How long to keep baby upright after feed reflux
Management tips - Reflux Infants Support Association Inc
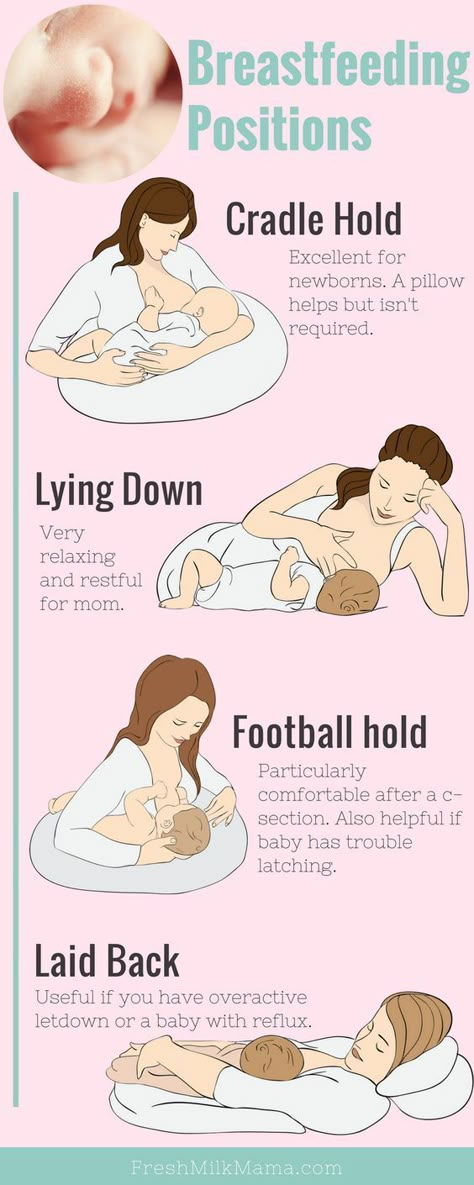
- Feed your baby while they are upright. Keep their body straight with their head higher than their stomach.
- Try to keep your baby upright for at least 30 minutes after a feed. Try to avoid the upright seated position during this time as this position can increase pressure in the abdomen and trigger reflux.
- Avoid placing your infant flat on their back immediately following a feed.
- Avoid exposure to tobacco smoke.
- Avoid overfeeding – if your baby vomits, wait until the next feeding rather than feeding them again. (Check with the doctor or Child Health Nurse that their intake is appropriate)
- Consider offering your baby a dummy (or your clean finger) if you are comfortable with the idea; the swallowing action may help your baby to settle. Talk to your child health nurse if you have any concerns.
- Avoid rough handling or bouncing your baby (you may need to remind family and friends of this).
- Use products to help keep baby upright or help calm them, such as an automatic baby swing, bouncer and/or baby hammock as suitable. (Important: Never leave them unattended or let them fall asleep unsupervised in these devices as they are not designed as sleeping products.)
- If possible, change your baby’s nappy before a feed rather than after, as reflux is more likely to occur with a full tummy. Take care to avoid lifting baby’s legs too high to change a nappy; try rolling your baby to the side instead.
- Avoid any tight clothing around their waist such as tight nappies or elastic waistbands.
- Thickened feeds (AR formulas or infant formulas thickened with commercial thickening agents) may be effective for some reflux babies, especially those who vomit. Discuss this option with your child’s doctor first.
- If a food allergy or intolerance is suspected, a two week trial of hypoallergenic formula can be helpful if your baby is formula-fed.
 If you are breastfeeding, you may choose to eliminate specific foods e.g. cow’s milk and soy from your diet (with medical supervision). Consider the possibility of food allergy or intolerance in older children as well. Seek medical advice regarding this. Do not change your child’s diet before seeking medical advice. Talk to a dietitian.
If you are breastfeeding, you may choose to eliminate specific foods e.g. cow’s milk and soy from your diet (with medical supervision). Consider the possibility of food allergy or intolerance in older children as well. Seek medical advice regarding this. Do not change your child’s diet before seeking medical advice. Talk to a dietitian. - Burp baby frequently during the feeds (as tolerated) e.g. after finishing each side in a breastfed baby, and after every 30-60ml in a bottle-fed baby.
