How to bottle feed a premature baby
Tips for Feeding Premature Babies – Children’s Health
Share:
When babies are born prematurely (before 37 weeks of pregnancy), they may have special feeding and nutritional needs. Preemies often need extra support to grow and continue developing, and parents may have questions about breastfeeding, bottles or feeding schedules.
Kikelomo Babata, M.D., a neonatologist at Children's Health℠ and Assistant Professor at UT Southwestern, answers these questions and shares advice for feeding your premature baby.
What are common feeding problems in premature infants?
Premature babies may face different feeding problems depending on their age and development. "Post-conceptual age is more important than chronological age for a baby's development," explains Dr. Babata. "A 4-week-old infant born at 32 weeks may not be as developmentally ready to feed as a 2-week-old infant born at 35 weeks. And every baby is different."
Some premature babies have difficulty breastfeeding or bottle-feeding for the first few weeks of their lives. This is because infants, both full-term and premature, continue developing their ability to suck, swallow and breathe after birth. This is a skill they need to feed, so they can coordinate how to suck, swallow then breathe through their nose. Additionally, premature babies may be sleepy and get tired during their feeds.
Premature infants might also have underdeveloped lungs. They might need to be on oxygen, which can make it difficult for them to eat.
Other common feeding problems in premature babies can include:
- Apnea (episodes where they stop breathing)
- Episodes of bradycardia (slow heartbeat that can cause oxygen levels to drop)
- Immature feeding pattern (sucking, swallowing and breathing incorrectly or out of order)
- Oral aversion (not taking a bottle or breast)
- Risk of aspiration (breathing in milk or formula)
If your baby experiences these feeding problems, they may need to be fed through a feeding tube. This tube is placed through the nose and down into the esophagus. If your baby has a feeding tube, they'll stay in the hospital until it is removed.
This tube is placed through the nose and down into the esophagus. If your baby has a feeding tube, they'll stay in the hospital until it is removed.
Once your baby goes home, your pediatrician can offer tips on feeding your baby and the importance of good nutrition. If needed, they can refer you to speech therapist for more support.
Can I breastfeed my premature baby?
Yes, you can breastfeed a premature baby. Your breastfeeding experience may depend on your baby's development and nutritional needs.
Breastmilk offers many benefits for premature babies, such as:
- Boosting digestion
- Helping baby’s immune system fight infection
- Promoting eye and brain development
- Providing bonding opportunities
"Breastmilk is linked to a lower risk of necrotizing enterocolitis, an illness that can be devastating for preterm infants," says Dr. Babata. Necrotizing enterocolitis is inflammation that can seriously damage or destroy intestinal tissue in babies. It can increase their risk of death or neurodevelopmental problems.
It can increase their risk of death or neurodevelopmental problems.
Breastfed infants also have a lower risk of ear infections, respiratory infections like respiratory syncytial virus (RSV) and bronchiolitis, rashes and gastroenteritis. Breastfeeding can have long-lasting benefits as well – lowering your child's risk for chronic illnesses in the future.
Advice for breastfeeding a premature baby
It's important to know that breastfeeding a premature infant might look different than breastfeeding a full-term infant. Breastfeeding may take more coordination for a preemie than bottle feeding, and depending on how premature your baby is, they may have difficulty latching. You may need to use bottles for a few weeks if your baby is having difficulty nursing. You can still choose to pump and provide breastmilk in a bottle. See tips for increasing your milk supply while pumping and how to safely store your breast milk.
If your premature baby can breastfeed, they still might need bottles of supplemental formula. Often, premature babies cannot exclusively breastfeed because they have higher caloric needs to support growth. Special high-calorie formula or human milk fortifiers can help your child grow while still getting the benefits of breastmilk.
Often, premature babies cannot exclusively breastfeed because they have higher caloric needs to support growth. Special high-calorie formula or human milk fortifiers can help your child grow while still getting the benefits of breastmilk.
If your premature baby is on a feeding tube, talk to your care team to learn what you can do and whether you should pump your breastmilk.
What type of bottle and formula is best for my premature infant?
Whether you give breastmilk or formula in a bottle, you should use a slow flow bottle nipple designed for premature infants. These bottle nipples help prevent your baby from getting more liquid than they can handle at once.
Most premature babies will use a special formula designed for preterm babies. Your pediatrician or neonatologist can recommend the right formula for your baby's needs. Depending on your baby's diet, they can also advise if any other nutritional supplements are needed, such as vitamin D or iron.
How much should I feed my premature baby and how often?
