How long should you breast feed a baby
Frequently Asked Questions (FAQs) | Breastfeeding
What are the benefits of breastfeeding?
Breastfeeding is good for both infants and mothers. Breast milk is the best source of nutrition for most infants. As an infant grows, breast milk changes to meet the infant’s nutritional needs. Breastfeeding can also help protect the infant and mother against certain illnesses and diseases:
Benefits to Infants
Infants who are breastfed have a lower risk of:
- Asthma.
- Obesity.
- Type 1 diabetes.
- Severe lower respiratory disease.
- Acute otitis media (ear infections).
- Sudden infant death syndrome (SIDS).
- Gastrointestinal infections (diarrhea/vomiting).
- Necrotizing enterocolitis (NEC) for preterm infants.
Benefit to Mothers
Mothers who breastfeed their infants have a lower risk of:
- Breast cancer.
- Ovarian cancer.
- Type 2 diabetes.
- High blood pressure.
Families can visit CDC’s Infant and Toddler Nutrition website to learn more about what to expect while breastfeeding.
When should a mother avoid breastfeeding (contraindications)?
Breast milk provides the best nutrition for most infants, including premature and sick newborns. However, there are rare exceptions when breast milk or breastfeeding is not recommended. Learn more about contraindications to breastfeeding.
Only a few medications are contraindicated (not recommended) while breastfeeding. Although many medications do pass into breast milk, most have little or no effect on milk supply or on an infant’s well-being. However, health care providers should always weigh the risks and benefits when prescribing medications to breastfeeding mothers.
Learn more about safe prescription medication use while breastfeeding.
Top of Page
How is growth assessed for breastfed infants?
In the United States, the World Health Organization (WHO) Growth Standard Charts are recommended for use with both breastfed and formula-fed infants and children, from birth to 2 years of age, to monitor growth.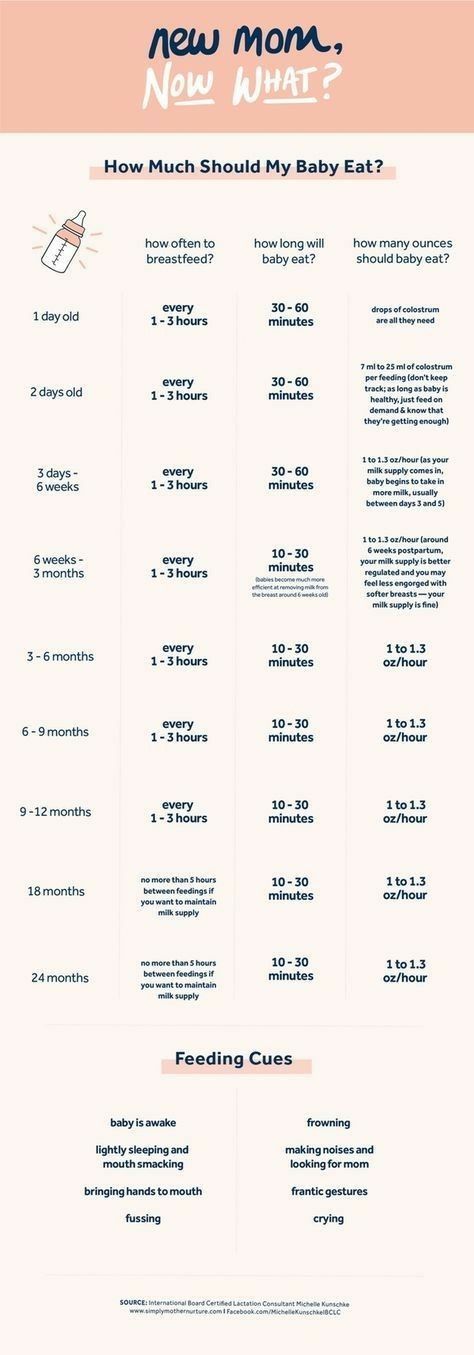 The WHO growth charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
The WHO growth charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
For children older than 2 years (2 to 19 years of age) CDC and the American Academy of Pediatrics recommend that health care providers use the CDC Growth Reference Charts.
Visit the Growth Chart Training website for a set of self-directed, interactive training courses.
Source: Grummer-Strawn LM, Reinold C, Krebs NF. Use of the World Health Organization and CDC growth charts for children aged 0 to 59 months in the United States.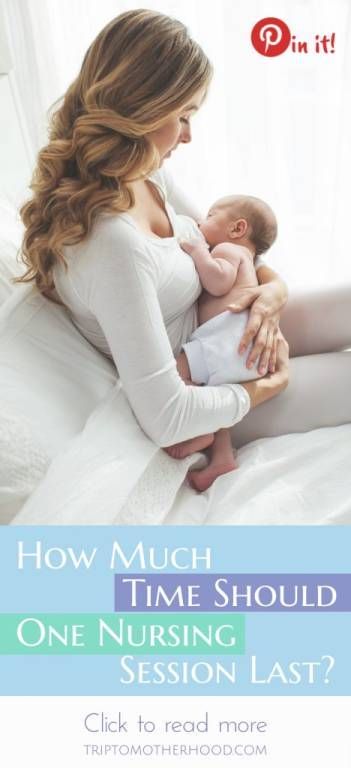 MMWR Recomm Rep. 2010;59(RR-9):1–15.
MMWR Recomm Rep. 2010;59(RR-9):1–15.
Top of Page
How long should a mother breastfeed?
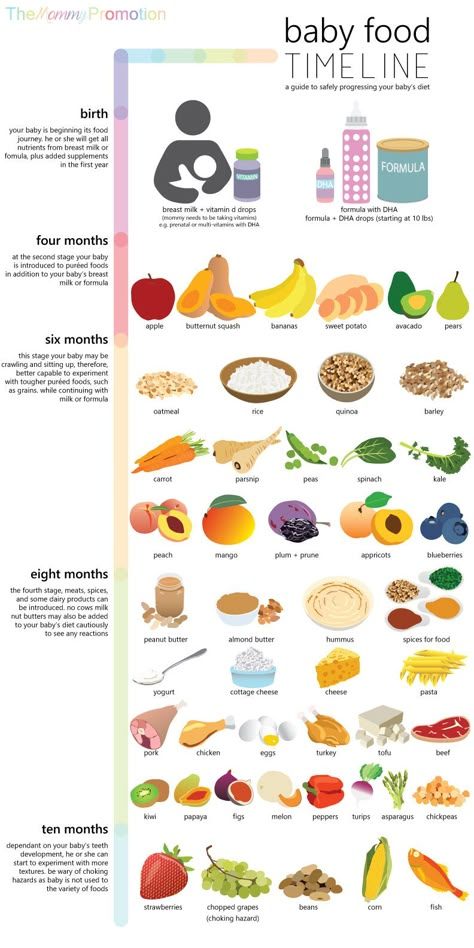
The U.S. Dietary Guidelines for Americans [PDF-30.6MB] recommend that infants be exclusively breastfed for about the first 6 months, and then continuing breastfeeding while introducing appropriate complementary foods until your child is 12 months old or older. The American Academy of Pediatrics and the World Health Organization also recommend exclusive breastfeeding for about the first 6 months, with continued breastfeeding along with introducing appropriate complementary foods for up to 2 years of age or longer.
Mothers should be encouraged to breastfeed their children for at least 1 year. The longer an infant is breastfed, the greater the protection from certain illnesses and long-term diseases. The more months or years a woman breastfeeds (combined breastfeeding of all her children), the greater the benefits to her health as well.
