If baby is sick should i feed again
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year. Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours.
 If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for.
 At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again.
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.

- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
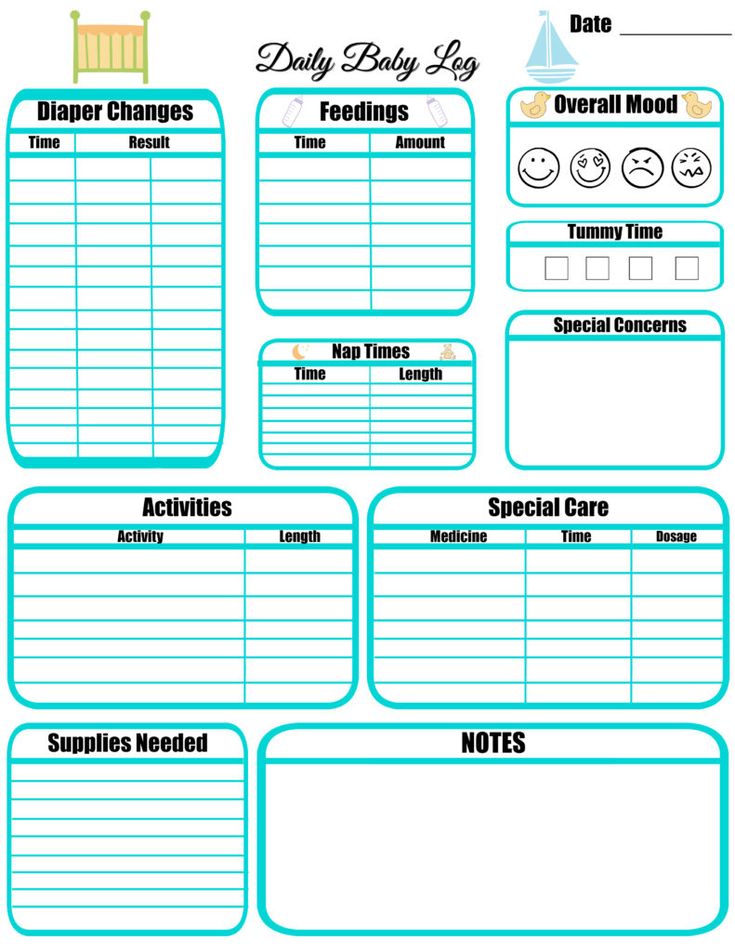
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.

- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/16/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
COVID-19 and breastfeeding Q&A
1. Can I breastfeed if I have COVID-19?
UNICEF and WHO argue that, given the benefits of breastfeeding and the low role of breast milk in the transmission of respiratory infections, a mother can continue to breastfeed as long as she takes all necessary precautions.
There is no evidence of the presence of active virus in breast milk or the possibility of transmission of novel coronavirus infection through breast milk.
At present, the main problem is not whether the virus can be transmitted through breast milk, but whether an infected mother can transmit the virus through respiratory droplets, through breathing, coughing or sneezing, while breastfeeding.
Therefore, precautions to prevent your baby from getting the virus include practicing good hand hygiene and making sure you wear a mask during close contact with your baby, including while breastfeeding.
2. Can COVID-19 be transmitted through breast milk?
UNICEF and WHO report that several studies of breastfeeding women with COVID-19 or other coronavirus infections have found no virus in their breast milk. There is some evidence that there is a possibility of viral RNA in breast milk, but there is no evidence that there is an active virus in breast milk that can cause disease.
3. Do I need to organize a separate stay with my child if I have COVID-19? Can I continue breastfeeding, or will it suck to feed my baby with expressed breast milk?
The decision to separate the mother and child can be made by medical professionals together with the parents (mother and father). Such decisions are made on the basis of an assessment of the health status of the mother and child.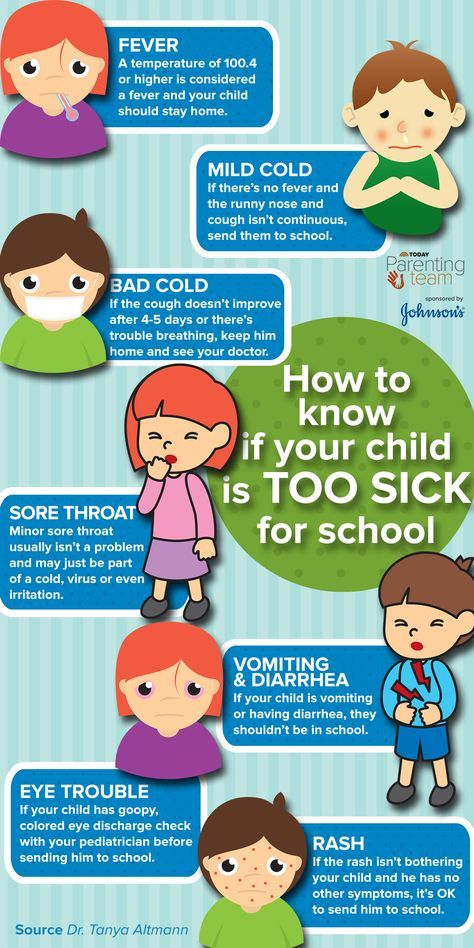
According to UNICEF and WHO, breastfeeding should not stop if mother and child can be together.
4. Do I need to switch my baby to formula if I have COVID-19?
UNICEF states that breastfeeding is the safest and most reliable way to feed your baby, especially in an emergency.
Given the benefits of breastfeeding and the evidence that breast milk plays a minor role in the transmission of other respiratory viruses, breastfeeding should be continued whenever possible.
