How soon after vomiting can i feed my baby
Vomiting
Nationwide Children’s Hospital
Vomiting (throwing up) is most often caused by a virus or stomach bug. Some serious illnesses may also cause vomiting. Vomiting caused by a virus usually lasts only a couple of days. It can often be treated at home.
The main danger from vomiting is dehydration. This means that the child has lost too much fluid and does not have enough electrolytes (salts) in their body for it to work the right way. It is most important for your child to drink plenty of liquids to prevent dehydration.
Do not lay your baby on their stomach to sleep after they have vomited. They are still safest sleeping on their backs. Toddlers may sleep on their side or stomach with their heads turned.
Liquids You May Give- Older children often do well with water or clear liquids to prevent dehydration.
Clear liquids include lemonade, fruit juices without pulp (cranberry, cranapple, or apple juice), and popsicles. The popsicles must be free from cream, pudding, yogurt, or bits of fruit.
- Your child may need to drink an oral rehydration solution (ORS) like Pedialyte®. An ORS helps replace the electrolytes and fluids that your child needs.
- You can buy ORS in liquid or powder form or as popsicles at most pharmacies without a prescription. ORS store brands are just as good as a brand name.
- Do not water down (dilute) or mix an ORS with formula.
- Offer your child other things to drink. ORS should not be given as the only fluid for more then 6 hours.
Children Younger Than 1 Year of Age:
- ORS
- Breast milk or formula mixed the normal way if they can drink it
- No water except when used to make formula
- Do not give fruit juices or liquids that are high in sugar, such as Hawaiian Punch®, Hi-C®, Kool-Aid®, sodas, or syrups.
 Do not give teas or broths. These liquids could make your child feel worse.
Do not give teas or broths. These liquids could make your child feel worse.
Children Older Than 1 Year of Age:
Same as above and:
- Water
- Clear liquids
- Ice popsicles made from ORS
- Milk, if tolerated
- Flavored gelatin cube
When your child is vomiting:
- Offer clear liquids after your child has not vomited for 30 to 60 minutes. This gives the stomach time to rest.
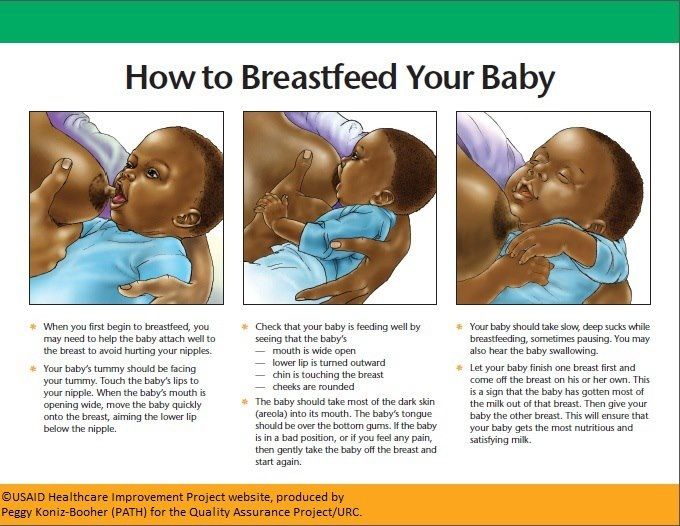
- Breastfeeding should not be stopped. Try to nurse your baby more often.
- If needed, you can stop giving formula if you are giving ORS. Try to restart formula as soon as possible.
- Start slow (Picture 1). Give small sips of liquids often. This may reduce the vomiting.
- For children under 1 year: use a spoon or syringe to give 1 to 2 teaspoons every few minutes (5 to 10 mL).

- For older than 1 year: give ½ to 1 ounce (1 to 2 tablespoons or 15 to 30 mL) every 20 minutes for a few hours.
- For children under 1 year: use a spoon or syringe to give 1 to 2 teaspoons every few minutes (5 to 10 mL).
- When your child can drink without vomiting, gradually increase the amount. If they still vomit, wait 30 to 60 minutes, and start again.
- Do not force your child to drink or wake them up to drink if they are sleeping.
- Do not give any kind of milk or yogurt drinks until the vomiting has stopped for 8 hours.
