How to bottle feed a tongue tied baby
Does a Lip-Tie or Tongue-Tie Affect Bottle-Feeding? - Alabama Tongue-Tie Center | Dr. Richard Baxter
by Richard Baxter, DMD, MS | Oct 17, 2021
These are excellent questions we hear from parents on a daily basis. Many parents are told by providers to “just give him a bottle” and it will solve the issues they are struggling with from the tongue-tie. The problem is, it’s not true. Switching to a bottle takes away the maternal aspect (pain, plugged ducts, supply issues, etc.), but it does not fix the infant issues of a poor latch, milk leaking out, reflux, excessive gas, colic, and slow feeding with possible weight gain issues.
In the 1920s when formula came out, it was sold to parents as “better than breastmilk” so if a baby was tongue-tied, you might as well feed them formula since it’s “superior.” Fast forward 70 years and with renewed research in the 1990s and an emphasis on breastfeeding, more moms began nursing because, in fact, breastmilk is far superior to infant formula. Also, the act of nursing is superior to bottle-feeding, as it helps to mold the palate, and set the child up for healthy airways and craniofacial growth. That is to say, if you are bottle-feeding, don’t feel that ever-present mom guilt, as babies can still thrive with formula or bottle-feeding, and many moms need to supplement for various reasons (our twins were bottle-fed, and are now thriving 7-year-olds).
With tongue-ties, it’s heartbreaking when moms come to see us months after the baby is born and has been struggling with an undiagnosed tongue or lip-tie, and mom had to give up nursing and has now lost her milk supply. It takes a while for parents to put the puzzling symptoms together, and providers lack education on the impact of tongue- and lip-ties. This happens on an almost daily basis, and to the parents’ surprise, switching to a bottle has not magically solved the problems. They have tried five different bottles and are still struggling. The baby is still leaking milk, fussy, gassy, colicky, struggling to sleep, spitting up all the time, hiccuping after every feed, and seems always hungry. Most of the time, it’s a less obvious posterior tongue-tie, as if it was to-the-tip, many providers would have seen it and informed the parents. (But we see lots of to-the-tip or anterior ties go undiagnosed for months as well, surprisingly! Education in this space is lacking at medical and dental schools and residency programs.)
The baby is still leaking milk, fussy, gassy, colicky, struggling to sleep, spitting up all the time, hiccuping after every feed, and seems always hungry. Most of the time, it’s a less obvious posterior tongue-tie, as if it was to-the-tip, many providers would have seen it and informed the parents. (But we see lots of to-the-tip or anterior ties go undiagnosed for months as well, surprisingly! Education in this space is lacking at medical and dental schools and residency programs.)
Posterior Tongue-Tie in Infant After Lifting Properly
Recently, a new study by Dr. Bobby Ghaheri confirmed what we see daily at our office. In a randomized controlled trial (RCT), he showed with a special bottle with a computerized nipple, that babies feed more efficiently, are better able to adapt to changes in feeding, and had more rhythmic and coordinated sucking after a proper posterior tongue-tie release. Moms also saw less nipple pain, were more confident in feeding their babies, and the babies had less spit-up, fewer hiccups, and were less fussy after having their posterior (less obvious!) tie released with a CO2 laser. This study is important because it shows that not just anterior or obvious ties cause problems, but posterior ties also cause issues. It also shows that switching to a bottle will not solve the issue. If there is a physical restriction of the tongue, and the baby has the symptoms of a tie (see image), then that baby would very likely experience improvement after a proper, full tongue-tie release by an experienced provider.
This study is important because it shows that not just anterior or obvious ties cause problems, but posterior ties also cause issues. It also shows that switching to a bottle will not solve the issue. If there is a physical restriction of the tongue, and the baby has the symptoms of a tie (see image), then that baby would very likely experience improvement after a proper, full tongue-tie release by an experienced provider.
