How long should i wait to feed my baby after vomiting
Vomiting
Nationwide Children’s Hospital
Vomiting (throwing up) is most often caused by a virus or stomach bug. Some serious illnesses may also cause vomiting. Vomiting caused by a virus usually lasts only a couple of days. It can often be treated at home.
The main danger from vomiting is dehydration. This means that the child has lost too much fluid and does not have enough electrolytes (salts) in their body for it to work the right way. It is most important for your child to drink plenty of liquids to prevent dehydration.
Do not lay your baby on their stomach to sleep after they have vomited. They are still safest sleeping on their backs. Toddlers may sleep on their side or stomach with their heads turned.
Liquids You May Give- Older children often do well with water or clear liquids to prevent dehydration.
Clear liquids include lemonade, fruit juices without pulp (cranberry, cranapple, or apple juice), and popsicles. The popsicles must be free from cream, pudding, yogurt, or bits of fruit.
- Your child may need to drink an oral rehydration solution (ORS) like Pedialyte®. An ORS helps replace the electrolytes and fluids that your child needs.
- You can buy ORS in liquid or powder form or as popsicles at most pharmacies without a prescription. ORS store brands are just as good as a brand name.
- Do not water down (dilute) or mix an ORS with formula.
- Offer your child other things to drink. ORS should not be given as the only fluid for more then 6 hours.
Children Younger Than 1 Year of Age:
- ORS
- Breast milk or formula mixed the normal way if they can drink it
- No water except when used to make formula
- Do not give fruit juices or liquids that are high in sugar, such as Hawaiian Punch®, Hi-C®, Kool-Aid®, sodas, or syrups.
 Do not give teas or broths. These liquids could make your child feel worse.
Do not give teas or broths. These liquids could make your child feel worse.
Children Older Than 1 Year of Age:
Same as above and:
- Water
- Clear liquids
- Ice popsicles made from ORS
- Milk, if tolerated
- Flavored gelatin cube
When your child is vomiting:
- Offer clear liquids after your child has not vomited for 30 to 60 minutes. This gives the stomach time to rest.
- Breastfeeding should not be stopped. Try to nurse your baby more often.
- If needed, you can stop giving formula if you are giving ORS. Try to restart formula as soon as possible.
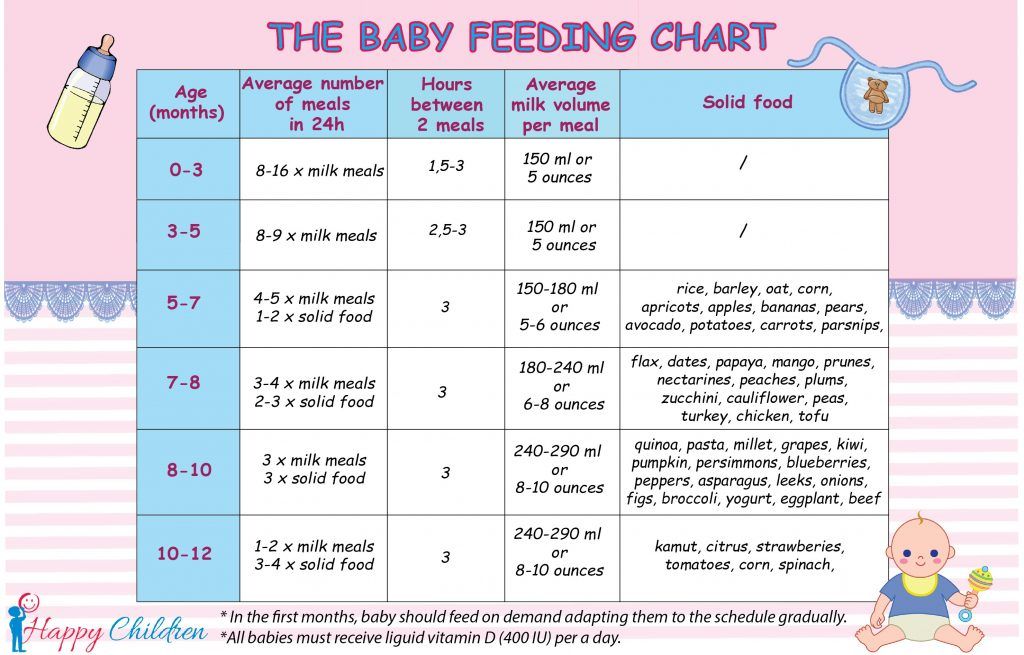
- Start slow (Picture 1). Give small sips of liquids often. This may reduce the vomiting.