- Try feeding smaller amounts slightly more frequently (unless this upsets baby). Frequent large feeds can trigger reflux.
- Massage can be soothing to babies and children, and it can also aid digestion. Learn how to massage your baby/child so they get the most out of it.
- Minimise foods and drinks if they cause irritation or increase the risk of reflux. Examples of these may be spicy foods, citrus fruits, tomatoes and other acidic food, fatty foods and caffeine
- If your baby is under 12 months of age, elevating the head of the bed to treat reflux is not supported by evidence from research studies.
 It may be helpful in reducing episodes of reflux in a child who is over the age of 12 months.
It may be helpful in reducing episodes of reflux in a child who is over the age of 12 months. - For children over the age of 2 years, adapt the management strategies to suit e.g. avoid lying down for several hours after meals, eat smaller meals more often etc. You may also like to encourage them to avoid large meals before exercise or stressful events such as exams; and avoid or minimise caffeine.
- Encourage older children to find a comfortable sleeping position. Sleeping on the tummy or left side may be helpful.
- Older children/teenagers may consider using sugar-free chewing gum after meals, as it may reduce acid reflux and help clear acid from the oesophagus.
Additional suggestions from RISA members “Go for a walk outside if you can – the screaming never seems quite so loud in the great outdoors.” “Put your answering machine on/take the phone off the hook when you get a chance to rest.” “Invest in a portable phone if possible.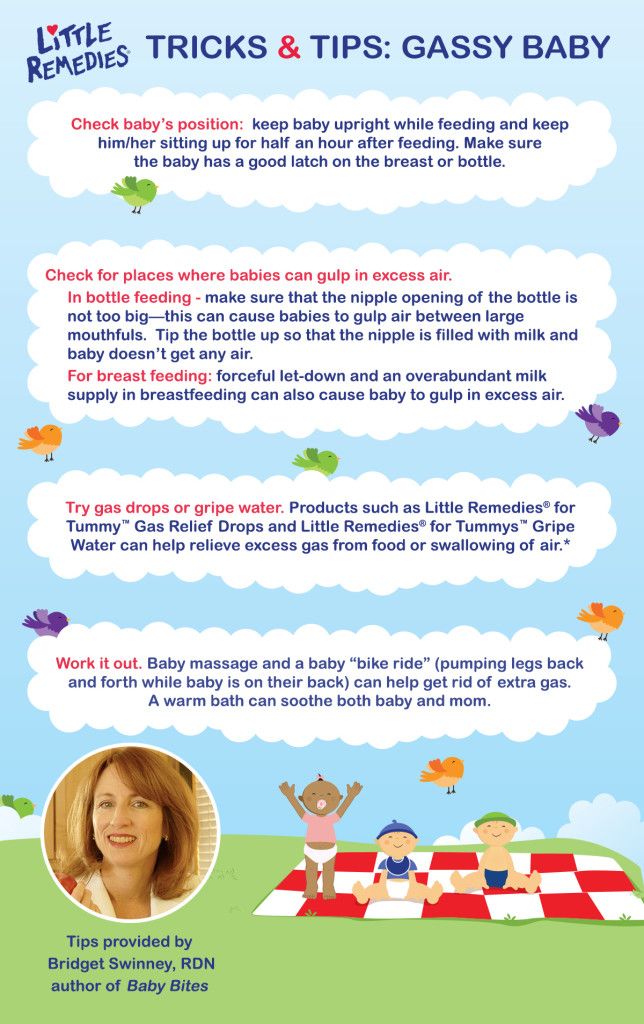 This allows you to keep in touch with friends and family whilst still attending to your baby’s needs. It is also perfect to keep beside you during baby feeding times, as the phone almost always rings after you get settled.”
This allows you to keep in touch with friends and family whilst still attending to your baby’s needs. It is also perfect to keep beside you during baby feeding times, as the phone almost always rings after you get settled.”