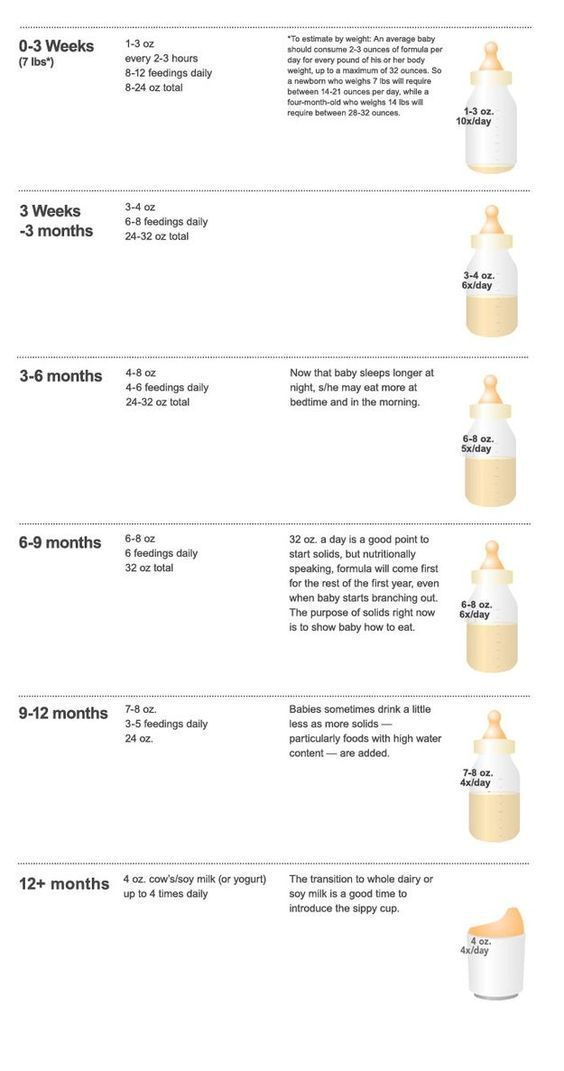
How much your baby needs to eat will change as they grow. Premature babies need 150 to 160 milliliters per kilogram of body weight each day. Your lactation consultant or pediatrician can help you determine how much this is for your baby.
No matter how much they eat per feeding, preemies need to eat at least every 3 to 4 hours.
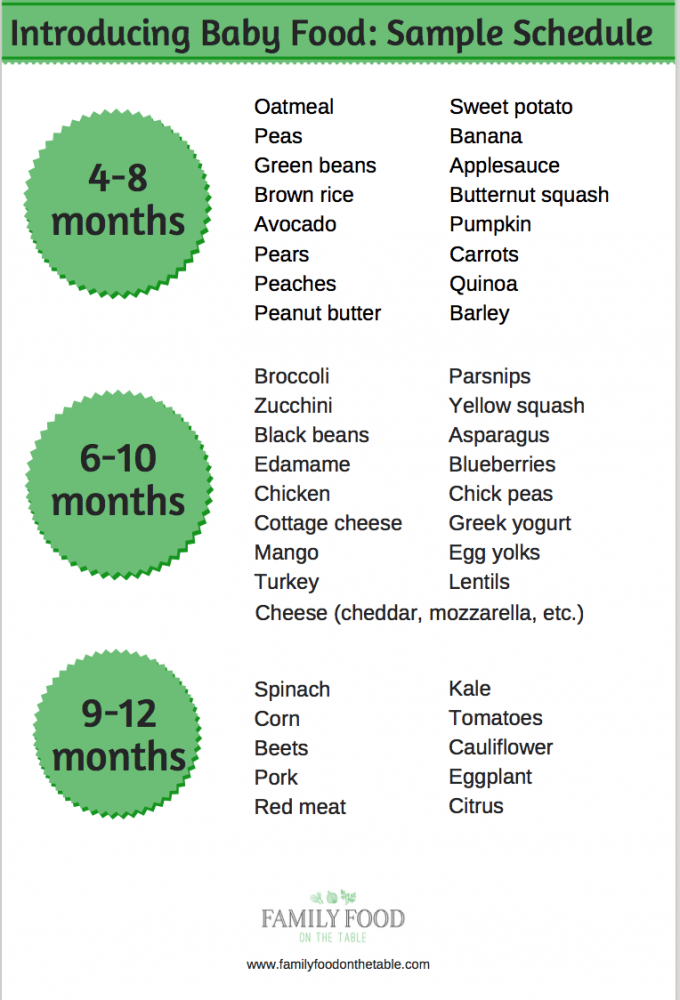
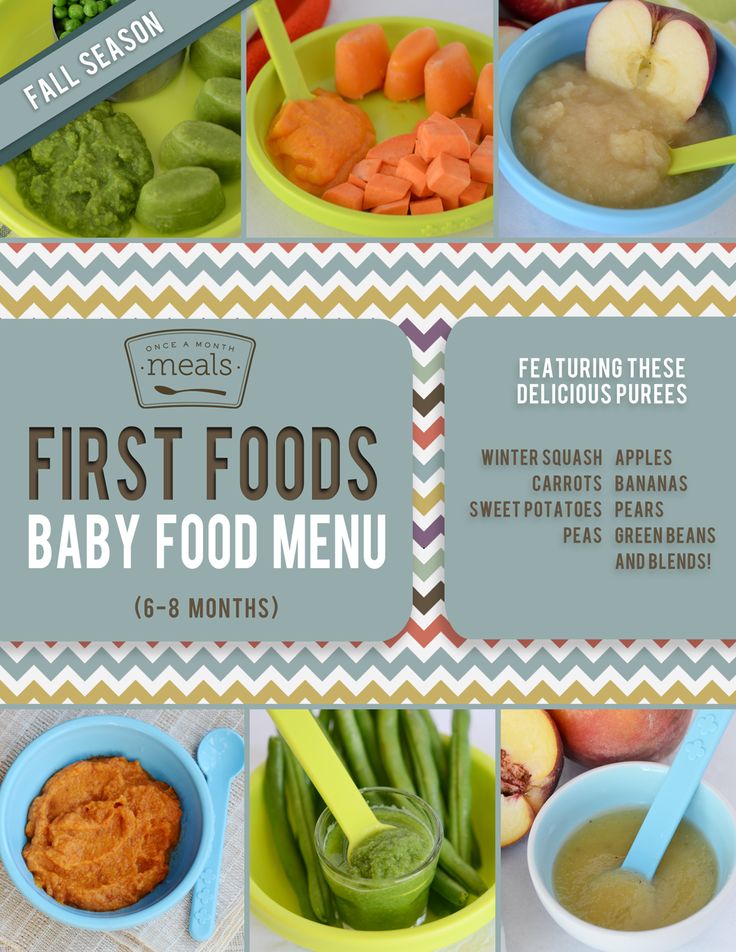
When can my premature baby eat solids?