- For children under 1 year: use a spoon or syringe to give 1 to 2 teaspoons every few minutes (5 to 10 mL).
- For older than 1 year: give ½ to 1 ounce (1 to 2 tablespoons or 15 to 30 mL) every 20 minutes for a few hours.
- For children under 1 year: use a spoon or syringe to give 1 to 2 teaspoons every few minutes (5 to 10 mL).
- When your child can drink without vomiting, gradually increase the amount. If they still vomit, wait 30 to 60 minutes, and start again.
- Do not force your child to drink or wake them up to drink if they are sleeping.
- Do not give any kind of milk or yogurt drinks until the vomiting has stopped for 8 hours.
Amount of Liquid to Give to Prevent Dehydration
| Child’s Weight | Minimum Goal to Give Every Hour* |
| 7 to 10 lbs. | At least 2 ounces (4 tablespoons or ¼ cup) |
| 11 to 15 lbs. | At least 2½ ounces (5 tablespoons) |
| 16 to 20 lbs. | At least 3½ ounces (½ cup) |
| 21 to 40 lbs. | At least 6½ ounces (¾ cup) |
| 41 to 60 lbs. | At least 10 ounces of liquid every hour (1¼ cups per hour) |
* Minimum fluid goals per hour may increase if vomiting, diarrhea, or fever are present.
Solid Foods- When children are vomiting, they usually don't feel like eating solid food. It will not hurt them to miss a few meals as long as they can drink enough fluids.
- After about 6 to 8 hours of giving clear liquids and your child is no longer vomiting, try to get them to start eating some food.
 Starchy, bland foods like cereals, crackers, or bread are easier to digest. Avoid foods high in sugar and greasy, fried foods. Do not give them red-colored foods that might look like blood in vomit.
Starchy, bland foods like cereals, crackers, or bread are easier to digest. Avoid foods high in sugar and greasy, fried foods. Do not give them red-colored foods that might look like blood in vomit.
Medicine: Some medicines used for vomiting in older children or adults are very dangerous for young children. WARNING: Do not give your child any medicine unless their doctor or health care provider tells you it's safe for them.
Sleep: It's important that your child gets plenty of rest. Sleep helps the stomach finish digesting any food in it. It may calm your child’s vomiting.
Preventing the Spread of InfectionYou can help stop the spread of viruses and protect others by:
- Make sure your child washes their hands with soap and water after using the toilet and before eating.
- Wash you hands often and after touching your child, their eating utensils, or anything that might have vomit on it.
 Use soap and water or a hand sanitizer.
Use soap and water or a hand sanitizer. - Keep the things your child uses, like toys and dirty clothes, away from others. Wash them in hot, soapy water.
- Clean the toilet and hard surfaces often with disinfectants or alcohol wipes. Let dry for 15 seconds.
- Use clean wipes or washcloths for each diaper change. Put the used diaper in the diaper pail or trash right away.
Call your child's doctor or health care provider if you think they're getting worse, do not get any better in 24 hours, will not breastfeed, or show these signs:
- Vomiting gets worse or happens more often. Vomit is bright green or has blood or dark specks that look like coffee grounds in it.
- Your child shows signs of being dried out (dehydration) (Picture 2).
