Methods of feeding babies
Baby-Led Weaning is a New Way of Feeding Your Baby - Learn More About it
Every parent remembers when they first introduced their baby to solid foods. This momentous occasion of spoon-feeding them pureed food is considered a major milestone for babies and their parents.
Today however, more and more parents are opting to skip the applesauce and mashed sweet potatoes and instead are adopting a new feeding technique called “baby-led weaning” ( or BLW) for their babies. This alternative approach to feeding, first introduced in the UK a decade ago, involves introducing solid chunks of foods much earlier on by placing them on the baby’s high chair and letting them grasp the food and feed themselves directly. As the name implies, feeding time is led by the baby as they determine the pace and the amount of food they consume; basically, baby-led weaning puts the baby in charge.
While children all develop at different paces, advocates of baby-led weaning agree that this method of eating shouldn’t be introduced until the baby is ready. Cues to begin BLW include making sure that your baby can sit up straight unassisted, have good neck strength and be able move food to the back of their mouth with up and down jaw movements. Most babies develop these skills by the sixth month, but some babies may not fully develop them until they are nine months old.
Proponents of BLW believe that it holds many benefits, including enhancing baby’s hand-eye coordination and other fine motor skills, including using their thumb and index finger to grasp their food. They also feel that it will produce healthier eaters than spoon-fed babies because BLW eaters get to choose how much they eat as opposed to traditional feeding methods, which sometimes results in force feeding. Other advantages that BLW supporters claim to be true is that it creates a more enjoyable feeding experience for babies and less stress on their parents.
Detractors of baby-led weaning feeders point out that these babies are generally underweight as compared to spoon-fed babies because they simply do not ingest that much when they are first introduced to this way of eating due to difficulties grabbing food. BLW babies also tend to be iron-deficient because they aren’t consuming the iron-fortified cereals that spoon–fed babies typically eat. Lastly, a big concern for many parents is the increased choking hazards associated with BLW, and while the American Academy of Pediatrics doesn’t have opinion of BLW, they do state that babies are ready for solid food once they are ready to sit up on their own and bring their hand to their mouth.
BLW babies also tend to be iron-deficient because they aren’t consuming the iron-fortified cereals that spoon–fed babies typically eat. Lastly, a big concern for many parents is the increased choking hazards associated with BLW, and while the American Academy of Pediatrics doesn’t have opinion of BLW, they do state that babies are ready for solid food once they are ready to sit up on their own and bring their hand to their mouth.
If you are considering baby led weaning for your child, here are a few tips:
- Continue breast feeding and / or formula feeding as this will continue to be your baby’s biggest source of nutrition until they are 12 months old.
- Begin BLW feedings with softer foods, such as ripe fruits, cooked egg yolks, and shredded meats, poultry and fish.
- Avoid foods that can pose as choking hazards, such as nuts, grapes, popcorn, or foods cut into coin shapes, like hot dogs.
- Do not leave your child unattended during BLW feeding times.
 Continue to supervise and socialize with them while they eat and to have them eat when the rest of the family does.
Continue to supervise and socialize with them while they eat and to have them eat when the rest of the family does. - Don’t panic if your baby gags as it is a safe a natural reflex. Instead of overreacting, prepare for a choking event by familiarizing yourself with the infant-specific Heimlich maneuver.
- Introduce new foods one at a time to pinpoint potential food allergies. A recommended length of time is three to four days between foods.
- The goal of BLW is to let your baby explore eating at their own pace. This may include the smashing, smearing, or dropping of food, so prepare for a mess.
Before you decide to adopt BLW to your child, it is a good idea to discuss with your child’s pediatrician as it may not be a good idea for all babies, especially those babies with known developmental delays or neurological issues.
To make an appointment with a pediatrician at Flushing Hospital’s Ambulatory Care Center, please call 718-670-5486.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment.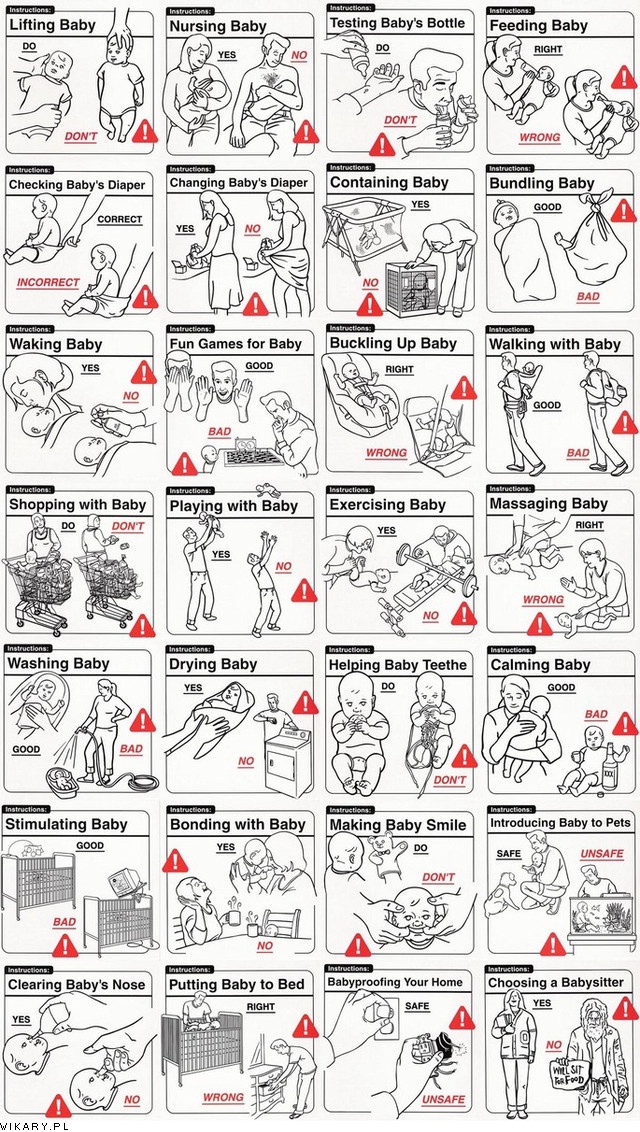 Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.
Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.
How should I feed my baby? | Baby Feeding Methods
In this series Breastfeeding Your Baby Mastitis and Breast Abscess Bottle-feeding Your Baby Weaning Your Baby Feeding Your Toddler
How should I feed my baby?
One of the first decisions you will make, after your baby is born, is how to feed him or her. Most mums will have the choice of either breastfeeding or bottle-feeding from the start.
How stopping breastfeeding can impact your mental health
It's common for new parents to struggle with their mental health. New parenthood comes with a wh...
Should I breastfeed or bottle-feed?
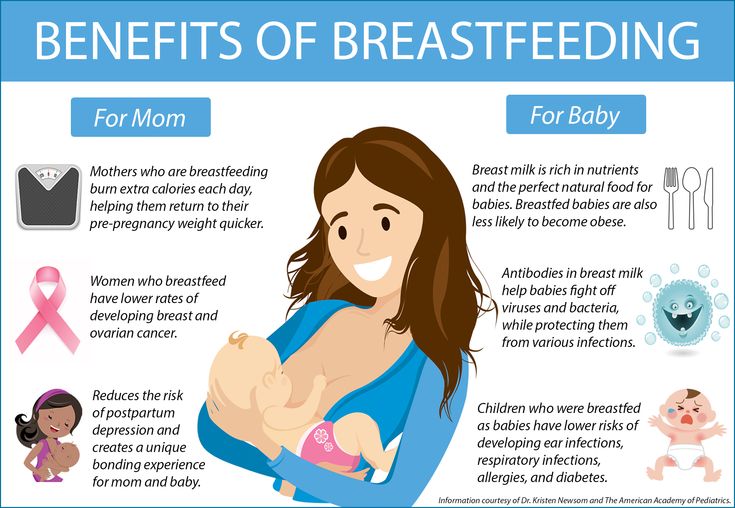
The benefits of breastfeeding for you and your baby are so great that experts recommend that, in almost every circumstance, breastfeeding your baby for the first six months is the best option for both your health and your baby's health, even in countries where infant formula is easily obtained and water supplies are clean and safe. Nevertheless, deciding whether to do this is a personal decision and you need to consider both the pros and cons of both types of feeding for you and your baby. You don't have to choose completely between them - you can do both, for different periods of time and in different proportions. Each approach has advantages and disadvantages, and to help you think them through we have listed the main ones here:
Nevertheless, deciding whether to do this is a personal decision and you need to consider both the pros and cons of both types of feeding for you and your baby. You don't have to choose completely between them - you can do both, for different periods of time and in different proportions. Each approach has advantages and disadvantages, and to help you think them through we have listed the main ones here:
Advantages of breastfeeding to your baby
- Breastfeeding provides your child with the perfect, tailor-made source of nutrition, the one that nature evolved for them. It is the easiest food for them to digest, so it possibly causes less gas and colic.
- Breast milk, particularly first milk, helps protect your baby from illness during infancy, particularly tummy bugs and ear infections. It also reduces the incidence of cot death (sudden infant death syndrome).
- Breastfeeding has lasting benefits for your baby's metabolism, reducing the chance of obesity and diabetes, and of allergies like eczema, later.

- Breastfeeding makes feeding simple: no other fluids (such as water) are needed for a breast-fed baby. In the hottest weather, the breast milk composition changes, to provide everything your baby needs.
- Breastfeeding enhances the bonding process between baby and mother. Being cuddled naked, against the mother's bare skin for as long as possible at birth, is important. This can of course be done even if you do not breastfeed.
- Babies generally 'take to' the taste of breast milk quickly, whereas not all babies like the taste of all bottled milks.
- A breast-fed baby's bowel movements are less smelly and are not irritating to a baby's skin. Breast-fed babies are less prone therefore to nappy rash.
- Breast-fed babies don't usually get diarrhoea or constipation.
- Breast-fed babies tend to be less fussy at weaning.
- Breast milk appears to help loosen a newborn baby's mucus and it acts as a laxative helping with the passage of the first poo (meconium).

- Breast-fed babies perform slightly better in intelligence tests in early childhood.
- Breastfeeding is comforting for you and your baby (although this can equally be true of bottle-feeding).
Advantages of breastfeeding to you
- Breastfeeding will help speed your recovery from childbirth, particularly the shrinking down of your womb after delivery.
- Breastfeeding helps you manage the initial breast 'engorgement' which often appears around day 3-4 and which can be very uncomfortable.
- Breastfeeding is convenient: you don't have to prepare bottles. It is also the cheapest option - it's free.
- Breastfeeding slightly reduces the chance of postnatal depression.
