How long does a food allergy rash last in babies
Does My Baby Have a Food Allergy Rash? — Prevent Food Allergies
Managing Food Allergies
Written By Jannie Huang
Do you think your baby’s rash may be caused by a food allergy? Let’s look at how to identify and treat a food allergy rash.
What is a Food Allergy Rash?
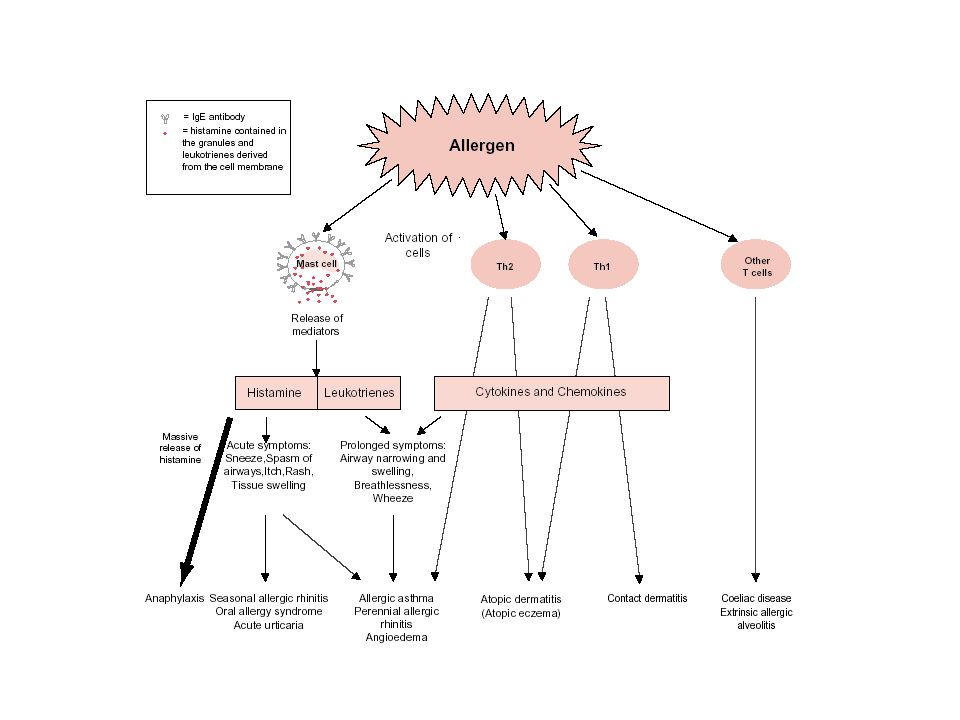
A food allergy rash is a rash that is caused by an overreaction of our immune systems to a particular food. Our immune systems are there to protect us from bacteria, viruses, and other invasions that can cause sickness. As is the case with other types of allergies, a food allergy occurs when the body reacts to an otherwise harmless item, wreaking havoc in our systems. With food allergies, the IgE antibodies overreact to a particular food(s), and a rash is often the first symptom to form.
How do IgE Antibodies Cause a Rash?
IgE antibodies detect the food and release histamine into the bloodstream to offer protection from the otherwise harmless food. In the process, blood vessels widen and release fluid which causes inflammation under the skin. A raised rash is the result, leaving the baby uncomfortable and the parents wondering what caused it and where to go from here.
Identifying a Food Allergy Rash
One of the most common signs your baby may have a food allergy is a rash that appears shortly after eating the offending food. It is often the first symptom to appear, the most common symptom of a food allergy, and can appear anywhere on the skin.
A food allergy often presents itself in the form of hives. Food allergy rashes often are concentrated in a couple areas on the body but can spread to other areas, especially in the case of a more severe food allergy. The individual bumps are often small in size, but they cluster together to form larger areas that may look like one larger rash.
In some cases, a food allergy can cause the skin to become red and inflamed without actually causing an actual raised rash. Food allergies can also cause eczema to become worse. Though worsening eczema is not a rash, it is important to watch this type of symptom closely since it is often associated with food allergies.
Food allergies can also cause eczema to become worse. Though worsening eczema is not a rash, it is important to watch this type of symptom closely since it is often associated with food allergies.
Though a rash may be the only symptom, one of the best ways to identify food allergy rashes is to pay attention to other signs that might accompany them. These signs will almost always occur within a few hours of eating the food. If you notice any of the following symptoms, along with a rash, contact your doctor to help determine if a food allergy might be the cause.