© Written by RISA Inc, revised by Glenda Blanch, RISA Inc member and author of “Reflux Reality: A Guide for Families” 2010
References BabyCentre UK Medical Advisory Board. (2008, January). Caffeine and pregnancy: what’s safe? Retrieved April 19, 2008, from Baby Centre UK: www.babycenter.com.au/pregnancy/nutrition/foodsafety/caffeine/ CDHNF. (2007, September 24). Pediatric Gastroesophageal Reflux Evaluation and Management. Retrieved April 28, 2008, from Children’s Digestive Health and Nutrition Foundation: http://gerd.cdhnf.org/User/Docs/PDF/Slides/GERD_Core_Set_1_Hour.pdf CDHNF. (2007). Pediatric GERD. What’s Up With My Kid’s Stomach? Retrieved April 2, 2008, from Children’s Digestive Health and Nutrition Foundation: http://gerd.cdhnf.org/cms/en/PatientsAndFamilies/Kids/Patients_Kids_Landing.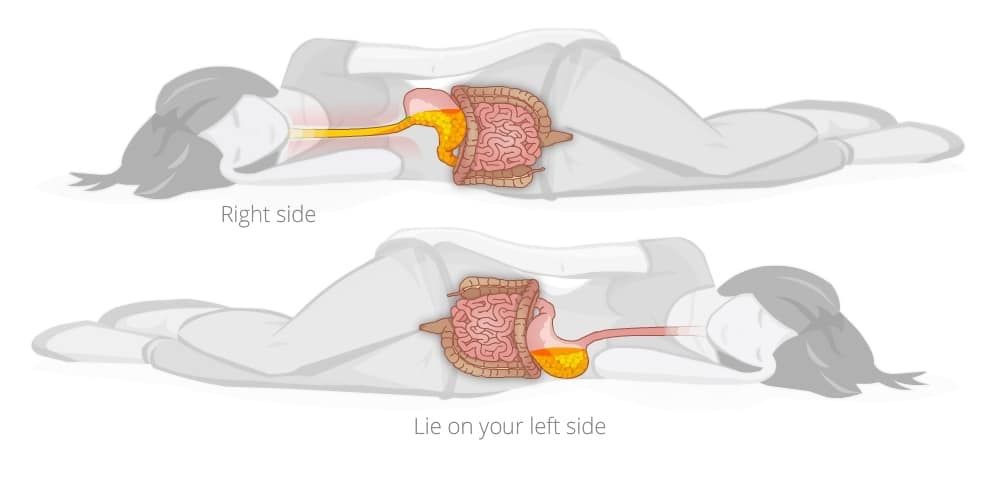 aspx?menu=patientskids CDHNF. (2006, March 9). Teen’s Checklist for GER or GERD. Retrieved April 30, 2008, from Children’s Digestive Health & Nutrition Foundation: http://gerd.cdhnf.org/User/Docs/pdf/GERDTeenChecklist.pdf Craig, W. R., Hanlon-Dearman, A., Sinclair, C., Taback, S., & Moffatt, M. (2004). Metoclopramide, thickened feedings, and positioning for gastro-oesophageal reflux in children under two years (Review). Cochrane Database of Systematic Reviews (3), Issue 3. Art. No.: CD003502. DOI:10.1002/14651858.CD003502.pub2 Harnsberger, J. K. (2008). Management Algorithm #2: Management of a Child or Adolescent With Chronic Heartburn. Retrieved April 2, 2008, from Medscape Pediatrics: http://www.medscape.com/viewarticle/494079_12 Henry, S. M. (2004). Discerning Differences: Gastroesophageal Reflux and Gastroesophageal Reflux Disease in Infants. Advances in Neonatal Care , 4 (4), 235-247 McLoughlin, H. (2008). How To Use Infant Massage to Relieve Reflux. Retrieved June 20, 2009, from How to Do Things: www.