The American Academy of Pediatrics recommends that children be introduced to foods other than breast milk or infant formula when they are about 6 months old.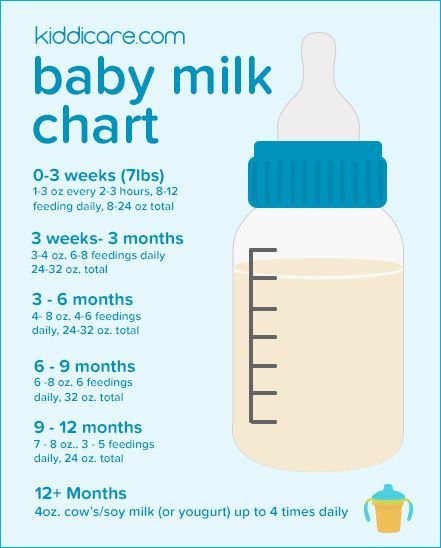 To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
Top of Page
What can happen if someone else’s breast milk is given to another child?
Very few illnesses are transmitted via breast milk. Learn more about what to do if an infant or child is mistakenly fed another woman’s expressed breast milk.
Top of Page
Are special precautions needed for handling breast milk?
CDC does not list human breast milk as a body fluid to which universal precautions apply. Occupational exposure to human breast milk has not been shown to lead to transmission of HIV or Hepatitis B infection. However, because human breast milk has been implicated in transmitting HIV from mother to infant, gloves may be worn as a precaution by health care workers who are frequently exposed to breast milk (e.g., people working in human milk banks (defined below). For additional information regarding universal precautions as they apply to breast milk in the transmission of HIV and Hepatitis B infections, visit the following resources:
Centers for Disease Control and Prevention. Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Top of Page
Where can mothers find more information about preparation and storage of breast milk?
CDC has guidelines for proper storage and preparation of breast milk to maintain the safety and quality of expressed breast milk for the health of the baby.
For more information about specific storage and preparation of breast milk questions, such as where to store breast milk at work, and what to do when the power goes out, visit CDC’s Storage and Preparation of Breast Milk Frequently Asked Questions.
Top of Page
What are human milk banks?
Human milk banks are a service established for the purpose of collecting milk from donors and processing, screening, storing, and distributing donated milk to meet the specific needs of individuals for whom human milk is prescribed by licensed health care providers.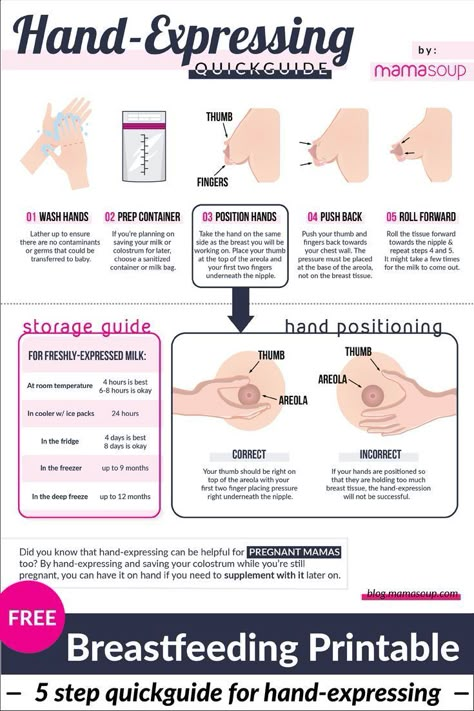 When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
Milk banks accept donations directly at their deposit sites or they can arrange for safe, overnight transportation of human milk at no cost to the donor. Learn more about donating to a milk bank by visiting the Human Milk Banking Association of North America (HMBANA).
Top of Page
Is it safe for families to buy breast milk on the internet?
The American Academy of Pediatrics and the Food and Drug Administration recommend avoiding Internet-based milk sharing sites and instead recommend contacting milk banks. Research has demonstrated that some milk samples sold online have been contaminated with a range of bacteria.1
Nonprofit donor human milk banks, where processed human milk comes from screened donors, have a long safety record in North America. All member banks of the Human Milk Banking Association of North America (HMBANA) must operate under specific evidence-based guidelines that require extensive testing and processing procedures as well as self-reported health information and a health statement from both the donor’s health care provider and the infant’s health care provider. Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
1Keim, SA, Hogan, JS, McNamara, KA, et al. Microbial contamination of human milk purchased via the internet. Pediatrics. 2013;132(5).
Top of Page
What legal rights do breastfeeding mothers have?
Breastfeeding Laws
- All 50 states, the District of Columbia, Puerto Rico and the Virgin Islands have laws that specifically allow women to breastfeed in any public or private location. Visit the National Conference of State Legislatures to learn more about federal and state laws that protect and support breastfeeding.
Workplace Laws
- The “Break Time for Nursing Mothers Provision” of the Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk.
 Visit the United States Department of Labor to learn more.
Visit the United States Department of Labor to learn more.
Travel Laws
- Air travelers are permitted by the Transportation Security Administration (TSA) to bring breast milk, formula, and juice in excess of 3.4 ounces in their carry-on baggage and it does not need to fit within a quart size bag. Ice packs, freezer packs, and other accessories needed to keep the liquid cool are also allowed in carry-on bags. All liquids and partially frozen accessories are subject to being screened by X-ray. TSA is required by the Bottles and Breastfeeding Equipment Screening Act (BABES act) to provide ongoing training to ensure TSA staff receive consistent training related to traveling with breast milk, formula, and infant feeding equipment. Visit the TSA to learn more about traveling with breast milk, formula, and juice. For tips on travel and breastfeeding, visit Travel Recommendations for the Nursing Mother.
Visit the Federal Policies, Programs, & Initiatives website to learn more about laws related to breastfeeding protections.
Top of Page
How can a mother continue to provide breast milk to her infant after returning to work or school?
Being prepared for returning to work or school can help a mother ease the transition and continue to breastfeed after her maternity leave is over. The Office on Women’s Health has information for making this transition easier.
When a mother is away from her infant, she can pump or hand express her breast milk so that her infant can drink breast milk from a bottle. Mothers can visit CDC’s Infant and Toddler Nutrition website to learn more about pumping breast milk.
Mothers who are expressing their breast milk should visit the CDC’s Proper Storage and Preparation of Breast Milk website to learn how to prepare and store breast milk safely for her infant.
The Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk.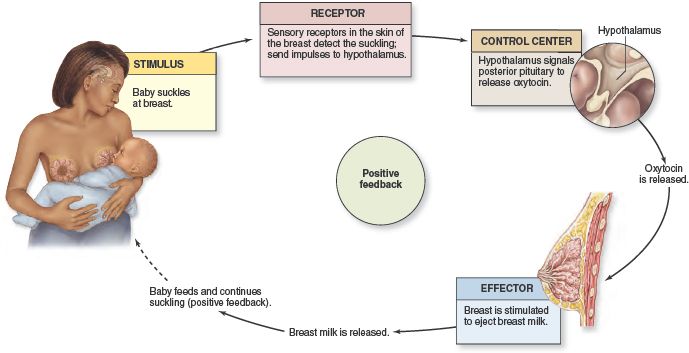 For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
Top of Page
Where can mothers find breastfeeding support and additional Information about breastfeeding?
Help mothers find lactation support through the following resources:
- International Lactation Consultant Association (IBCLCs)
- United States Lactation Consultant Association (IBCLCs)
- Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics
- La Leche League
Help mothers find resources about breastfeeding by directing them to the following websites:
- CDC— Infant and Toddler Nutrition
- Office on Women’s Health—Breastfeeding
- American Academy of Pediatrics—Healthy Children
- United States Breastfeeding Committee—State Coalitions Directory
- US Department of Agriculture—WIC Breastfeeding Support
Top of Page
Does breastfeeding during a child’s vaccine injections help with pain management?
Parents who are breastfeeding should be encouraged to breastfeed children age 2 years or younger before, during, and after their child’s vaccination. Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Top of Page
Does breastfeeding after a child’s rotavirus vaccine impact the vaccine’s efficacy?
