High allergy baby foods
Food Allergies (for Parents) - Nemours KidsHealth
What Are Food Allergies?
A food allergy happens when the body's immune system, which normally fights infections, sees the food as an invader. This leads to an allergic reaction.
Even if previous reactions have been mild, someone with a food allergy is always at risk for the next reaction being life-threatening. So anyone with a food allergy must avoid the problem food(s) entirely and always carry emergency injectable epinephrine.
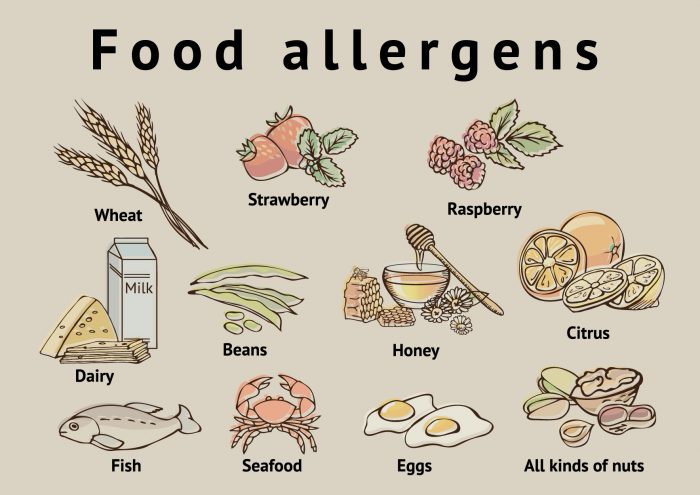
What Are the Most Common Food Allergens?
A child could be allergic to any food, but these common allergens cause 90% of all reactions in kids:
- milk
- eggs
- peanuts
- soy
- wheat
- tree nuts (such as walnuts and cashews)
- fish
- shellfish (such as shrimp)
- sesame
What Are the Signs & Symptoms of a Food Allergy?
An allergic reaction is an immune system response in which chemicals like histamine are released in the body. An allergic reaction can be mild or severe. A person can have a severe reaction to a food even if their previous reactions were mild. Symptoms of an allergic reaction can include:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- belly pain
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- red spots
- swelling
- a drop in blood pressure, causing lightheadedness or loss of consciousness (passing out)
Sometimes, an allergy can cause a severe reaction called anaphylaxis. Anaphylaxis might start with some of the same symptoms as a less severe reaction, but can quickly get worse. The person may have trouble breathing or pass out. More than one part of the body might be involved. If it isn't treated with injectable epinephrine, anaphylaxis can be life-threatening.
What Is a Food Intolerance?
People often confuse food allergies with food intolerance. The symptoms of food intolerance can include burping, indigestion, gas, loose stools, headaches, nervousness, or a feeling of being "flushed." But food intolerance:
The symptoms of food intolerance can include burping, indigestion, gas, loose stools, headaches, nervousness, or a feeling of being "flushed." But food intolerance:
- doesn't involve the immune system
- can happen because a person can't digest a substance, such as lactose
- can be unpleasant but is rarely dangerous
How Is a Food Allergy Diagnosed?
If your child might have a food allergy, the doctor will ask about:
- your child's symptoms
- the time it takes between eating a particular food and the start of symptoms
- whether any family members have allergies or conditions like eczema and asthma
The doctor might refer you to an
allergist(allergy specialist doctor), who will ask more questions and do a physical exam. The allergist probably will order tests to help make a diagnosis, such as:
- a skin test. This test involves placing liquid extracts of food allergens on your child's forearm or back, pricking the skin, and waiting to see if reddish raised spots (called wheals) form.
 A positive test to a food shows that your child might be sensitive to that food.
A positive test to a food shows that your child might be sensitive to that food. - blood tests to check the blood for IgE antibodies to specific foods
Your child may need to stop taking some medicines (such as over-the-counter antihistamines) 5 to 7 days before the skin test because they can affect the results. Check with the allergist's office if you are unsure about what medicines need to be stopped and for how long.
If the test results are unclear, the allergist may do a food challenge:
- During this test, a person slowly gets increasing amounts of the potential food allergen to eat while being watched for symptoms by the doctor. The test must be done in an allergist's office or hospital with access to immediate medical care and medicines because a life-threatening reaction could happen.
Food challenge tests are also done to see if people have outgrown an allergy.
How Are Food Allergies Treated?
A child who has a food allergy should always have two epinephrine auto-injectors nearby in case of a severe reaction. An epinephrine auto-injector is a prescription medicine that comes in a small, easy-to-carry container. It's easy to use. Your doctor will show you how. Always have two auto injectors nearby in case one doesn't work or your child needs a second dose.
An epinephrine auto-injector is a prescription medicine that comes in a small, easy-to-carry container. It's easy to use. Your doctor will show you how. Always have two auto injectors nearby in case one doesn't work or your child needs a second dose.
The doctor can also give you an allergy action plan, which helps you prepare for, recognize, and treat an allergic reaction. Share the plan with anyone else who needs to know, such as relatives, school officials, and coaches. Wherever your child is, caregivers should always know where the epinephrine is, have easy access to it, and know how to give the shot. Also consider having your child wearing a medical alert bracelet.
Time matters in an allergic reaction. If your child starts having serious allergic symptoms, like trouble breathing or throat tightness, use the epinephrine auto-injector right away. Also use it right away if symptoms involve two different parts of the body, like hives with vomiting. Then call 911 and have them take your child to the emergency room. Medical supervision is important because even if the worst seems to have passed, a second wave of serious symptoms can happen.
Medical supervision is important because even if the worst seems to have passed, a second wave of serious symptoms can happen.
If your child has a food allergy, carefully read food labels so you can avoid the allergen. Ingredients and manufacturing processes can change, so it's important to read labels every time, even for foods your child has had safely in the past. The most common allergens should be clearly labeled. But less common allergens can be hidden in ingredients like natural flavors or spices.
One thing that might not show up on a label is cross-contamination risk. Cross-contamination happens when a food you are not allergic to comes in contact with a food you are allergic to. This can happen if a manufacturer uses the same equipment to grind lots of different foods, for example. Some companies state this on their labels to alert customers to the risk of cross-contamination with messages like: "May contain peanuts," "Processed in a facility that also processes milk," or "Manufactured on equipment also used for eggs. " You'll want to avoid products that have these kinds of alerts.
" You'll want to avoid products that have these kinds of alerts.
But companies are not required to put cross-contamination alerts on a food label. So it's best to contact them to see if a product might been in contact with your child’s allergens. You may be able to get this information from a company website. If not, contact the company and ask.
When your child eats away from home, make sure anyone preparing food knows about the allergy and which foods to avoid. You may want to provide food that you know is safe for your child.
You can learn more about managing food allergies online at:
- Food Allergy Research and Education Network (FARE)
Reviewed by: Larissa Hirsch, MD
Date reviewed: January 2022
Common food allergens and kids
Share:
Sharing new foods with your baby is an exciting milestone. Unfortunately, amongst the fun of watching your child experience new tastes remain questions and fears about food allergies. Recommendations of when to introduce certain foods seem to change often, and for many parents, it can be confusing to know what is best for your child at each age.
Recommendations of when to introduce certain foods seem to change often, and for many parents, it can be confusing to know what is best for your child at each age.
April Clark, registered dietitian with the Food Allergy Center at Children’s Health℠, offers tips on when and how to introduce the top allergenic foods.
How to decrease the chance of food allergies in kids
The eight most common food allergens include: cow’s milk, eggs, peanuts, soy, tree nuts, finned fish, shellfish and wheat (gluten). According to the FDA, they account for approximately 90% of all food allergies in the United States.
Previously, the American Academy of Pediatrics (AAP) recommended that the introduction of certain highly allergenic foods be delayed in high-risk children. However, the AAP now recognizes that early introduction of peanuts decreases the chance of developing peanut allergies. Clark recommends following new guidelines to slowly introduce allergenic foods after the addition of solid foods, which often occurs during a baby’s first 4 to 6 months.
Tips on introducing new foods
Clark recommends that any of the foods noted below should be introduced one at a time, and parents should carefully observe their child’s reactions. Foods should first be given as single ingredients – not as part of a recipe like eggs in a baked good. They can also be given with complementary fruits and vegetables that have already been proven safe.
If there isn’t an allergic reaction once a food is introduced, continue including it at least three times a week in your child’s meals to ensure the best results. There isn’t a firm deadline to stop serving the foods. Instead, Clark notes that a healthy, well-balanced diet should normally contain variations of these common foods.
- Cow’s milk (dairy) may be one of the first allergies to be noticed, as many formulas are made with milk. Unlike the other foods listed, experts recommend waiting until after age 1 to introduce cow’s (whole) milk into a child’s diet.
 Instead, Clark notes babies eating solid foods should try yogurt or cheeses.
Instead, Clark notes babies eating solid foods should try yogurt or cheeses. - Eggs are an excellent source of protein for growing children. Clark recommends either scrambled eggs or pieces of hard-boiled eggs. Depending on the child, they may enjoy the squishy texture and prefer to feed themselves.