Mild Food Allergy Symptoms
Nausea and vomiting
Swelling
Sneezing
Congestion
Stomach pain
Itchy, watery eyes
Coughing
Worsening eczema
Swelling of the tongue
Tightness of the throat
Coughing
Wheezing
Difficulty breathing
Shortness of breath
Paleness of skin
Fainting
Rapid heartbeat
Loss of consciousness
Anaphylaxis
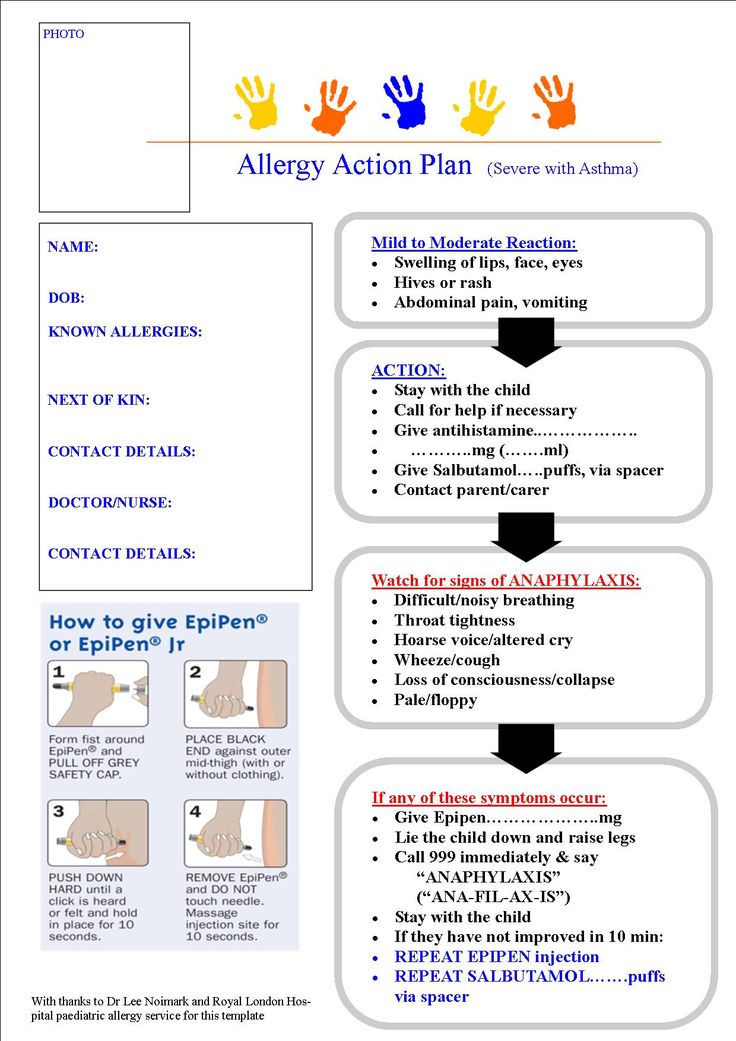
Anaphylactic reactions are rare in babies under the age of one, but it is good to be aware of the symptoms. Anaphylaxis is a swift, intense allergic reaction that is life-threatening and requires immediate medical attention. If you notice any of the following symptoms in your child, seek medical help right away:
Anaphylaxis is a swift, intense allergic reaction that is life-threatening and requires immediate medical attention. If you notice any of the following symptoms in your child, seek medical help right away:
Difficulty breathing
Shortness of breath
Swelling of the tongue
Widespread hives, covering a large part of the body
Wheezing
Pale appearance
Fainting
Rapid heartbeat
Persistent coughing
How to Treat a Food Allergy Rash
A food allergy rash actually doesn’t last very long, oftentimes clearing up in less than 48 hours. It is important to keep track of what your baby ate prior to the rash forming so that you can revisit your list should another rash appear later. You may also want to start a food journal and continue to keep track of what your child eats in the coming weeks and months. This can help you determine if there are other allergies.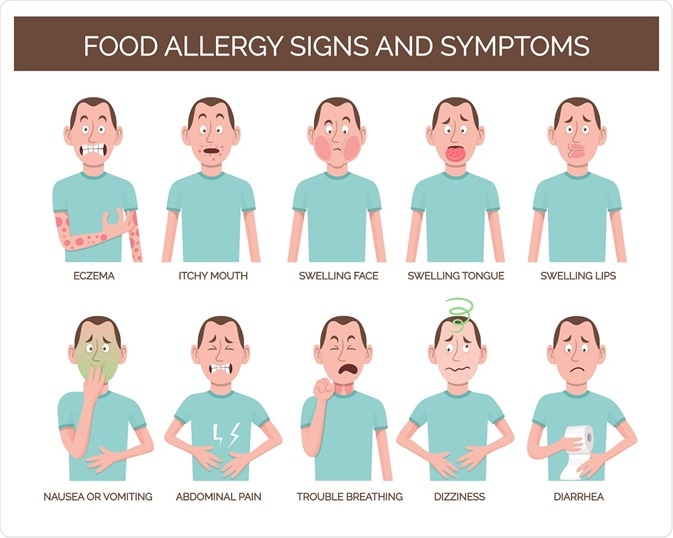
Even though rashes often go away on their own, they can be itchy and uncomfortable. Thankfully, there are some things that can provide relief.
Treating a Mild Food Allergy Rash
If your baby has a small rash that is confined to one area of his body and you suspect it was caused by food, you are most likely dealing with a mild food allergy. One of the best ways to treat a rash is with an antihistamine. Antihistamines block the histamine response, which helps clear up the rash. Be sure to ask your doctor about types and dosage before administering antihistamines to your baby.
You can also apply hydrocortisone cream to the area which will help relieve the itchiness. Hydrocortisone cream will not cause the rash to go away but can provide some relief.
Continue to monitor your baby in case the mild reaction turns severe.
Treating a Severe Food Allergy Rash
If your baby develops a widespread rash all over his body shortly after eating, you should call your doctor immediately. He could be experiencing an allergic reaction that can become life threatening if not treated right away. Continue to monitor your baby as you make your way to your doctor so you can inform the staff of other symptoms.
He could be experiencing an allergic reaction that can become life threatening if not treated right away. Continue to monitor your baby as you make your way to your doctor so you can inform the staff of other symptoms.
More About Food Allergies
Food allergies can develop at any time, though it is more rare to develop a food allergy late in life. Usually, they are detected early in childhood, when the child reacts to a certain food. As noted previously, often the first sign of a food allergy is a rash. If you suspect your child has developed a rash as a result of a food allergy, you may want to learn more about allergies and how to proceed safely.
Learn more from the Mayo Clinic on food allergic reactions:
YouTube Video: Mayo Clinic Minute: What happens to your body when you're allergic to food?
