Is it ok to feed baby when mother has fever
Should you breastfeed your baby when you have a fever?
By -
TIMESOFINDIA.COM
Created: Jun 24, 2020, 12:00 IST
facebooktwitterPintrest
No one likes getting sick. But for a new mom, it's even more problematic as she has to breastfeed her little one.
As per experts, it is safe to feed a baby during fever. The chances of you passing the fever to your baby through breastfeeding are very rare. In fact, your breastmilk carries antibodies that your body is making to fight the infection. These same antibodies can help your baby too. In fact, chances of your baby getting infected from you are more than getting infected by the breastmilk.
Medication during breastfeeding
Just like in your pregnancy, you have to careful about the medicines you take. It is said Paracetamol and ibuprofen are usually safe but one should not have ibuprofen if they have asthma or ulcer. One should also not take Aspirin as it can be harmful to your baby when passed through the breastmilk.
If your fever doesn't go away in three days, it's best to visit your doctor along with your baby. Ask your doctor to prescribe you medicines that will not be harmful to the baby. If your doctor asks you not to feed your baby while on medication, you can pump and dump your milk.
Pump and dump means pumping your breasts and then dumping that milk. This is important to be done if you are not allowed to breastfeed as it helps keep up your milk supply for nursing your baby in future.
You can give your baby formula milk after consulting the doctor. Sometimes, it is allowed to feed the baby right before you have to take medication. Ask your doctor if that is applicable in your case.
Verdict
So, unless you have specifically been told not to breastfeed the baby, keep doing it. Not breastfeeding can lead to fuller breasts, which can cause mastitis and worsen your fever.
Not breastfeeding can lead to fuller breasts, which can cause mastitis and worsen your fever.
Stopping breastfeeding for a longer period of time can also reduce the production of the breastmilk, which can make it difficult for your baby.
Precautions to take to reduce the risk of passing on the fever to baby
- Wash or sanitize your hands frequently, especially before picking and breastfeeding the baby.
- Cover your nose and mouth while coughing and sneezing.
- Throw the used tissues straight into the dustbin.
- Do not touch your baby's pacifier.
- Do not kiss the baby when ill.
End of the article
Visual Stories
LEGO Winter Playgrounds: Experience the joy of play
Featured in Parenting
Ideal nutritional requirement your child needs
Dwayne Johnson looks unrecognizable in video
How to keep your peace of mind when its tough
Kate Hudson on co-parenting with 3 dads
Things I wish I knew when my kids were born
How to help your kids stay focused on studies
Foods that can make your child taller
Which zodiac signs make the best parents?
2 reasons why kids have anger issues
- Pregnancy Due Date Calculator This calculator tells you the estimated date of your delivery.

- Ovulation Calculator Calculate and understand your fertility window
LATEST VIDEOS
Parenting
- How to help your kids cope with divorce00:53
Japan needs Indian tech workers. But do they need Japan?
Funeral homes expose the reality of China's Covid toll
Smooth road ahead for BJP if the Oppn stays divided
Is Musk playing an elaborate joke at our expense?
Breastfeeding while mum or baby are sick
If you or your baby are unwell, you may wonder whether it’s safe to breastfeed. The good news is breastfeeding while sick can have many benefits for both of you – read on to find out more
The good news is breastfeeding while sick can have many benefits for both of you – read on to find out more
Share this content
Did you know that if you breastfeed, your baby is less likely to get ill in the first place? While it won’t completely stop her becoming sick, breast milk’s protective properties mean breastfed babies tend to be unwell less often,1 and recover faster, than formula-fed babies.
Breast milk has antibacterial and antiviral elements.2 Depending on how long you breastfeed for, you’ll be lowering your baby’s risk of contracting colds and flu, ear and respiratory tract infections, sickness and diarrhoea.1 Scientists are even investigating breast milk’s potential for treating conditions ranging from conjunctivitis to cancer.3,4
Should I breastfeed my sick infant?