aspx?menu=patientskids CDHNF. (2006, March 9). Teen’s Checklist for GER or GERD. Retrieved April 30, 2008, from Children’s Digestive Health & Nutrition Foundation: http://gerd.cdhnf.org/User/Docs/pdf/GERDTeenChecklist.pdf Craig, W. R., Hanlon-Dearman, A., Sinclair, C., Taback, S., & Moffatt, M. (2004). Metoclopramide, thickened feedings, and positioning for gastro-oesophageal reflux in children under two years (Review). Cochrane Database of Systematic Reviews (3), Issue 3. Art. No.: CD003502. DOI:10.1002/14651858.CD003502.pub2 Harnsberger, J. K. (2008). Management Algorithm #2: Management of a Child or Adolescent With Chronic Heartburn. Retrieved April 2, 2008, from Medscape Pediatrics: http://www.medscape.com/viewarticle/494079_12 Henry, S. M. (2004). Discerning Differences: Gastroesophageal Reflux and Gastroesophageal Reflux Disease in Infants. Advances in Neonatal Care , 4 (4), 235-247 McLoughlin, H. (2008). How To Use Infant Massage to Relieve Reflux. Retrieved June 20, 2009, from How to Do Things: www.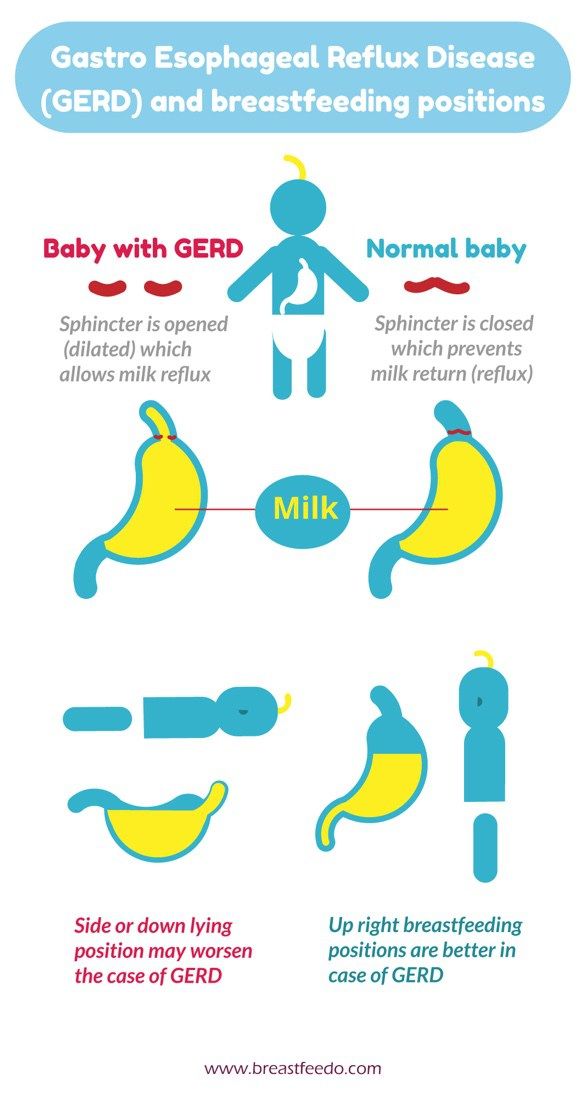 howtodothings.com/family-relationships/how-to-use-infant-massage-to-relieve-reflux Nielsen, R. G., Bindslev-Jensen, C., Kruse-Andersen, S., & Husby, S. (2004). Severe Gastroesophageal Reflux Disease and Cow Milk Hypersensitivity in Infants and Children: Disease Association and Evaluation of a New Challenge Procedure. Journal of Pediatric Gastroenterology and Nutrition , 39, 383 – 391 Schwarz, S. M., & Hebra, A. (2009, May 13). Gastroesophageal Reflux. Retrieved August 26, 2009, from eMedicine: http://emedicine.medscape.com/article/930029-print Van Niel, C. W. (2008, March 12). Treat Babies with Reflux Conservatively. Retrieved March 31, 2008, from Journal Watch Pediatrics and Adolescent Medicine : http://pediatrics.jwatch.org/cgi/content/full/2008/312/4 Vandenplas, Y., & Sacré, L. (1987). Milk-Thickening Agents as a Treatment for Gastroesophageal Reflux. Clinical Pediatrics , 26 (2), 66-4 Vandenplas, Y., Rudolph, C. D., Di Lorenzo, C., Hassall, E., Liptak, G., Mazur, L., et al.