- Breastfeeding gives you later protection, to some degree, against ovarian and breast cancer. It also decreases your chances of developing 'thinning' of the bones (osteoporosis), diabetes and obesity as you age.
- Night-time feedings are easier and quicker when you breastfeed, meaning that you get more sleep.

- Breastfeeding usually delays the return of your period for three months or more. Whilst you are breastfeeding exclusively, your fertility is suppressed for up to six months - a natural birth control method which is up to 98% effective.
- Pumping or expressing your breast milk can give you some freedom, allowing you to spend time away from your baby yet continue to provide breast milk, and giving your partner the ability to participate in feedings.
- Exclusive breastfeeding for the first six months of life provides the maximum benefit. However, any breastfeeding that you do will bring you and your baby benefits.
Advantages of bottle-feeding
- You have more flexibility in being away from your baby if you have to work, for example. (Although you can express or supplement breastfeeding with bottle-feeding, in the first few days when your breast milk supply is just establishing this is not so easy to do, so you can't easily be away from your baby.
 )
) - Breastfeeding can be tiring, especially during the first few weeks when you are feeding your baby on demand. Bottle-feeding is easier to delegate when you are tired, allowing you to rest properly and have more energy overall.
- Breastfeeding can be painful: common problems include breast engorgement, leaking, sore nipples and infection of the breast (mastitis). Bottle-feeding allows your breasts to settle down more quickly after pregnancy.
- Your partner can't breastfeed, and may feel a little left out (although you can express to allow them to bottle-feed).
- You may find breastfeeding in public awkward and embarrassing, making it difficult to go out with your baby. Bottle-feeding removes this worry (whether feeding expressed milk or formula).
- Bottle-feeding allows you to see how much milk your baby has taken, which you may find reassuring.
- Breastfeeding can be difficult at first. Not all babies latch on immediately and breastfeed well, and you may find breastfeeding stressful and be unsure whether your baby has fed properly.

- Breastfeeding can be particularly difficult if you have more than one baby to feed; partially or completely using bottles may help you manage.
- Women who have had surgery to their breasts, including cosmetic surgery, can have a decreased flow of breast milk - the effect depends on precisely what surgery they have had.
- Some women worry that they cannot produce enough milk to satisfy their baby, and bottle milk relieves this anxiety.
- Bottle-feeding may be safer for your baby if you need to be on medications which would enter your breast milk and be harmful for your baby, or if your baby needs a specially adapted milk because they have a medical condition.
- Women who are HIV positive are advised not to breastfeed unless in a country or situation where safe supplies of formula and water are not readily available.
- Other, practical reasons why your baby might need to bottle-feed include you not being with your baby (for example, because of adoption, prematurity, or sickness in you or your baby, or because you need to return to work early).
- If your baby is born before 32 weeks it can be harder to establish your breast milk supply, so some bottle-feeding may take the pressure off you as you try to establish your supply.
- Some women just prefer the idea of bottle-feeding (although they may be able to express for a while if they want to give their baby breast milk).
Advantages of combination feeding
Breastfeeding or bottle-feeding doesn't have to be all or nothing. You can breastfeed fully or partly, and many mums combine breastfeeding and formula feeding, and breast-milk pumping, in differing proportions. It's easiest to begin combination feeding once you have breast-fed for six weeks so that your supply is fully established; however, you can try it sooner if you need or want to.
Combining breastfeeding with bottle-feeding offers the advantages and disadvantages of both options. It makes you more flexible, as you can move between the two, which might suit you if, for example:
- You want to breastfeed but would like your partner to share in the feeding routines
- You want to breastfeed but also to preserve your energy and offer the baby the best of both worlds
- You are breastfeeding but want to be able to give bottles of formula for one or more feeds so that you can get some rest
- You began by bottle-feeding your baby and have decided that you want to start breastfeeding
- You need to leave your baby and want to make sure they have some milk while you're away
- You have twins or more and feel this would be more manageable
Introducing formula feeds will tend to reduce the amount of breast milk you produce and this is more so if you do so in the first six weeks, whilst your breast-milk supply is adjusting to an 'even keel'. Your baby also has to learn to use a different kind of suck at the bottle than at the breast. However, with perseverance many mothers manage it successfully.
Your baby also has to learn to use a different kind of suck at the bottle than at the breast. However, with perseverance many mothers manage it successfully.
How do I express breast milk?
You might want to express milk because your breasts are engorged and you want to relieve the pressure, because your baby is very premature and not yet able to suck (see below), or because you need or want someone else to be able to feed your baby too. Expressing your own breast milk is a technique you can learn quite quickly, although it may take a little practice at first. Expressing breast milk is as it sounds: you 'milk' your breast for the supply it contains, and store the expressed milk so that you (or someone else) are able to give it to your baby from a bottle.