- Urine is very dark
- Newborn (0 to 4 months) has less then 6 wet diapers in a day
- Child (4 months or older) has less than 3 wet diapers in a day or pees less than 3 times in a day
- No tears when crying
- Dry or sticky mouth
- Hard or fast breathing
- Sunken-looking eyes
- Soft spot on baby’s head is flat, sunken, or pulls in
- Hard to wake up (lethargic), acts confused or does not know what they are doing
- Urine is very dark
- Your child has a high fever.
 Use a digital thermometer and wash it after each use.
Use a digital thermometer and wash it after each use. - Younger than 3 months of age - 100.4° Fahrenheit (F) or 38° Celsius (C) or above
- Older than 3 months of age - 104°F (40°C) or above, above 102F (38.9C) for more than 2 days or keeps coming back, or they have been treated to bring their fever down but it hasn't worked.
- If your child has a fever and:
- Looks very ill, is fussy, or is drowsy
- Has an unusual rash
- Has a stiff neck, a bad headache, or sore throat
- Has immune system problems that make them more likely to get sick, such as sickle cell disease or cancer, or takes medicine that weakens the immune system
Vomiting (PDF), Somali (PDF), Spanish (PDF)
HH-I-71 ©Copyright 1977, revised 8/22 | Nationwide Children’s Hospital
You Might Also Be Interested In
Article
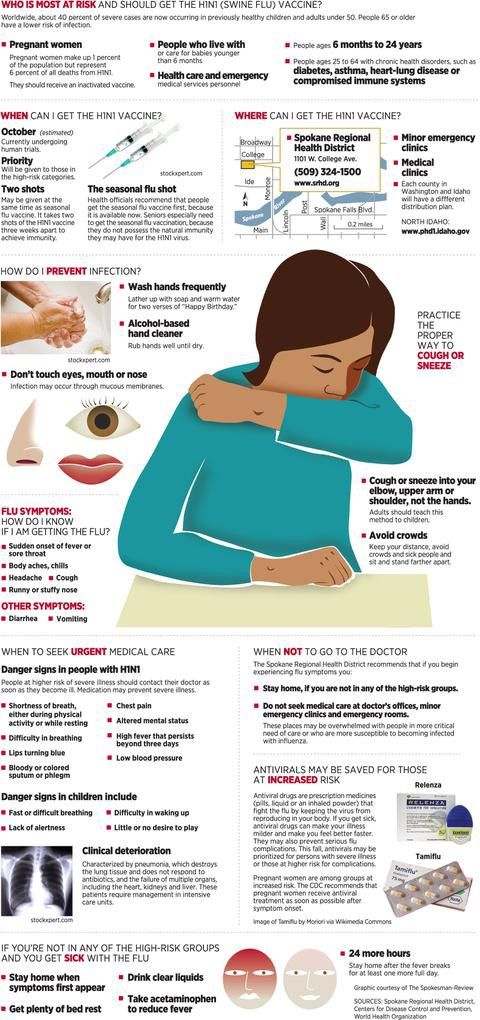
Seasonal Flu Resources
Rotavirus
Blog
Bivalent COVID Vaccines: What You Need to Know
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding.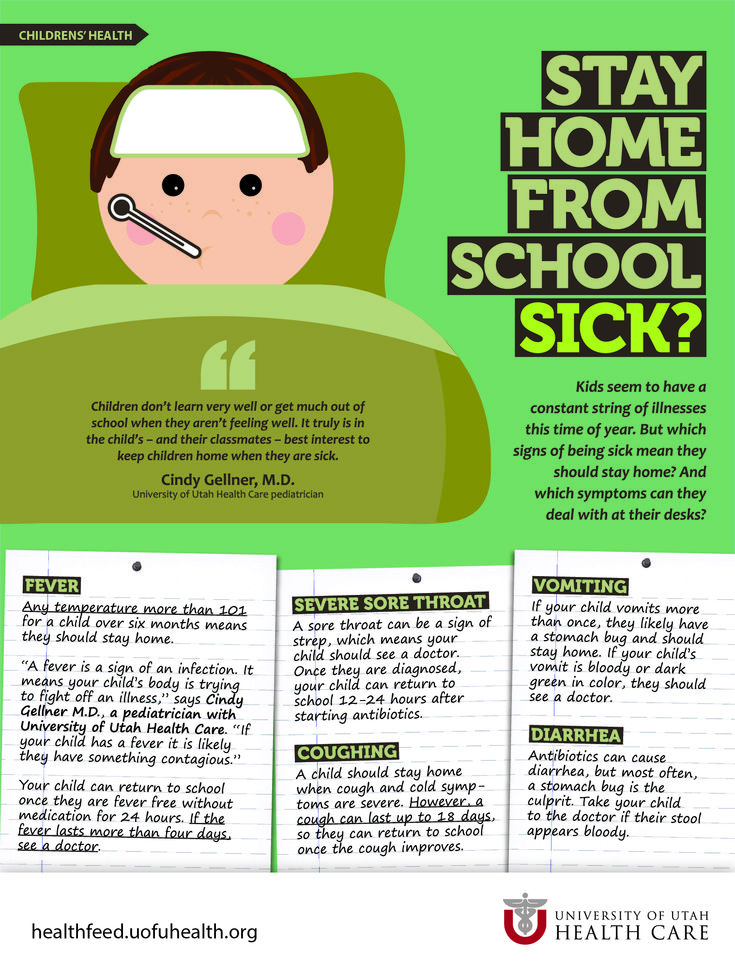 How soon should you feed your baby after vomiting?
How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year.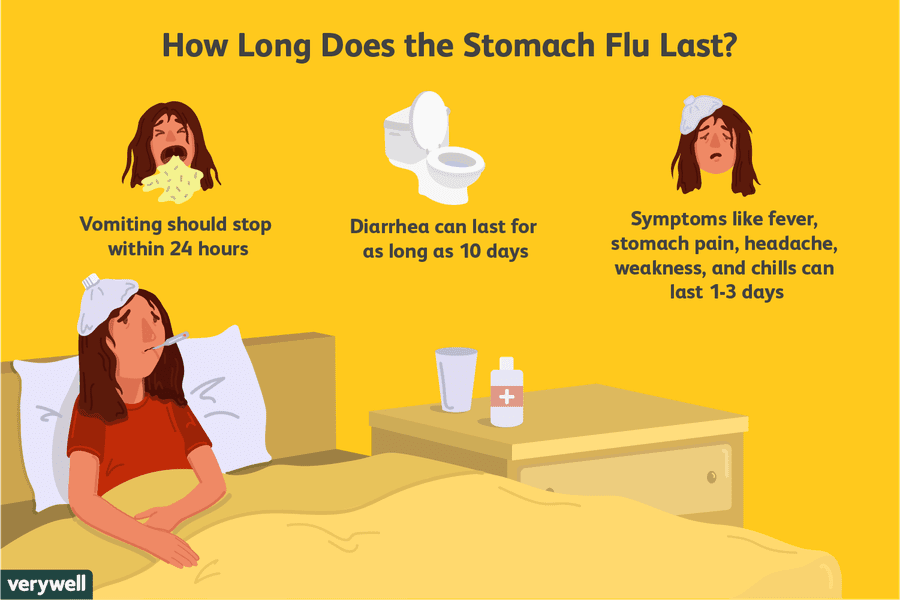 Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
4
What is a "milk flush"?