howtodothings.com/family-relationships/how-to-use-infant-massage-to-relieve-reflux Nielsen, R. G., Bindslev-Jensen, C., Kruse-Andersen, S., & Husby, S. (2004). Severe Gastroesophageal Reflux Disease and Cow Milk Hypersensitivity in Infants and Children: Disease Association and Evaluation of a New Challenge Procedure. Journal of Pediatric Gastroenterology and Nutrition , 39, 383 – 391 Schwarz, S. M., & Hebra, A. (2009, May 13). Gastroesophageal Reflux. Retrieved August 26, 2009, from eMedicine: http://emedicine.medscape.com/article/930029-print Van Niel, C. W. (2008, March 12). Treat Babies with Reflux Conservatively. Retrieved March 31, 2008, from Journal Watch Pediatrics and Adolescent Medicine : http://pediatrics.jwatch.org/cgi/content/full/2008/312/4 Vandenplas, Y., & Sacré, L. (1987). Milk-Thickening Agents as a Treatment for Gastroesophageal Reflux. Clinical Pediatrics , 26 (2), 66-4 Vandenplas, Y., Rudolph, C. D., Di Lorenzo, C., Hassall, E., Liptak, G., Mazur, L., et al. (2009). Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of NASPGHAN and ESPGHAN. Journal of Pediatric Gastroenterology and Nutrition , 49 (4), 498-547 von Schönfeld, JV et al 1997, ‘Oesophageal acid and salivary secretion: Is chewing gum a treatment option for gastro-oesophageal reflux?’, Digestion, vol. 58:2, pp. 111-114, viewed 21 July 2008
(2009). Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of NASPGHAN and ESPGHAN. Journal of Pediatric Gastroenterology and Nutrition , 49 (4), 498-547 von Schönfeld, JV et al 1997, ‘Oesophageal acid and salivary secretion: Is chewing gum a treatment option for gastro-oesophageal reflux?’, Digestion, vol. 58:2, pp. 111-114, viewed 21 July 2008
How to Feed a Baby With Reflux – bökee
We know spit up down the front of your shirt isn’t your best look, but for many new moms, it’s a rite of passage. You finally just go with it because changing would mean even more laundry added to the ever-growing pile of burp cloths. But the truth is that changing the way you feed your baby can actually reduce or eliminate their uncomfortable reflux that’s causing all that spit-up.
Even though young babies’ immature digestive systems make them prime candidates for reflux, there are several feeding strategies we suggest to improve it. Not only does reflux cause spit-up, but it can also cause your baby a lot of discomfort, and we know more than anything you want your baby to feel good.
You’ll first want to identify if your baby is experiencing reflux and what might be causing it. Then we’ll give you our top tips to get your baby’s tummy back on track (and your shirts back to pristine condition.)
What is acid reflux in babies?When a baby drinks breast milk or formula, it has a tendency to back up from her stomach. This is referred to as reflux, or gastroesophageal reflux (GER). Reflux is most common during the newborn stage (0-4 months) and improves as time goes on.
According to the Mayo Clinic, this is because an infant’s ring of muscle between the esophagus and the stomach is not fully mature, allowing the contents of the stomach to flow backward.
So how do you know if your baby has reflux?
How to Identify Acid Reflux or GER in Your BabyMild reflux in young babies is common. According to Medline Plus, “About half of all babies spit up many times a day in the first 3 months of their lives.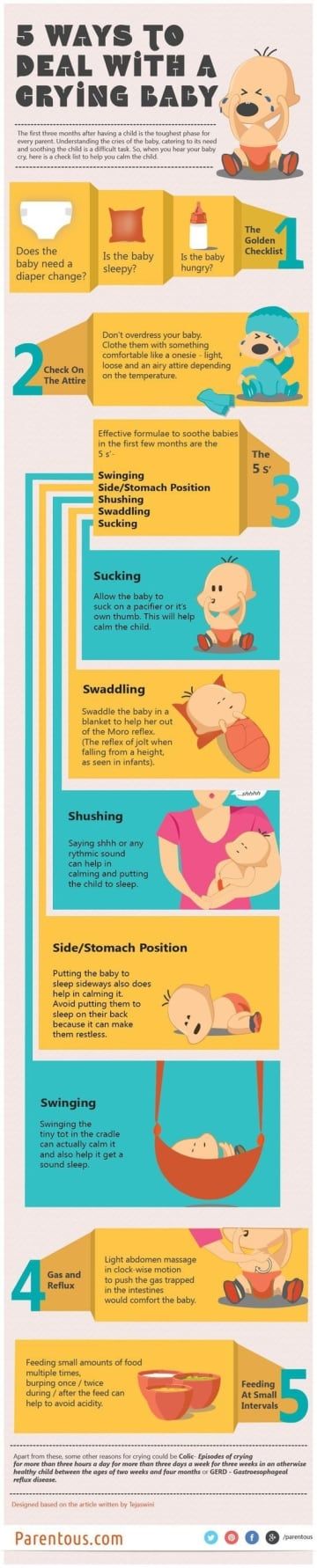 ”
”
And even more will spit up about once or twice per day. In other words, it’s generally not a condition to be concerned about (and it’s temporary.)