Amount of Liquid to Give to Prevent Dehydration
| Child’s Weight | Minimum Goal to Give Every Hour* |
| 7 to 10 lbs. | At least 2 ounces (4 tablespoons or ¼ cup) |
| 11 to 15 lbs. | At least 2½ ounces (5 tablespoons) |
| 16 to 20 lbs. | At least 3½ ounces (½ cup) |
| 21 to 40 lbs. | At least 6½ ounces (¾ cup) |
| 41 to 60 lbs. | At least 10 ounces of liquid every hour (1¼ cups per hour) |
* Minimum fluid goals per hour may increase if vomiting, diarrhea, or fever are present.
Solid Foods- When children are vomiting, they usually don't feel like eating solid food. It will not hurt them to miss a few meals as long as they can drink enough fluids.
- After about 6 to 8 hours of giving clear liquids and your child is no longer vomiting, try to get them to start eating some food.
 Starchy, bland foods like cereals, crackers, or bread are easier to digest. Avoid foods high in sugar and greasy, fried foods. Do not give them red-colored foods that might look like blood in vomit.
Starchy, bland foods like cereals, crackers, or bread are easier to digest. Avoid foods high in sugar and greasy, fried foods. Do not give them red-colored foods that might look like blood in vomit.
Medicine: Some medicines used for vomiting in older children or adults are very dangerous for young children. WARNING: Do not give your child any medicine unless their doctor or health care provider tells you it's safe for them.
Sleep: It's important that your child gets plenty of rest. Sleep helps the stomach finish digesting any food in it. It may calm your child’s vomiting.
Preventing the Spread of InfectionYou can help stop the spread of viruses and protect others by:
- Make sure your child washes their hands with soap and water after using the toilet and before eating.
- Wash you hands often and after touching your child, their eating utensils, or anything that might have vomit on it.
 Use soap and water or a hand sanitizer.
Use soap and water or a hand sanitizer. - Keep the things your child uses, like toys and dirty clothes, away from others. Wash them in hot, soapy water.
- Clean the toilet and hard surfaces often with disinfectants or alcohol wipes. Let dry for 15 seconds.
- Use clean wipes or washcloths for each diaper change. Put the used diaper in the diaper pail or trash right away.
Call your child's doctor or health care provider if you think they're getting worse, do not get any better in 24 hours, will not breastfeed, or show these signs:
- Vomiting gets worse or happens more often. Vomit is bright green or has blood or dark specks that look like coffee grounds in it.
- Your child shows signs of being dried out (dehydration) (Picture 2).
- Urine is very dark
- Newborn (0 to 4 months) has less then 6 wet diapers in a day
- Child (4 months or older) has less than 3 wet diapers in a day or pees less than 3 times in a day
- No tears when crying
- Dry or sticky mouth
- Hard or fast breathing
- Sunken-looking eyes
- Soft spot on baby’s head is flat, sunken, or pulls in
- Hard to wake up (lethargic), acts confused or does not know what they are doing
- Urine is very dark
- Your child has a high fever.
 Use a digital thermometer and wash it after each use.
Use a digital thermometer and wash it after each use. - Younger than 3 months of age - 100.4° Fahrenheit (F) or 38° Celsius (C) or above
- Older than 3 months of age - 104°F (40°C) or above, above 102F (38.9C) for more than 2 days or keeps coming back, or they have been treated to bring their fever down but it hasn't worked.
- If your child has a fever and:
- Looks very ill, is fussy, or is drowsy
- Has an unusual rash
- Has a stiff neck, a bad headache, or sore throat
- Has immune system problems that make them more likely to get sick, such as sickle cell disease or cancer, or takes medicine that weakens the immune system
Vomiting (PDF), Somali (PDF), Spanish (PDF)
HH-I-71 ©Copyright 1977, revised 8/22 | Nationwide Children’s Hospital
You Might Also Be Interested In
Article
Seasonal Flu Resources
Rotavirus
Blog
Bivalent COVID Vaccines: What You Need to Know
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year. Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.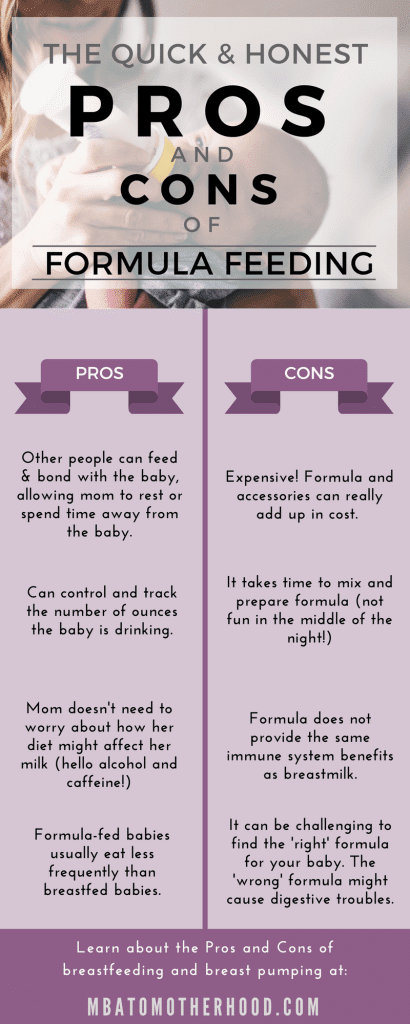
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
In gentle mode. Nutrition of children after food poisoning. What to feed a child after food poisoning and vomiting
Unfortunately, food poisoning in young children is not uncommon. In addition to treatment, in such cases, the doctor will recommend special nutrition that will help the baby's body replenish the loss of vital substances and recover faster after illness.
Food poisoning can be conditionally divided into two groups: poisoning itself and food poisoning. nine0005
Food poisoning is a disease that occurs after eating poisonous or toxic substances. This includes poisoning by mushrooms, poisonous berries and seeds. You can also get poisoned by chemicals: they can get into food by negligence. More often than not, we encounter food poisoning.
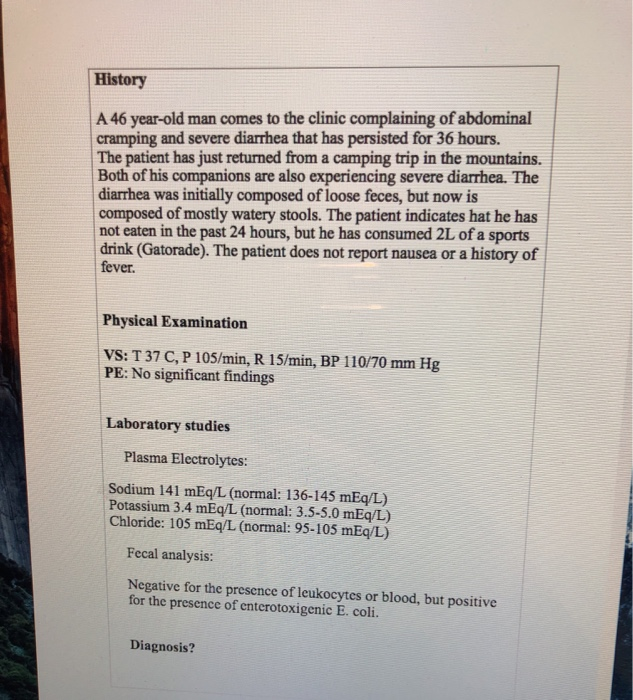
Food poisoning (FTI) is an acute, non-contagious disease that results from the consumption of foods containing certain types of microorganisms and their toxins. This disease occurs only in connection with the consumption of foods richly contaminated with toxins and / or living cells of a specific pathogen. It usually has the character of a group disease, characterized by a short incubation period (the length of time from the moment the microbial agent enters the body to the onset of symptoms of the disease) and an acute, short course. Most often, the causative agent of PTI is salmonella and opportunistic flora (bacteria, fungi, viruses, protozoa, quite widespread in the environment, and also living in the intestines of healthy people). Normally, they do not have a negative effect on a healthy body, but begin to actively multiply and harm their owner when normal conditions are violated - for example, when local immunity is reduced. Their ability to cause infectious diseases of the body contributes to the tendency to colonization, the rapid acquisition of resistance to adverse factors, including antimicrobial drugs. Under the influence of various external and intra-environmental factors, opportunistic bacteria quickly change their biological properties and turn into pathogenic (capable of causing infectious diseases).