At the beginning of each feed, a hungry baby actively sucks on the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding.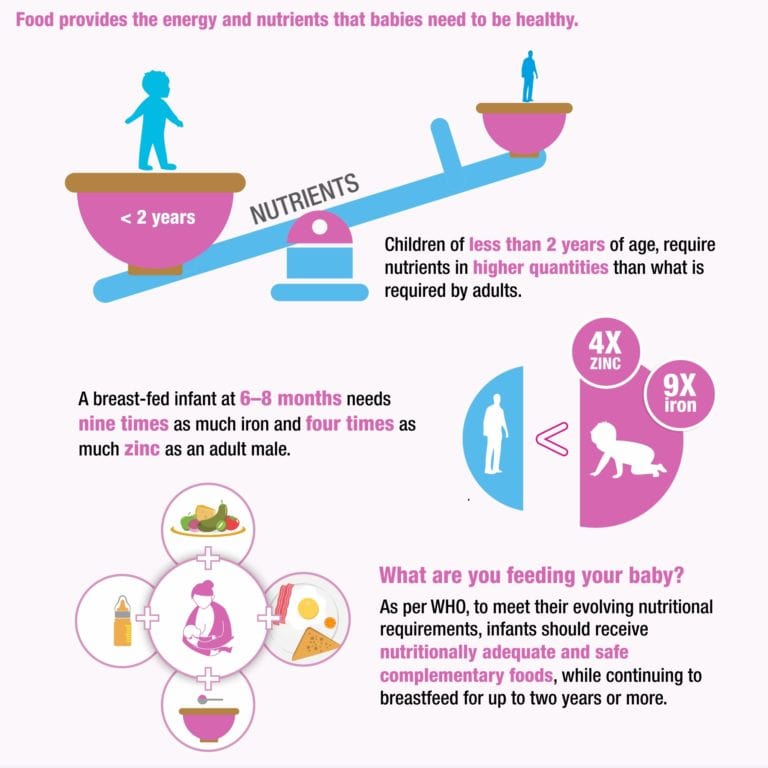 6
6
“When a child has had enough, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more.”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks to breastfeed very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, just when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“Nobody told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will begin to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11–13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” says Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding Beyond the First Month: What to Expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al. , Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
, Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation .Am J Clinl Nutr . 1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
- Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev .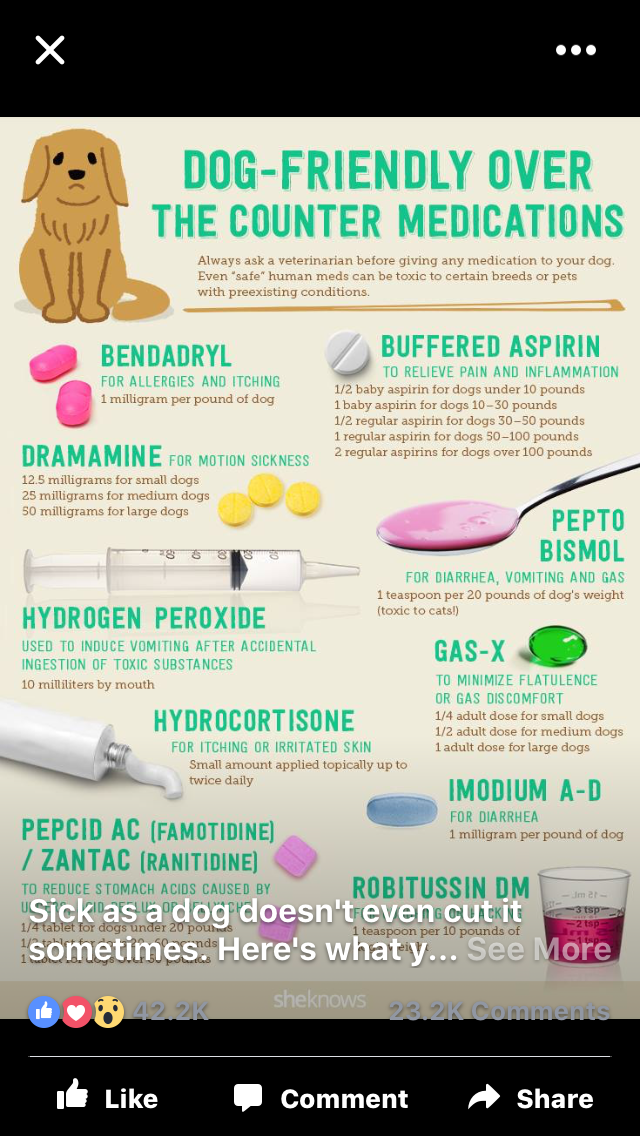 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas J Cancer Prev. 2014;15(12):4829-4837.