Usually most parents just take the spitting up in stride if their baby seems comfortable and happy. In these cases, it’s mostly a nuisance to you while they could care less!
But there are also babies who may experience gas along with their reflux making them pretty uncomfortable or they might have what is called “silent reflux.”
Whereas a baby who spits up will usually feel instantly better, a baby experiencing silent reflux will likely be in pain. This is because the acid will come up the throat, but then they swallow it back down.
If you have a baby showing the following symptoms, they’re likely suffering from one of the types of reflux:
- Frequent spit-ups
- Arching body during or after feeding
- Crying when laid on their back
- Inconsolable crying after feeding (but could also be hours later)
- Pulling legs up
- Trouble sleeping
If your baby is under 4 months and growing well, you don’t need to be concerned about your baby’s reflux. But even though you don’t need to be “concerned,” it's still stressful when you feel like your baby isn't feeling their best but you can't help them.
But even though you don’t need to be “concerned,” it's still stressful when you feel like your baby isn't feeling their best but you can't help them.
Identifying your baby’s symptoms as reflux is the first step to fixing it. Knowing what causes it helps, too. That's when you’ll be able to utilize our tips to help your baby feel their best (while keeping the spit up to a minimum.)
Cause of Reflux in BabiesThe cause of reflux in a young baby is pretty straightforward. It’s really not about anything you’re doing wrong, instead, you just have a tiny little human on your hands whose digestive system is still maturing.
Other than that, the fact that babies lie on their backs so often and are on a completely liquid diet make them susceptible to reflux symptoms. Premature babies, especially, have a hard time.
This all sounds pretty standard, right? And the fact that your baby is on a 100% liquid diet is out of your control. Luckily, there are some easy strategies that you can start implementing today that will improve your baby’s reflux or even eliminate it altogether.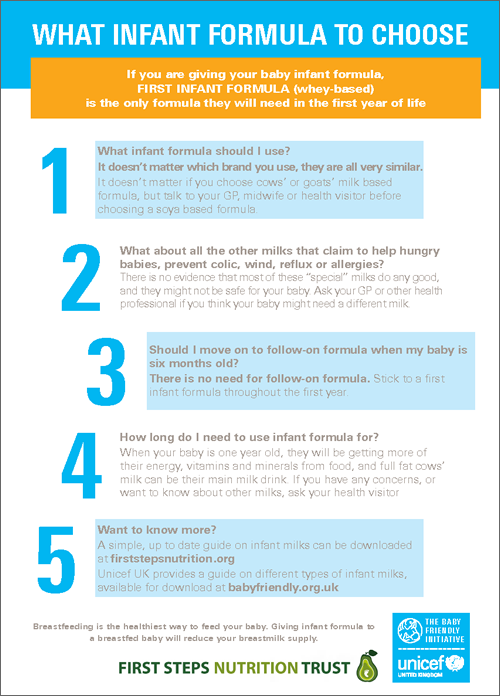
We at bökee are all parents. Though we can’t say necessarily that we’ve experienced it all, we’ve certainly experienced a lot raising babies. What we do know is that no two are alike and what works perfectly for your first baby will surely be the one thing that doesn’t work with the next. With that said, we suggest giving these different strategies a shot in order to help your baby through their reflux.
1.) Try Paced Bottle Feeding
If you bottle feed, implementing paced bottle feeding is a good place to start.