Yes. Breastfeeding a sick baby gives her a great chance of a speedy recovery, as well as helping to comfort her. Your breast milk contains antibodies, white blood cells, stem cells and protective enzymes that fight infections and may help with healing.1,5,6 It also has a constantly adjusting balance of vitamins and nutrients, supporting her to get better as quickly as possible. And that means fewer sick days and visits to the doctor for both of you.7
Your breast milk contains antibodies, white blood cells, stem cells and protective enzymes that fight infections and may help with healing.1,5,6 It also has a constantly adjusting balance of vitamins and nutrients, supporting her to get better as quickly as possible. And that means fewer sick days and visits to the doctor for both of you.7
“Breastfeeding provides everything your baby needs if she’s poorly – it’s her medicine as well as her food, fluid and comfort. It’s the best thing on the planet for her,” says Sarah Beeson, a UK-based health visitor and nurse.
Amazingly, the composition of your breast milk changes when your baby is ill. If you’re exposed to a bacterial or viral infection, your body makes antibodies to combat it; these are then transferred to your baby through your milk.8 The levels of immunity-boosting cells, called leukocytes, in your milk also rise rapidly whenever your baby is unwell.5
And because breast milk is very easy to digest, it’s also the ideal food for babies with upset tummies.
“My daughter contracted norovirus when she was 12 months old, and breast milk was the only thing she could keep down,” remembers Maya, mum of two, Spain. We had weaned naturally to one breastfeed a day at bedtime, but the supply-and-demand effect of breastfeeding her more often again was quite astonishing. Within 48 hours, I was at dairy levels of production! It saved my baby girl being put on a drip.”
Bear in mind that you may have to alter the way you breastfeed your baby while she is sick. For example, a baby with a cold may want to feed more often, but for shorter periods, both for comfort and because a blocked nose may make it harder to stay at the breast for long. If your baby has a stuffy nose she might also prefer to feed upright, so you could experiment with different breastfeeding positions.
What if my baby seems too unwell to breastfeed?
Sometimes when a baby is feeling really ill she may not have the appetite or energy to breastfeed. If you’re struggling to get her to feed, contact a healthcare professional, lactation consultant or breastfeeding specialist for advice to prevent her becoming dehydrated.
They may advise you to express some milk to feed to your baby from a syringe, cup, or other method that you’ve found requires the least effort from her to drink from. Expressing when you would normally breastfeed will also keep your milk supply steady.
If you have any concerns about your baby’s health or milk intake, always seek medical advice quickly.
Can I still breastfeed when sick?
It may be the last thing you feel like doing, but it’s best to keep breastfeeding through almost any common illness. If you have a cold or flu, fever, diarrhoea and vomiting, or mastitis, keep breastfeeding as normal. Your baby won’t catch the illness through your breast milk – in fact, it will contain antibodies to reduce her risk of getting the same bug.
“Not only is it safe, breastfeeding while sick is a good idea. Your baby is actually the person least likely to fall ill with your tummy upset or cold, as she has already been in close contact with you and is getting a daily dose of those protective antibodies from your milk,” says Sarah Beeson.
However, being sick and continuing to breastfeed can be extremely tiring. You’ll need to look after yourself so you can look after your baby. Keep your fluid levels up, eat when you can, and remember your body needs extra rest. Book a seat on your sofa and snuggle up with your baby for a few days, and ask family or friends to help with caring for your baby when possible so you can focus on recovering.
“Don’t worry about your breast milk supply – you will keep producing it. Just don’t stop breastfeeding abruptly as you’ll run the risk of getting mastitis,” Sarah adds.
Good hygiene is important to minimise the risk of spreading the illness. Wash your hands with soap before and after feeding your baby, preparing and eating food, going to the toilet or changing nappies. Catch coughs and sneezes in a tissue, or in the crook of your elbow (not your hands) if you don’t have one with you, and always wash or sanitise your hands after coughing, sneezing or blowing your nose.
Is it OK to take medicines while breastfeeding?
It’s fine to take paracetamol, ibuprofen and some antibiotics while breastfeeding,9,10 as long as you discuss it with a healthcare professional and follow the dosing instructions. Remember ibuprofen has contraindications for asthmatic mums.