You can express milk using a pump (hand or electric) or by hand (often easiest at first). You can rent 'hospital-grade' breast pumps, which are the most effective. You can keep expressed milk in the fridge for up to five days, or freeze it for up to six months.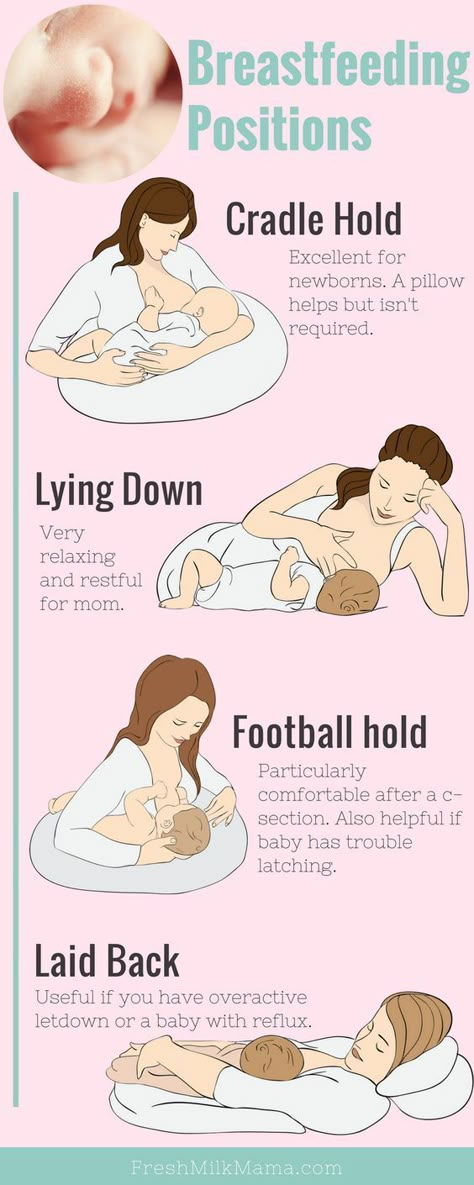
More detail on how to express breast milk is given in the separate leaflet called Breastfeeding Your Baby.
How should I feed my newborn baby?
You should offer your newborn baby a feed as soon as possible after birth. You can usually choose breastfeeding or bottle-feeding from the very start. Breastmilk, particularly early breast milk, is massively beneficial for your baby, and for this reason many mums who want to bottle-feed decide to breastfeed for the first couple of weeks. This means that they give their baby the important first milk (colostrum) before switching over to formula.
Your midwife will be there to help you establish feeding, until you can do it confidently without help, so you won't be doing this alone.
How often will my baby want to feed immediately after birth?
Straight after birth your baby will, like you, be tired and probably hungry. Some babies will want to feed straightaway; others may seem less keen to do so. Your midwife will encourage your baby to feed in the first hour after birth, as this helps both you and your baby recover from labour. It is particularly important for the babies of mums with diabetes to be encouraged to feed in the first half an hour or so after birth, as these babies can be particularly prone to developing low blood sugar otherwise.
It is particularly important for the babies of mums with diabetes to be encouraged to feed in the first half an hour or so after birth, as these babies can be particularly prone to developing low blood sugar otherwise.
Babies will vary greatly as to whether they will want to keep feeding in the first few hours after birth, or as to whether they seem to need a sleep. Newborn babies should be allowed to feed as often as they wish. If the baby is sucking actively they should be kept on the breast or bottle until they slow or stop. If you are breastfeeding you should offer the second breast before stopping (because it may be that the flow has slowed in the first breast but your baby is still hungry).
Will I have any milk in the first few hours?
When your baby is born your breasts will already be producing colostrum, which you may have noticed leaking from your breasts in late pregnancy. This yellowish 'milk' is a bit thicker than mature breast milk. Colostrum is only produced for the first few days of your baby's life, after which it gradually changes (and increases in quantity) to mature breast milk.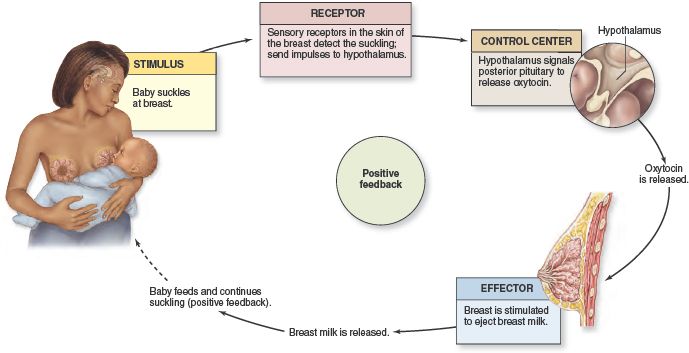 Colostrum is very important to your baby. Even if you don't plan to breastfeed in the long term, any colostrum that you feed your baby will have long-term value to him or her.
Colostrum is very important to your baby. Even if you don't plan to breastfeed in the long term, any colostrum that you feed your baby will have long-term value to him or her.
What is colostrum?
Colostrum is a milky yellow 'first milk' which contains proteins, carbohydrates, fats, vitamins, minerals, antibodies and immune cells that fight disease-causing agents such as bacteria and viruses. It helps you pass on to your baby the immunity you have 'earned' through fighting infections yourself. This is hugely helpful to your baby, whose own immune defence system is not yet fully developed. Having their mother's colostrum reduces tummy and ear infections in babies in later childhood. Colostrum also helps prevent babies from developing early jaundice.
Many mothers who don't want to go on to breastfeed decide to give their baby that vital, initial colostrum. After this, over the first two weeks the milk gradually changes from colostrum through a 'transitional milk' to 'mature' breast milk. In the first 24 hours after the birth you will produce about 40 ml of colostrum, and your baby will take about a fifth of this during a feed.
In the first 24 hours after the birth you will produce about 40 ml of colostrum, and your baby will take about a fifth of this during a feed.
How does feeding my baby the colostrum help my body?
Breastfeeding in the minutes and hours just after your baby is delivered helps your womb expel the afterbirth (placenta) more efficiently and then helps it contract firmly down towards its pre-pregnant size. This helps kick-start the process of your own return to normal shape and can also help relieve the breast engorgement that usually arrives around day 3-4 after birth (whether or not you breastfeed).