5. If I had COVID-19hard enough and could not continue breastfeeding, or I was separated from the baby for a while, can she start breastfeeding again?
If you have been separated from your baby for a certain period of time and breastfeeding has been interrupted, you can usually restore lactation. The restoration of milk production and continued breastfeeding is called relactation.
WHO and UNICEF recommend the following key actions to restore breastfeeding:
- Interact more with your baby, including skin contact and breast massage, to increase the hormonal response that increases lactation.
- Breast massage and pumping up to 8-10 times a day can help if you are separated from your baby or between feedings.
- The baby should suckle regularly on both breasts (on average at least 8-12 times a day, about 15 minutes on each breast). Try not to exclude night feedings.
- Ensure that the baby is in the correct position during feeding so that he can suckle effectively and to prevent injury to the nipples.
- Pay attention to the contents of the baby's diapers.
If you need further advice and support, be sure to contact your pediatrician. You can also use the services of a lactation consultant to restore milk production.
6. If I have COVID-19 and I express my breast milk, how do I store it properly?
WHO says that although it is not yet completely known whether mothers with COVID-19 can, to transmit the virus through breast milk, studies currently conducted demonstrate the complete absence of the virus in breast milk.
If you have been expressing breast milk in good hygiene, you can store it at room temperature, in the refrigerator or in the freezer, depending on how quickly you want to use it.
The permissible storage time at various temperatures is shown in the table.
If you store your expressed milk in the refrigerator or freezer, be sure to label the bottles/bags with the volume and date of expression so that you use it within the allowed time frame.
COVID-19 Frequently Asked Questions about Breastfeeding
Frequently Asked Questions about COVID-19 related to breastfeeding- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- t
- U
- Ф
- x
- C
- h
- Sh
- Sh. WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Questions and answers /
- Questions and answers /
- Breastfeeding COVID-19 FAQ
May 7, 2020 | Questions and answers
Can COVID-19 be transmitted through breastfeeding?
There is currently no evidence of transmission of active COVID-19 (a virus that can cause infection) through breast milk or breastfeeding.
 There is no reason to refuse or stop breastfeeding.
There is no reason to refuse or stop breastfeeding. Should women living in COVID-19 affected areas breastfeed?
Yes. In all socioeconomic settings, breastfeeding increases survival rates and has long-term health and developmental benefits for newborns and infants. Breastfeeding also has a positive effect on the health of the mother.
Is it still recommended to practice skin-to-skin contact between mother and baby after childbirth and breastfeeding, even if the mother is suspected of having COVID-19?or a confirmed coronavirus infection?
Yes. Prolonged skin-to-skin contact immediately after birth, including kangaroo nursing, normalizes the newborn's body temperature and is associated with better neonatal survival. Placing the newborn in close proximity to the mother also promotes early breastfeeding, which also reduces neonatal mortality.
The many benefits of skin-to-skin contact and breastfeeding far outweigh the potential risk of COVID-19 transmissionand development of the disease.
Can women with suspected or confirmed COVID-19 breastfeed?
Yes. Women with suspected COVID-19 or confirmed coronavirus infection can breastfeed if they choose to. In this case, they are advised to:
- frequently wash their hands with soap and water or use alcohol-based hand rub, especially before touching a child;
- wear a medical mask before any contact with the child, including during breastfeeding;
- when sneezing or coughing, cover your face with a disposable tissue. The used tissue should be thrown away immediately and the hands washed again;
- Regularly wash and disinfect surfaces touched by the baby's mother.
It is important to change medical masks as soon as they become damp and discard them immediately. Do not touch the front of the mask and reuse the mask.
If a mother has suspected or confirmed COVID-19 but does not have a medical mask, can she breastfeed?
Yes. Breastfeeding has undeniably reduced mortality in newborns and infants and has many positive and long-term effects on the health and development of the child's brain.
It is recommended that mothers with symptoms of COVID-19 wear a medical mask, but even if this is not possible, breastfeeding should be continued. In this case, the mother should follow other infection prevention practices, such as washing hands, disinfecting surfaces, and covering her mouth and nose when sneezing or coughing with a disposable handkerchief.
The efficacy or safety of non-medical masks (eg, homemade masks made from cloth or other materials) has not yet been studied. At the moment, it is not possible to make recommendations for or against the use of these masks.
I have suspected or confirmed COVID-19 and feel too sick to breastfeed. What should I do?
If you are too unwell to breastfeed because of COVID-19 or other complications, you should be assisted in making your breastmilk available to your baby in a safe, convenient and acceptable way. To do this, you can:
- express milk;
- use donor breast milk.
If expressing milk or using donor milk is not possible, consideration may be given to using a wet nurse (another breastfeeding woman) or formula feeding to the baby, if the formula can be prepared correctly, hygienically and affordably.
I was ill with suspected COVID-19or confirmed coronavirus infection and could not breastfeed. When can I resume breastfeeding?
You can resume breastfeeding as soon as you feel well enough. There is no specific length of time during which a mother with suspected COVID-19 or confirmed coronavirus infection should refrain from breastfeeding. There is currently no data on the impact of breastfeeding on the clinical course of COVID-19at mother. Your healthcare provider or lactation consultant should be able to help you resume breastfeeding.
I have suspected COVID-19 or confirmed coronavirus infection. Wouldn't it be safer to feed my baby artificial milk?
No. Feeding newborns and infants with artificial milk is always associated with some risk, regardless of other conditions. The risk associated with formula feeding increases if there are adverse conditions at home or where the mother and child live, such as limited access to health care if the child is sick, limited access to clean drinking water, or no secure supply of infant formula.