All of the issues at the top of the symptoms sheet can be experienced by bottle-feeding babies. Tongue-ties do not always lead to weight gain issues, so we hear daily that the primary care provider said “he’s gaining weight, so he is fine” and the parents think the tie doesn’t need to be treated. First, mom may have an oversupply, or be constantly feeding him, or any number of other ways to compensate, so the baby is still “fine” but not “thriving.” We want optimal health and growth, not just “fine” or survival. If moms and babies have more than a few symptoms on this form, it means they are on the struggle bus and are not thriving! Plus, a tongue restriction can have lifelong effects including speech, solid feeding, or sleep issues in the future (see below for child to adult symptoms).
If moms and babies have more than a few symptoms on this form, it means they are on the struggle bus and are not thriving! Plus, a tongue restriction can have lifelong effects including speech, solid feeding, or sleep issues in the future (see below for child to adult symptoms).
Probably 75% of the babies that come see us have a lip-tie that is fairly obvious (that’s what brings them to our office), but also have a less obvious tight, thick, restrictive tongue-tie that is causing feeding difficulty. In fact, for moms that are nursing, the posterior tongue-tie very often is to blame for the 7+, toe-curling pain they are experiencing. This is highly unfortunate because those are the babies that are told to switch to a bottle because of the terrible pain, and moms are told the baby has “no tongue-tie” because it is not easily seen with a tongue depressor or on a quick inspection of the mouth.
If your baby is struggling with these symptoms, whether nursing or bottle-feeding, and you are concerned there might be a tongue-tie, please contact our office and we would love to get you in for a consultation to check for a restricted lip- or tongue-tie. The more checkmarks on that list of symptoms, the higher the chances of having a tongue- or lip-tie. Call 205-419-4333 to set up a consult, or send us a message. It would be an honor to help you and your family. – Dr. Baxter
The more checkmarks on that list of symptoms, the higher the chances of having a tongue- or lip-tie. Call 205-419-4333 to set up a consult, or send us a message. It would be an honor to help you and your family. – Dr. Baxter
Bottle Feeding a Baby with Tongue Tie | Helping Babies with Tongue Tie
When we think of tongue tie, we often think of a nervous speaker stumbling over their words, or mixing up our words during a conversation. However, many people don’t realise that tongue tie is a medical condition found in some babies, also known in medical terminology as ankyloglossia. From how common it is, to the implications for your child, here’s everything you need to know about tongue tie in babies.
Tongue tie occurs when a baby’s frenulum (the strip of tissue connecting the tongue to the floor of the mouth) is shorter than usual. This is a relatively common condition, affecting between 4%-11% of babies, but studies have shown it’s actually slightly more common in baby boys. Tongue tie is present at birth, and some studies have shown that it can be hereditary (passed from parent to baby), so if you know that you suffered from this then make sure to tell your doctor or midwife.
Tongue tie is present at birth, and some studies have shown that it can be hereditary (passed from parent to baby), so if you know that you suffered from this then make sure to tell your doctor or midwife.
What Is Tongue Tie?
Tongue tie is where the little strip of skin which connects your baby’s tongue to the bottom of their mouth is shorter than that of most other babies. This is sometimes diagnosed during a newborn’s physical examination after birth. However, tongue tie can be hard to spot and it may not become obvious until your baby has problems feeding. Babies who are born with this condition have a restricted range of motion in their tongue and as they age, the way that they eat, speak and swallow can be affected. For some babies with tongue tie, they are unbothered by the condition but for those who incur problems they may need a simple surgical procedure for correction.
How To Tell If Your Baby Has Tongue Tie
Caregivers may notice that their baby with tongue tie or lip tie does not meet appropriate feeding milestones or has atypical feeding behaviours. Possible symptoms for this condition include:
Possible symptoms for this condition include:
- Difficulty latching and feeding when babies breastfeed or bottle feed; they lift their lower jaw during suckling, and use their top gum and the tip of the tongue (which lies on the lower gum) to keep the nipple / bottle in place. Tongue tie and lip tie can prevent the baby from taking enough breast tissue into the mouth to latch properly for feeding and the latch is often very shallow. Many babies may be able to latch but are unable to get the correct movements for sucking. Tongue tie may also result in a poor suck, breathing pattern or swallow.