A premature baby can start eating solid foods when their adjusted or conceptual age is 4 to 6 months. A conceptual or adjusted age means that instead of counting your baby’s age from their date of birth, it's calculated from their due date. For instance, if your baby is born 10 weeks before their due date, their age at 10 weeks past their due date is 10 weeks (even though they were born 20 weeks ago).
Around the adjusted age of 4 to 6 months, premature babies should be able to support their head and have lost their tongue-thrust reflex. This reflex causes them to spit out anything put in their mouth that's not milk or formula. This is a good time to introduce solids.
This reflex causes them to spit out anything put in their mouth that's not milk or formula. This is a good time to introduce solids.
Taking care of a baby is a challenging job. While these special feeding needs can add extra stress to those early days of your child's life, parents should remember that patience is key.
"Most babies will eventually learn to feed orally," says Dr. Babata. "Just take it one step at a time and be sure to notice and enjoy progress as it occurs."
Learn more
With the only nationally ranked Level IV NICU in North Texas, Children's Health provides expert multidisciplinary care for a wide variety of complex neonatal conditions. Learn more about our top-ranking Neonatology program.
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Feeding your baby after the NICU
After your baby leaves the NICU, you can feed her breast milk, formula or both.

Your baby gives you cues for when she’s feeling hungry and when she’s had enough to eat.
Your baby most likely is eating enough if she’s gaining weight and makes six to eight wet diapers 4 to 5 days after birth.
If you have trouble feeding your baby, ask for help from your baby’s health care provider or your lactation consultant.
If you’re feeding your baby from a bottle, use a cup of warm water to warm breast milk or formula. Never microwave your baby’s bottle.
What does your baby eat after the NICU?
Breast milk (milk from your breast) is the best food for babies in the first year of life. Breast milk has antibodies that help keep your baby from getting sick. It contains nutrients that help your baby grow and develop. And it changes as your baby grows so he gets exactly what he needs at the right time. This is true even if your baby was born prematurely. Premature birth is birth that happens before 37 weeks of pregnancy.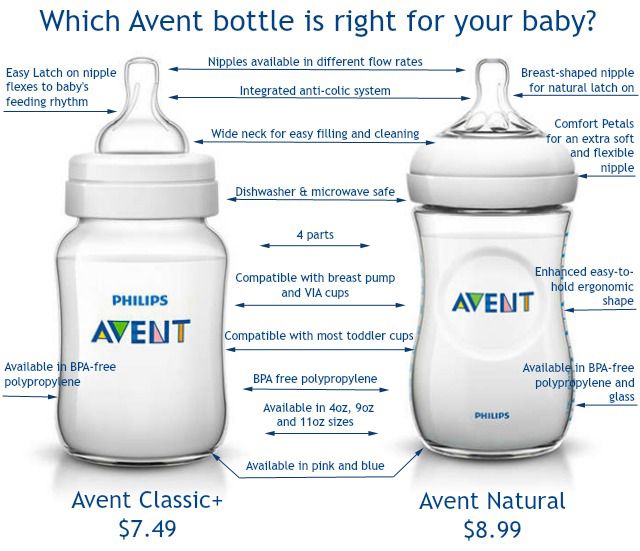
In the NICU, you may not have been able to feed your baby the way you wanted to. For example, some babies in the NICU can’t breastfeed directly (feed from the breast). They may not have a good suck, swallow breathe pattern to be able to breastfeed well, or breastfeeding may be too tiring. Now that you’re home, you and your baby can get used to breastfeeding together.
You can feed your baby your own breast milk or donor breast milk. Donor breast milk is breast milk that a woman donates to a milk bank. A milk bank receives and stores donated breast milk, tests it to make sure it’s safe and sends it to families of babies who need it. Donor breast milk is prescribed by your baby’s health care provider. It has all the benefits of your own breast milk.
Formula is a milk product you can feed your baby instead of breast milk. If you’re not breastfeeding or if your baby needs extra nutrients, he may need to have formula. Your baby’s provider can recommend one that helps your baby get all the nutrients she needs. Sometimes babies get both breast milk and formula.
Sometimes babies get both breast milk and formula.
How do you know when your baby is ready to eat?
Babies eat a lot, and each baby is different. Some babies are hungrier in the morning, and other babies are hungrier at night. Most babies eat every 2 to 3 hours, or eight to 12 times a day. Over time, you get to know your baby’s eating habits.
Ask your baby’s provider about how often to feed your baby to make sure she’s gaining enough weight. If your baby sleeps for long periods of time, you may need to wake her up every few hours to eat.
Look for and learn your baby’s feeding cues. Feeding cues are signs that your baby is hungry. Feeding cues include:
- Rooting. This is turning her head toward anything that touches her cheek or mouth.
- Sucking movements or sounds
- Putting her hand to her mouth
- Crying. This is a late feeding cue. Try to feed your baby before she starts to cry.
To make nighttime feedings easier, you may want to put the baby’s crib in your room so she’s nearby during the night.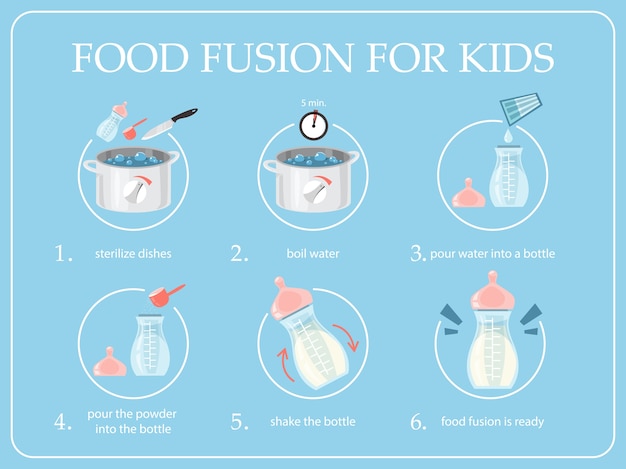 The American Academy of Pediatrics (also called AAP) recommends that you and your baby sleep in the same room, but not in the same bed, for the first year of your baby’s life but at least for the first 6 months.
The American Academy of Pediatrics (also called AAP) recommends that you and your baby sleep in the same room, but not in the same bed, for the first year of your baby’s life but at least for the first 6 months.
How do you know when your baby has had enough to eat?
Look for your baby’s cues. These are some ways your baby is telling you he’s full:
- He starts and stops feeding.
- He unlatches often or spits out bottle.
- He slows down or falls asleep.
- He gets distracted easily.
- He closes his mouth or turns his head away.
Your baby most likely is eating enough if he’s gaining weight and makes six to eight wet diapers 4 to 5 days after birth. If you’re worried that he’s not getting enough to eat, tell your baby’s provider.
Who can help you with breastfeeding after your baby leaves the NICU?
Most NICU babies can learn to breastfeed. It may take time and practice for you and your baby to get comfortable with it. Be patient and ask for help if you need it. You can get breastfeeding help from a lot of different people:
Be patient and ask for help if you need it. You can get breastfeeding help from a lot of different people:
- Your health care provider and your baby’s provider
- A lactation consultant. You can find a lactation consultant through your health care provider or your hospital. Or go to the International Lactation Consultants Association.
- A breastfeeding peer counselor. This is a woman who breastfed her own children and wants to help and support mothers who breastfeed. She has training to help women breastfeed, but not as much as a lactation consultant. You can find a peer counselor through your local WIC nutrition program. Or visit womenshealth.gov/breastfeeding or call the National Breastfeeding Helpline at (800) 994-9662.
- A breastfeeding support group. This is a group of women who help and support each other with breastfeeding. Ask your provider to help find a group near you. Or go to La Leche League.

Can you pump and store breast milk?
Yes. If you’re breastfeeding, a breast pump helps you remove milk from your breasts. You may have used a breast pump in the NICU. Or you may want to use a one now that your baby is home because you’re going back to work or school. Some moms use a breast pump because they want a break between feedings or so their partner can feed the baby.
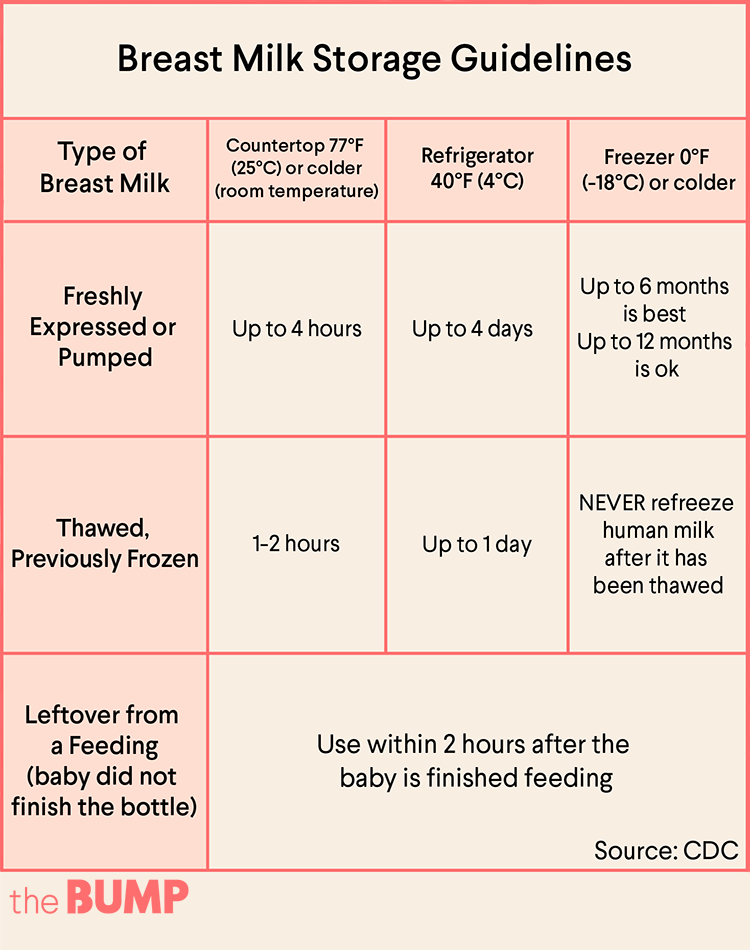
After you pump, put your breast milk in containers (bottles or bags) and store them in the refrigerator or freezer. Put just the amount of milk your baby needs for each feeding in the container. Breast milk doesn’t last forever, so write the date on the container before you store it. Fresh breast milk is safe at room temperature for 4 hours.
If you’re using formula, how do you know what kind to get?
If you’re feeding your baby formula, your baby’s provider can tell you what kind to get and how much to feed your baby. Some babies leave the hospital on regular infant formula. Other babies need a special formula that has more calories or certain nutrients. Prepare the formula using the package directions or using instructions from your baby’s health care provider.
Other babies need a special formula that has more calories or certain nutrients. Prepare the formula using the package directions or using instructions from your baby’s health care provider.
There are three kinds of formula:
- Ready-to-use liquid formula. You pour this formula right into your baby’s bottle.
- Concentrated liquid formula. You add water to this liquid formula before giving it to your baby.
- Dry or powdered formula. You add powder to the water before giving it to your baby. Use the scoop that comes with the formula to measure the right amount. Put the water in the bottle first, then the formula, and shake well to mix.
If your baby doesn’t drink all the formula within 1 hour, throw it away. Give her a new bottle of fresh formula at his next feeding.
How do you make bottle feeding safe for your baby?
If your baby has done well with the nipples and bottles used in the hospital, ask to take some home with you.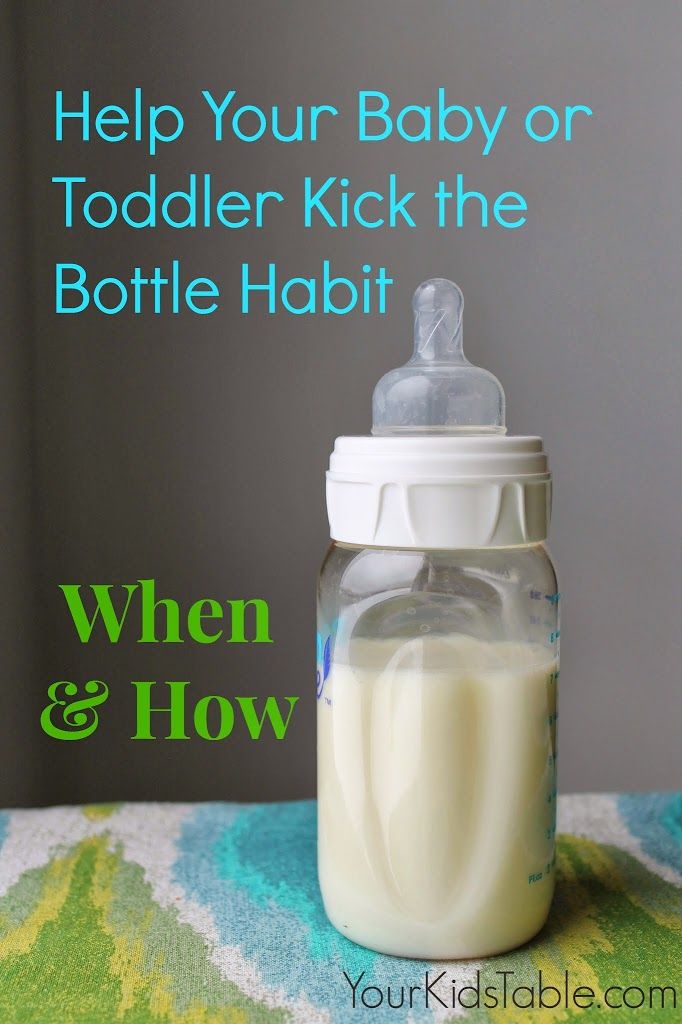 And ask the NICU staff where you can buy them. If the nipples and bottles used in the hospital didn’t work well, try different kinds to find the ones your baby likes. Clean and store the nipples and bottles as it says on the package directions.
And ask the NICU staff where you can buy them. If the nipples and bottles used in the hospital didn’t work well, try different kinds to find the ones your baby likes. Clean and store the nipples and bottles as it says on the package directions.
If you’re bottle feeding, warm the bottle before you give it to your baby. Put the bottle of milk or formula in a cup of warm water. Test the milk on your wrist to make sure it’s not too hot—it should be lukewarm. Never microwave your baby’s bottle. The breast milk or formula can heat unevenly and burn your baby’s mouth.
When bottle feeding, hold your baby upright and support his head so he can breathe and swallow in a comfortable way. You and your partner can take turns so that both of you feel comfortable feeding your baby. Bottle feeding is a great way to be close and bond with your baby.
Last reviewed June, 2019
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
Professor Katsumi Mizuno, Department of Pediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. 1 The causes of preterm birth are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth. nine0003
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit.
They often require hospitalization in the neonatal intensive care unit.
Why is breast milk so important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for premature babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). nine0012 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that make it easier for the baby to digest, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended that the deficiency be replenished with donor milk rather than formula. nine0003
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious diseases that preterm infants are susceptible to, 8 such as severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
The more milk your baby gets, the lower the risk of developing diseases. nine0012 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
Most importantly, premature infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. nine0012 14 They also have a 6% lower risk of readmission in the first year of life. 15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. 15 In addition, their cardiovascular system works better during their lifetime. nine0012 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy. After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first. nine0003
After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first. nine0003
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. nine0012 19 This is why it is important to start expressing breast milk as early as possible.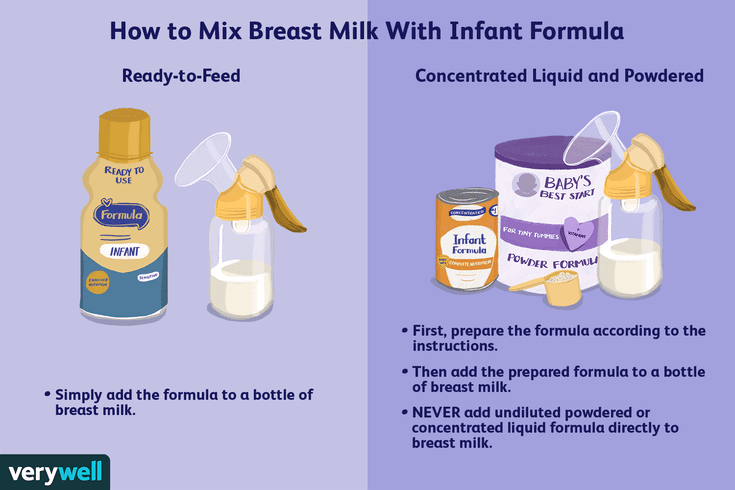
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If your baby is too weak to latch on and suckle milk, you can use a breast pump* available at the hospital or maternity hospital to “do the job for the baby”. Breast stimulation with research-based technology, 20 mimics the rhythm of the baby's suckling, plays an important role in starting and maintaining milk production in the first hours after birth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This is how your baby learns the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. You can be involved in the care of your premature baby in a variety of ways - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk. nine0003
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply. nine0003
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support.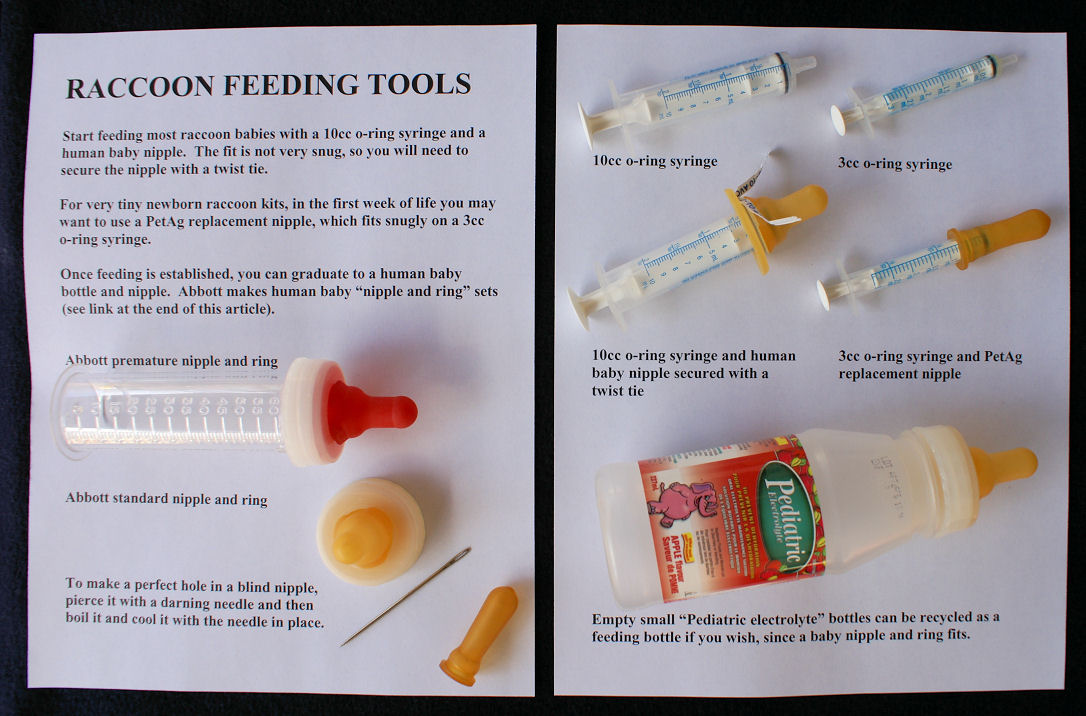 Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding? nine0018
At whatever gestational age a baby is born, if the baby is stable enough for skin-to-skin contact, it can seek the breast for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breastmilk, so you can put some milk on the nipple before putting your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety. nine0003
You can put your baby to the breast for sedative suckling as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood. You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization. Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. nine0085 Prog Lipid Res . 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
4 Underwood Ma. Human Milk Formature North Am . 2013;60(1):189-207. - Underwood, M.A., "Breast milk for the premature baby." 1):189-207.
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight. Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights. " Akta Pediatr. 1987;76(2):328-331.
" Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312. nine0085
nine0085
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. 12 MEIER PP ET AL AL AL AL . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." nine0085 Perinatol wedge. (Clinical perinatology). 2010;37(1):217-245. 13 Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. nine0085 Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406. 15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. nine0085 Pediatrics. 2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. 16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. nine0085 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490. 17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." nine0085 Pediatrix (Pediatrics). 2016;138(1):pii:e20160050. 18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. 19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209. 20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants. 21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." nine0085 Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91. 22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366. - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. nine0085 23 Prime PK et al. 24 Uvn ä s Moberg K Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206. 25 Boundy EO et al. nine0085 Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". 26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. nine0085 J Hum Lact . 2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46 27 Nyqvist KH et al. Towards universal kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on kangaroo mother care. nine0085 Acta Paediatr . 2010;99(6):820-826.- Nukvist K.H. et al., "On the Universality of the Kangaroo Method: Recommendations and Report from the First European Conference and the Seventh International Kangaroo Method Workshop". 28 American Academy of Pediatrics - Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics . 2012;129(3): e 827-841.- American Academy of Pediatrics - Section "Breastfeeding", "Breastfeeding and the use of breast milk". Pediatrix (Pediatrics). 2012;129(3): e 827-841. *RC No. ФСЗ 2010/06525 dated 17/03/2021 %PDF-1.5 % 10 obj >/OCGs[14 0 R]>>/Pages 3 0 R/Type/Catalog>> endobj 20 obj >stream application/pdf Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.
Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.  1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523.
1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523.  Pediatrix (Pediatrics). 2006;118(1):e115-123.
Pediatrix (Pediatrics). 2006;118(1):e115-123. 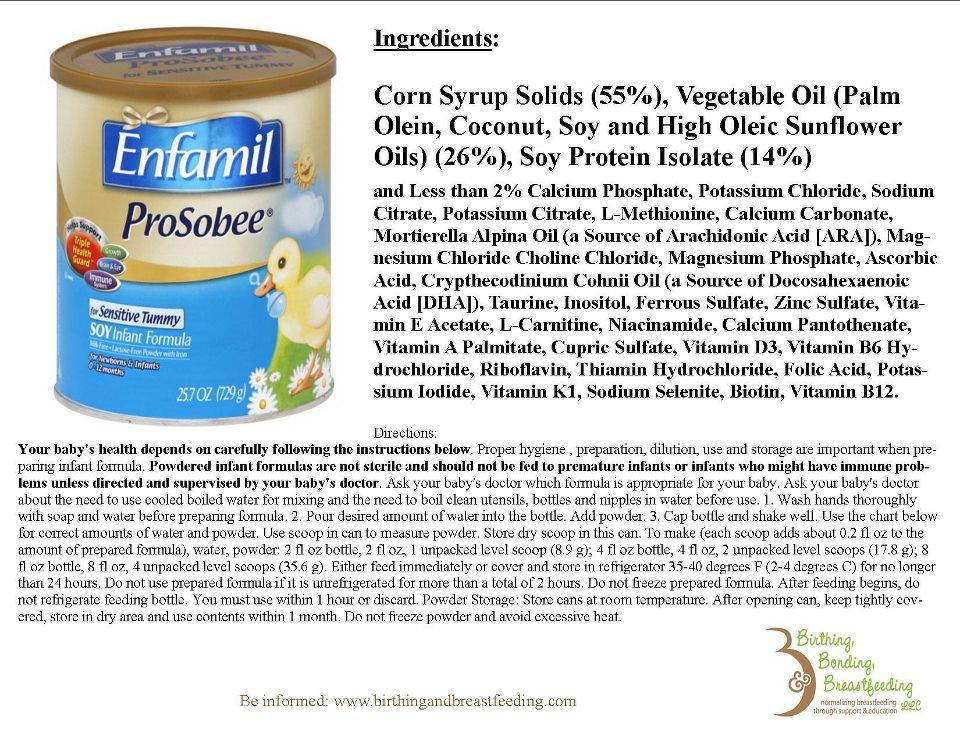 - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
- Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.  " nine0085 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
" nine0085 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.  Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.  Pediatrix (Pediatrics). 2015;137(1): e20152238.