Remember ibuprofen has contraindications for asthmatic mums.
Previously mums were advised to avoid aspirin, but a recent study indicated low doses are likely to be safe while breastfeeding.11 However, high doses have been linked to a rare but serious condition called Reye’s syndrome in infants,12 so it’s best to discuss the use of aspirin with your healthcare professional.
Stronger prescription painkillers, such as codeine and tramadol, aren’t recommended.10 Since guidelines and recommendations are continually updated, your healthcare professional or pharmacist will be able to give you more information on specific medicines if you have any concerns.
Some cold, flu and cough remedies contain decongestants or expectorants, and these could reduce your milk supply. Steer clear of those that have phenylephrine, phenylpropanolamine or guaifenesin listed in their ingredients.9 Medicines that cause drowsiness are best avoided when you’re breastfeeding too.
“Check the packaging and if you’re still uncertain, ask a healthcare professional,” Sarah advises. “And if your baby was born prematurely, at a low birth weight, or has a medical condition, you should check before taking any medications while breastfeeding – even paracetamol.
“Whenever you go to a doctor or a pharmacist, for any reason, always make it clear you’re breastfeeding and ask for the best option,” she adds.
How about long-term medication?
If you’re on long-term medication for diabetes, asthma, depression or any other chronic health condition, the benefits of breastfeeding can outweigh the risks. “Breastfeeding is often still possible with nearly all illnesses, except for a few rare conditions,” says Sarah. “You’ll be familiar with your regular medications and should have an opportunity to discuss them with your doctor or specialist while pregnant. There is guidance available for all healthcare professionals on the safety of different drugs.” In any event, you should discuss this issue with your doctor or healthcare professional.
I was on a high dose of medication for my epilepsy but breastfeeding was still possible,” says Nicola, mum of one, UK. “I was monitored by my neurologist to get a balance between safety for my son and keeping my risk of a seizure low. Seizures can be triggered by lack of sleep and I was feeding day and night, but I took good care of myself, as did my husband. It’s been a positive experience.”
What if I have to go into hospital?
Whether you need planned or emergency treatment, there are ways to ensure your baby continues to receive the benefits of breast milk, and that you can continue breastfeeding once discharged.
“Express and freeze your breast milk so a caregiver can feed it to your baby. Have a practice ahead of time, and make sure you tell healthcare professionals you are a breastfeeding mum when you’re booked in, and again when you’re admitted,” suggests Sarah.
“If your baby is small, they may let you have her with you. Ask whether there’s a hospital lactation consultant or breastfeeding specialist you can see too – they’ll be a great advocate for you, especially if you’re on a general ward. If it’s an emergency, make sure the healthcare professionals know you have a baby – it’s not something they might think about otherwise.”
If it’s an emergency, make sure the healthcare professionals know you have a baby – it’s not something they might think about otherwise.”
Having surgery under local or general anaesthetic doesn’t mean you need to stop breastfeeding, or to ‘pump and dump’ your breast milk. By the time you feel well enough to hold your baby after an operation, the amount of anaesthetic in your breast milk will be minimal and it should nearly always be safe to breastfeed.10 However, you should seek the advice of a healthcare professional, lactation consultant or breastfeeding specialist in any of these circumstances.
Should I ever not breastfeed?
There are a few situations in which it’s safest to stop breastfeeding temporarily and pump and discard your milk to keep up your supply until treatment is complete. These include if you have radiotherapy or chemotherapy for cancer, herpes lesions on your breast, or infections such as tuberculosis, measles or septicaemia, that could be transmitted through your milk. 13,14 Seek expert medical advice about your condition and whether it’s best to continue or interrupt breastfeeding.
13,14 Seek expert medical advice about your condition and whether it’s best to continue or interrupt breastfeeding.
References
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Paediatr Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomised trials. [cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au/tropical-treatment-with-breastmilk-randomised-trials
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells. Adv Nutr. 2014;5(6):770-778.
Adv Nutr. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med. 2017;12(9):500-506.