- Peanuts or peanut butter are another reliable source of protein. Do not give whole or even peanut pieces, as they can be a choking hazard; instead, peanut butter is a safer alternative, but the thick consistency can be difficult for most children to swallow. Clark recommends melting down the peanut butter with warm water or adding it to a fruit or veggie puree. If a child has severe eczema, and/or already has been diagnosed with egg allergy, they should be evaluated prior to peanut introduction.
- Soy is another allergy that is noticed early due to formulas with a soy base. Protein-packed tofu and edamame (soy beans) can be introduced when your child is ready.
 They are great options for self-feeding. Like cow’s milk, Clark says parents should not offer soy milk until after age 1.
They are great options for self-feeding. Like cow’s milk, Clark says parents should not offer soy milk until after age 1. - Finned fish and shellfish (shrimp, crab, clams, etc.) can be introduced as a puree around the 4 to 6-month mark, or in bite-size pieces once your child is ready. In addition to possible allergies, the AAP warns parents not to serve raw or undercooked items due to possible bacteria or viruses that can make your child seriously ill. Also, the AAP notes children shouldn’t eat more than 12 ounces of fish a week due to concerns about traces of mercury in fish or shellfish.
- Tree nuts (almonds, cashews or walnuts) follow the same guidelines as peanut and peanut butter above.
- Wheat (gluten) can be introduced as finger foods in teething biscuits, puffs and crackers that contain wheat.
Signs of a food allergy
Clark notes children with a first-degree relative (parent or sibling) with allergies are more likely to also have food allergies. Children (and their parents) who have a history of severe or recurring eczema and/or asthma are also at a higher risk to develop food allergies. If your child has any of these factors, you many want to consult your pediatrician for guidance on the best way to proceed.
Children (and their parents) who have a history of severe or recurring eczema and/or asthma are also at a higher risk to develop food allergies. If your child has any of these factors, you many want to consult your pediatrician for guidance on the best way to proceed.
Allergy symptoms and reactions can vary between children and may appear differently, depending on the age. Reactions can develop minutes after the food is ingested, or there may be a delayed reaction a few hours later. Clark cautions anyone can have a severe reaction at any time, and recommends following guidelines developed by Food Allergy Research & Education (FARE) to identify an allergic reaction. See FARE's list of symptoms here.
What to do if an allergic reaction occurs
Contact your pediatrician if your child has a mild allergic reaction and it is not an emergency. Call 911 immediately for severe and life-threatening reactions.
If you suspect your child has a food allergy, Clark recommends seeing a board-certified allergist to discuss your concerns. Bring any information about the food, the reaction and your family history to the appointment. The physician will likely take a detailed medical and diet history, and recommend appropriate testing that’s specific to your child’s symptoms and suspected food allergens. Your allergist will be able to manage the diagnosis and answer any questions. Specialists can also provide useful information like recipes and food allergy guidelines.
Bring any information about the food, the reaction and your family history to the appointment. The physician will likely take a detailed medical and diet history, and recommend appropriate testing that’s specific to your child’s symptoms and suspected food allergens. Your allergist will be able to manage the diagnosis and answer any questions. Specialists can also provide useful information like recipes and food allergy guidelines.
Download your guide to allergen-free lunches
Looking for tips to pack allergy-friendly school lunches? Download the Parents' Guide to Allergen-Free Lunches for kid-friendly recipes that are free of the top eight food allergens. Download now.
Learn more
Food allergy experts at Children’s Health can help with testing, questions and offer patient resources. Learn more about our program and services.
For more information, please see the following additional references:
- Food Allergy Research & Education (FARE)
- Instructions for feeding peanut butter and recipes
- Additional information about introducing peanut butter
- LEAP study in the U.
 K. (Learning Early About Peanuts)
K. (Learning Early About Peanuts) - Recommendations from the AAP for introducing food
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Therapeutic nutrition of children of the first year of life suffering from food allergies | #06/02
In recent years, pathologies caused by food intolerance, especially allergy to protein components of food, have acquired a large proportion in the structure of morbidity in young children. Almost any product used in a child's diet can cause the development of allergic and pseudo-allergic reactions, the frequency of which depends on the nature of the product and its individual tolerance.
The program of dietary treatment developed by us for patients with food allergies provides for the earliest possible detection of causally significant allergens, the justification and timely appointment of an elimination hypoallergenic diet. Therapeutic diets are built taking into account the age and nutritional status of the child, the period of the disease, the results of allergological testing, the characteristics of the functional state of the gastrointestinal tract, and comorbidities [1].
Therapeutic diets are built taking into account the age and nutritional status of the child, the period of the disease, the results of allergological testing, the characteristics of the functional state of the gastrointestinal tract, and comorbidities [1].
For the diagnosis of food hypersensitivity in the acute period of the disease, the main, most accessible studies that allow the determination of IgE-specific antibodies remain immunological (RAST, MAST, ELISA) conducted "in vitro". Tests such as skin tests (prick tests) in young children, especially in the first year of life, can be extremely difficult to properly perform and evaluate; The double-blind, placebo-controlled test, the “gold standard” for diagnosing food allergies, is certainly accurate, but technically complex and can only be performed in scientific clinical centers [2, 3].
Our studies have shown that in children of the first year of life suffering from atopic dermatitis, hypersensitivity to proteins of cow's milk (85%), banana (81%), chicken egg (62%), gluten (53%) is most often detected. Less common is sensitization to buckwheat proteins (48%), potatoes (26%), soybeans (26%), and even less often to corn proteins (12%), various types of meat (0-3%). It should be noted that the majority of children (76%) have polyvalent sensitization, i.e. allergy to three or more food proteins [4].
Less common is sensitization to buckwheat proteins (48%), potatoes (26%), soybeans (26%), and even less often to corn proteins (12%), various types of meat (0-3%). It should be noted that the majority of children (76%) have polyvalent sensitization, i.e. allergy to three or more food proteins [4].
An important component of the complex treatment of children suffering from food allergies is diet therapy [5].
Children of the first year of life need to make individual elimination diets (dairy-free, agliadin, with the exception of certain complementary foods, etc.). Patients older than a year for the duration of the survey (7-10 days) are prescribed a non-specific hypoallergenic diet, then an individual hypoallergenic diet.
In the acute period of the disease, the diet should be as strict as possible and provide, on the one hand, the elimination of products with high sensitizing activity, the exclusion or restriction of causally significant and cross-reacting allergens, and on the other hand, an adequate replacement of the eliminated products with natural or specialized products or mixtures.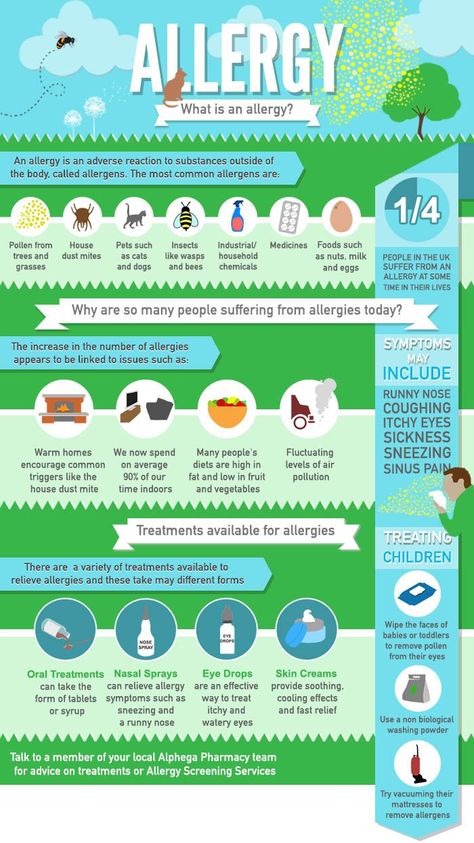 In the remission phase, the diet is gradually expanded due to previously excluded foods and dishes. At the same time, regardless of the period of illness, the diet should provide the physiological needs of children for basic nutrients, energy, vitamins, mineral salts, and microelements [6].
In the remission phase, the diet is gradually expanded due to previously excluded foods and dishes. At the same time, regardless of the period of illness, the diet should provide the physiological needs of children for basic nutrients, energy, vitamins, mineral salts, and microelements [6].
Breastfed children should be breastfed for as long as possible, prescribing a hypoallergenic diet to the mother, which is used throughout the lactation period and provides for the elimination of products with increased sensitizing activity, as well as products and dishes containing extractives and essential oils ( meat, chicken, fish and mushroom broths, hot spices, garlic, radish, radish, raw onion, etc.). Dairy products are allowed only in the form of fermented milk drinks, sour cream and mild cheese. The amount of cereals and pasta, wheat bread, sugar is reduced by 20-25%, salt - by 30%.
As noted above, cow's milk proteins are often the cause of the development of food allergies in children of the first year of life. This product contains about 15-20 antigens, of which the most allergenic are b-lactoglobulin, casein, a-lactoalbumin, bovine serum albumin. It is known that in the first year of life, allergy to cow's milk proteins occurs in 0.5-1.5% of children who are breastfed, and in 2-5% of children who are formula-fed. Among patients with atopic dermatitis 85-90% of children are allergic to cow's milk proteins [1, 3].
This product contains about 15-20 antigens, of which the most allergenic are b-lactoglobulin, casein, a-lactoalbumin, bovine serum albumin. It is known that in the first year of life, allergy to cow's milk proteins occurs in 0.5-1.5% of children who are breastfed, and in 2-5% of children who are formula-fed. Among patients with atopic dermatitis 85-90% of children are allergic to cow's milk proteins [1, 3].
Currently, the consumer market has a wide range of therapeutic mixtures that can be used in the nutrition of children with milk allergies. The doctor has the opportunity to choose the necessary mixture in accordance with the age of the child, the period of the disease, the degree of sensitization to cow's milk proteins (Table 1).
Children with low sensitivity to cow's milk proteins, as a rule, tolerate fermented milk formulas well: adapted (Agusha 1, Nan fermented milk) and partially adapted (Agusha 2, Bifilin), and such products based on partially hydrolyzed milk protein: Humana GA1, Humana GA2 , Frisopep, Hipp GA (Table 2 and Table 3). In the diet of children older than 7 months, non-adapted fermented milk products (kefir, biokefir, Biolact, Narine, Acidolact, etc.) can be used in the amount of one feeding.
In the diet of children older than 7 months, non-adapted fermented milk products (kefir, biokefir, Biolact, Narine, Acidolact, etc.) can be used in the amount of one feeding.
In the absence of a positive effect from the use of fermented milk products in the nutrition of children with an average sensitivity to cow's milk proteins, specialized mixtures based on soy protein isolate can be used: Humana SL, Alsoy, Nutrilak-soy, Nutri-soy, Soy-Samp, Frisovoy, as well as mixtures Suprolact and Supromilk produced in children's dairy kitchens (Table 4). These products are enriched with a vitamin-mineral complex and microelements in accordance with the physiological needs of children of the first year of life, do not contain milk protein, lactose, gluten. A positive effect should be expected no earlier than 3-4 weeks from the start of their use. The duration of the use of soy mixtures depends on the timing of achieving clinical and laboratory remission and can range from 3 to 9months or more.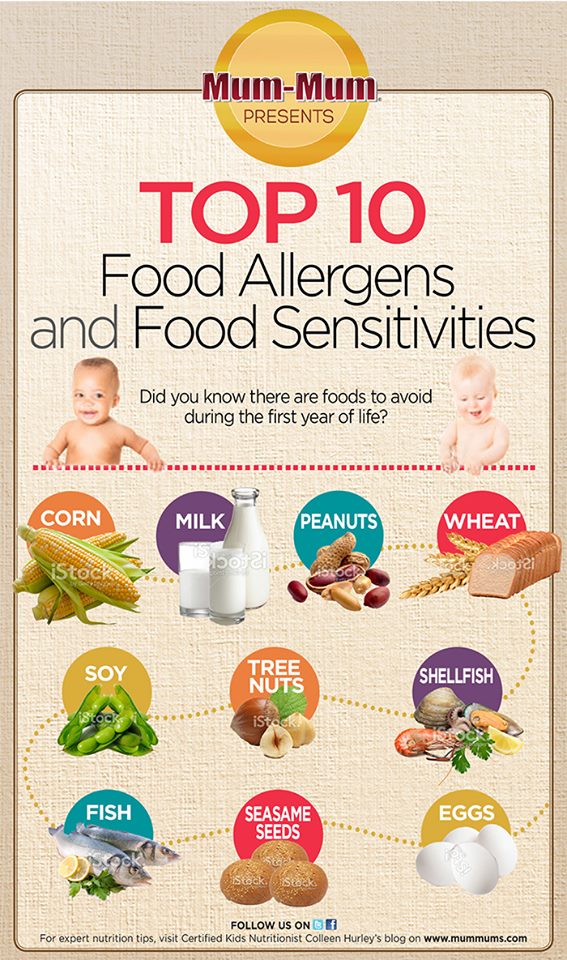
However, it is known that 20-25% of children have allergic reactions to soy mixtures. The most common reason for their development is the rapid (within 1-2 days) introduction of these products, as well as the age of children (mainly the first six months of life) [7]. In such cases, the use of specialized hypoallergenic therapeutic mixtures prepared on the basis of milk protein hydrolysates with a high degree of hydrolysis is indicated: Alfare, Nutramigen, Pepti TSC, Peptidi-Tutteli (Table 3). When using these products in most patients (89-93%) it is possible to achieve positive dynamics on the part of skin, gastrointestinal and respiratory manifestations of food allergy after 2-3 weeks from the start of their use, and clinical remission is achieved after another 2-4 months.
During the period of remission, hypoallergenic, dairy-free diets are expanded through the introduction of fermented milk products and mixtures based on partial protein hydrolysates. Children older than a year are trying to add diluted dry milk to cereals and cottage cheese.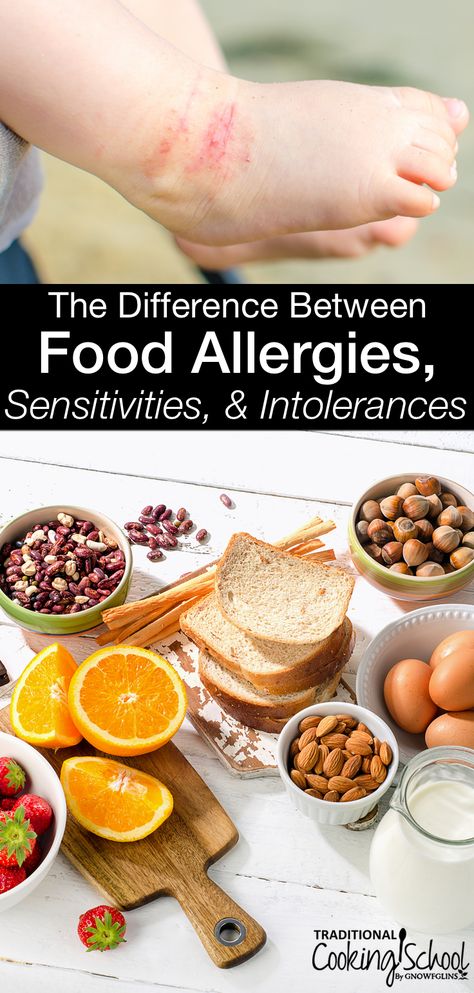 The expansion of the diet is carried out carefully and gradually under the control of the general condition of the child, clinical and immunological parameters with the obligatory registration of allergic reactions that have arisen in the food diary.
The expansion of the diet is carried out carefully and gradually under the control of the general condition of the child, clinical and immunological parameters with the obligatory registration of allergic reactions that have arisen in the food diary.
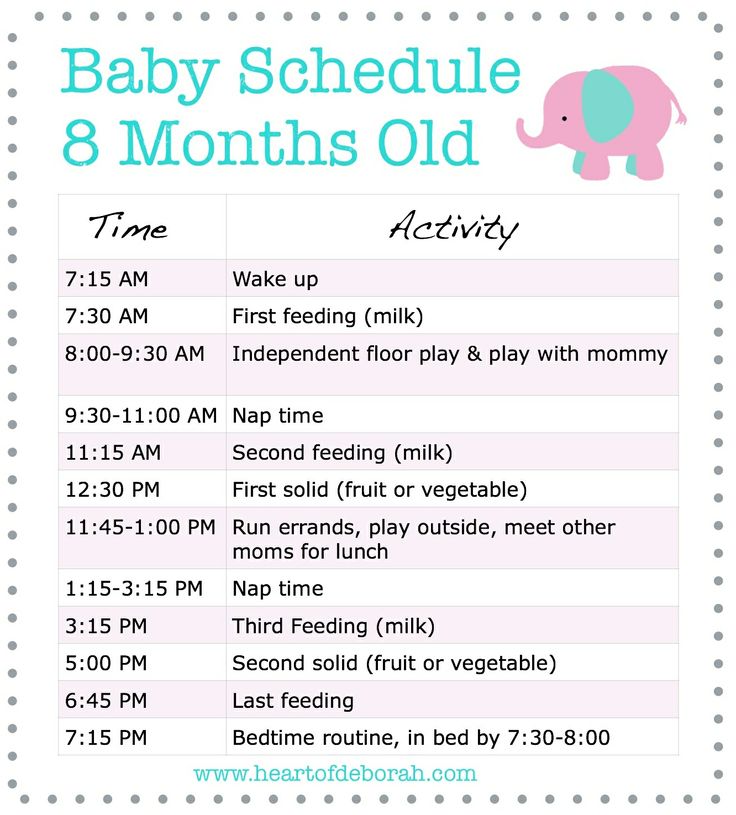
At present, due to the wide choice of therapeutic mixtures, the timing of the appointment of complementary foods for children with food allergies practically does not differ from those in healthy children (Table 5 and Table 6). At the same time, it is necessary to take into account the individual tolerance of products [5, 6, 8].
The first complementary food - vegetable puree - is prescribed at 4.5-5 months. It can include zucchini, squash, cauliflower, white and Brussels sprouts, light-colored pumpkin, potatoes and other green or white vegetables. For the preparation of puree, both natural (including frozen) vegetables and canned vegetables for baby food from the above vegetables can be used.
The second complementary food - dairy-free porridge - is included in the diet of children from 5 months. It can be buckwheat, corn, rice, oatmeal. Hypoallergenic oatmeal, buckwheat, and corn porridges from the Heinz company, which have been tested at the National Health Center of the Russian Academy of Medical Sciences, have proven themselves well. Preference should be given to dairy-free cereals for baby food of industrial production, which are prepared from environmentally friendly raw materials, enriched with vitamins, mineral salts (including iron) and do not require cooking. Porridges are cooked on water or with the addition of a specialized mixture (based on soy or hydrolyzate).
It can be buckwheat, corn, rice, oatmeal. Hypoallergenic oatmeal, buckwheat, and corn porridges from the Heinz company, which have been tested at the National Health Center of the Russian Academy of Medical Sciences, have proven themselves well. Preference should be given to dairy-free cereals for baby food of industrial production, which are prepared from environmentally friendly raw materials, enriched with vitamins, mineral salts (including iron) and do not require cooking. Porridges are cooked on water or with the addition of a specialized mixture (based on soy or hydrolyzate).
In order to correct the protein part of the diet, meat puree is introduced into the child's diet from 5.5-6 months. In case of intolerance to beef, which has antigenic affinity for cow's milk proteins, it is recommended to use lean pork, rabbit meat, turkey, as well as specialized children's canned meat from horsemeat "Humpbacked Horse", pork "Pork Puree", a combination of these products "Cheburashka", as well as other domestic and foreign analogues.
As a third complementary food (from 8-9months) you can introduce a second vegetable or vegetable-cereal dish (zucchini with corn grits, cauliflower with buckwheat) into the diet, thus achieving some restriction of dairy products.
From fruits, preference is given to apples of green and white color (Antonov, Simirenko, white filling). Taking into account individual tolerance, pears, white and red currants, yellow and red cherries, yellow plums are used. Boiling and baking fruits somewhat reduces their allergenicity.
Eggs, fish, cottage cheese are completely excluded from the diets of children with food allergies.
It should be noted that the timing of the appointment of an elimination hypoallergenic diet, as a rule, is individual. The effect of diet therapy depends not only on the severity of therapeutic nutrition, but also on the severity of atopy.
For literature inquiries, contact the editor
Allergy Child Diet – Allergy and Asthma Treatment at Allergomed
The birth of a child is a joy for every family and, of course, parents want their child to grow up healthy, especially those who themselves suffer from allergic diseases.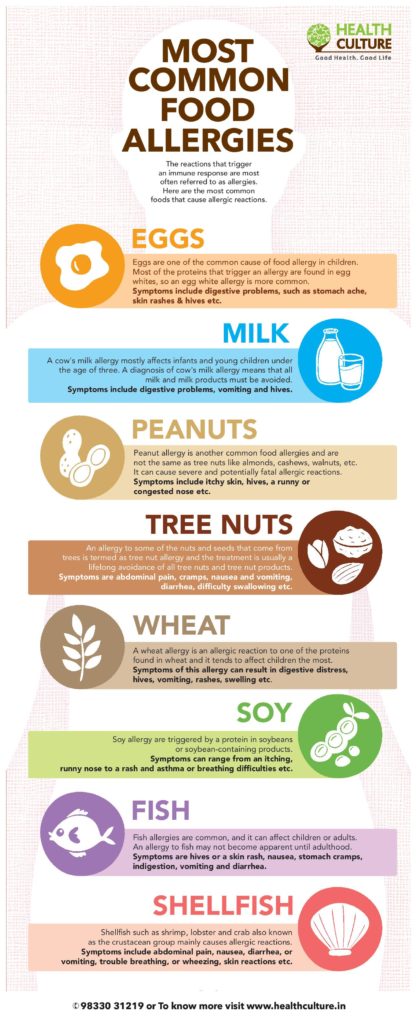
BREASTFEEDING
Breastfeeding is essential to keep your baby less sick. What gives breastfeeding? It not only improves bowel function, forms the correct bite, protects against infectious diseases, but also strengthens the emotional bond between mother and child.
When a mother is breastfeeding, she must follow certain nutritional rules: exclude milk, replacing it with sour dairy products, and limit the consumption of chicken, fish, citrus fruits, nuts, cocoa coffee, because these products most often cause allergies. If the baby gains enough weight while breastfeeding, then the first complementary foods can be introduced at 6 months.