Pediatrix (Pediatrics). 2015;137(1): e20152238.  Akta Pediatr. 2010;99(6):820-826.
Akta Pediatr. 2010;99(6):820-826. Read instructions before use. Consult a specialist about possible contraindications.
power supply
 did:1e78dbf1-03f3-7246-846b-aa029f6efd31uuid:5D20892493BFDB11914A8590D31508C8proof:pdfxmp.iid:3d8e54f0-3bfc-4245-9150-047bf0c8e023xmp.did:3d8e54f0-3bfc-4245-9150- 047bf0c8e023uuid:5D20892493BFDB11914A8590D31508C8proof:pdf
did:1e78dbf1-03f3-7246-846b-aa029f6efd31uuid:5D20892493BFDB11914A8590D31508C8proof:pdfxmp.iid:3d8e54f0-3bfc-4245-9150-047bf0c8e023xmp.did:3d8e54f0-3bfc-4245-9150- 047bf0c8e023uuid:5D20892493BFDB11914A8590D31508C8proof:pdf  jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e
jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e  iid:f6c9fdc7-d444-9548-bf4f-3806865f965e
iid:f6c9fdc7-d444-9548-bf4f-3806865f965e  jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e
jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e  jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e
jpgxmp.did:f6c9fdc7-d444-9548-bf4f-3806865f965exmp.iid:f6c9fdc7-d444-9548-bf4f-3806865f965e 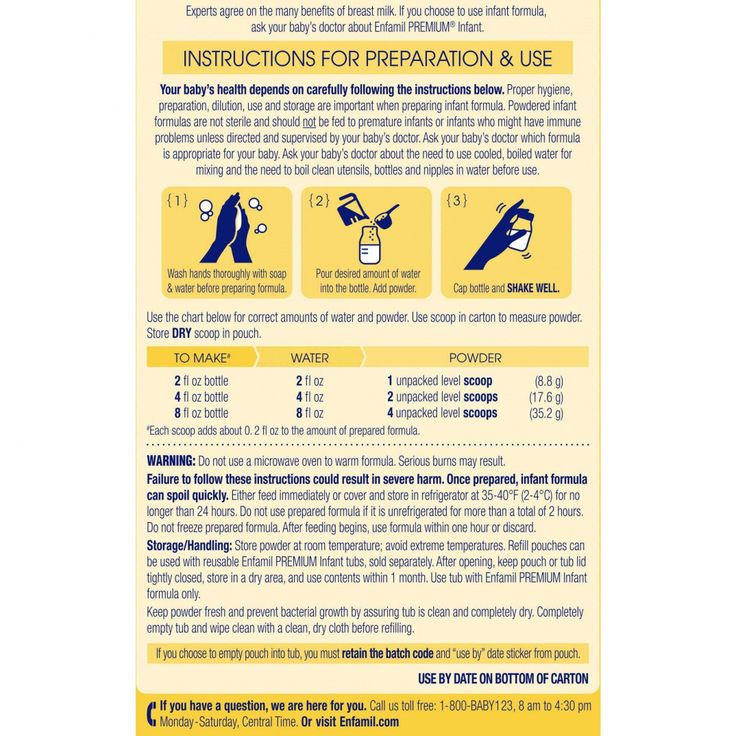 00 endstream endobj 3 0 obj > endobj 16 0 obj > endobj 17 0 obj > endobj 10 0 obj >/Resources>/ProcSet[/PDF/ImageC]/Properties>/XObject>>>/Thumb 25 0 R/TrimBox[0.
00 endstream endobj 3 0 obj > endobj 16 0 obj > endobj 17 0 obj > endobj 10 0 obj >/Resources>/ProcSet[/PDF/ImageC]/Properties>/XObject>>>/Thumb 25 0 R/TrimBox[0.