This disease occurs only in connection with the consumption of foods richly contaminated with toxins and / or living cells of a specific pathogen. It usually has the character of a group disease, characterized by a short incubation period (the length of time from the moment the microbial agent enters the body to the onset of symptoms of the disease) and an acute, short course. Most often, the causative agent of PTI is salmonella and opportunistic flora (bacteria, fungi, viruses, protozoa, quite widespread in the environment, and also living in the intestines of healthy people). Normally, they do not have a negative effect on a healthy body, but begin to actively multiply and harm their owner when normal conditions are violated - for example, when local immunity is reduced. Their ability to cause infectious diseases of the body contributes to the tendency to colonization, the rapid acquisition of resistance to adverse factors, including antimicrobial drugs. Under the influence of various external and intra-environmental factors, opportunistic bacteria quickly change their biological properties and turn into pathogenic (capable of causing infectious diseases). nine0005
nine0005
Signs of poisoning
You can determine that a child has been poisoned by the following signs: the baby's health worsens - he becomes weak, capricious, lethargic, complains of pain in the abdomen, tightens his legs; further nausea, vomiting appear. In the case of food poisoning, following vomiting, the temperature may rise and diarrhea may begin. The development of symptoms, the severity of the disease and the tactics of treatment are completely dependent on which pathogen has entered the body.
In the case of food poisoning, a child may develop a serious condition due to dehydration - a large loss of fluid with feces and vomit. Children who, after gastric lavage, continue to experience nausea, vomiting, stool disorders, there are signs of dehydration and mild or moderate intoxication, are prescribed oral rehydration (rehydration - replenishment of lost fluid) and detoxification (aimed at removing toxins from the body - for example, taking enterosorbents) therapy , which is currently recommended before hospitalization. nine0005
nine0005
Replenishing fluid loss
The principles of dietary planning should take into account the manifestations of the disease - which dominates: vomiting (acute gastritis), diarrhea (enteritis) or gastroenteritis (vomiting and diarrhea). And most importantly, any formulated diet should have a sparing effect on the inflamed mucous membrane of the gastrointestinal tract. Drinking mode. Due to high temperature and significant fluid loss, the water-salt balance is disturbed, blood thickens, intoxication increases - a painful state of the body due to the action of harmful or toxic substances on it, coming from outside or produced in the body itself. Therefore, it is necessary first of all to provide the child with a plentiful drinking regimen. nine0005
For oral rehydration, water-salt solutions containing salt, soda, glucose, potassium are used. Pharmacies sell dry powders for the preparation of solutions - rehydron, citraglucosolan, etc. The contents of the packages are dissolved in 0. 5 or 1 liter of warm boiled water. The child needs to drink the solution during the day, calculating the required amount of fluid from body weight indicators. So, a baby under 1 year old for every kilogram of body weight should be given 150-200 ml of liquid, older children - 120-170 ml. The volume of liquid calculated per hour is given to the child every 5-10 minutes in a teaspoon. It is not necessary to increase the dose, as a large amount of liquid can cause repeated vomiting. Water-salt solutions can be alternated with sweet tea, rosehip broth. In the acute period, the drink should be at room temperature. nine0005
5 or 1 liter of warm boiled water. The child needs to drink the solution during the day, calculating the required amount of fluid from body weight indicators. So, a baby under 1 year old for every kilogram of body weight should be given 150-200 ml of liquid, older children - 120-170 ml. The volume of liquid calculated per hour is given to the child every 5-10 minutes in a teaspoon. It is not necessary to increase the dose, as a large amount of liquid can cause repeated vomiting. Water-salt solutions can be alternated with sweet tea, rosehip broth. In the acute period, the drink should be at room temperature. nine0005
The first thing to do is to make sure your child is drinking plenty of fluids.
Rehydration is carried out until the child is no longer bothered by vomiting and frequent, debilitating diarrhea. If diarrhea remains against the background of an improvement in the condition, then after each liquid stool, it is recommended that the baby be given a drink at the rate of 10 ml / kg. It is not recommended to carry out the so-called water-tea break - the complete exclusion of food for a long time. As soon as the child stops tormenting vomiting, you can offer him food. nine0005
It is not recommended to carry out the so-called water-tea break - the complete exclusion of food for a long time. As soon as the child stops tormenting vomiting, you can offer him food. nine0005
Principles of nutrition after poisoning
In the acute period of the disease, with high fever, nausea and vomiting, decreased appetite, a sparing diet is recommended for the baby, which ensures better absorption of food. To do this, all dishes are prepared and given in liquid or semi-liquid form, vegetables and cereals are boiled to a soft state and rubbed, meat of animals and birds, fish are prepared in the form of a soufflé. During this period, it is recommended to use canned meat and vegetables for baby food, as easily digestible fortified products with a delicate texture. nine0005
In the acute period, in the presence of high temperature, poor health of the child, it is advisable to feed fractionally - up to 7 times a day, reducing the intervals between meals to 2-2.5 hours and reducing its amount for each meal. This will allow you to quickly restore the disturbed functions of the body.