There is not sufficient evidence to suggest that breastfeeding can have a negative effect on rotavirus vaccine efficacy. A previous study found that human milk from women who live in areas with endemic rotavirus contains antibodies that can neutralize live rotavirus vaccine virus. However, in licensing trials, the effectiveness of rotavirus vaccine in breastfed infants was comparable to that in non-breastfed infants.
CDC does not recommend restricting or discontinuing breastfeeding before or after a child receives the rotavirus vaccine. Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Learn More about prevention of Rotavirus Gastroenteritis among infants and children.
Top of Page
Breastfeeding FAQs: How Much and How Often (for Parents)
Breastfeeding is a natural thing to do, but it still comes with its fair share of questions. Here's what you need to know about how often and how long to breastfeed your baby.
How Often Should I Breastfeed?
Newborn babies should breastfeed 8–12 times per day for about the first month. Breast milk is easily digested, so newborns are hungry often. Frequent feedings helps stimulate your milk production during the first few weeks.
By the time your baby is 1–2 months old, he or she probably will nurse 7–9 times a day.
In the first few weeks of life, breastfeeding should be "on demand" (when your baby is hungry), which is about every 1-1/2 to 3 hours. As newborns get older, they'll nurse less often, and may have a more predictable schedule. Some might feed every 90 minutes, whereas others might go 2–3 hours between feedings.
Some might feed every 90 minutes, whereas others might go 2–3 hours between feedings.
Newborns should not go more than about 4 hours without feeding, even overnight.
How Do I Count the Time Between Feedings?
Count the length of time between feedings from the time your baby begins to nurse (rather than at the end) to when your little one starts nursing again. In other words, when your doctor asks how often your baby is feeding, you can say "about every 2 hours" if your first feeding started at 6 a.m., the next feeding was around 8 a.m., then 10 a.m., and so on.
Especially at first, you might feel like you're nursing around the clock, which is normal. Soon enough, your baby will go longer between feedings.
How Long Does Nursing Take?
Newborns may nurse for up to 20 minutes or longer on one or both breasts. As babies get older and more skilled at breastfeeding, they may take about 5–10 minutes on each side.
How long it takes to breastfeed depends on you, your baby, and other things, such as whether:
- your milk supply has come in (this usually happens 2–5 days after birth)
- your let-down reflex (which causes milk to flow from the nipple) happens right away or after a few minutes into a feeding
- your milk flow is slow or fast
- the baby has a good latch, taking in as much as possible of your areola (the dark circle of skin around your nipple)
- your baby begins gulping right away or takes it slow
- your baby is sleepy or distracted
Call your doctor if you're worried that your baby's feedings seem too short or too long.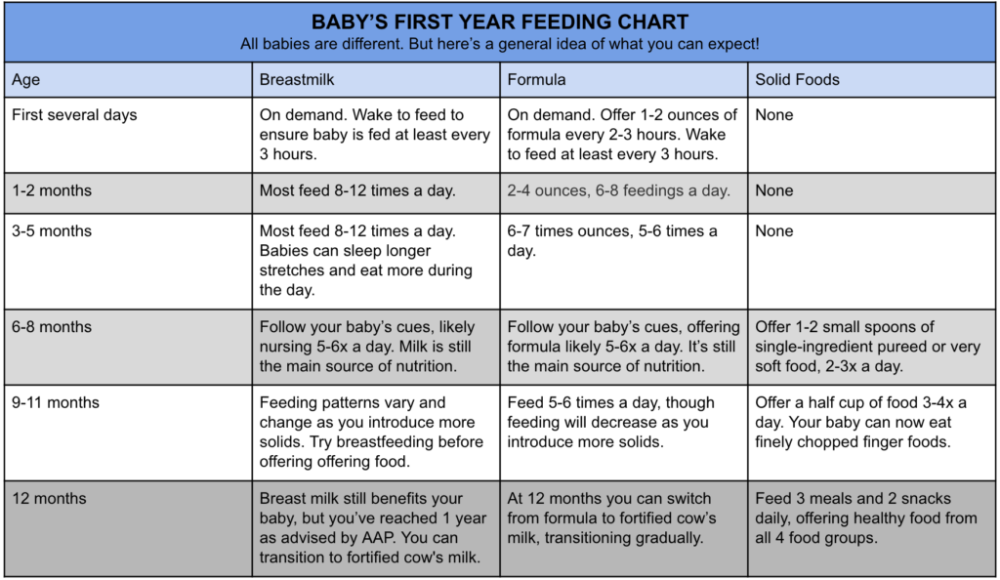
When Should I Alternate Breasts?
Alternate breasts and try to give each one the same amount of nursing time throughout the day. This helps to keep up your milk supply in both breasts and prevents painful engorgement (when your breasts overfill with milk).
You may switch breasts in the middle of each feeding and then alternate which breast you offer first for each feeding. Can't remember where your baby last nursed? It can help to attach a reminder — like a safety pin or small ribbon — to your bra strap so you'll know which breast your baby last nursed on. Then, start with that breast at the next feeding. Or, keep a notebook handy or use a breastfeeding app to keep track of how your baby feeds.
Your baby may like switching breasts at each feeding or prefer to nurse just on one side. If so, then offer the other breast at the next feeding. Do whatever works best and is the most comfortable for you and your baby.
How Often Should I Burp My Baby During Feedings?
After your baby finishes on one side, try burping before switching breasts. Sometimes, the movement alone can be enough to cause a baby to burp.
Sometimes, the movement alone can be enough to cause a baby to burp.
Some infants need more burping, others less, and it can vary from feeding to feeding.
If your baby spits up a lot, try burping more often. While it's normal for infants to "spit up" a small amount after eating or during burping, a baby should not vomit after feeding. If your baby throws up all or most of a feeding, there could be a problem that needs medical care. If you're worried that your baby is spitting up too much, call your doctor.
Why Is My Baby Hungrier Than Usual?
When babies go through a period of rapid growth (called a growth spurt), they want to eat more than usual. These can happen at any time. But in the early months, growth spurts often happen when a baby is:
- 7–14 days old
- 2 months old
- 4 months old
- 6 months old
During these times and whenever your baby seems extra hungry, follow your little one's hunger cues. You may need to breastfeed more often for a while.
How Long Should I Breastfeed My Baby?
That's a personal choice. Experts recommend that babies be breastfed exclusively (without formula, water, juice, non–breast milk, or food) for the first 6 months. Then, breastfeeding can continue until 12 months (and beyond) if it's working for you and your baby.
Breastfeeding has many benefits for mom and baby both. Studies show that breastfeeding can lessen a baby's chances of diarrhea, ear infections, and bacterial meningitis, or make symptoms less severe. Breastfeeding also may protect children from sudden infant death syndrome (SIDS), diabetes, obesity, and asthma.
For moms, breastfeeding burns calories and helps shrink the uterus. In fact, breastfeeding moms might return to their pre–pregnancy shape and weight quicker. Breastfeeding also helps lower a woman's risk of diseases like:
- breast cancer
- high blood pressure
- diabetes
- heart disease
It also might help protect moms from uterine cancer and ovarian cancer.
Termination of breastfeeding | Stopping breastfeeding
When is it time to stop breastfeeding and what is the best way to do it? Read our article for useful practical tips on weaning.
Share this information
How long should breastfeeding continue? Three months? Six? Year? Or maybe a few years?