11 Datta P et al. Transfer of low dose aspirin into human milk. J Hum Lact. 2017;33(2):296-299.
12 Morello O. Safe in breastfeeding [Internet]. Italy: Orfeo Morello; 2016. Aspirin: Can I take aspirin while breastfeeding? [cited 2018 Apr 4]. Available from: https://www.safeinbreastfeeding.com/aspirin/
13 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr (Rio J). 2004;80(5 Suppl):181-188.
J Pediatr (Rio J). 2004;80(5 Suppl):181-188.
14 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res. 2014;140(1):32-39.
Feeding when sick | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less prone to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often 1 and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed? nine0021
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. nine0009 7
“Breastfeeding gives the baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0009 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0009 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip." nine0003
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed? nine0021
Occasionally, if a child feels unwell, they may not have an appetite or the strength to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable. nine0003
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue to breastfeed if I become ill myself? nine0021
You may not want to do this if you feel unwell, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson. nine0003
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery. nine0003
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers. Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, certain medications are allowed. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues. nine0003
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged. nine0003
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account. nine0003
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, it is always best to consult your doctor or attending physician beforehand. nine0003
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. nine0009 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
nine0009 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page. nine0003
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. nine0120 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk".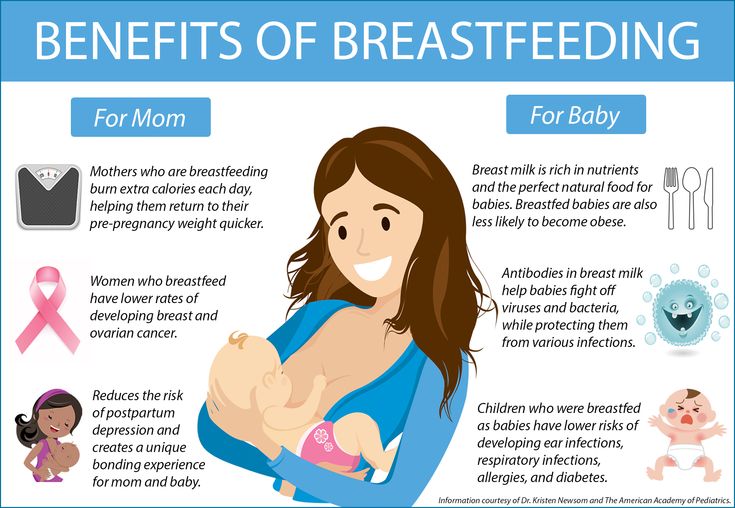 F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458. nine0120
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0120 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0120 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188. nine0120
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps". Indian W Med Res. 2014;140(1):32-39.
Indian W Med Res. 2014;140(1):32-39.
13 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am JClin Nutr. 2003;77(6):1537S-1543S. Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7
14 Prime et al., Simultaneous Breast Expression in Breastfeeding Women Is More Efficacious Than Sequential Breast Expression, Breastfeed Med. Dec 2012; 7(6): 442–447. Prime DK and co-authors. "During the period of breastfeeding, the simultaneous pumping of both breasts is more productive than consecutive." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447. nine0120
15 ClinicalTrials.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985. Clinical Research.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985.
Check out the instructions, consult with a specialist
* Ru FSZ 2010/07353 dated 07/19/10
** RU No. FCZ 2010/06525 dated 17/03/2021
FCZ 2010/06525 dated 17/03/2021
9000 9000 9000 9000 9000
000 Is it possible to breastfeed at a temperature: what to do if a nursing mother or child is ill
High temperature during breastfeeding makes mothers pretty nervous. How to help yourself with an illness and not harm the baby? Not so long ago, breastfeeding at a temperature was undesirable. They advised either to stop breastfeeding or to express and boil milk. Although today doctors are against such recommendations, they still insist that self-medication in a nursing mother is not acceptable.