- Mother experiences pain while nursing due to restricted and atypical tongue movements or improper latching. While the infant nurses, the mother may experience additional friction. This can lead to pain, bruising and bleeding.
- Frequent feeding patterns occur because during each feed, the infant consumes less milk than typical infants. Shortly after feeding, the infant may also show signs of hunger.
- Fatigue during or directly after feeding; the stressful experience of feeding means that the child expends more time and effort when feeding. During feedings, she might become irritated or fall asleep within one to two minutes.
- Dimpling of cheeks or clicking sounds when feeding; this is tongue tie-specific and is caused by atypical latching and sucking movements. There may also be jaw tremor here. Children with tongue tie are sometimes fussy and / or often pull away from the breast or bottle.
Some babies with tongue tie have no problems stemming from the condition at all; bottle fed babies are usually fine, as the teat from the bottle doesn’t require the same tongue action as breastfeeding. However, tongue tie can cause difficulty when breastfeeding, as the baby’s tongue is essential for proper suction to the breast.
A baby with tongue tie may end up compressing the breast tissue during feeding, which can lead to nipple soreness and damage. This inability to feed correctly can lead to low weight gain and fussiness.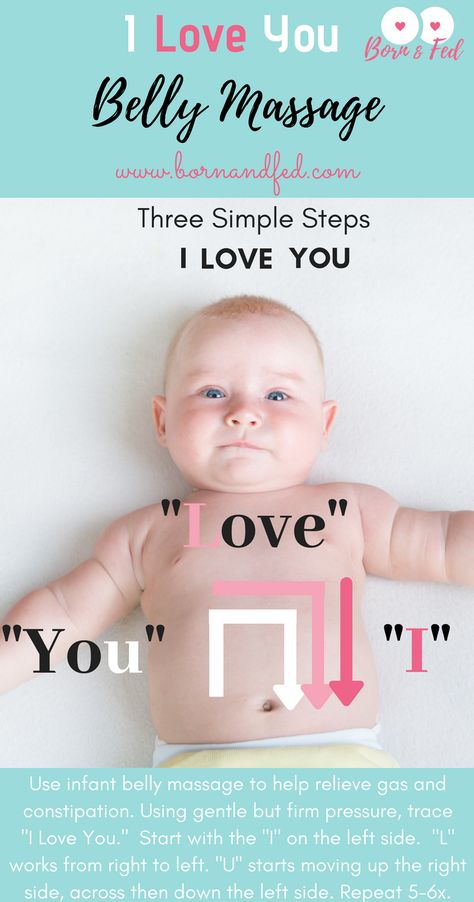 A tell-tale sign of a baby with tongue tie is a clicking sound when feeding, but this can also be a sign that you need support with the positioning and attachment of the baby at your breast, so check to make sure.
A tell-tale sign of a baby with tongue tie is a clicking sound when feeding, but this can also be a sign that you need support with the positioning and attachment of the baby at your breast, so check to make sure.
I was contacted by a very upset mum a couple of weeks ago who’s baby was extremely unhappy. Cheryl was at her wits’ end after several visits to her GP, Health Visitor and A & E with her daughter resulted in no clarity whatsoever as to what was going on with poor Jessica. Cheryl was desperate and wanted to try the babocush as soon as possible but I knew, after seeing photos of Jessica’s swollen tummy that it would take more than the babocush to sort out whatever was going on.
Want to find out more about tongue tie? Read Baby Jessica's Tongue Tie Story
How might an upper lip-tie impact feeding?
The impact of the upper lip-tie can vary - as the fullness of the upper lip can come into play. According to Melanie Potock, MA, CCC-SLP, you should consider these key points:
Breastfeeding and Bottle Feeding with Tongue Tie
- Breast – Inadequate latch: An infant has to flange his lips to establish ample suction and a proper seal of the nipple and surrounding tissue.
 It is important for babies to take in sufficient breast tissue to activate the suckling reflex, stimulating both the touch receptors in the lips and in the posterior oral cavity in order to obtain enough milk without fatigue. One (not always present) sign is a callus on the upper lip of the infant, immediately at midline.
It is important for babies to take in sufficient breast tissue to activate the suckling reflex, stimulating both the touch receptors in the lips and in the posterior oral cavity in order to obtain enough milk without fatigue. One (not always present) sign is a callus on the upper lip of the infant, immediately at midline.
- Bottle – Inadequate Seal: Since bottles and nipple shapes are interchangeable, and modifications can be made, a weak lip seal can be compensated. These compensatory measures are often adopted, however, because all attempts at breastfeeding have become too difficult, too exhausting, or result in poor weight gain ... and the culprit has been the upper lip-tie all along.
It can be difficult to tell if a baby has tongue tie, but if your baby struggles to extend his tongue out beyond his lips or if his tongue has a heart shaped appearance at the tip, it might be worthwhile getting him evaluated by a doctor.
Can Tongue Tie Go Away By Itself?
In most cases, the frenulum will recede by itself over the baby's first year, but in some cases a small surgical procedure may be required. This is a very simple operation known as a frenotomy, which is a safe and uncomplicated procedure, usually performed in office at the GP’s surgery. No anaesthesia or stitches are needed; it’s a very easy and painless procedure.
This is a very simple operation known as a frenotomy, which is a safe and uncomplicated procedure, usually performed in office at the GP’s surgery. No anaesthesia or stitches are needed; it’s a very easy and painless procedure.
Tongue Tie In Babies: What You Need To Know
However, needing this procedure is rare, and only required in cases where the baby is struggling to feed or when mum is very uncomfortable. The baby can feed with ease straight after the procedure, and many mums note that comfort during breastfeeding improves almost instantly!
If your newborn is having problems feeding and showing symptoms of tongue tie then you should flag this up with your pediatrician. If you are nursing and experiencing pain, bruising or bleeding then you should definitely notify your doctor ASAP to get your baby evaluated to see if tongue tie is the cause. We hope you have found our tips helpful and please remember that if your baby is diagnosed with tongue tie there is nothing to be afraid of. Your baby’s tongue will either grow to a normal capacity during their first year or a simple painless surgical procedure may be required. The most important thing is that feeding time runs smoothly for both mom and baby, so don’t hesitate to contact a medical professional if you are experiencing difficulties.
Your baby’s tongue will either grow to a normal capacity during their first year or a simple painless surgical procedure may be required. The most important thing is that feeding time runs smoothly for both mom and baby, so don’t hesitate to contact a medical professional if you are experiencing difficulties.
Bottle feeding
When breastfeeding is not possible, or there is not enough breast milk and supplementary feeding is required, the use of infant milk formulas allows you to establish good nutrition for the baby.
The mixtures contain all the necessary nutrients, vitamins and trace elements. As a rule, they are well tolerated and digested, especially if the feeding process is properly established.
If you plan to bottle feed or supplement your baby with formula, our article will help you navigate the basic rules and intricacies of artificial feeding.
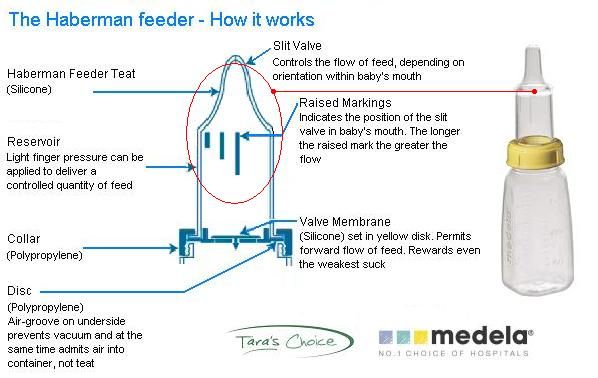
How to choose a teat (nozzle) for a bottle
Teats differ in composition (silicone, latex), shape and flow rate. While the shape of the nipple and the material are often chosen according to the preferences and needs of a particular baby, the flow rate is strictly determined by the age category.
While the shape of the nipple and the material are often chosen according to the preferences and needs of a particular baby, the flow rate is strictly determined by the age category.
Babies are fed from birth using the slowest flow nipple (these are usually labeled from 0 and one drop). Next, the teat flow rate in most bottle manufacturers increases at 3 months, 6 months, 12 months.
In order not to be mistaken, pay attention to the labeling and the age group for which the nipple to the bottle of the selected manufacturer is intended.
Whether such a nipple is right for you, you will also probably be able to understand during feeding.
- The baby should be able to comfortably grip the nipple and drink formula confidently (without too much effort).
- He should not choke/choke frequently.
- The mixture should flow well. If the mixture does not flow until you shake the bottle, the hole may be clogged with powder.
- If the mixture flows too much, check if the nipple is not torn.

How to treat the bottle
For newborn babies in the first months of life, it is recommended to sterilize the bottles before each feeding. Sterilization is the immersion of all feeding accessories (bottles, nipples, other parts) in boiling water for about 5 minutes to destroy pathogenic microflora.
You can choose any convenient method of sterilization: using a special device (sterilizer), in a microwave oven, dishwasher, ordinary boiling. Read more about how to properly sterilize bottles in our other article.
It is important to ensure that the baby bottle you use is made of safe plastic that can be heated. Some types of plastic release harmful chemicals when heated. As a rule, information about the possibility of sterilization and heating is indicated on the packaging. If there is no such information, it is not worth the risk. Use special baby bottles from well-known manufacturers. For example, a Dino Reno feeding bottle with nipple can be sterilized completely by any of the listed methods.
How to prepare formula and feed your baby
- Wash your hands with soap and water and dry with a dry towel.
- Remove the bottle and nipple from the sterilizer using the special holder (tweezers), assemble the bottle with the nipple, being careful not to touch the part that will go into the baby's mouth with your hands.
- Take boiled or special baby water heated to body temperature, dilute the mixture in the proportion indicated on the package.
- Use the special measuring spoon for preparation (it is included in each box with the mixture).
- Dilute the mixture strictly in the proportion indicated by the manufacturer. A thicker or thinner formula can harm your baby and cause stomach problems.
- Shake the bottle thoroughly to mix the contents evenly. Make sure that there are no lumps and clots left in the liquid and on the walls of the bottle.
- Check the temperature of the prepared mixture by dropping a little liquid on your wrist, it should not burn.
- Hold the bottle at the right angle. So that the tip of the nipple is always filled with milk and not with air.
- After feeding, hold the baby upright, let him burp the excess air.
- Feed your baby only fresh formula. According to the recommendations of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) of 2004, the reconstituted dry formula can be stored in a sealed bottle at a cool temperature for no more than 4 hours.
- If the mixture has cooled down, it can be warmed up with a special heater or in a water bath.
- If you are going on a long trip or outing, do not prepare the formula ahead of time. Better just pour the required amount of water into the bottle, and pour the right amount of the mixture into a separate container. Mix before feeding.
You will also find recommendations on the amount of formula to eat at a time, taking into account the age of the child, on the package. But some features of the baby's behavior can tell you whether he is full or not.
- If the baby pushes the nipple out of the bottle with his tongue and spit out the formula, he is probably already full and the feeding should be stopped.
- If the baby drank the contents of the bottle quickly and is crying, he may not have eaten enough and it is time to increase the portion.
- When your baby grows up, a feeding bottle with handles will come to your rescue. The child will be able to hold it himself and regulate the amount eaten.