The World Health Organization (WHO) and other authorities recommend that infants be exclusively breastfed for the first six months and then continue to be breastfed along with other foods (complementary foods) for at least two years. 1
The fact is that breast milk is not just food. It is a natural sedative if the child is anxious or tired. In addition, milk contains immune-boosting components, the amount of which increases dramatically when the baby gets sick. 2
According to anthropologists, the natural age of a person to stop breastfeeding is even more than two years.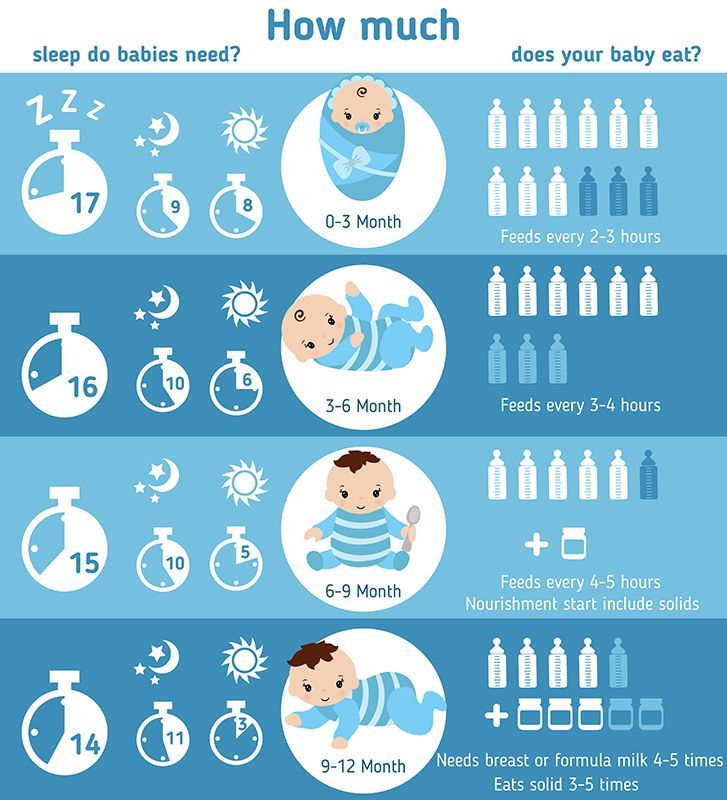 Given factors such as tooth development, body weight, comparison with other primates, and historical evidence, some scientists believe that breastfeeding may last up to two to four years. A number of researchers even believe that our ancestors breastfed children up to six or seven years of age. 3
Given factors such as tooth development, body weight, comparison with other primates, and historical evidence, some scientists believe that breastfeeding may last up to two to four years. A number of researchers even believe that our ancestors breastfed children up to six or seven years of age. 3
Today, more than 60% of mothers in developed countries start giving their babies formula or complementary foods before six months of age, 4 although WHO does not recommend this.
When is it time to stop breastfeeding?
Weaning means that you gradually stop breastfeeding your baby. Ideally, the first step in this process is the gradual introduction of complementary foods, starting at about six months of age. In this case, breastfeeding continues. The weaning process continues until the mother's milk has been completely replaced by other foods and drinks.
“After six months, the baby needs higher doses of certain nutrients, such as iron, zinc, vitamins B and D, that he cannot get from breast milk or from his own reserves,” says Sarah Beeson, health visitor from Great Britain.
“But solid food should at first only supplement the main diet with breast milk and gradually replace it. Mother's milk remains the main source of nutrition for the baby for many months to come.”
On average, a seven-month-old baby gets 93% of its calories from breast milk. And even between the 11th and 16th months, milk provides him with about half of the daily calorie intake. 5
“Sometimes moms think that breastmilk isn't that important once a baby has started solid foods, but the truth is, no matter how many months old a baby is, there's nothing better than your milk,” continues Sarah.
In fact, the process of finishing breastfeeding can take as long as mother and baby want. “When to stop breastfeeding is up to you,” says Sarah. The only thing that matters is what you think is right for you and your child.”
How to wean
Whenever you decide to start weaning your baby, it's best to do it gradually. An abrupt cessation of breastfeeding can lead to lactostasis, blockage of the milk ducts and mastitis, and in a child such a sudden change can adversely affect the state of the digestive and immune systems.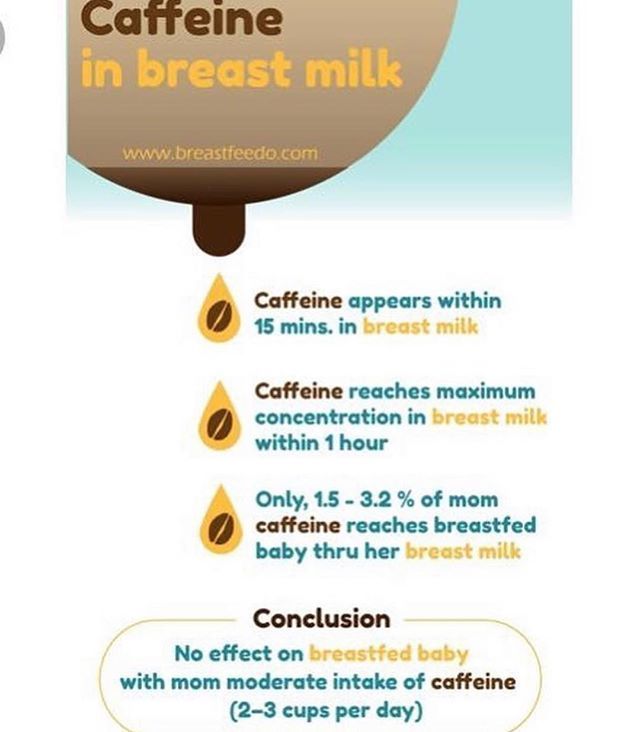 In addition, it will be difficult for both of you psychologically.
In addition, it will be difficult for both of you psychologically.
When should I stop breastfeeding?
Sometimes mothers mistakenly believe that it is time to stop breastfeeding, when in fact there is no reason to. If you're returning to work, breastfeeding can be a great way to stay close to your baby during this difficult time for both of you. You can express milk at work, and morning and evening feeding sessions will give you the opportunity to spend time alone with your baby. If you need to leave without your baby, you can also express milk and bring or send it home.
If you get sick, this is not always a reason to stop breastfeeding. Read our advice in the article on breastfeeding when sick and consult with your healthcare professional.
Weaning up to six months
If you cannot continue breastfeeding until six months and want to try weaning your baby, start by replacing one feeding a day with a bottle of formula.
“It's best to start with midday feedings.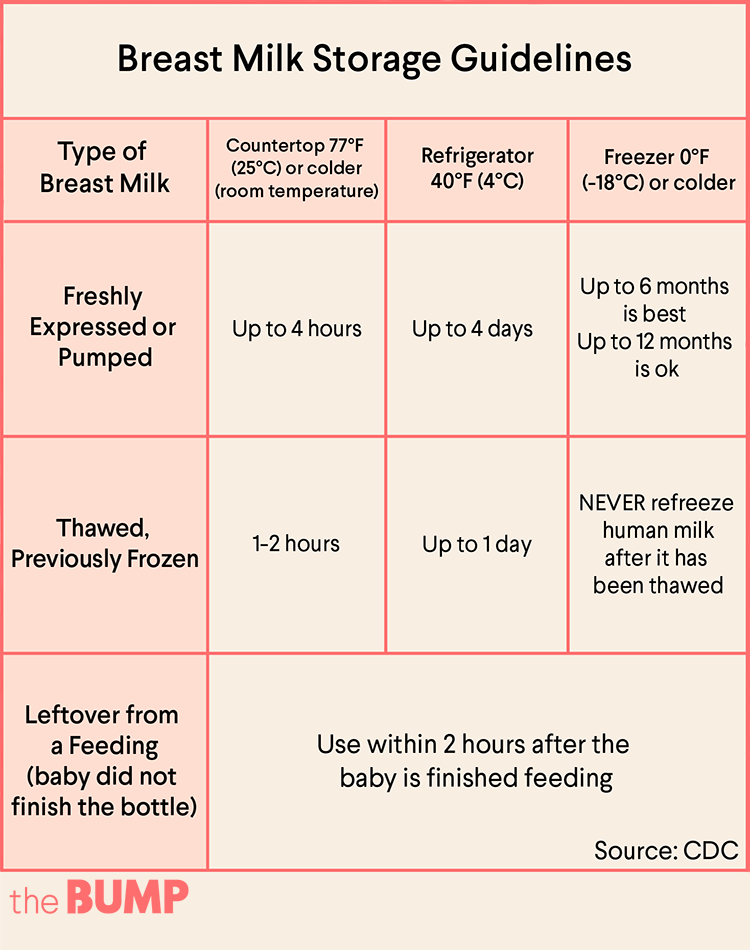 Babies are very alert and able to smell breast milk nearby, so ask your partner or relative to give your baby a bottle when you're in the other room,” Sarah advises.