This will allow you to quickly restore the disturbed functions of the body.
With a sharp decrease in appetite in a child, do not be afraid of malnutrition. It is unacceptable to force-feed the baby, as this can cause nausea and vomiting. As mentioned earlier, all the missing volumes of food in the acute period of the disease must be replenished with liquid. nine0005
First aid for poisoning
If you know for sure that the child ate or drank an inedible or toxic substance, spoiled food, then the first thing to do is to wash the stomach of the affected baby. It is carried out drinking, and for young children - either special children's or boiled water at room temperature at the rate of: a child of 10 months - 1 year - 20 ml / kg, 2-6 years - 16 ml / kg, 7-14 years - 14 ml /kg. After the child has drunk the required amount of liquid, press on the root of the tongue to induce vomiting. After washing the child's stomach, it is necessary to make the child drink sorbents: this is activated carbon or filtrum, enterosgel, etc. nine0005
nine0005 If the child refuses any offered food, do not force him to eat: this may provoke a new bout of vomiting. You should also not be led by a sick baby: he may want to eat "unhealthy" foods (chips, cola, etc.), the intake of which in a healthy person can cause a painful condition, and even the harm that these foods can cause to a weakened child's body, it is easy to imagine. It can be both inflammation of the pancreas and inflammation of the biliary tract, especially in conditions of damage to the gastrointestinal tract by toxins. nine0005
In the acute period of the disease, the body's need for vitamins and minerals increases sharply. Therefore, it is necessary to additionally prescribe vitamin preparations that contain, without fail, vitamins of groups B, C and A, which improve metabolic processes and increase the body's resistance. A recovering child (who has stopped vomiting) is prescribed children's vitamin preparations, since it is impossible to replenish the amount of missing and "lost" vitamins with food alone. nine0005
nine0005
Menu features. When compiling a menu for a sick baby, you need to take care of a sufficient amount of animal protein in his diet. First of all, we are talking about milk protein, which has a lipotropic effect. This is important for improving the function of the liver, which suffers by neutralizing the toxic substances that accumulate in the body.
The amount of dietary fats in the diet of a sick child should not exceed the physiological norm (and in the first days of illness, their amount should be reduced by 10-20%), since in conditions of dehydration and a decrease in appetite, the production of enzymes that "digest" fats is disturbed, and they, in turn, act on the acid-base balance of the body, contributing to a shift to the acid side, thereby worsening the child's condition. All types of fats should be given to the baby only as part of ready-made meals and not offered in their pure form (for example, butter for a sandwich), as this will aggravate the decrease in appetite. nine0005
In the acute phase of illness, all meals are prepared and given in liquid or semi-liquid form.
The carbohydrate component of the diet should not be high, especially during the acute period of the disease, at high temperature, toxicosis, as they enhance the fermentation processes in the intestine.
As the child's condition improves, the temperature normalizes, and the effects of toxicosis are eliminated, his diet should gradually expand, approaching the physiological one.
Nutrition in case of food poisoning depends entirely on which part of the digestive tract has been affected by the infectious/toxic agent and, therefore, how pronounced inflammatory changes and impaired functions are in it. nine0005
Nutrition for vomiting and pain in the stomach. If the child is concerned only with pain in the epigastric region and vomiting, the therapeutic diet is built on the principles of diet therapy for acute gastritis. In the presence of frequent vomiting, you can skip one, maximum two meals. Oral rehydration should be carried out with special solutions. Then it is necessary to switch to fractional nutrition with a decrease in the daily volume of food by 40-50%, while continuing oral rehydration. Starting from the 2nd day, the volume of food increases by 10-15% daily with lengthening the intervals between feedings. The daily volume of food should be brought to the physiological norm no later than 3-5 days from the start of treatment. nine0005