How do I feed my premature baby?
Premature babies are ideally given breast milk from birth, although before 32 weeks of gestation they may not yet be strong enough to feed directly. If you are making milk and your baby is strong enough to suckle, you will usually be encouraged to breastfeed, as breastfeeding is particularly helpful for premature babies. If you are unable to breastfeed initially, or decide not to, your premature baby may be given formula milk or, occasionally after discussion with you, expressed donor milk.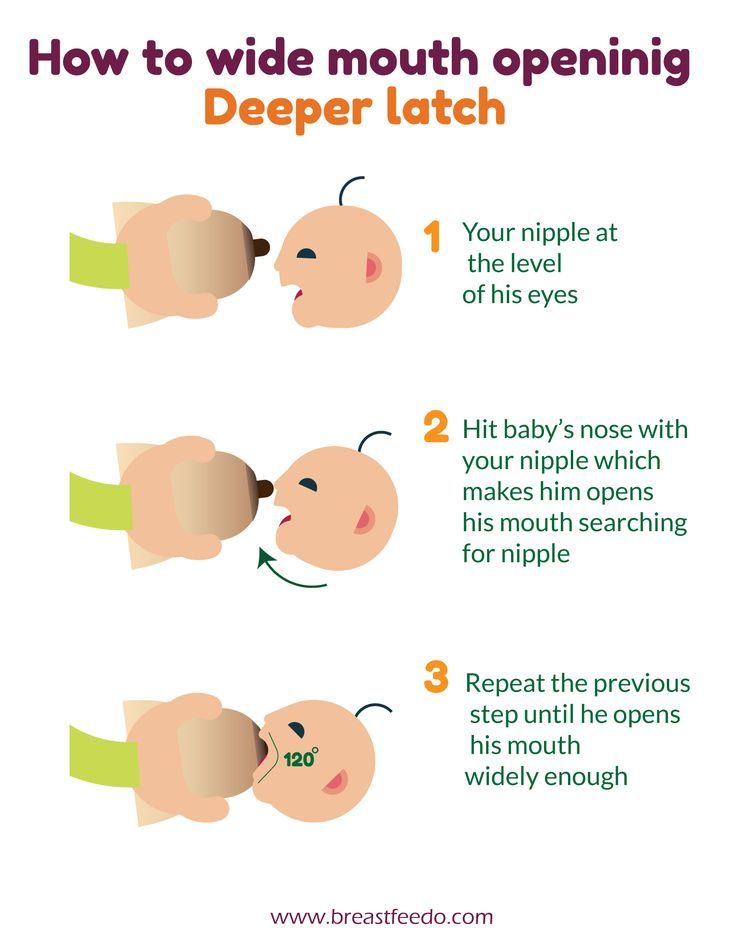
- If your baby is extremely premature, his or her digestive system may not yet be mature enough to have food in the stomach, so feeding may need to be into a vein using a special nutrient rich solution called TPN (this stands for total parenteral nutrition).
- Premature babies who are ready to digest milk but not yet strong enough to suckle, may be given breast or formula milk through a tiny tube which goes to the stomach. Ideally your own breast milk will be used, if you can express it. Premature babies may also need food supplements, or special premature baby formula, to make up for the time in the womb that they have missed.
- If your baby is very early it may take a little while for you to produce milk. However, if you keep expressing regularly, eight times a day, the milk is likely to come in. Whilst your milk supply isn't fully established then the team may talk consider using donated human breast milk or formula, until you can replace it with your own breast milk.

- Your baby may continue tube feeding while they are learning to feed from the breast, from a cup or from a bottle, to make sure they get enough food.
How do I express breast milk for my premature baby?
To express milk for your premature baby, you should start hand expressing within six hours of delivering your baby. You'll need to do this eight to ten times a day, including once during the night. In the first few days you may make only a few drops of milk each time, which can seem like very little, but every single drop counts.
How many calories are there in colostrum and breast and formula milk?
Colostrum has around 50 calories per oz and mature breast milk has 60-75 calories, as does infant formula. When producing mature milk, each breast will produce 'richer' milk with a higher fat content towards the end of a feed when it is nearly empty, so it is important that breastfeeding babies get the opportunity to empty one breast before feeding from the other, so that they can access this richer milk.
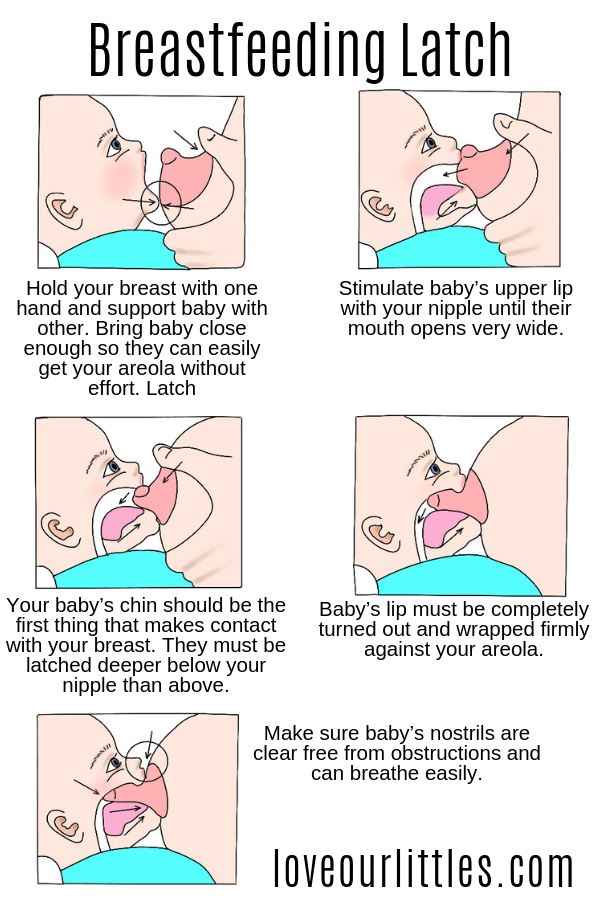
How do I breastfeed my baby?
See the separate leaflet called Breastfeeding Your Baby.
How do I bottle-feed my baby?
See the separate leaflet called Bottle-feeding Your Baby.
Can I go back to breastfeeding after bottle-feeding?
You can restart breastfeeding for weeks or even months after you have stopped, if you want to do so. It can take a little perseverance, but there are a few things which may help your milk to come back in:
- Hold your baby as much as possible, skin to skin.
- Express your breast milk around eight times a day - this releases the hormone prolactin, which stimulates your breasts to make milk. It may be easier to express by hand to begin with, although pumps are also available.
- If your baby is latching on but you don't yet have much milk, feed little and often, when your baby is relaxed and not too hungry.
- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid.
 This is a tiny tube which is taped next to your nipple and goes to your baby's mouth, so that when your baby suckles on your nipple he or she can get milk via the tube as well as from your breast. This helps keep your baby suckling, giving your breasts the stimulation they need to keep producing milk.
This is a tiny tube which is taped next to your nipple and goes to your baby's mouth, so that when your baby suckles on your nipple he or she can get milk via the tube as well as from your breast. This helps keep your baby suckling, giving your breasts the stimulation they need to keep producing milk.
Can I breastfeed if I adopt?
It can be possible to breastfeed even if you have not just had a baby - it is called adoptive nursing. The principle is that repeated stimulation of the nipples triggers milk production. It is more difficult to trigger milk production if you have not been pregnant recently. This is because although the milk production itself is triggered by nipple stimulation, you won't have the high levels of pregnancy hormones that also prepare your body for breastfeeding by enlarging and sensitising the milk-producing apparatus. But it is possible.
It can take considerable perseverance to get a good supply of milk, but a lactational aid (as those described above) can be very helpful in persuading the baby to keep suckling, delivering the stimulation needed to create a milk supply.
How do I wean my baby?
Weaning is the gradual introduction of additional food to your baby, on top of infant formula or breast milk. See the separate leaflet called Baby-led Weaning.
What is the best way to help my baby eat a balanced diet after he or she is fully weaned?
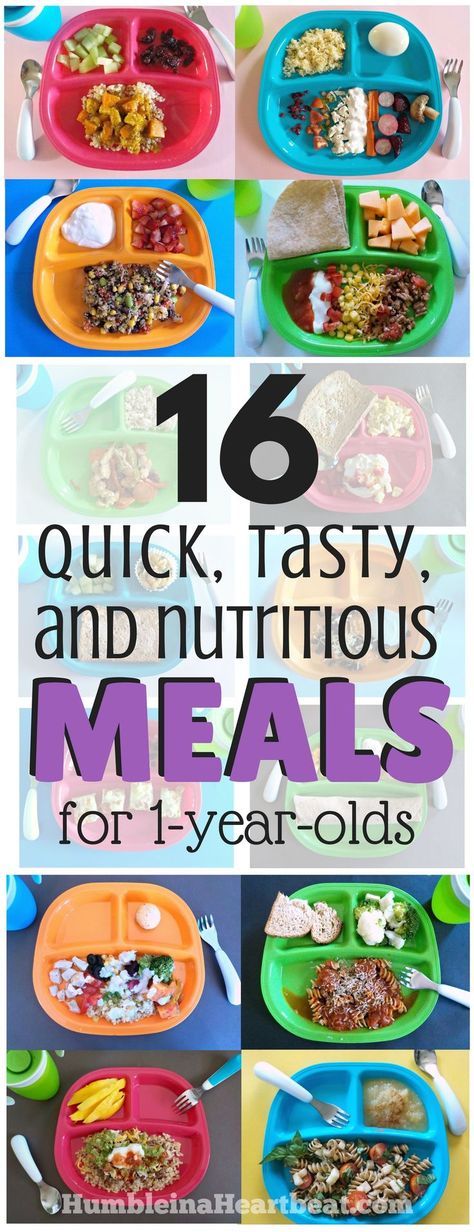
Feeding children over the age of 12 months is both an art and a science. Your aim is to encourage healthy tastes and eating habits, which will set your child up for life.
See the separate leaflet called Feeding Your Toddler.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. nine0011 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
nine0011 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time! nine0018
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding. nine0018
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help.
 The specialist will also be able to show you how to hold your baby more comfortably.
The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance. nine0003
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2. 7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ” nine0003
7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ” nine0003
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding.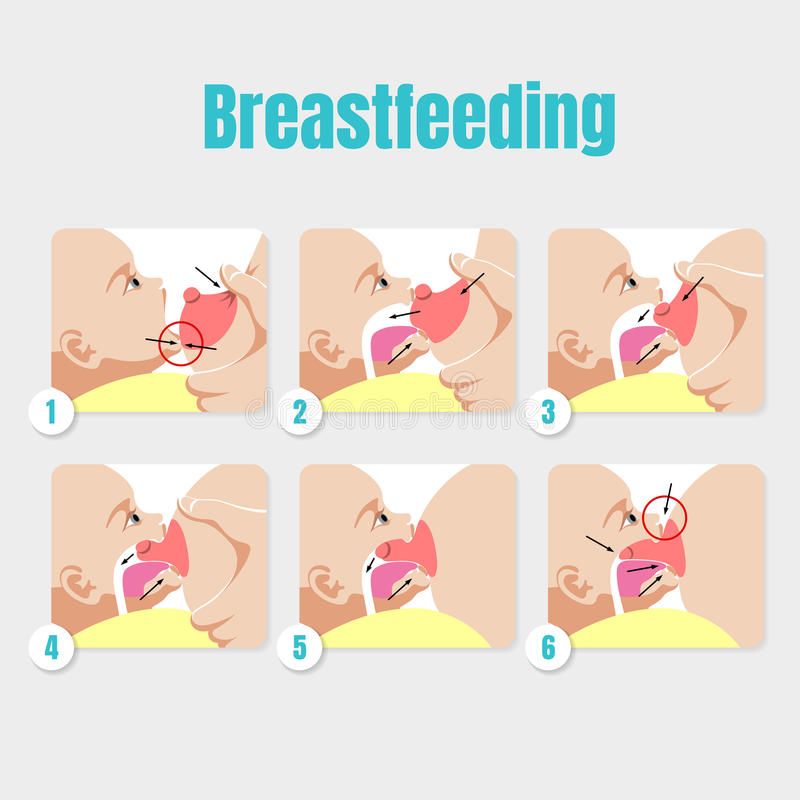 The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided. nine0003
The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided. nine0003
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost exactly like the cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand. nine0003
Julie, a mother of two from the UK, finds this position very practical: “I usually feed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above). nine0003
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This pose is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.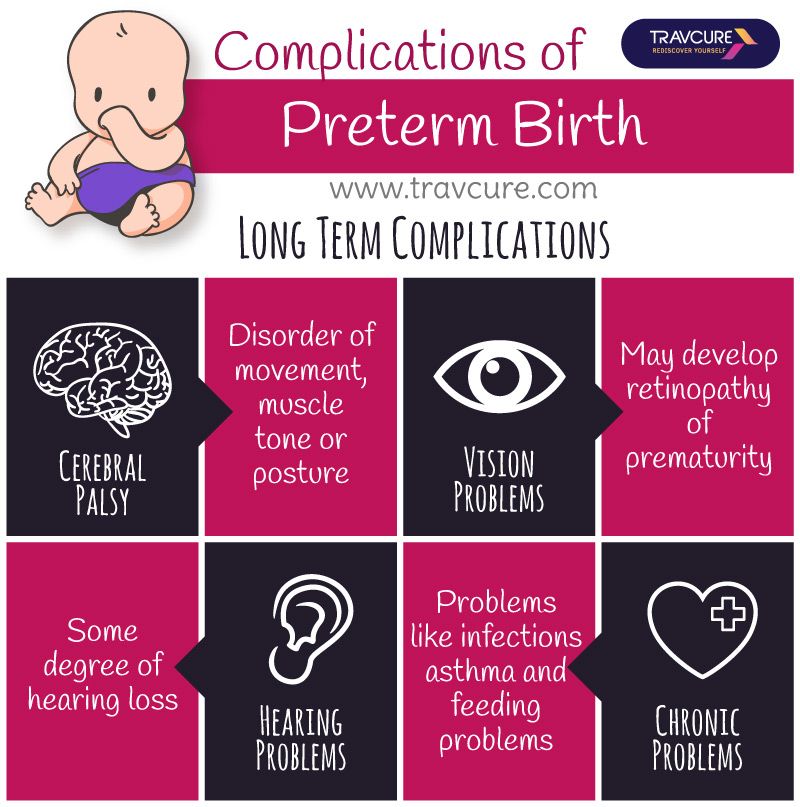 nine0003
nine0003
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time. ” nine0003
” nine0003
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she grew older, she became much better at grabbing her breasts in normal positions, ”says Sarah, mother of two children from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone. nine0003
4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone. nine0003
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain. nine0003
Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain. nine0003
“I have breastfed several times in the overhang position for clogged milk ducts when no other means of resolving the clogs worked. And this pose seems to have helped. I think it’s because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful. nine0003
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK.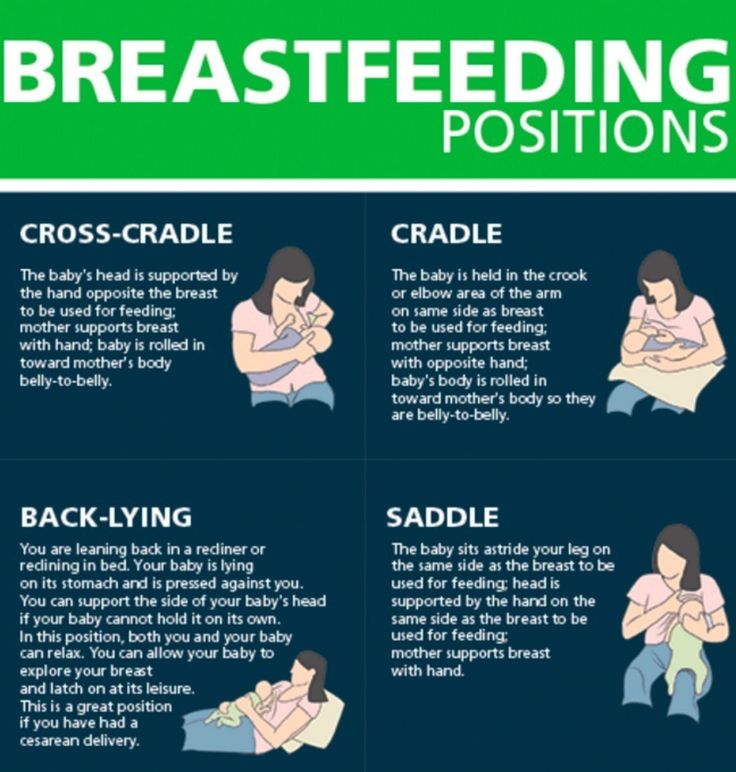 - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