2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas J Cancer Prev. 2014;15(12):4829-4837.
when is it really dangerous? What to do with bouts of vomiting? When should you see a doctor for vomiting?
+7 (495) 780-07-71
Call center open 24/7
Ambulancearound the clock
Author
Dmitrieva Valentina Alexandrovna
Leading physician
Therapist
Cashback 1000 rub for all services for a visit in October More All promotions
Vomiting is a reflex eruption through the mouth of the contents of the stomach, and sometimes the duodenum.
The gag reflex is quite complex - it involves various muscle groups. It is controlled by the vomiting center located in the brain stem. By its very nature, vomiting is a mechanism by which the body defends itself against poisoning. Normally, vomiting is a reaction to the ingestion of toxic substances into the gastrointestinal tract or simply something that cannot be digested - for example, too fatty foods. Therefore, after an attack of vomiting, a person often feels relieved: the body has cleansed itself.
Normally, vomiting is a reaction to the ingestion of toxic substances into the gastrointestinal tract or simply something that cannot be digested - for example, too fatty foods. Therefore, after an attack of vomiting, a person often feels relieved: the body has cleansed itself.
However, the intoxication that caused vomiting may have an internal source, that is, be the result of any pathology or disease. It is also possible that the irritation of the nervous system, leading to vomiting spasms, is not related to the state of the stomach at all. This makes one perceive vomiting as a very serious, and even formidable symptom. An attack of vomiting is almost always a sufficient reason to see a doctor. In case of recurring attacks, you should definitely consult a doctor!
Causes of vomiting
In most cases, vomiting is due to irritation of the receptors of the stomach or, in medical terms, has a visceral origin. The cause is most often acute or chronic diseases of the stomach itself (acute food poisoning, gastritis, stomach ulcers, food allergies). Also, the receptors of the stomach can also respond to diseases of other organs - the gallbladder, uterus, heart (vomiting is included in the complex of possible symptoms of myocardial infarction).
Also, the receptors of the stomach can also respond to diseases of other organs - the gallbladder, uterus, heart (vomiting is included in the complex of possible symptoms of myocardial infarction).
Vomiting can also be of central origin, that is, caused by pathologies of the central nervous system (brain), such as meningitis, encephalitis, trauma, and brain tumors. Quite often, vomiting is observed with migraines. Problems in the inner ear can also lead to vomiting (in which case, vomiting may be accompanied by dizziness). With excessive irritation of the receptors of the inner ear (during motion sickness), even a healthy person can vomit, especially if the vestibular apparatus is not trained. Sometimes vomiting is caused by an emotional disorder (stress) or is a reaction to something that causes extreme disgust (conditioned reflex vomiting).
Irritation of the vomiting center can be caused by toxic substances carried by the blood stream ( hematogenous toxic vomiting). Toxic substances can enter the body from the outside (for example, chlorine or carbon monoxide - by inhalation), or can be produced in the body itself - as a result of impaired liver or kidney function.
Toxic substances can enter the body from the outside (for example, chlorine or carbon monoxide - by inhalation), or can be produced in the body itself - as a result of impaired liver or kidney function.
Vomiting and other symptoms
Usually vomiting is preceded by nausea, because, in fact, vomiting is the resolution of nausea, its logical conclusion. The fact that nausea turned into vomiting indicates the severity of the pathological process. Vomiting spasms can be observed against the background of elevated temperature, accompanied by diarrhea. In the vomit, in addition to food debris, gastric juice and mucus, bile, blood, and pus may be present.