Oral rehydration should be carried out with special solutions. Then it is necessary to switch to fractional nutrition with a decrease in the daily volume of food by 40-50%, while continuing oral rehydration. Starting from the 2nd day, the volume of food increases by 10-15% daily with lengthening the intervals between feedings. The daily volume of food should be brought to the physiological norm no later than 3-5 days from the start of treatment. nine0005
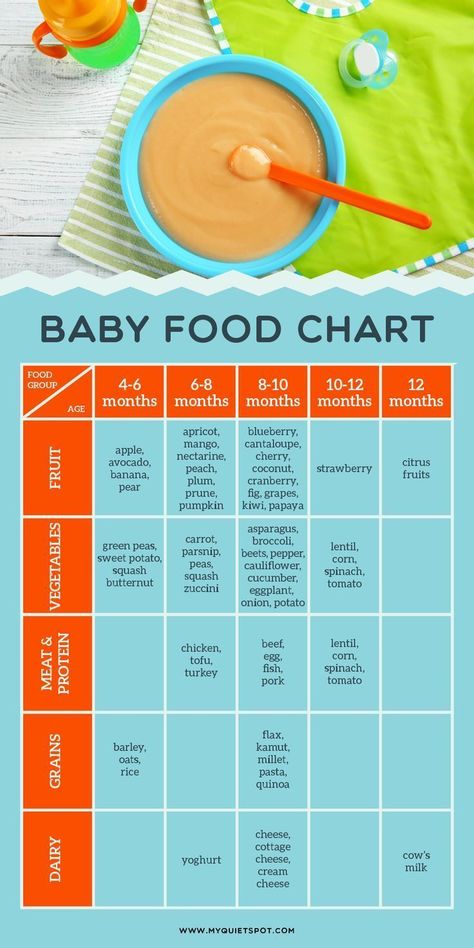
Breast milk is the optimal product for diet therapy of children under 1 year of age. Children of the second half of life, who had previously been introduced to the menu of complementary foods after the indicated pause, are first introduced into the diet with half milk cereals (rice, buckwheat), after a few days, 10-20 g of baby cottage cheese are added to this complementary food, after another 1- 2 days - vegetable purees and then fruit juices. Older children, when their general condition improves, along with cereals, are allowed to introduce vegetable purees, 1/2 egg yolk, and then vegetable soups and meat complementary foods. nine0005
nine0005
Nutrition for children older than 1 year old is built on the same principles, only a single amount of food is increased and foods allowed for this age are included in the diet faster. So, with frequent vomiting, it is recommended to unload in the diet: on the first day, it is advisable for the child to give kefir or any other fermented milk product, 100-200 ml (depending on age) every 3-3.5 hours. The next day, you can return to age-appropriate food.
Within 1-3 weeks after the illness, it is recommended to follow the principles of mechanical, chemical and thermal sparing. Mechanical sparing provides for the following culinary processing: steaming dishes, boiling, the consistency of dishes - first liquid, semi-liquid, mushy, and then crushed and just a piece. Thermal sparing involves taking only warm food. And chemical sparing is the exclusion from the diet of foods that irritate the mucous membrane of the stomach and intestines. Such products include snacks, sauces, spices, black bread, raw vegetables and fruits, raw and boiled white cabbage, turnips, radishes, radishes, peas, beans, cucumbers, millet, pearl barley, freshly squeezed and sour juices. nine0005
nine0005
Nutrition for enteritis. If the manifestations of the disease were not limited to the upper gastrointestinal tract and the child began to be disturbed by diarrhea (enteritis), then when compiling the menu, the specifics of digestion in the small intestine should also be taken into account.
The use of whole cow's milk in the acute period is not recommended, as it enhances intestinal motility, fermentation processes, thereby leading to increased diarrhea. Dairy products are replaced with sour-milk drinks, while it must be remembered that one-day kefir has a laxative effect, the rest have a fixing effect, sour-milk sourdough helps the intestinal microflora to cope with harmful agents. Porridges are prepared either with half milk or water. Vegetables and fruits rich in fiber that cause flatulence are excluded from the diet: beets, radishes, turnips, radishes, cucumbers, legumes, oranges, tangerines, sauerkraut, plums, grapes, herbs, black bread. Refractory fats (fats of animals and birds) are excluded. Ghee and vegetable oil are recommended in dishes, in a small amount - one and a half times less than for a healthy child. The rules of sparing thermal, mechanical and chemical processing of products are observed: food must be mashed, chopped, warm and not contain irritating substances. nine0005
Recipes
Meat soufflé
- Meat - 60 g;
- wheat bread - 5 g;
- egg -1/4 pc.,
- butter - 1/2 teaspoon;
- broth - 1-2 tbsp. spoons.
Meat, cleaned of films and tendons, cut into pieces and stew in a small amount of water until half cooked. Then add wheat bread soaked in cold water, pass everything twice through a meat grinder with a fine mesh, add broth, egg and stir. Put this mass into a saucepan, greased with oil and sprinkled with breadcrumbs, and bake, covering the saucepan with a lid, in an oven in a water bath. Cooking time - 20-25 minutes. nine0005
Rice porridge mashed with half milk
- Rice — 1.