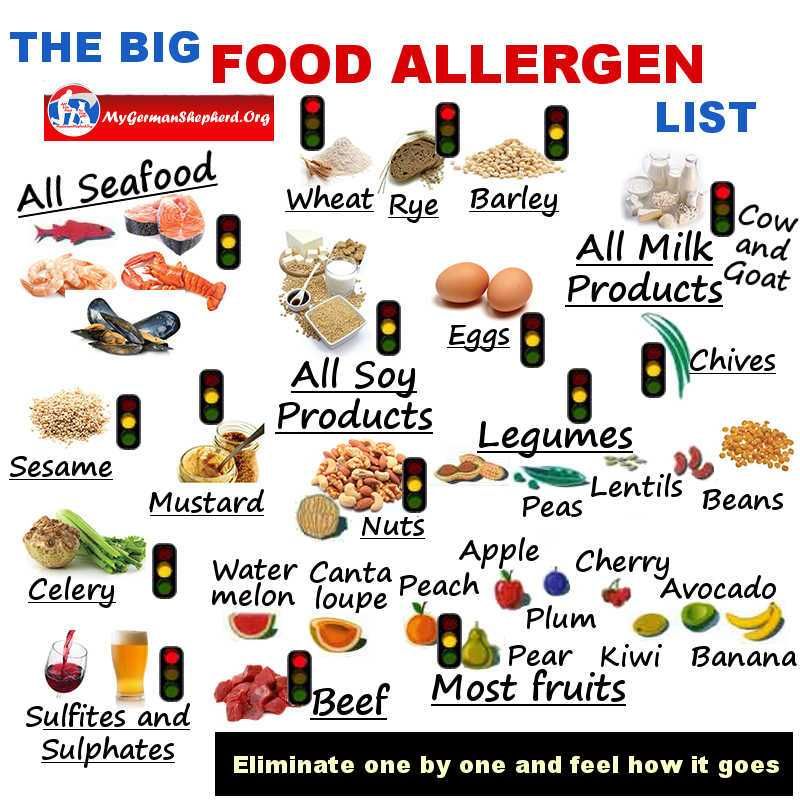
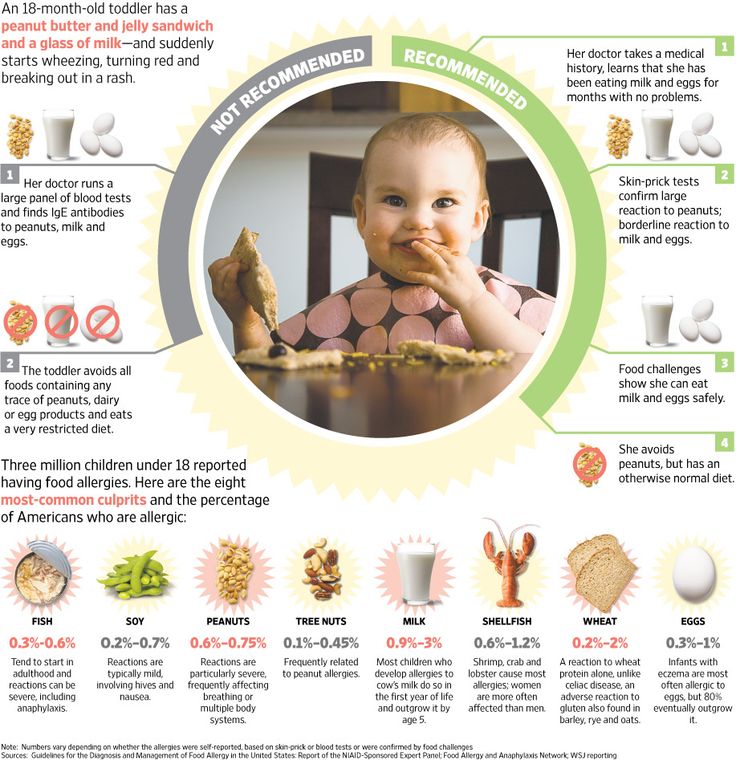
Allergies in Children vs in Adults
Both adults and children alike develop food allergies, though what they become allergic to often varies. Children are more likely to be allergic to cow’s milk, eggs, and peanuts, or tree nuts whereas the most common food allergens for adults is shellfish and finned fish.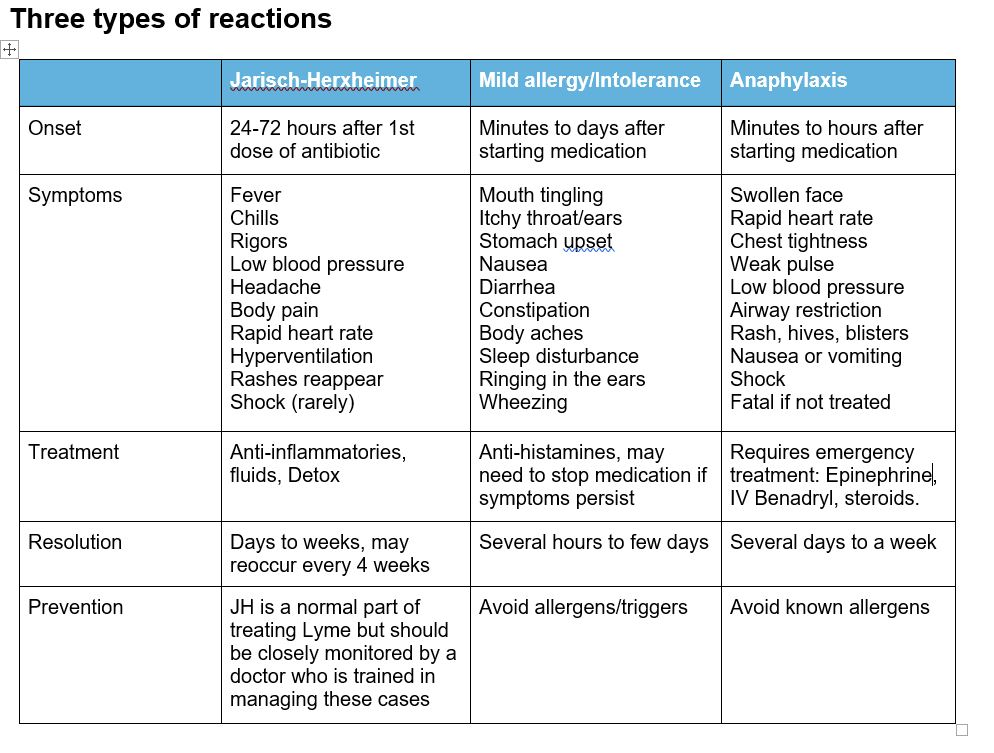 In either case, both adults and children are likely to develop a rash after eating an offending food.
In either case, both adults and children are likely to develop a rash after eating an offending food.
Peanut and tree nut allergies are more likely to cause serious reactions than the other allergies, but any allergy can become severe at any time.