Babies are very alert and able to smell breast milk nearby, so ask your partner or relative to give your baby a bottle when you're in the other room,” Sarah advises.
“Be hygienic when preparing meals. Be prepared for the fact that the baby will take fewer servings of expressed milk per day than if he was fed directly from the breast. Don't make him eat more milk than he wants."
You will probably feel that your breasts are fuller and more tender. This is due to the fact that your body is rebuilding to produce less milk. If this creates discomfort, try expressing some milk—just enough to relieve the discomfort without stimulating extra production.
When your body adjusts to the new volume - usually after a few days - replace with formula for one more meal a day. Continue this until you have changed all feedings and your baby is completely weaned.
“I had complications after my first birth, as a result I lost a lot of weight very quickly, and besides, I developed mastitis. Lactation was very weak, and at three months I was forced to stop breastfeeding,” recalls Jennifer, a mother of two from the UK, “I gradually replaced one feeding, so physically it was easy, but mentally it was hard for me.”
Lactation was very weak, and at three months I was forced to stop breastfeeding,” recalls Jennifer, a mother of two from the UK, “I gradually replaced one feeding, so physically it was easy, but mentally it was hard for me.”
If you want to maintain closeness with your baby and all the health benefits of breastfeeding, but still need to cut down on breastfeeding, try partial weaning, replacing only a few feeds a day with formula.
Weaning after six months
Once your baby starts eating solid foods (about six months old), you will notice that breastfeeding naturally occurs less and less. For a year, it can be reduced to just a couple of times a day, and feedings will be replaced by full meals and healthy snacks.
Anyway, if you intend to continue to reduce breastfeeding, do it gradually, replacing one feeding at a time. Use formula milk if your baby is under 12 months old. With cow's milk, you should wait at least up to a year.
“When I decided to wean my son, I breastfed him three times a day and gave him other foods three times plus light snacks.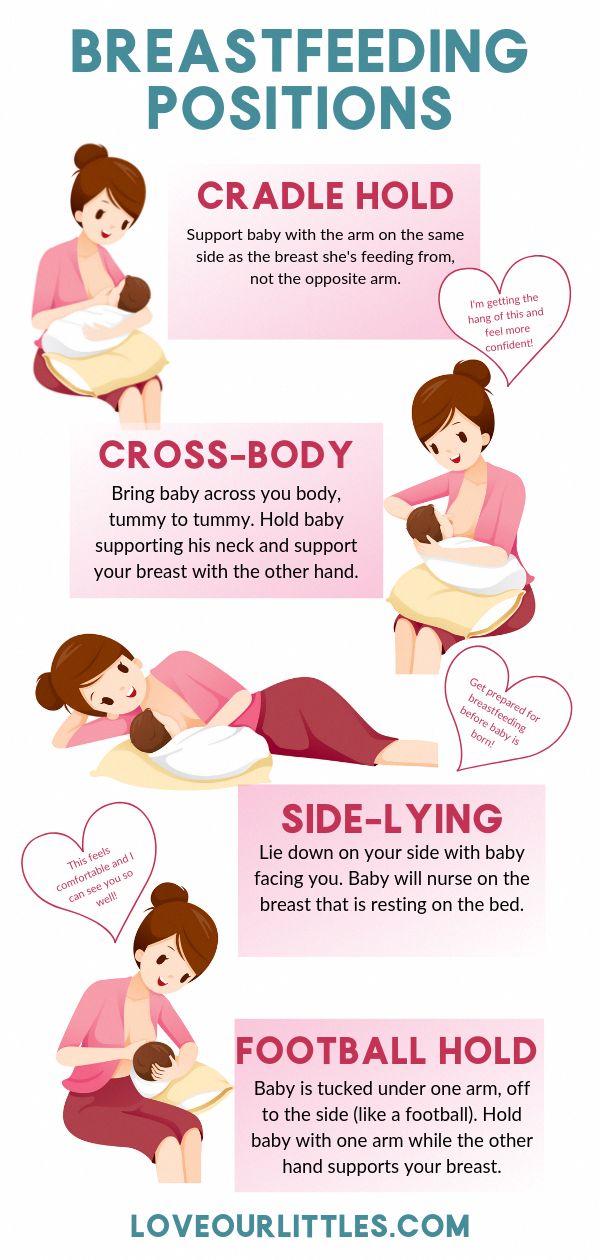 Gradually, I replaced all breastfeedings with formula. By 11 months, we only had one nighttime breastfeed left,” says Ruth, a UK mom.
Gradually, I replaced all breastfeedings with formula. By 11 months, we only had one nighttime breastfeed left,” says Ruth, a UK mom.
There are various ways to distract a child from changes in his diet. Some mothers suggest that instead of breastfeeding something to drink and eat together to maintain a sense of closeness. You can also change your daily routine, play your favorite game, or replace feeding with caresses - from you or from your partner. Some children take longer to get used to the new food, but in the end everything falls into place. If you are having difficulty weaning, ask your healthcare provider for advice.
Ending breastfeeding naturally
Ending breastfeeding can be guided by the baby's wishes. This is called baby-initiated weaning, or the natural termination of breastfeeding. Such a process is likely to be long and gradual. Month after month, feeding sessions will become shorter and less frequent, until one day the child completely loses interest in the breast.
“My daughter stopped breastfeeding on her own when she was four years old,” says Sarah, a mother from the UK. And once, when we were on vacation, she seemed to just forget about her breasts. Now, six months later, she sometimes still asks for breasts, but she already knows that there is no milk there.
You will have a huge amount of time for the body to adapt, so there should be no discomfort or swelling of the breast. However, you may find it difficult emotionally, so spend more time petting and bonding with your baby.
“Child-initiated termination of breastfeeding was right for me because I never gave my son formula or a bottle. I didn’t want to abruptly stop feeding and refuse him,” recalls Kelly, a mother from the UK, “He himself lost interest in breasts at the age of two and a half years. For us, it was the best scenario, although emotionally it was not very easy for me.”
What if you need to stop breastfeeding quickly?
It is best not to stop breastfeeding abruptly, but sometimes it is necessary for medical reasons or because you cannot be near the baby.
If you have been breastfeeding your baby up to this point, you will most likely have to express your milk to avoid breast swelling. Some mothers prefer to use a breast pump for this, others find it easier to express milk manually. You only need to pump a little, just to eliminate the discomfort, otherwise your body will take it as a signal to produce more milk.
At first, the breasts may swell and become tender, but this will pass. Breast milk contains a so-called feedback lactation inhibitor. When breastfeeding is stopped, this inhibitor tells your body to slow down milk production, but it can take days or even weeks for your breasts to rebuild.
Certain medications can relieve pain and should be discussed with your doctor. Always follow your pharmacist's instructions or directions, and consult your healthcare professional before taking any medication.
“I had to abruptly stop breastfeeding when my daughter was eight months old because she had to take strong painkillers,” says Peggy, a mother from Switzerland. “It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
“It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
Can I continue breastfeeding if I want to get pregnant again?
Breastfeeding is a natural contraceptive. However, this method is not the most reliable, especially after six months or if you are not exclusively breastfeeding. This means that you can get pregnant even while you are breastfeeding.
Pregnant and breastfeeding mothers sometimes receive conflicting advice about whether to stop breastfeeding. Consistent feeding of two children of different ages is of course possible, and with the advent of the second baby, your body will produce the kind of milk that both of them need.
It is not uncommon for an older child to refuse to breastfeed or skip feedings if the mother is pregnant. This may be due to changes in milk composition that occur during pregnancy. Milk can change the taste and become less sweet. 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Milk can change the taste and become less sweet. 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Talk to your doctor if you want to continue breastfeeding during pregnancy, but have had a preterm birth or miscarriage, or have any bleeding in the past.
If you need medical help to conceive, certain drugs and procedures may not be suitable while you are breastfeeding. Discuss all possible options before deciding to stop breastfeeding.
And finally...
Whenever you decide to end breastfeeding, and whatever method you choose to do so, be kind to yourself and your baby. This is a huge change for both of you physically, hormonally, and emotionally, so proceed thoughtfully and carefully.
“Although my body responded normally to stopping breastfeeding, it was psychologically difficult for me. The thing that united us for so long is over, - Jane, a mother of two children from the USA, shares her impressions, - I worked long hours, five days a week, and breastfeeding made me feel that I occupy a special place in the lives of children. But when it stopped, we soon found other ways to be together.”
But when it stopped, we soon found other ways to be together.”
Literature
1 World Health Organization. [Internet] Health Topics: Breastfeeding: 2018 [Accessed: 02/08/2018]. Available from : http://www.who.int/topics/breastfeeding/en - World Health Organization. "Health Issues: Breastfeeding" [Internet]. Geneva, Switzerland: WHO; 2018 [Visit 02/08/2018]. Article linked: http://www.who.int/topics/breastfeeding/e
2 Hassiotou et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
3 Dettwyler KA. When to wean: biological versus cultural perspectives. Clin Obstet Gynecol . 2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
4 Victora CG Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
5 Dewey KG et al. Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr . 1984;3(5):713-720. — Dewey C.G. et al., "Amount and composition of breast milk in late lactation (7-20 months)". F Pediatrician Gastroenterol Nutr. 1984;3(5):713-720.
6 Prosser CG et al. Mammary gland function during gradual weaning and early gestation in women. Aust J Exp Biol Med 9021 9029 Sci. 1984;62( Pt 2):215-228. - Prosser S.G. et al., "Breast Function During Gradual Weaning and Early Gestation." Aust J Exp Biol Med Sai. 1984;62( Pt 2):215-228.
Aust J Exp Biol Med 9021 9029 Sci. 1984;62( Pt 2):215-228. - Prosser S.G. et al., "Breast Function During Gradual Weaning and Early Gestation." Aust J Exp Biol Med Sai. 1984;62( Pt 2):215-228.
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.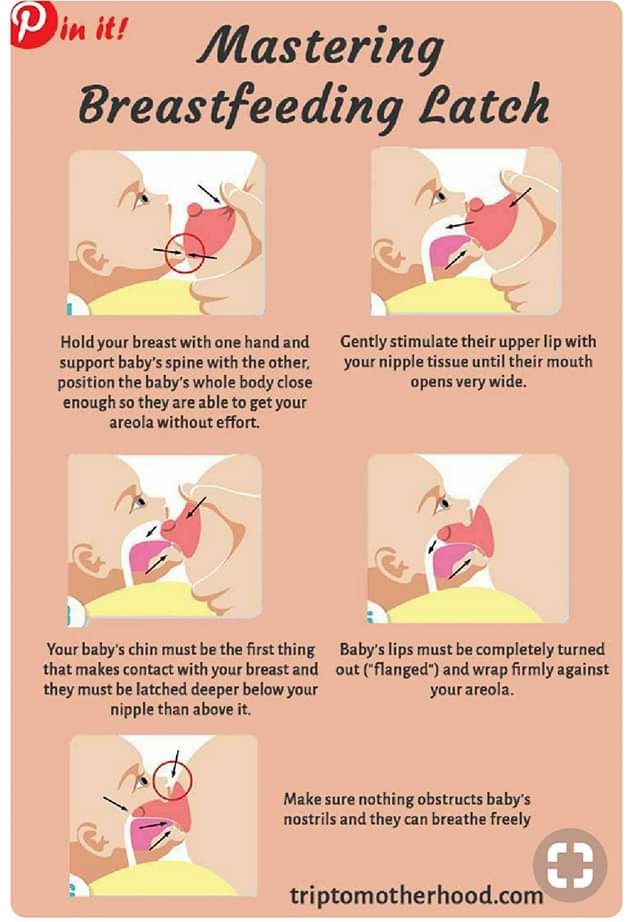
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly as milk production increases: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large hen's egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger.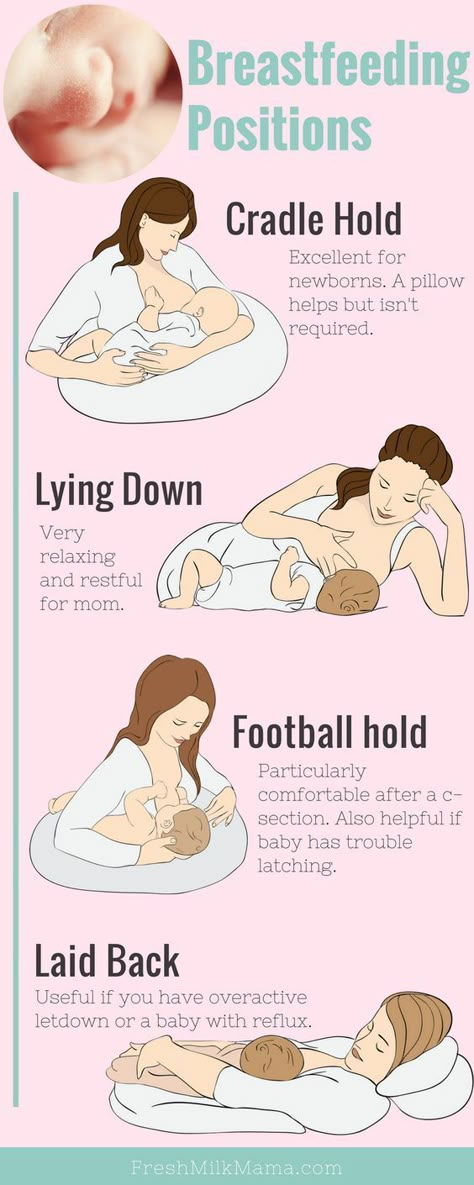 Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
What is a "milk flush"?
At the beginning of each feed, a hungry baby actively suckles the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it.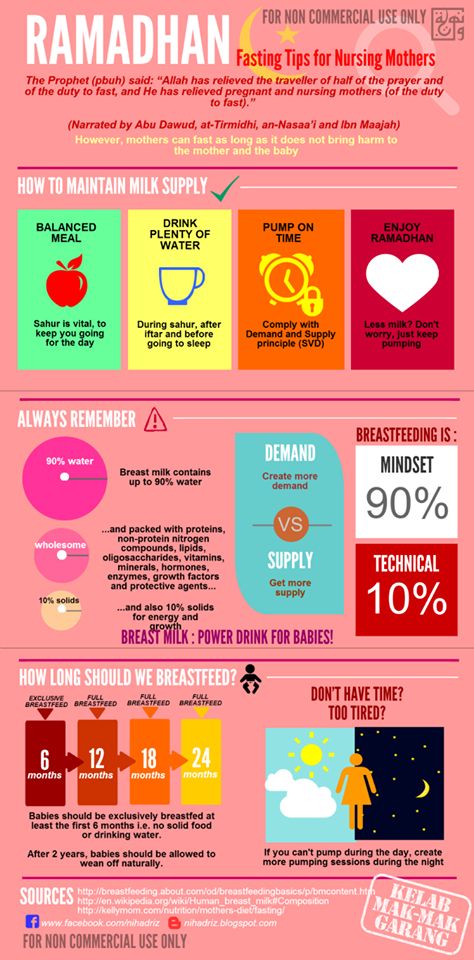 But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has had enough, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more.”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%.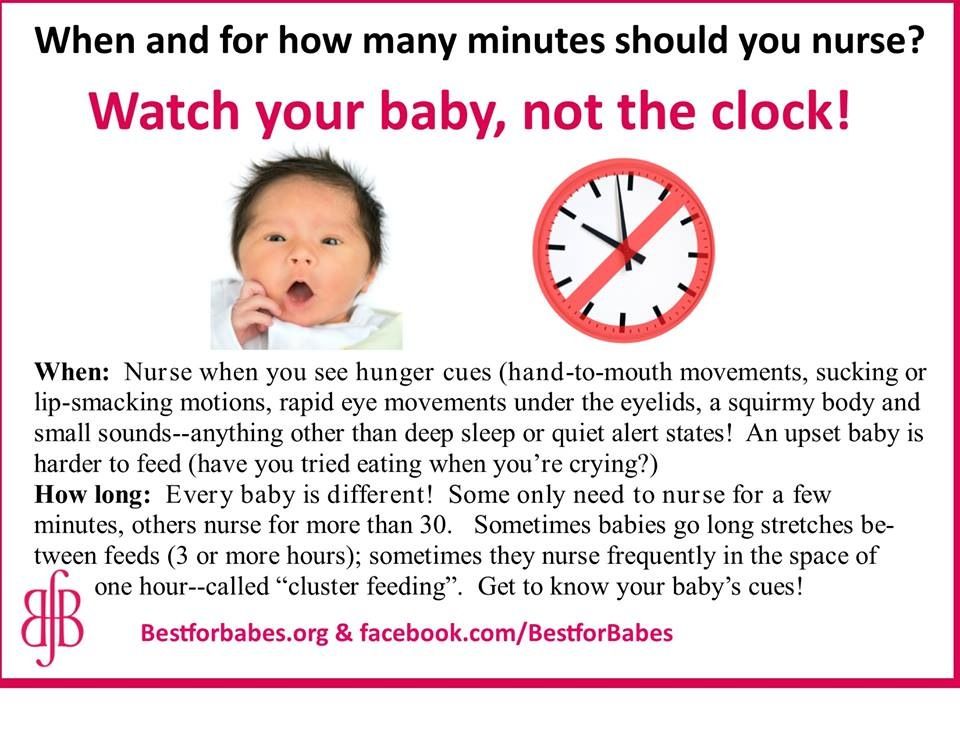 One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks for a breast very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, just when many babies are especially restless and need close contact with their mother.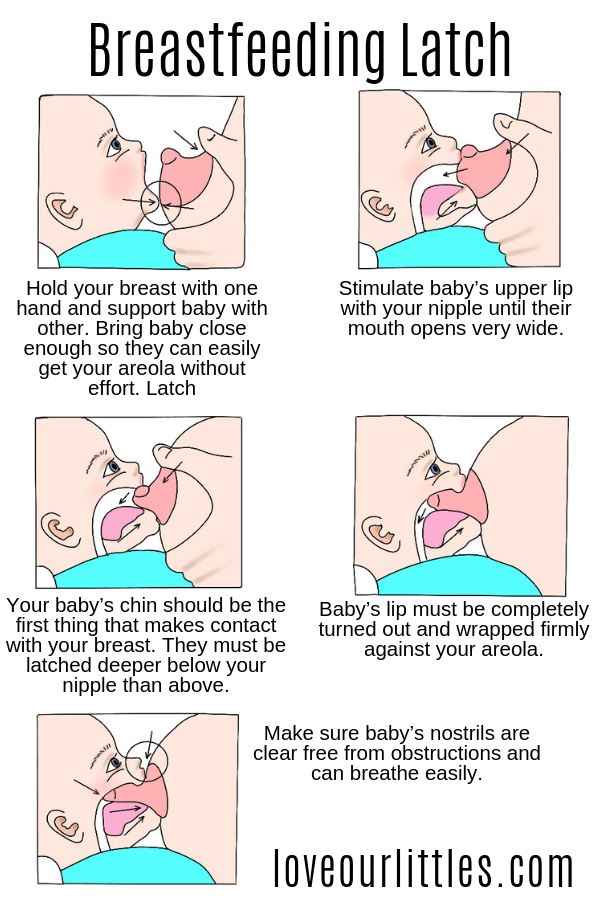 Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“Nobody told me about cluster feeding, so for the first 10 days I just went crazy with anxiety - I was sure that my milk was not enough for the baby,” recalls Camilla, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.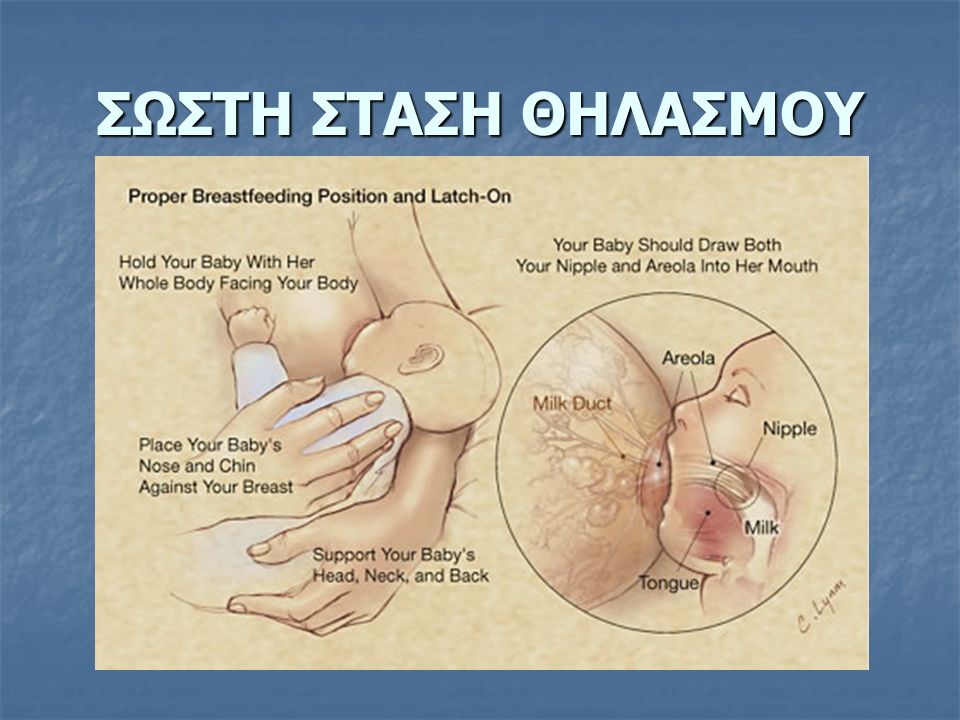
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will start to subside.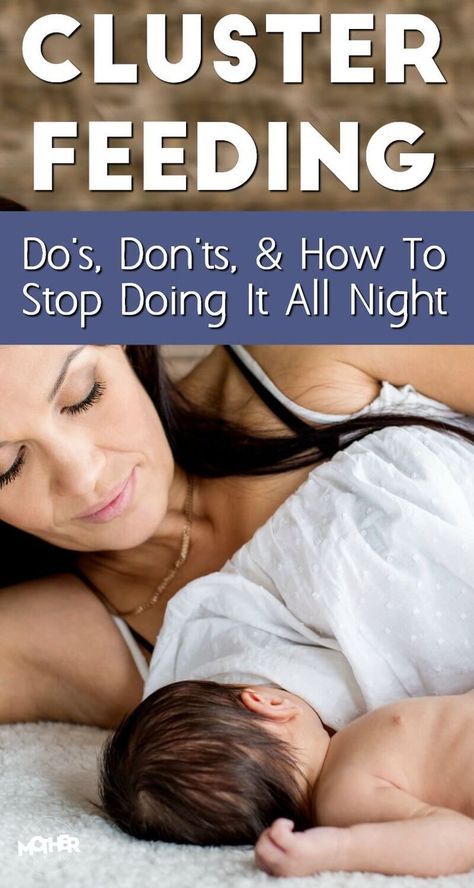
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11-13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” advises Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding beyond the first month: what to expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al. , Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
, Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation . Am J Clinl Nutr . 1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Association [ Internet ].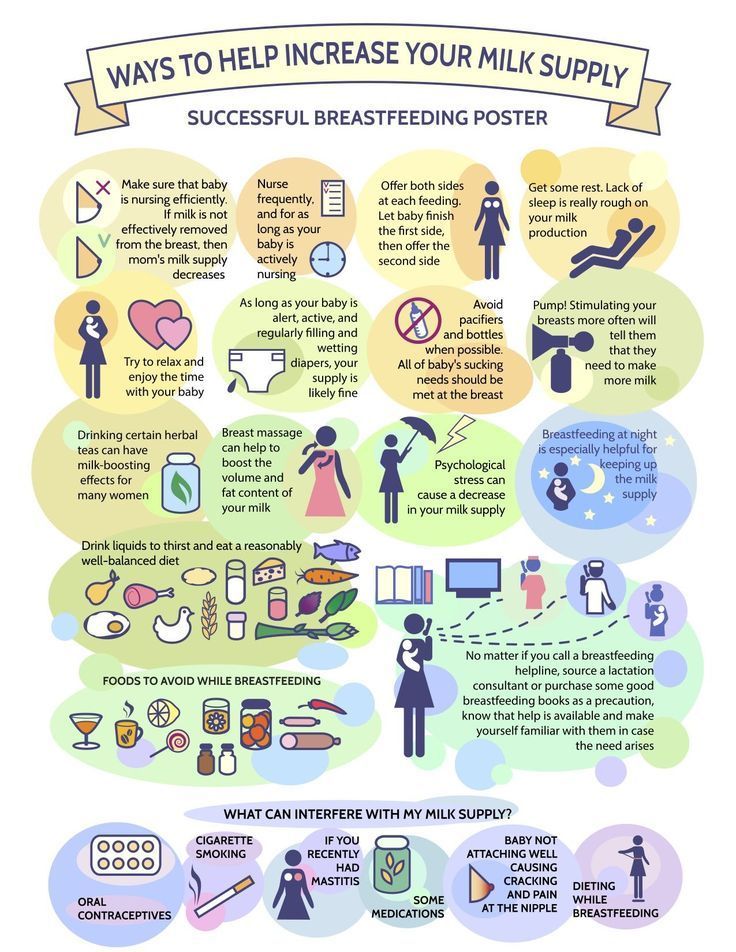 Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day.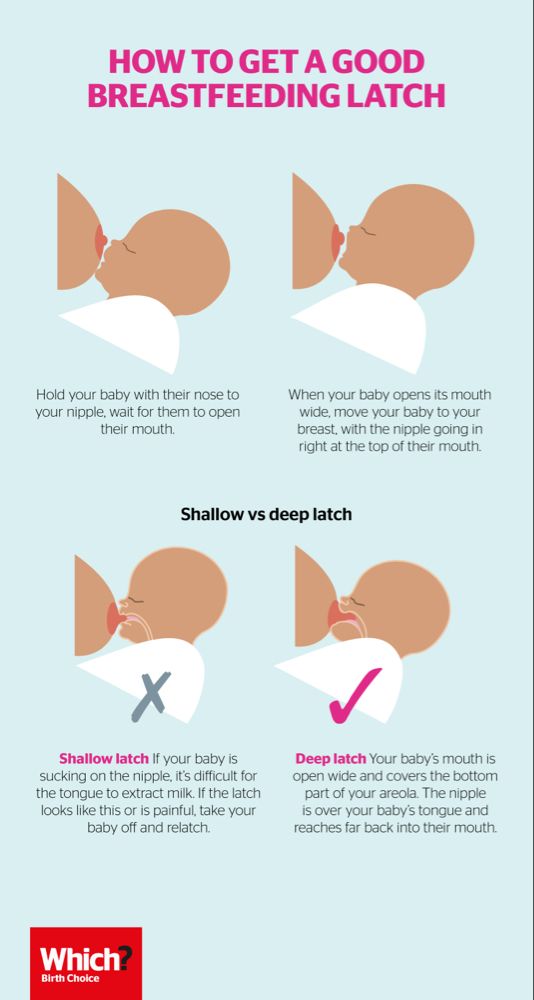 " Pediatrix (Pediatrics). 2006;117(3):e387-95.
" Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].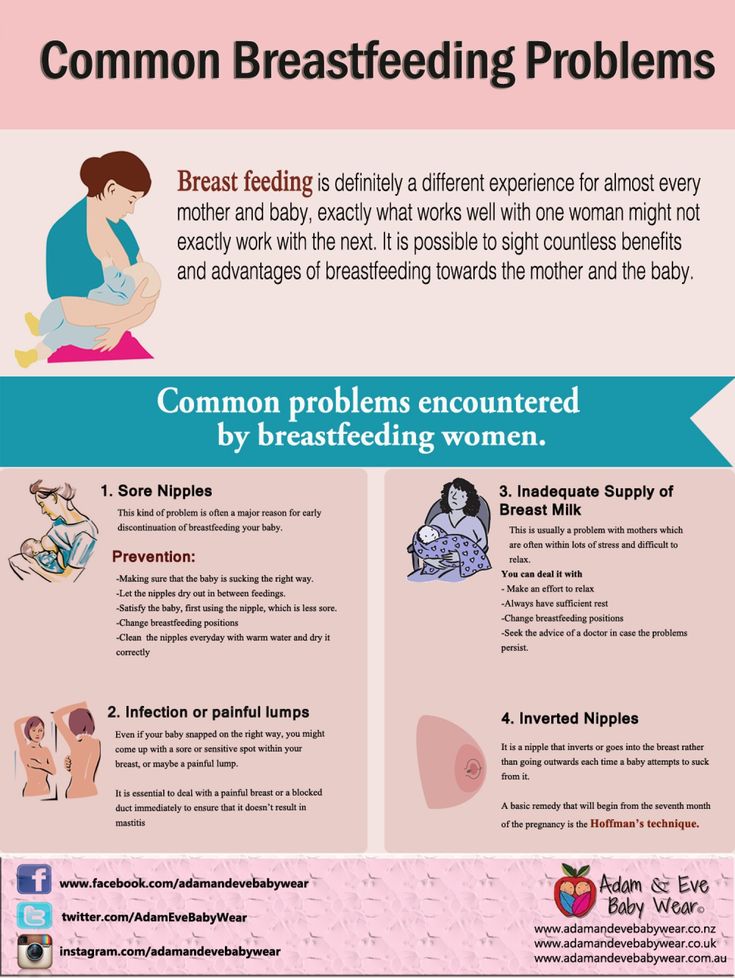
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev .