Inverted nipple feeding baby
Can I breastfeed if I have flat or inverted nipples?
Many women worry that their breasts and/or nipples are not the right size or shape for breastfeeding. Actually, your ability to breastfeed has little to do with the size and shape of your breasts. Breast shape is seldom significant, and nipple shape poses a problem for only a small number of women. As long as your baby is able to take in a mouthful of breast, even flat or inverted nipples will not interfere with breastfeeding, and your baby’s strong suck will likely draw out the nipple.
It may be a little more difficult for women with inverted nipples to get their baby to latch onto the breast well, but with preparation and knowledge, most women with flat or inverted nipples will experience few problems with breastfeeding.
To find out if you have flat or inverted nipples, you can try the “Pinch Test.” Here’s how:
- Place your thumb and first finger on the areola about 1-2 inches from the base of the nipple.
- Press your thumb and finger together.
- If your nipple does not protrude or extend out, it is considered flat.
- If your nipple retracts or sinks in, it is considered inverted. Truly inverted nipples are rare.
Another sign of flat or inverted nipples is no movement of the nipple when stimulated or in response to cold. If your nipples protrude (extend out) when stimulated, they shouldn’t pose a problem when breastfeeding.
Suggestions for drawing out a flattened or inverted nipple:
- Use a breast pump to gently draw out the nipple and to make it easier for your baby to latch on. Most nipples will extend out with only a minute or two of pumping. Once you see the nipple lengthen, remove the pump, and quickly place your baby on your breast.
- Keep your breasts from getting engorged. It is harder to draw out a flat or inverted nipple when your breast is overly full. To keep your breasts from becoming engorged, be sure to breastfeed at least 8 to 12 times in each 24-hour period.

- Pay particular attention to your baby’s position and latch. Your baby’s mouth should be opened wide and filled with breast tissue. When your baby is positioned well, your nipple will be at the back of your baby’s mouth, near the junction of the hard and soft palate.
- Some women choose to wear breast shells (plastic, circular, dome-shaped devices with an opening in the back that you place over your nipple) during pregnancy to slowly cause a flat or inverted nipple to extend out. However, research shows that breast shells are seldom helpful and may, in fact, do more harm than good by making mothers all the more anxious. It may be worthwhile to wait until after your baby’s birth to see if there is a problem with breastfeeding before exploring this option.
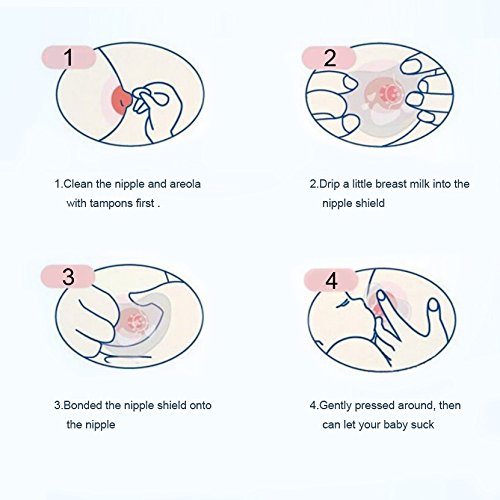
- Consider using a nipple shield (a circular device with a pin-holed nub that allows for the flow of breast milk) to aid attachment, support milk transfer, and maintain breastfeeding. Typically, a nipple shield is used at the start of a feeding to encourage the baby to latch on and then removed after he begins to suckle and swallow, but it can be used throughout the feeding.
 Different types of nipple shields are available, and the effects on breastfeeding are varied. For example, a thick rubber (latex) nipple shield is more likely to interfere with milk transfer than an ultra-thin silicone shield. Nipple shields are intended for short-term use (only until your baby has learned to latch on well or your nipples are no longer flat or inverted). Always talk with your health care provider before using a nipple shield. Because nipple shields can interfere with milk transfer, you should weigh your baby routinely (at least weekly) to make sure he is gaining an adequate amount of weight.
Different types of nipple shields are available, and the effects on breastfeeding are varied. For example, a thick rubber (latex) nipple shield is more likely to interfere with milk transfer than an ultra-thin silicone shield. Nipple shields are intended for short-term use (only until your baby has learned to latch on well or your nipples are no longer flat or inverted). Always talk with your health care provider before using a nipple shield. Because nipple shields can interfere with milk transfer, you should weigh your baby routinely (at least weekly) to make sure he is gaining an adequate amount of weight.
Remember that flat or inverted nipples don’t mark an end to breastfeeding. Many mothers breastfeed their babies despite having flat or inverted nipples. Still, it’s probably a good idea to discuss your concerns with a knowledgeable health care provider or lactation consultant both before and after your baby is born.
Last updated July 11, 2020
Inverted and Flat Nipples - La Leche League International
Inverted or Flat Nipples
Prepared by Mary Marine
The size and shape of nipples and breasts vary from person to person and can change during the breastfeeding journey.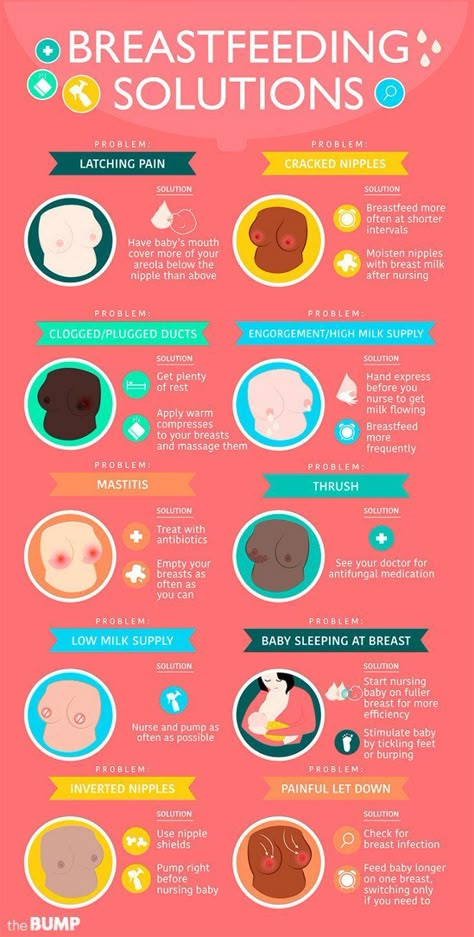 It is common for nipples to gradually change shape, become more elastic and protrude more during pregnancy and while breastfeeding. When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
It is common for nipples to gradually change shape, become more elastic and protrude more during pregnancy and while breastfeeding. When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
If you have inverted or flat nipples, your baby may need more time and patience to breastfeed. A flat nipple is smooth next to the breast tissue. Inverted nipples withdraw below the surface of the nipple. If you think your nipple may be inverted, try placing your thumb and finger on opposite sides of the areola (the darker area of skin surrounding the nipple) and squeezing gently inwards. Sometimes nipples may be partly inverted, looking dimpled or folded. Severely inverted nipples retract deeply when compressed or stimulated. A nipple that stands out when stimulated is not inverted.
Severely inverted nipples retract deeply when compressed or stimulated. A nipple that stands out when stimulated is not inverted.
After your baby is born, your nipples may appear flatter than usual but babies often lick the nipple to stimulate it before latching on. Your nipples may also appear flatter if your breasts are very full or engorged.
A deep latch and comfortable position helps your baby latch and breastfeed effectively. In the beginning, the following techniques may help you initiate breastfeeding:
- Immediately after birth, place your baby in skin-to-skin contact on your chest. Continue to use skin to skin during early breastfeeding to soothe your baby and to ease frustrations during breastfeeding. Ideally, the breastfeeding dyad is kept together until both are discharged.
- Being with your baby helps you to recognize your infant’s hunger cues.
- Before breastfeeding, express several drops of milk, so the milk is immediately available when your baby latches.

- You may massage your breast while breastfeeding to assist your baby in receiving milk.
To help evert the nipple:
- Pull back on breast tissue so nipple will protrude more.
- Breastfeed in a laidback or side-lying position especially if you have large breasts.
- Breast engorgement can contribute to the nipple being less protruded. Massage the nipple and areolar area so milk will move back into the breast or will leak out, softening the areola and everting the nipple. Also try reverse nipple softening. Reverse pressure softening involves using gentle finger pressure around the base of the nipple to temporarily move some of the swelling slightly backward and upward into the breast.
- Roll the nipple between the thumb and index finger and immediately afterwards touch the nipple with a moist cold cloth. Avoid making the nipple too cold because it can result in the nipple being numb, and inhibit let down.
- Use nipple and breast support to help protrude the nipple.
 Use both hands on each side of breast to make a “sandwich”, to squeeze nipple and areola. Use hands to press in on breast like the way you hold a big sandwich to put in the mouth.
Use both hands on each side of breast to make a “sandwich”, to squeeze nipple and areola. Use hands to press in on breast like the way you hold a big sandwich to put in the mouth. - Use a breast pump for several minutes to draw out the nipple. The suction from a pump will often cause the nipple to protrude more.
- If you have had assistance with latch and tried the tips in this article and your nipples are still sore, consider trying a nipple shield. The nipple shield is a thin silicone devise that goes on top of your nipple and areola while breastfeeding. It looks like a brimmed hat. The nipple shield is a commercially made product. A nipple shield can be used temporarily to help establish breastfeeding or in some cases to help ensure that breastfeeding continues. A shield provides a firm stimulus at the roof of a baby’s mouth where the soft and hard palate meet. This may help your baby suckle more effectively.
- Commercial products that are intended to assist in drawing out inverted nipples such as breast shells or everters are best used only with the guidance of a trained lactation consultant.

If Nipple Soreness Occurs
- You may experience nipple soreness for about the first two weeks of nursing while your flat or inverted nipple is gradually drawn out by baby’s suckling. This discomfort is generally the result of adhesions or skin binding to underlying breast tissue. If the soreness is severe, or continues past the initial two weeks, consult your health professional.
- If your nipple retracts after feedings, that skin may remain moist, leading to chapping of the skin. After feeding, pat your nipples dry and apply a moisturizer safe for breastfeeding. You may also want to wear breast shells or other devices to keep your nipple out between feedings so the skin can dry.
When Nipple Soreness is Prolonged
Rarely, sore nipples may persist for a longer period because instead of stretching, the adhesions remain tight. This can create a stress point which may lead to cracks or blisters.
- If one breast is easier for your baby to grasp and he nurses well from that breast, you can continue to feed on that side.
 You can pump the breast with the deeply inverted nipple until the adhesions loosen and the nipple is drawn out. Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast.
You can pump the breast with the deeply inverted nipple until the adhesions loosen and the nipple is drawn out. Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast. - If both nipples are deeply inverted, you can pump both breasts simultaneously for 15-20 minutes 8 or more times in 24 hours. You can feed your baby with an alternative feeding device until she is able to latch on effectively and comfortably.
- How long you will need to pump in order to draw out your nipples depends upon the strength of the adhesions and the degree of inversion. One pumping may be enough to completely draw out the nipple. If the nipple continues to deeply invert, you may need to continue pumping. When your nipple stays out after pumping, you can resume breastfeeding immediately.
- Once your nipple can be drawn into the baby’s mouth correctly and the baby can breastfeed effectively, you should be able to discontinue pumping and breastfeed without discomfort.

- On rare occasions you may continue to feel some discomfort even after your nipple has been drawn out. This could be due to the correction to the nipple.
- The nipple may invert again as your baby pauses during a feeding. In this case, you may need to stop breastfeeding and pump again for a few minutes before putting baby back to the breast.
- As a temporary transition to exclusive breastfeeding, breast compressions or the use of a nursing supplementer might help to encourage continuous sucking and swallowing so that the nipple won’t be as likely to invert during feeding.
If you do encounter challenges during your breastfeeding journey, support from a La Leche League Leader and other participants in Group meetings may help you to overcome the challenges. (Find a Leader or meeting.)
Additional Resources
Cotterman, Jean K., Reverse Pressure Softening, http://breastfeedingmadesimple.com/wp-content/uploads/2016/02/SimplerRPSsheet2. pdf
pdf
Cotterman, Jean K., Reverse Pressure Softening, http://www.breastfeedingonline.com/rps.shtml#sthash.2MPE4KHE.T3v63FBt.dpbs
Cotterman, Jean K., Engorgement Help: Reverse Pressure Softening
… a technique to aid latching when a mother is engorged, https://kellymom.com/bf/concerns/mother/rev_pressure_soft_cotterman/
Cotterman, Jean K. Reverse Pressure Softening, http://www.health-e-learning.com/articles/RPS_JCotterman_ver2005.htm
Genna, Catherine Watson, Supporting Sucking Skills in Breastfeeding Infants, C. Burlington, MA: Jones & Bartlett, 2012.