Getting Tested for Food Allergies
The only way to determine if your child’s rash was caused by a food allergy is to make an appointment to undergo food allergy testing. Once you have talked to your doctor about possible causes for the rash and applied any acute medical care needed, you should make an appointment for your child to get tested for food allergies. There are a few ways this is done. You and your doctor will work together to determine the best testing for your child.
Oral Food Challenge
In this method of diagnosing a food allergy, your doctor will give your baby a small amount of the suspected food and watch him closely to see if he develops an allergic reaction. An oral food challenge is a safe, accurate method when used under the direct supervision of a doctor. This is the most accurate way to determine a true food allergy.
An oral food challenge is a safe, accurate method when used under the direct supervision of a doctor. This is the most accurate way to determine a true food allergy.
Skin Prick Test
During this test, your doctor will prick your child’s skin with the suspected allergen and watch to see if a rash develops around the area. Since a food allergy rash is often the first symptom of an allergy, this is a fairly accurate way to see if your child is allergic to a specific food.
Blood Test
When your child undergoes blood testing for allergies, your doctor will check for IgE antibodies in the blood. The presence of these antibodies will indicate an allergy to a specific food or variety of foods.
The Bottom Line
If your child develops a rash shortly after eating, you should take note of the suspected food and stop feeding to your child right away. You may want to start a food journal to monitor your child’s food intake and any potential rashes or other symptoms that might arise.
If the rash is mild and limited to one small part of the child’s body, you can treat it with antihistamines or with topical hydrocortisone cream after first discussing treatment options and dosages with your child’s doctor. If your child develops a major rash that is widespread, you should contact your doctor immediately and watch for signs of anaphylaxis.
Talking to your doctor about the rash is important both in the treatment of the rash and in discovering the cause. If you and your doctor think a food may be the cause of your child’s rash, you should continue to keep the suspected food away from your child and schedule allergy testing. There are a few different tests your doctor may use to determine if your child has a food allergy
Discovering your child has a food allergy can be a scary time for parents, but there are many ways to manage food allergies in children. Learning more about food allergies, their causes, signs, and symptoms, and management are all ways parents can be prepared.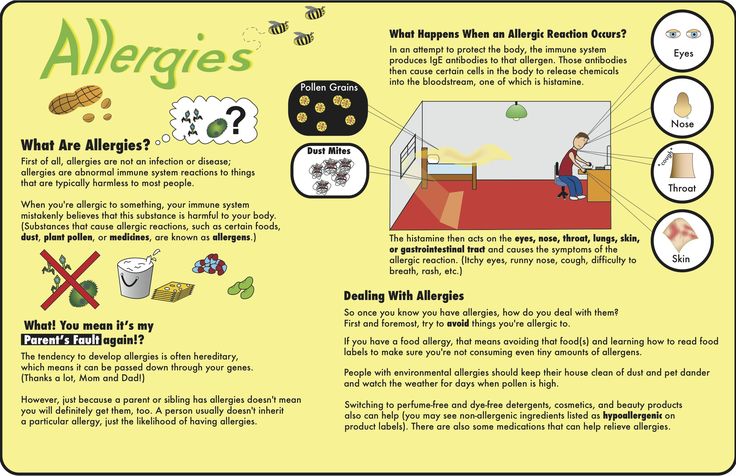
--------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.
Jannie Huang
Food Allergy
Is this your child's symptom?
- Allergic reactions to foods
- The most common symptom is hives
- Questions about food allergies
- Oral Allergy Syndrome is also covered. The main symptom is mouth itching and swelling. The main triggers are raw fruits and veggies.
Symptoms of Food Allergies
- Hives all over and swelling of the face are the most common symptoms.
 Hives are raised pink bumps with pale centers (welts). They look like bug bites.
Hives are raised pink bumps with pale centers (welts). They look like bug bites. - Mouth itching and swelling
- Runny nose and coughing
- Vomiting and diarrhea
- Life-threatening allergic reactions also must have trouble breathing and/or swallowing. The medical name for this is anaphylaxis. Most of these reactions have a sudden onset within 10 to 20 minutes. All occur within 2 hours of eating a certain food. People who have had this carry an emergency kit like an Epi-Pen.
Causes of Food Allergies
- 8 foods cause 90% of food allergies
- In the first year of life: cow's milk, soy milk and egg
- Older children: peanuts, tree nuts, fish, shellfish and wheat
- Shellfish include shrimp, crab, lobster, clams, oysters and scallops
- Tree nuts include all the nuts (such as almonds and cashews) except peanuts.
- Of children with a proven food allergy, 40% have severe reactions. The other 60% have mild reactions.
- Peanuts and tree nuts are the most common triggers for severe reactions.
Cross Reactions with Other Foods
Children with allergies listed below can react to other foods:
- Cow's milk allergy: 90% also react with goat's milk and 40% with soy milk
- Egg: 5% react with chicken
- Peanut: 5% react with other legumes (like peas or beans). About 30% also react to tree nuts.
- Tree nut: 40% react with other tree nuts
- Fish: 50% react with other fish. Only 10% also react to shellfish.
- Shellfish: 70% react with other shellfish
- Melon: 90% react with banana and avocado
How Long do Food Allergies Last?
- Cow's milk: 80% outgrown by age 16
- Soy milk: 80% by age 16
- Egg: 70% by age 16
- Peanut: 20% by age 16
- Tree nut: 10% by age 16
Allergic Disease - Can You Prevent with Diet?
- Most allergic diseases (food allergies, eczema and asthma) cannot be prevented.
- Helpful: Feeding only breastmilk for 6 months or longer
- Not helpful: Avoiding high-risk foods for pregnant or breastfeeding women
- Not helpful: Soy formulas instead of cow's milk formula
- Not helpful: A delay in starting baby foods past 6 months
- Not helpful: A delay in starting high-risk foods like peanut butter or eggs
- Source: AAP
Oral Allergy Syndrome (OAS)
- A minor reaction to some raw fruits and veggies
- Causes itching and swelling only to the lips and tongue
- Also called Pollen-Food Syndrome
Symptoms of OAS
- Rapid onset of itching (or tingling) and swelling of the mouth.
- This can involve the lips, tongue, throat, and roof of the mouth.
- The uvula (tag of tissue hanging down in back) can become very swollen.
- These symptoms follow eating a high-risk raw fruit or veggie.
- OAS can start by age 5.
- Serious symptoms or very bad reactions rarely happen.
Causes of OAS
- A contact allergy. It only involves the parts of the mouth that touch the raw food.
- Trigger foods for OAS are always raw (not cooked.)
- Fresh Fruits. These include apple, apricot, banana, cherry, melons, orange, peach and pear.
- Raw Veggies. These include carrot, celery, parsley, potato and tomato. Carrots and celery have the highest risk for also causing serious symptoms.
- Certain Seeds. These include sunflower seeds and fennel seeds.
OAS and Nose Allergies Can Be Linked
- Over 50% of people who are allergic to pollen also have OAS. This means 10% of all people.
- Ragweed pollen allergy can cross-react with all melons. Also, sometimes with bananas and tomatoes.
- Birch pollen allergy can cross-react with raw potatoes, carrots, celery and apples.
- Grass pollen allergy can cross-react with tomato and kiwi.
When to Call for Food Allergy
Call 911 Now
- Life-threatening allergic reaction to similar food in the past.
 Food eaten less than 2 hours ago.
Food eaten less than 2 hours ago. - Trouble breathing or wheezing
- Hoarse voice or cough start all of a sudden
- Trouble swallowing, drooling or slurred speech start all of a sudden
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hives all over start 2 to 4 hours after eating high-risk food. High-risk foods include nuts, fish, shellfish, or eggs.
- Major face swelling (not just lips) starts 2 to 4 hours after eating high-risk food
- Vomiting or stomach cramps starts 2 to 4 hours after eating high-risk food
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Other symptoms that might be from a food allergy and present now
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Recurrent symptoms that might be from a food allergy but not present now
- Oral Allergy Syndrome suspected but never confirmed by a doctor
- Food allergy diagnosed and you want to restart that food
- You have other questions or concerns
Self Care at Home
- Food allergy: mild reaction
- Oral allergy syndrome
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice
Treatment of a Food Allergy
- What You Should Know About Food Allergies:
- About 5% of children have food allergies.
- Most children with a new food reaction need to be seen.

- If your child is stable, hives often can be treated at home.
- Hives as the only symptom can have many causes.
- Your child can be seen later to decide future risks and best treatment.
- Here is some care advice that should help.
- Allergy Medicine for Hives:
- Give Benadryl 4 times per day for hives all over. Age limit: 1 and older.
- Use the allergy medicine until the hives are gone for 12 hours.
- If the hives last more than a few days, switch to a long-acting antihistamine, such as Zyrtec. No prescription is needed. Age limit: 2 and older.
- Caution: if your child is less than 1 year, call your doctor for advice.
- Cool Bath for Itching:
- To help with any itching, can also give a cool bath. Do this for 10 minutes.
- Caution: Do not cause a chill.
- How to Prevent Future Reactions:
- Help your child avoid the food that caused the symptoms.
- Read labels on all food products fully.
- Tell other people who care for your child of your child's food allergy. Also, inform the staff at your child's school.
- Learn more at Food Allergy Research and Education.
- Help your child avoid the food that caused the symptoms.
- What to Expect:
- Hives from foods often last just a short time.
- They often are gone in less than 6 hours.
- Return to School:
- Hives cannot be spread to others.
- Your child can go back to school once feeling better. The hives shouldn't keep him from doing normal things.
- Call Your Doctor If:
- Trouble breathing occurs
- Trouble swallowing or drooling occurs
- Severe hives not better after 2 doses of Benadryl
- Hives last over 24 hours
- You think your child needs to be seen
- Your child becomes worse
Treatment of Oral Allergy Syndrome Symptoms
- What You Should Know:
- Oral Allergy Syndrome (OAS) is very common.
 It happens in 10% of people. Most of them also have pollen allergies.
It happens in 10% of people. Most of them also have pollen allergies. - The symptoms are not harmful and can be treated at home.
- Needed for OAS: Your child has never had any serious symptoms with this food.
- OAS symptoms don't last very long.
- Here is some care advice that should help.
- Oral Allergy Syndrome (OAS) is very common.
- Rinse the Mouth:
- Rinse the lips and mouth with warm water. Do this a few times.
- Reason: To remove any traces of the food.
- Cold Pack:
- Use ice or a cold pack to the swollen lips or tongue for 10 minutes.
- Reason: To lessen the swelling and the itch.
- Allergy Medicine:
- One dose of Benadryl may help the symptoms go away faster.
- No prescription is needed. Age limit: 1 or older.
- How to Prevent Future OAS:
- Keep a list of the foods that cause your child's symptoms.
- Avoid these foods if they are raw (fresh).
- The cooked version of these foods usually won't cause any symptoms.
- What to Expect:
- With or without treatment, the itching will go away in 1 to 2 hours.
- The mouth swelling will also go away quickly.
- Call Your Doctor If:
- Trouble swallowing or drooling occurs
- Trouble breathing occurs
- Swelling or rash occurs anywhere else
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 04/24/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
Food allergies in young children!
Food allergies in young children!
Every mother remembers the calm days of pregnancy, where you could eat various foods in your diet without dieting. The main table during pregnancy should be as balanced as possible, fortified and the necessary ratio of proteins, fats, carbohydrates. There comes a happy moment in life, this is the birth of a baby. Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions.
The main table during pregnancy should be as balanced as possible, fortified and the necessary ratio of proteins, fats, carbohydrates. There comes a happy moment in life, this is the birth of a baby. Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions.
Very often, young parents face the first difficulties in the neonatal period (such as intestinal colic), in early childhood, such manifestations as rashes on the body, stool disorders (loose stools / constipation).
The most frequently asked questions of parents we will consider in this article:
- How does a food allergy manifest itself?
2. What is the duration of manifestation of external signs?
3. Is it worth giving up breastfeeding in favor of artificial (hydrolyzed and amino acid mixtures) or switching to goat's milk?
4. Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Food allergy is a food-induced reaction that causes a pathological reaction based on immune mechanisms (specific IgE-mediated reactions, cellular immune response (non-IgE-mediated) or a combination of both - a mixed type reaction).
As a food allergen, there can be any substances, most often of a protein nature, that stimulate the production of IgE.
The most common foods that cause allergic reactions are cow's milk, chicken eggs, peanuts, tree nuts, fish, seafood, wheat, soy, and beef.
The most significant allergen is Cow's milk protein, which according to clinical guidelines is 2-3% among infants. With age, tolerance develops in 80% of sick children, by the age of 6 years, the incidence decreases by less than 1%.
Any protein component of milk can cause sensitization, but most often: beta-lactoglobulin, alpha-lactalbumin, bovine serum albumin and gamma globulin, alpha-casein and beta-casein.
Food allergy is a symptom complex of diseases and is not a nosological diagnosis.
Therefore, the clinical and etiological significance of food allergy is taken into account, it is included in the full clinical diagnosis after the designation of the nosological form.
- Atopic dermatitis
- Allergic urticaria
- Allergic gastroenteritis and colitis
Laboratory diagnostics:
- IgE (sIgE) - immunoglobulin E, specific immunoglobulin
The main function of IgE is to provide an individual immune response of the body to the introduction of an irritant (antigen) with a certain biological activity
- Food panel
In case of food allergy in young children, manifestations in the form of constant itching (characteristic of any age period), skin syndrome are more common. Atopic dermatitis in young children is infancy, during this period the exudative form of the disease predominates. The clinical picture is represented by erythematous spots, papules, vesicles on the forehead, cheeks, scalp, accompanied by intense itching, swelling, weeping. Pronounced red dermographism. Most often, rashes are localized on the extensor and flexor surfaces of the limbs.
The clinical picture is represented by erythematous spots, papules, vesicles on the forehead, cheeks, scalp, accompanied by intense itching, swelling, weeping. Pronounced red dermographism. Most often, rashes are localized on the extensor and flexor surfaces of the limbs.
The duration of rashes depends on the timely start of treatment, as well as the complete exclusion of allergens (food). In children of the first year of life, the most common allergen is cow's milk protein.
Breastfed infants develop a clinically significant allergy to CMP due to the passage of dietary proteins into breast milk. I often see surprise in the eyes of young mothers and the rejection of the recommendation to exclude cow's milk protein. Counter questions: what exactly to use in the diet for mom? Dear mothers, a balanced diet for a nursing mother should be varied, complete and as natural as possible. The use of cereals (rice, buckwheat, corn, oatmeal, etc.), soups, meat products (turkey, chicken, pork), quail or chicken eggs, green fruits, etc. Therefore, the absence of whole cow's milk will not affect your menu variety in any way.
Therefore, the absence of whole cow's milk will not affect your menu variety in any way.
Should I give up breastfeeding?
Indeed, mothers often ask such questions. My answer is no! Breastfeeding is the key to the full development of the child. Only in the case when breastfeeding is impossible (complete hypogalactia of the mother, impossibility of breastfeeding due to congenital diseases (example: congenital malformation of cleft lip and palate), the presence of chronic infectious diseases in the mother are life-threatening for the child.
In the case where it is not possible to store the GW. The recommendations use hydrolyzed mixtures, or amino acids!
Hypoallergenic mixtures do not belong to clinical nutrition, they are prescribed only for children prone to the development of allergies (taking into account history and heredity).
Soy Blend is also not a health food and may cause a cross reaction!
Switching to goat's milk is not the smart way. Since in this case, goat milk can act as a cross-allergen, causing cross-allergic reactions in patients with an allergy to CMP, and is an independent allergen, causing severe reactions in patients who are tolerant to cow's milk. And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment.
Since in this case, goat milk can act as a cross-allergen, causing cross-allergic reactions in patients with an allergy to CMP, and is an independent allergen, causing severe reactions in patients who are tolerant to cow's milk. And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment.
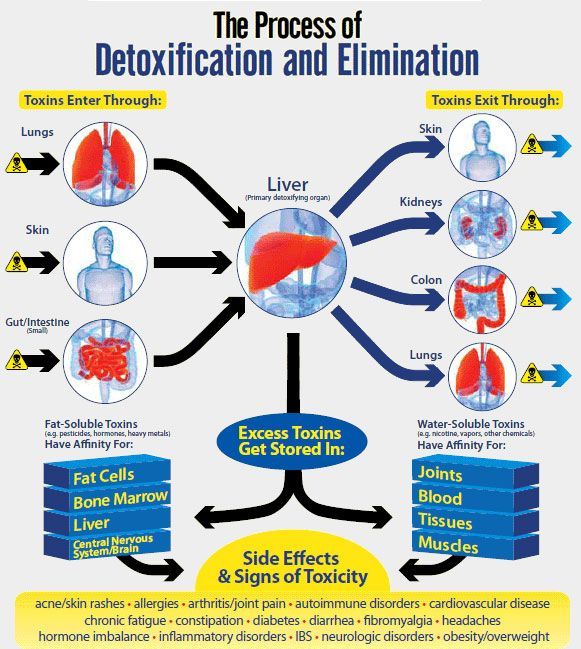
Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Gastrointestinal manifestations are manifestations of the digestive organs. Food allergies are not only when there are rashes on the body. An allergen that passes through the gastrointestinal tract can cause dyspeptic manifestations (regurgitation, intestinal colic, abdominal pain, vomiting, blood streaks in the stool). Such children very often end up in an infectious diseases hospital. Receive symptomatic therapy, which brings only temporary improvement. If not diagnosed in time, unfortunately, this can lead to irreversible consequences.
If your baby does not have subfebrile / febrile body temperature, for a long time there is no improvement after a course of medication prescribed by your doctor, the presence of streaks of blood, mucus, discoloration in the stool, then most likely your child has a Gastrointestinal form of food allergy.
Gastrointestinal form of food allergy can occur both on breastfeeding and on artificial.
For mothers following a therapeutic diet with complete exclusion of CMP. Children with artificial feeding, the transition to clinical nutrition. The effect of timely treatment comes quickly. Following a diet in the future leads to a rapid recovery of the gastrointestinal tract.
Yours sincerely, pediatrician GAUZ KO KGDKB No. 1
Ryazanova Svetlana Sergeevna
back
Food allergy
Food allergy is an excessive reaction of the body to substances contained in certain types of food.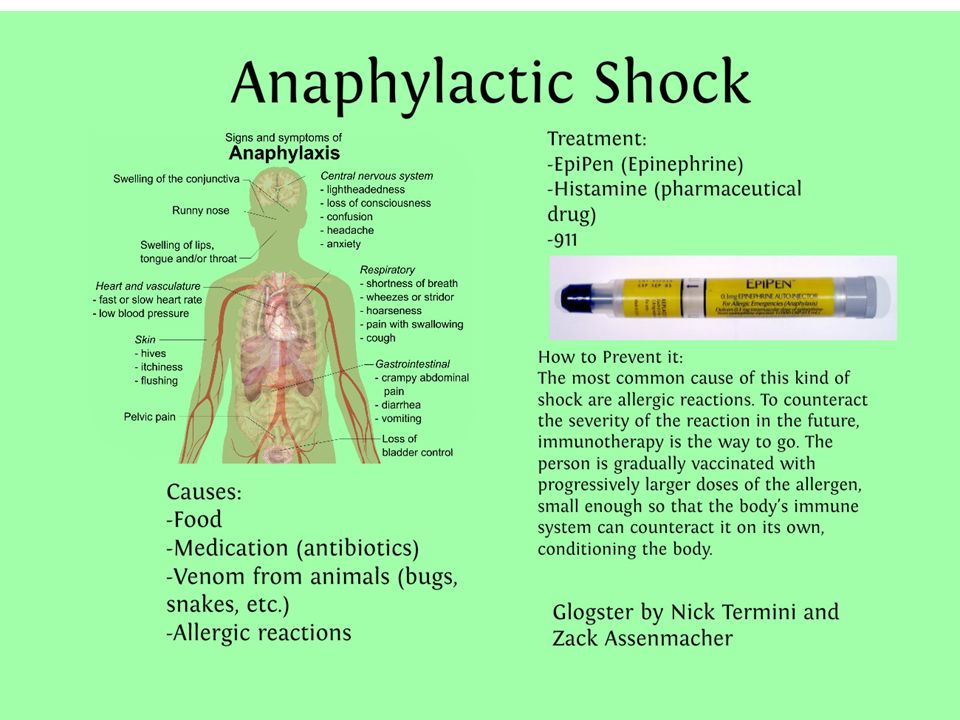 As a result, eating even small amounts of these foods causes unpleasant symptoms. Food allergies are often confused with intolerance to certain types of food, since their symptoms are similar, but with intolerance, the immune system is not involved in the pathological reaction.
As a result, eating even small amounts of these foods causes unpleasant symptoms. Food allergies are often confused with intolerance to certain types of food, since their symptoms are similar, but with intolerance, the immune system is not involved in the pathological reaction.
Food allergies are mild in most people, although anaphylactic shock, a severe life-threatening condition, rarely occurs.
Food allergies affect 2-3% of adults and 6-8% of children under 6 years of age. 5% of them develop bronchial asthma. There is no cure for food allergies, but more than half of children outgrow them. Of primary importance is the complete exclusion from the diet of foods that cause an allergic reaction.
Synonyms Russian
Nutritional allergy.
Synonyms English
Allergy to food, food allergies, alimentary allergy.
Symptoms
Usually the symptoms of a food allergy develop immediately, within the first minutes and no later than two hours after the allergen enters the body. Less common is the so-called delayed variant of an allergic reaction, when symptoms develop over a period of several hours to several days and are less pronounced. The combination of immediate and delayed food allergies is especially common in children.
Less common is the so-called delayed variant of an allergic reaction, when symptoms develop over a period of several hours to several days and are less pronounced. The combination of immediate and delayed food allergies is especially common in children.
The main symptoms of a food allergy are:
- rash,
- itching,
- swelling of the face, neck, lips, tongue,
- shortness of breath,
- cough,
- runny nose, lacrimation,
- abdominal pain,
- diarrhea,
- nausea, vomiting,
- malaise, weakness.
General information
Food allergies are based on an excessive reaction of the body's immune system to the components of certain products - allergens. With food allergies, blood cells (lymphocytes) produce specific proteins - immunoglobulins E, which interact with food proteins. That is, a reaction occurs that is similar to the response of the body to the ingestion of pathogenic microorganisms, but erroneously directed to the proteins of certain products.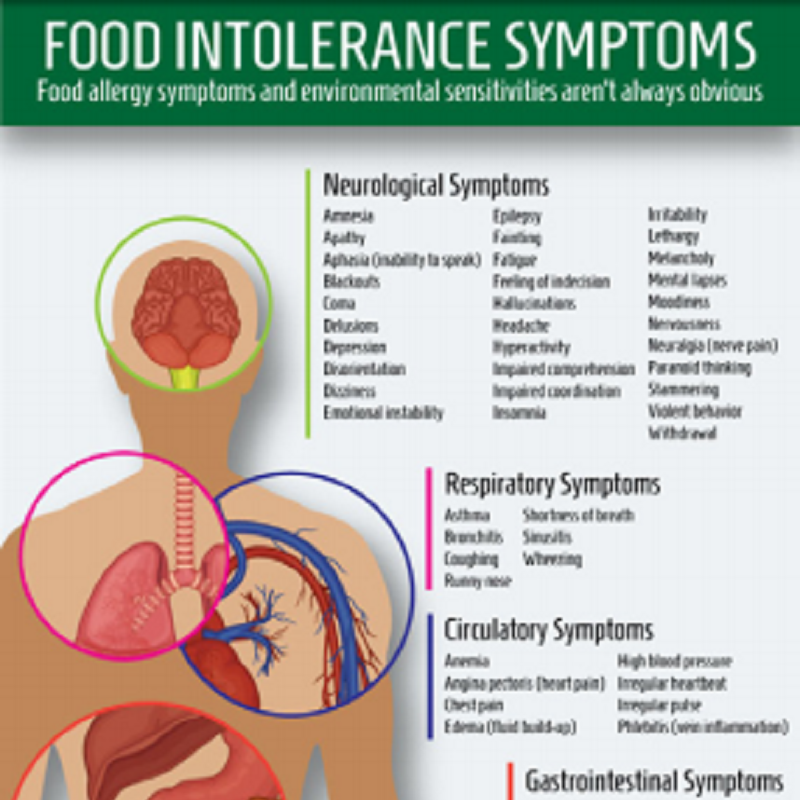
When immunoglobulins E interact with the allergen, biologically active substances are released that affect various organs - the skin, respiratory tract, gastrointestinal tract. As a result, characteristic allergy symptoms occur: rash, itching, swelling, respiratory failure, disruption of the digestive system. With the participation of immunoglobulins E, an immediate reaction to the allergen occurs.
When the allergen enters the body for a long time, immunoglobulins G enter into the reaction. A delayed, delayed allergic reaction is formed. Most often, it is manifested by a rash, itchy skin, which develop over several hours or days, which makes it difficult to diagnose this type of food allergy. Children may experience colic, constipation, flatulence, often in combination with symptoms of an immediate reaction to the allergen.
A very severe reaction to an allergen can lead to anaphylaxis (anaphylactic shock). Anaphylaxis develops within a few minutes after a food allergen enters the body and is accompanied by a sharp difficulty in breathing, swelling of the face, lips, pallor, a drop in blood pressure, a rapid spread of a rash, and skin itching. If you suspect anaphylactic shock, you should immediately seek medical help, as it can be fatal.
If you suspect anaphylactic shock, you should immediately seek medical help, as it can be fatal.
The most common allergies are eggs, milk, soy, wheat, peanuts, tree nuts, fish, and shellfish. In some cases, there are cross-reactions - this means that a person who is allergic to peanuts may have a reaction to beans, with an allergy to wheat, a reaction to rye.
The prevalence of allergies to a particular type of food also depends on the region of residence. For example, in Norway, the most common food allergy is to fish, in Japan - to rice.
Food allergies have become much more common in recent decades, especially among children. This is associated, on the one hand, with a change in the principles of nutrition of children in the first years of life, and on the other hand, with the fact that children grow up in a "sterile" environment, which makes it difficult for the full development of the immune system.
However, most children outgrow food allergies. This means that a child who suffered from an allergy to a product during the first years of life can get rid of it by adolescence.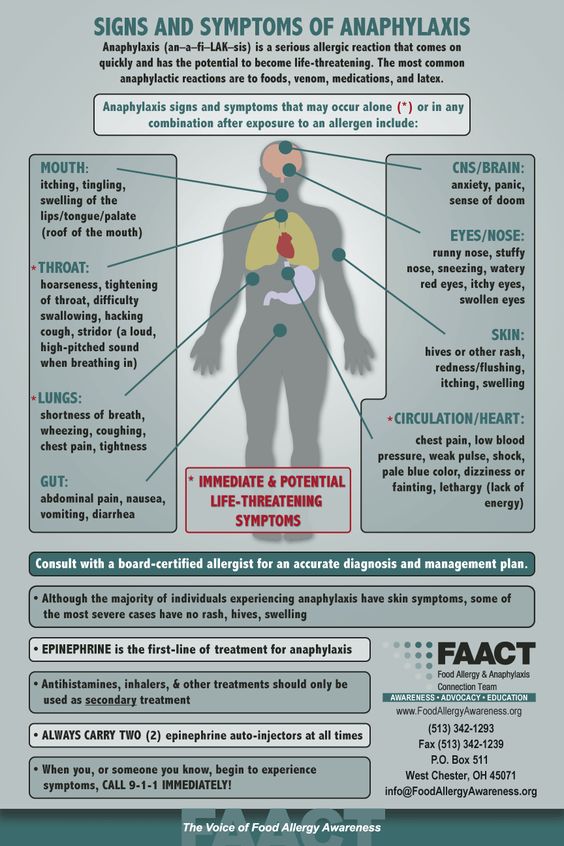 This, apparently, is due to the cessation of the production of specific immunoglobulins with prolonged exclusion of the allergen from the diet. Adults who are allergic to any food component are usually forced to permanently eliminate it from the diet.
This, apparently, is due to the cessation of the production of specific immunoglobulins with prolonged exclusion of the allergen from the diet. Adults who are allergic to any food component are usually forced to permanently eliminate it from the diet.
Who is at risk?
- People whose relatives suffer from food allergies
- Patients with other types of allergies - bronchial asthma, atopic dermatitis.
Diagnosis
In the diagnosis of a food allergy, examination of the patient and his careful questioning to identify the relationship between the intake of a certain food and the symptoms of an allergic reaction are of great importance. If the determination of the allergen is difficult, the doctor may prescribe a number of additional studies.
Laboratory diagnostics
- Complete blood count (without leukocyte formula and ESR). With food allergies, the level of eosinophils, leukocytes (white blood cells), which are involved in allergic reactions due to the release of biologically active substances, such as histamine, may increase.

- Determination of the amount of immunoglobulins E in the blood. Immunoglobulins E are proteins that come into contact with the allergen, which leads to the release of active substances and the appearance of symptoms. Their level in food allergies can be increased.
- Specific Immunoglobulins E and G - to identify the specific food component that causes an allergic reaction.
Other research methods
- Food diary analysis. It consists in carefully recording the time of eating, its composition and the time of the onset of allergy symptoms. Helps the doctor to establish the relationship between the intake of certain foods and the occurrence of allergic reactions.
- Elimination samples. A component that can cause allergies is removed from the diet, and the patient's condition is monitored.
- Provocative tests. After the probable allergen is excluded from the diet and the symptoms disappear, the patient is injected with this allergen and the body's reaction is monitored.