In a nutshell, paced bottle feeding utilizes the following:
- A slow-flow nipple
- An upright feeding position
- Only 20-30 seconds of continuous feeding and then pull the bottle back to give your baby a break
With paced bottle feeding, you slow down a bottle-feed in order to better mimic typical breastfeeding patterns. “Paced feeding reduces the risk of overfeeding that may result in discomfort to the baby,” writes the Minnesota Department of Health.
In our article, “How Paced Bottle Feeding Will Benefit Your Baby,” we discuss this feeding strategy further and give you the steps on how to put it into practice.
2.) Feed in Smaller Quantities, but More FrequentlyJust as paced bottle feeding reduces the likelihood that your baby will overeat and get reflux, feeding your baby in smaller quantities but more often can have the same effect.
When babies take in a large meal at one time, it can be difficult to digest all at once. It also makes it more likely that some will come right back up through your baby’s immature ring muscle between the esophagus and stomach.
With this strategy, your baby will still drink the same amount of breast milk or formula in a 24-hour period, but could be given in 10 feeds instead of 7 (as an example.)
3.) Keep Baby in an Upright Position During Feeding and AfterBabies sleep a lot and that means a lot of laying down. But reducing this amount of time is one of the easiest ways to prevent reflux symptoms.
We recommend the following:
- Keep baby upright during feeds
- Hold your baby upright for the 20 - 30 minutes following a feed
- Wear your baby in a baby carrier so you can get a break while being able to keep your baby upright more often
With this said, we want to caution you against usually sleep positioners. You may be tempted to try these due to their promises of reducing a baby’s reflux, but the AAP advises against their use due to SIDS concerns. Even babies with reflux should be placed on their back on a flat mattress to sleep.
4.) Burp FrequentlyThis works great with a paced bottle feeding approach. Every 20-30 seconds try burping your baby. At a minimum, you should burp your baby after every 1-2 ounces of milk ingested.
The best way to burp a baby experiencing reflux is by holding them with their tummy side against your chest and burping them over your shoulder.
This will allow for removal of trapped gas and acid from your baby’s system before giving them further milk to drink. They may still have “wet burps” but that's a whole lot better than a full-blown spit-up at the end of a feed!
They may still have “wet burps” but that's a whole lot better than a full-blown spit-up at the end of a feed!
The tips we just covered are the easiest to implement right away. And for many babies, it will be all you need to do! If your baby is still spitting up or is experiencing irritability related to gas or silent reflux, we recommend trying these last two suggestions:
5.) Consider “Drops” Prior to or After FeedingGripe Water is a natural remedy that helps to relieve reflux and other infant stomach aches. The herbs can help ease digestion. Utilizing these drops in combination with the above recommendations will likely work for many babies.
If you think your baby’s discomfort is related to gas, Mylicon is an over-the-counter remedy that many parents swear by. It’s common for babies to have both reflux and gas, so it’s worth a shot if what you’ve done hasn’t shown a lot of improvement.
We love using these two options with the bökee. Because a baby experiencing silent reflux or gas is often crying and inconsolable, this leaves you having to open these bottles one-handed while you carry your baby in the other. The last thing you want to do is put your baby down in these moments. The bökee may have originally been designed for easier bottle prep, but it works great to stabilize medicine bottles to get the tops off so you can get the medicine to your baby more quickly.
Because a baby experiencing silent reflux or gas is often crying and inconsolable, this leaves you having to open these bottles one-handed while you carry your baby in the other. The last thing you want to do is put your baby down in these moments. The bökee may have originally been designed for easier bottle prep, but it works great to stabilize medicine bottles to get the tops off so you can get the medicine to your baby more quickly.
Though it can be annoying to have to go out and buy a brand new set of bottles, getting the right bottle can often be the solution you’re looking for to eliminate your baby’s reflux. You'll want to look for bottles with a type of vent system that eliminates air bubbles in your baby's breast milk or formula.
You can find some great anti-reflux bottle options here.
You may also see recommendations to use a special formula designed for reflux relief or to put rice cereal in your baby’s bottle to thicken your baby’s milk (making it more difficult for them to bring it back up). But these two options should be done at the direction of your doctor. So, how do you know when it’s time to contact your pediatrician?
But these two options should be done at the direction of your doctor. So, how do you know when it’s time to contact your pediatrician?
Though mild cases of reflux can usually be improved by using the above strategies, some babies may need further intervention if those don’t help.
Babies who experience further distress may be experiencing a more severe form of reflux called GERD. Consulting a doctor at this time is necessary.
This may be noted by the following symptoms:
- Large volumes of spit-up
- Vomiting
- Difficulty eating
- low/no weight gain
If you notice any of these in your baby, getting direction from your doctor is imperative.
Final Word on Feeding a Baby With RefluxLuckily for most families, dealing with reflux and spit-up is a challenge that’s easy enough to work through. Taking the time to implement a few of the simple strategies above will help you avoid the milk stain while keeping a smile on your sweet baby’s face.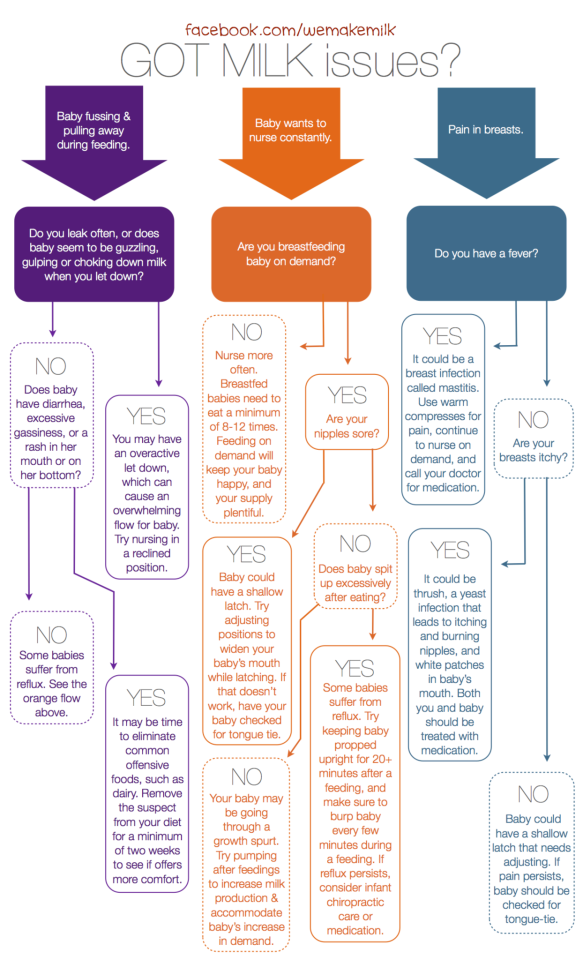
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.

GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
The following are some of the symptoms of laryngopharyngeal reflux:
- breathing problems;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.
4. Let the baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences.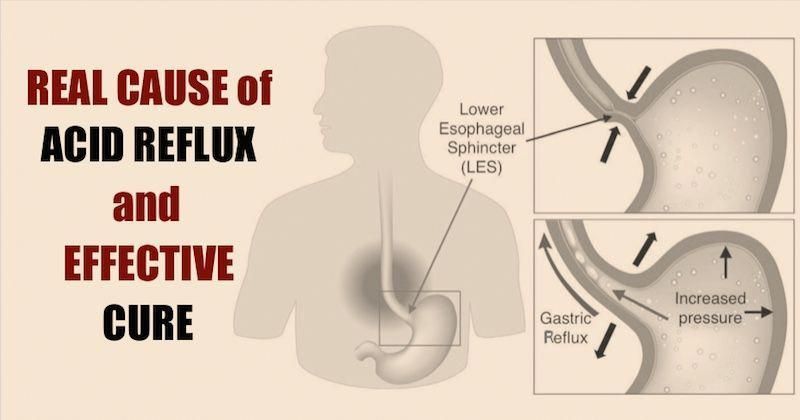 Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.
Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.
4 Seattle Children’s Hospital
5 The National Institute of Diabetes and Digestive and Kidney Diseases - Treatment for GER & GERD in Infants
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
You are about to visit the Philips USA website.
How to help the baby when regulating
Support Support iconKeywords for searching
Home Home ›!! How to help a child in sprinkling
Home home ›› How to help a child in regurgitation
9000 a very special time for a mother and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: Why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagia. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
- Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby lying on his tummy in his lap. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up while feeding. If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
- When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.