First of all, it is necessary to deal with the cause of the fever. Only in exceptional cases is it possible to interrupt breastfeeding. An accurate diagnosis should be made by a doctor and prescribe medications that can be combined with breastfeeding. nine0003
pixabay.com
Breast milk is the best food for a baby's health. But the process of feeding is also useful for a woman. Breastfeeding helps to avoid mastitis, increases resilience to stress and reduces the risk of breast cancer by 50%.
Breastfeeding helps to avoid mastitis, increases resilience to stress and reduces the risk of breast cancer by 50%.
But what to do if a nursing mother has a fever?
Fever is a symptom that indicates a malfunction in the body. The first thing to do is to deal with the cause of the rise in temperature. The exact diagnosis will depend on the treatment regimen that will not harm the child. nine0003
The American Academy of Pediatrics states that in most cases, it is not necessary to stop breastfeeding if you have a fever. Milk contains antibodies that protect the baby from infection. In addition, the abrupt cessation of breastfeeding can cause mastitis in the mother and deprive the child of natural protection, since infant formulas do not contain antibodies.
Is it possible to breastfeed with a cold? In this case, you should not wean the baby from the breast and you should continue to feed on demand. If the child managed to catch the virus from the mother, then the antibodies in the milk will help him recover faster and more easily endure the disease.
 nine0003
nine0003 When visiting a doctor or pharmacy, be sure to tell them that you are breastfeeding. In this case, you will be prescribed medicines that are compatible with feeding your baby. For example, let's take ibuprofen or paracetamol if the temperature has risen during HB.
A breastfeeding mother should also adhere to the rules of hygiene in case of SARS:
- wash hands after going outside, going to the toilet, changing diapers;
- wash hands after sneezing, blowing nose and coughing, before and after feeding; nine0398
- ventilate and humidify the room.
High temperatures (above 38°C) do not affect the production and quality of breast milk. But in any case, you should consult with your doctor in order to get quality care and prevent complications.
In addition, breastfeeding should not be interrupted at a temperature caused by mastitis, unless it is complicated by a purulent process. In the absence of severe pain and pus, breastfeeding can be continued. nine0003
nine0003
Sometimes the benefits of breastfeeding far outweigh the possible risks, so doctors do not always advise against breastfeeding during long-term treatment or hospitalization of the mother. In the first case, there are drugs and even antibiotics that are compatible with breastfeeding. In the second case, you can express and freeze milk for feeding from a bottle.
But with mild acute respiratory infections, and with more serious illnesses that are accompanied by high fever, you should definitely consult with your doctor. nine0003
Fears associated with taking medication during breastfeeding and pregnancy are dispelled by the famous pediatrician Yevgeny Komarovsky in his program “School of Doctor Komarovsky”
or immediately after, the thermometer will show 37. Even if a nursing mother is ill, in most cases breastfeeding is not cancelled. Protective antibodies continue to be produced in mother's milk, which prevent the baby from catching a cold or diarrhea. But at this moment, a woman needs additional help and care in order to cope with the disease and feed the baby. The abrupt cancellation of breastfeeding, on the contrary, will have a bad effect on the condition of the child and the health of the mother. nine0003 When breastfeeding at a temperature should be abandoned: On the advice of a doctor, you will need to either temporarily stop breastfeeding or switch to infant formula. nine0003 pixabay.com The uniqueness of breast milk is that it is not only food for a growing baby, but also a medicine. Therefore, an increase in temperature in an infant does not become a reason to cancel breastfeeding. In addition to being rich in nutrients, mother's milk helps the baby fight off an infection or virus. For this, protective enzymes, leukocytes and antibodies are produced in it. The most amazing and soothing thing for mothers is that when a child is sick, the composition of milk changes to help him recover faster. It increases the level of white blood cells, which strengthen the baby's immune system. nine0003 Not to mention that the process of breastfeeding is a period of close communication for mother and baby. This helps the sick child to calm down and be comforted. 1-37.3 ° C even in a healthy woman. Therefore, for reliable information it is better to measure the temperature 25-40 minutes after feeding .
1-37.3 ° C even in a healthy woman. Therefore, for reliable information it is better to measure the temperature 25-40 minutes after feeding .
Is it possible to breastfeed when a child has a temperature