 5 tbsp. spoons;
5 tbsp. spoons; - water - 1 glass,
- milk - 1/2 cup diluted halfway with water;
- sugar -1h. spoon;
- butter -
- 1/4 teaspoon;
- salt - to taste.
Rinse rice, add to boiling water and cook until soft. Then rub through a sieve, add hot (but not boiling) milk, stir well. Add sugar and cook for 2-3 minutes to thicken the porridge. Remove from heat, season with butter. nine0005
How to feed a child with vomiting: principles of gentle nutrition
During and after a child's vomiting, parents should review the diet. This condition disrupts the electrolyte balance, microflora, and causes dehydration. The body does not take food well - the rich taste and smell of the dish can provoke nausea, in addition, appetite often decreases. What to feed the baby?
Contents [ show ]
- Why children vomit
- What to do after vomiting and what to feed the child? nine0079
- Sample daily menu for a child over one year old
- What foods not to eat when vomiting
- Tips for parents when a baby vomits
- Drinking regimen for vomiting
Why children vomit
The following problems can provoke vomiting05 9007 disease;

Vomiting accompanies diseases more serious than ordinary food poisoning: appendicitis, helminthiasis, kidney failure, intestinal obstruction. But in this case it is combined with other characteristic symptoms. nine0005
In addition, vomiting is a natural human reaction to feeding against will. Don't be surprised if you run into her when you try to feed your baby when he doesn't want to. This is not a whim of a child. So his body reacts to the excess portion size. Another situation in which vomiting can begin is exposure to a new, most often exotic food with an unusual smell, taste or texture.
What to do after vomiting and what to feed the baby?
In case of poisoning, the digestive organs begin to suffer. The mucous membranes become inflamed, nausea and diarrhea occur. The body loses a huge amount of water, dehydration occurs, which can lead to serious consequences. nine0005
First of all, you need to compensate for the lack of liquid - give weak, slightly sweet black tea, you can also green, dried fruit compotes, pharmacy (for example, Regidron) or a salt solution prepared by yourself.

For newborns, follow the following feeding schedule :
- When breastfeeding: before the condition returns to normal, do not breastfeed the baby for at least 3-6 hours - this may provoke a new attack of vomiting. Drinking is allowed. When the vomiting has passed, you can return to the usual feeding pattern. nine0079
- When formula-feeding: with the approval of a pediatrician, stop feeding, give the newborn only water. When the condition normalizes, start offering the mixture at first in small portions, gradually returning to the usual ones.
If complementary foods have already been introduced, on the first day after vomiting, offer:
- first courses: chicken broth, rice soup, soups with broccoli or homemade noodles;
- biscuits;
- boiled round rice porridge (mucilaginous). nine0079
A day after the baby has been poisoned, second courses can also be included in the diet. Buckwheat or rice porridge will do. Cook them with water, formula, breast or cow's milk diluted with water.
Cook them with water, formula, breast or cow's milk diluted with water.
Gradually, as with the introduction of complementary foods, return to the menu the dishes familiar to the child in accordance with his age - meat soufflé, vegetable / fruit puree, fish, cottage cheese, eggs.
Older children (from 8-12 months) can include in the diet not very fatty fish, lean broth with chicken, boiled rice, and a baked apple will not harm. Introduce fruits later - they contain acids that can irritate the stomach lining already damaged by vomiting. Bananas, pears and apples are suitable, preferably boiled or baked, wait a while with sour berries and fruits. nine0005
Sample daily menu for a child older than one year old
If the child has already become familiar with the main complementary foods and almost switched to a common table, after vomiting, you can make the following menu for the day:
| Meals | Food | Breakfast | 1. 2. Oatmeal, buckwheat or rice porridge 3. Sweet tea with cookies |
|---|---|---|---|
| Snack Lunch | 1. Chicken stock 2. Cooks prepared from white bread | ||
| SPEC | 1. BURNE with cooked meat of chicken | ||
| Dinner | 1. Boiled potatoes and carrots 2. Fruit, for example, banana | 9024 the time of vomiting and at least a week after it, one should not introduce new complementary foods and generally give the child unfamiliar food, and heavy food (pork, seafood, etc.) should be excluded for at least 7–10 days.


 nine0079
nine0079