How to bottle feed properly
Feeding your baby is not only an important process for healthy growth and development, but also a way to establish close emotional contact with the child and build trusting and loving relationships. The transition from breastfeeding to bottle feeding should be carried out after the mother and the child are fully prepared for this. We are talking about both the moral aspect, and about choosing the right bottle and getting adults the necessary skills so that eating brings only positive emotions and benefits to the baby. In this article, we will talk more about how to properly bottle feed your baby and where to start.
In this article, we will talk more about how to properly bottle feed your baby and where to start.
How to prepare your baby for bottle feeding
If this way of eating is a completely new experience for the baby, or if parents decide to bottle feed their baby from a very young age, slow flow nipples should be preferred. So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
Feeding bottle selection and daily care
All baby accessories should be kept clean and sterilized regularly and thoroughly.
There are several ways to sterilize dishes:
- select the appropriate mode when using the dishwasher;
- or place the bottle and teat in a vessel of boiling water for 5 minutes.
Before using this method of cleaning the bottle, make sure that the material from which it is made can be exposed to high temperatures. Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles.
Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles.
The need for thorough cleansing of everything that the baby will touch is caused by the fact that in the first months of life, the child's immune system is just beginning to strengthen. Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
How to bottle feed your baby
Before starting a meal, mom or dad should wash their hands well with soap and warm running water. Particular attention should be paid to the area between the fingers and under the nails. The hand washing process should take at least 20 seconds. And after carrying out this hygienic procedure, hands should be wiped dry with a paper towel or clean towel.
The next step is to prepare for the meal. If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
Breast milk is the most beneficial for a newborn. Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture.
In the first six months after birth, cow's or goat's milk or its substitute in the form of soy milk should not be included in the baby's diet. Valid options for supporting healthy development of a newborn are breast milk or formula milk only.
What temperature should the bottle filler be? Under no circumstances should the bottle be heated on the stove or in the microwave.
 If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method:
If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method: - put a saucepan on the stove with a little water;
- bring the water to a boil, then remove the pan from the heat;
- place a bottle of milk in a vessel and heat it to 37◦С;
- check the temperature with a pre-cleaned thermometer or a special device for measuring the temperature of foodstuffs.
You can also check the temperature of the ready-to-use bottle as follows:
- turn the bottle over;
- drip several times into your wrist area.
In this way, you can check not only the temperature of the milk or formula, but also how well the liquid flows out of the bottle. If you have to shake or squeeze the bottle hard to drip, the nipple is blocked and needs to be cleaned out. If, on the contrary, the filler pours out when the bottle is turned over, this means that the nipple is damaged and another nipple should be used to feed the baby, having previously sterilized it.
How to bottle feed your baby lying down
There are several techniques for feeding your baby. However, it is the feeding of the child lying down from the bottle that young parents consider the most comfortable. It is worth noting that eating in this position will only be safe when the baby's head is slightly raised. Otherwise, the child may simply choke. In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest.
Make sure that the feeding bottle is closed correctly: the ring at the connection of the nipple to the bottle must not be too tight. Air must enter the bottle, otherwise a vacuum will be created there, which, in turn, will complicate the consumption of food for the child.
How to bottle feed without spitting up
Since the newborn is not able to fully control the process of feeding, along with milk, he can also take in air. This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding.
This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding.
As soon as you notice that the baby has stopped sucking on the pacifier, is tired or thoughtful, pick him up and press his face to you, holding his head and back. To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
The air will quickly rise up and the baby will burp it without any extra effort. However, you should be prepared for the fact that, along with the air, part of the consumed mixture or milk may also return. Therefore, before taking the baby in your arms, cover yourself with a diaper, because it will be easier to wash it than clothes.
Never leave your baby alone with the bottle or let him fall asleep while using it. After eating, mom or dad must help their child burp. This will help to avoid colic, bloating and other manifestations of stomach discomfort.