Repeated, periodically recurring and indomitable vomiting exhausts and dehydrates the body, leads to a violation of mineral metabolism and acid-base balance.
Diarrhea and vomiting
Vomiting and fever
When vomiting scares
Any bout of vomiting is a very unpleasant experience. Even if a person experiences relief with the resolution of an attack, vomiting itself is perceived as an extraordinary event, which should not normally be. The shock of the body, domestic and social inconvenience - all this makes vomiting a process of a different order compared to other reflex actions, such as coughing or sneezing. We always react sharply to vomiting (we do not leave it unattended), and rightly so.
Even if a person experiences relief with the resolution of an attack, vomiting itself is perceived as an extraordinary event, which should not normally be. The shock of the body, domestic and social inconvenience - all this makes vomiting a process of a different order compared to other reflex actions, such as coughing or sneezing. We always react sharply to vomiting (we do not leave it unattended), and rightly so.
However, in some cases, vomiting worries us especially strongly. Such is vomiting of bile , vomiting with blood . Parents are concerned about cases of vomiting in a child . Quite often, vomiting is observed during pregnancy , attracting increased attention.
These cases should be mentioned separately:
Vomiting of bile
Vomiting blood
Vomiting during pregnancy
Child vomiting
What to do if you throw up
Because anyone can experience vomiting, it's helpful to know how to prevent vomiting, what to do during and immediately after an attack, and when to see a doctor.
Nausea is a precursor to vomiting. If you feel sick, try opening a window (increase the oxygen supply), drinking some sweetened liquid (this will calm the stomach), sitting or lying down (physical activity increases nausea and vomiting). You can dissolve a tablet of validol. If you get sick on the road, take candy with you and dissolve on the way. This will help prevent vomiting.
What to do when vomiting
During an attack, it is important to exclude the ingress of vomit into the respiratory tract. The patient during vomiting should never lie on his back. Do not leave young children unsupervised if they may vomit. An elderly or weakened person must be helped to turn on his side, head to the edge of the bed, put a pelvis in front of him.
What to do after vomiting
After an attack, rinse your mouth with cold water. If the patient himself cannot do this, it is necessary to moisten a piece of gauze in a soda solution and wipe his mouth.
Immediately after the attack, you can drink only a few sips of water, and then if there was no blood in the vomit. You can drink properly only after 2 hours, and eat only 6-8 hours after the attack. Food should be dietary, sparing; best of all - porridge on the water, rice, low-fat soup.
With repeated attacks of vomiting, dehydration of the body is possible. Therefore, it is necessary to drink a special solution that restores the water-electrolyte and acid-base balance.
Any questions?
Leave the phone -
and we will call you back
When should you see a doctor if you vomit?
Vomiting - in many cases, a sign that the body is experiencing serious problems and needs to be cleansed, and therefore, most likely, in treatment. If the disease is accompanied by vomiting, this usually indicates that the disease is quite severe.
If the attack of vomiting was one-time and there is reason to believe that it was caused by overeating, motion sickness, alcohol poisoning or stress, there is no direct need to see a doctor. In all other cases, a doctor's consultation is necessary. Especially if the attacks are repeated for two days or more, as well as in the presence of diabetes or other chronic diseases.
In all other cases, a doctor's consultation is necessary. Especially if the attacks are repeated for two days or more, as well as in the presence of diabetes or other chronic diseases.
Sometimes emergency care is required for vomiting. You need to call an ambulance if:
- vomiting accompanied by persistent or severe abdominal pain;
- there are repeated bouts of vomiting after a head injury;
- with vomiting observed dehydration, dry mouth, increased urination;
- in the deterioration of mental and functional activity in the elderly;
- there is blood in the vomit (for example, impurities in the form of "coffee grounds").
Which doctor should I contact if I vomit?
Complaints of nausea and vomiting are usually addressed to a gastroenterologist or general practitioner (general practitioner, family doctor or pediatrician). In case of nausea and vomiting during pregnancy, you should contact your gynecologist.