With a decrease in mother's milk, it is better to use non-traditional methods of treatment: homeopathy and reflexology.
FORMULA FEEDING
Formula-fed infants must receive formula. If the baby did not have any manifestations of allergies, then hypoallergenic mixtures are used (Humana, Nan GA, Hip GA), in the presence of allergic manifestations, the so-called hydrolysates (Alfare, Nutramigen, Pregestemil). Allergic reactions are caused by proteins.
Allergic reactions are caused by proteins.
In special mixtures, they are broken down into smaller components that no longer cause allergies. Parents need to remember that the new mixture is introduced gradually, adding 20 ml to each feeding. Thus, the introduction of a new mixture will take 5-7 days.
In recent years, soy allergy has become more common. Since soy inclusions are included in many products, soy mixtures are not recommended as substitutes for women's milk during artificial feeding.
Recently, a lot of various canned baby food has appeared. When choosing canned food for your baby, pay attention that green apple juice is included as a natural preservative, and not ascorbic acid or lemon juice.
PREVENTION OF FOOD ALLERGIES
In children of the first year of life, cow's milk, chicken egg (protein), fish and cereals (wheat, corn, barley, less often rice and buckwheat) cause allergies more often. For the prevention of food allergies in children under 1 year of age, cow's milk is excluded, up to 1. 5 years - chicken eggs, fish and seafood, up to 3 years of age - nuts.
5 years - chicken eggs, fish and seafood, up to 3 years of age - nuts.
It should be noted that children do not have “accumulation allergies”, after using the “guilty product”, allergy manifestations develop within a few minutes up to 4-5 hours.
FOOD FOR OLDER CHILDREN
Older children also need to follow certain nutritional guidelines.
All food products can be conditionally divided into three groups according to allergenicity: high, medium and low degree
- First - (high degree of allergenicity): eggs, fish, seafood, caviar, wheat, rye, carrots, tomatoes, celery , bell pepper, wild strawberry, strawberry, raspberry, citrus, kiwi, pineapple, mango, coffee, cocoa, chocolate, mushrooms, nuts, honey, pomegranate, persimmon, melon;
- Second - (moderate allergenicity): whole milk, butter, beef, chicken meat, buckwheat, oatmeal, potatoes, beets, peas, soybeans, apricots, peaches, cranberries, bananas, dark red cherries, rose hips, blueberries, lingonberries, black currants;
- Third - (low degree of allergenicity): sour - dairy products, horse meat, rabbit meat, lean pork, lean lamb, pearl barley, millet, refined vegetable oil, green varieties of apples and pears, white and red currants, yellow and white cherries , yellow varieties of plums, gooseberries, zucchini, squash, cucumbers, cabbage, corn, parsley, dill;
Despite the conditional division of products into degrees of allergenicity, it is recommended to start expanding the child's diet with products of the third group, gradually adding products from the second group and lastly from the first. Parents should be careful and exclude exactly those products that caused an allergic reaction. It must be remembered that the diet can not permanent. With age, the child's diet should be expanded.
Parents should be careful and exclude exactly those products that caused an allergic reaction. It must be remembered that the diet can not permanent. With age, the child's diet should be expanded.
It must be emphasized that products such as chocolate, fish, citrus fruits, strawberries, egg white, tomatoes, when used, can cause the formation of active substances that cause allergic reactions. The composition of a number of products, such as soy, spinach, Gouda cheese, Cheddar, canned food, tomatoes, corned beef, sauerkraut, tuna, mackerel, includes histamine - the main "culprit" of allergic reactions.
Some foods should be completely excluded from the diet of a child with an allergy, regardless of age: chewing sweets and gums, sauces, fruit juices, soft drinks, instant soups, confectionery, yogurt, jams, ice cream if they contain industrial dye - tartrazine (E 102).
Parents often try to adjust the child's diet on their own and their views on this problem are completely opposite.
Some of the parents believe that the child should be on the strictest diet, leaving the child literally "on water and cabbage." At the same time, they do not take into account the fact that a child is a growing organism, therefore he needs “building materials” for normal growth and development, as well as the fact that with age the list of “forbidden foods” decreases. So, for example, milk allergy is most typical for children under 1.5 years old. If at an older age the child has any health problems when drinking milk and dairy products, this is most likely a gastroenterological disease and further dietary correction should be discussed with a gastroenterologist.
Some parents, on the contrary, allow the child to eat literally everything, citing pity for the child. Of course, if the doctor recommends excluding any products from the diet, they should not be on the general table so as not to cause the child to feel “inferiority”, but strict adherence to the diet should be mandatory at a certain stage of treatment.