La Leche League Great Britain, Nursing Supplementers, https://www.laleche.org.uk/nursing-supplementers/
Mohrbacher, N. Breastfeeding Answers: A guide to helping Families, 2nd edition
(Revised February 2022)
Baby won't take a bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle.
 Try changing the nipple to a nipple with a different flow.
Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast.
 Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.![]()
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding.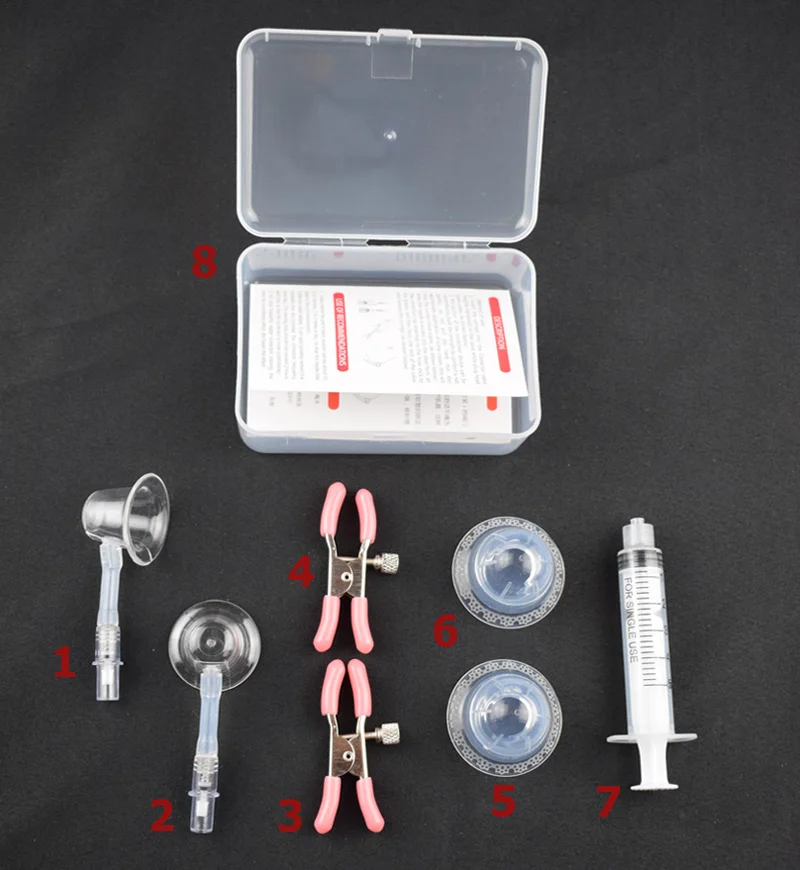 This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even retracted nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.”
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely.
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains. “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk. ”
”
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue.
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.
Preparing inverted and flat nipples during pregnancy
You may have noticed that your breasts have changed during pregnancy and your nipples have become more protruding. If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
“In a normal pregnancy, nipple formers can be worn from 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.”
“Nipple formers can be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding.”
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.”
She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.”
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breast, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before every feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- place fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.

“I had a flat nipple, but I only found out when I noticed Austin was having a hard time sucking on that side,” says Jennifer, mother of two in the UK. “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.”
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
With time, as your baby learns to suckle properly and your nipples get used to breastfeeding, you will be able to breastfeed without the pads.
“My nipples are rather flat. The doctor advised me nursing pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!”
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production begins,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ”
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breast milk.
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only expressed milk. You can also try the supplementary feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother-of-two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.”
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first.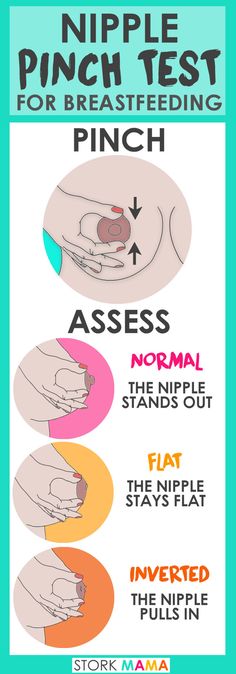 Tips on how to care for sore nipples can be found in Nursing Nipple Care.
Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside.
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK.
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast.![]() The youngest is now nine months old and I still breastfeed him.”
The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015. - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." The Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine).