True, sometimes you have to wear a special magnifying glass, since manufacturers print such information in unacceptably small print and in the most “unreadable” places. If the patient has a non-immune food intolerance, thermally processed foods can be recommended if the raw food caused painful manifestations. The golden rule to follow is: "If in doubt, don't eat!" Food intolerance, unlike a true allergy, can manifest itself inconsistently and even disappear after the exclusion of an intolerable product from the diet for a long time. Stress, infections, physical overwork can exacerbate an existing food intolerance. Even playing sports after eating can provoke a pseudo-allergic reaction.
The golden rule to follow is: "If in doubt, don't eat!" Food intolerance, unlike a true allergy, can manifest itself inconsistently and even disappear after the exclusion of an intolerable product from the diet for a long time. Stress, infections, physical overwork can exacerbate an existing food intolerance. Even playing sports after eating can provoke a pseudo-allergic reaction.
And one more rule: cook your own food, then there will be less fears about additives: homemade cutlet is better than sausage, porridge is better than potato chips, homemade bun is better than a pie from a stall.
In any case, the child must be shown to a doctor - an allergist-immunologist, who, after clarifying the nature of food intolerance, must issue a "Passport of a patient with an allergic disease." The passport contains the diagnosis, a complete list of intolerable foods and first aid measures in case of reactions to food, as well as the phone numbers of the doctor of the allergological office in which the sick child is observed.







:max_bytes(150000):strip_icc()/robin-feeding-babies-5a1d6f59beba33003700d88b.jpg)