- This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores. nine0003
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest. nine0003
nine0003
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second. nine0003
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other). nine0003
nine0003
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast. nine0003
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. nine0133 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors.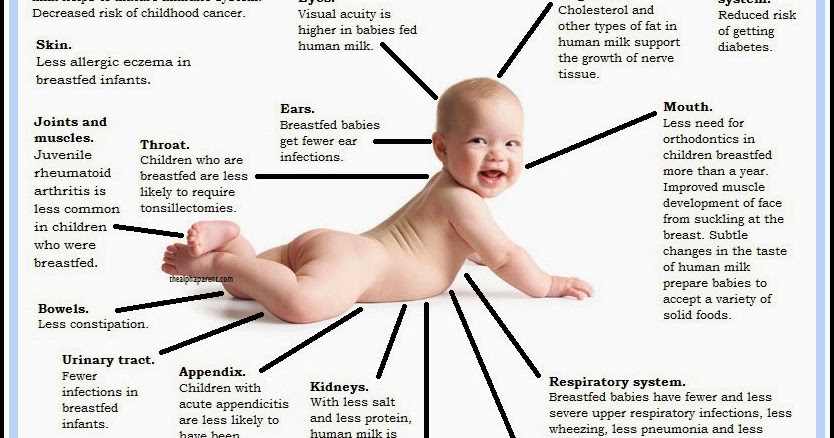 Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Features of feeding premature babies
Successful nursing of premature newborns, in addition to therapeutic measures, largely depends on the creation of optimal external conditions and adequate nutrition. According to the modern theory of nutrition programming , the quantity and quality of nutrients supplied during the prenatal period and the first months of a child's life determines the nature of metabolism and, as a result, affects a person's health throughout later life. nine0003
Proper and nutritious nutrition in the early stages of life affects the overall development of the child, and also contributes in direct proportion to reducing the development of chronic diseases in adulthood (such as diabetes and arterial hypertension).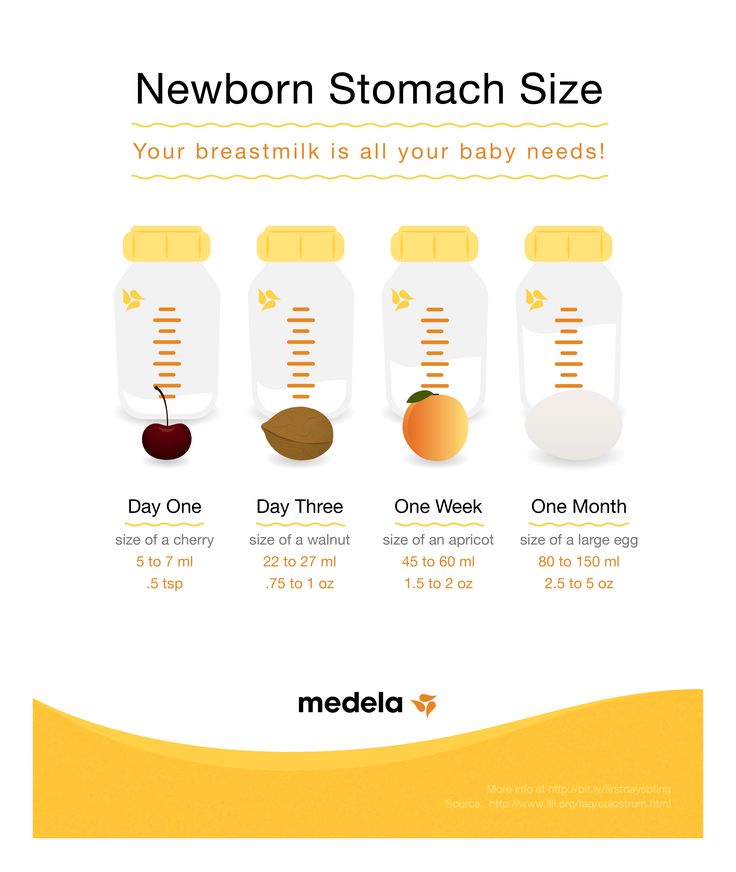
The purpose of enteral nutrition is to provide the body with the nutrients it needs to grow and develop.
Providing a premature newborn with an optimal amount of nutrients is quite difficult, given the morphofunctional immaturity of the digestive system and the lability of metabolic processes. The relatively high need of premature infants for nutrients is in conflict with the limited ability to assimilate them. nine0003
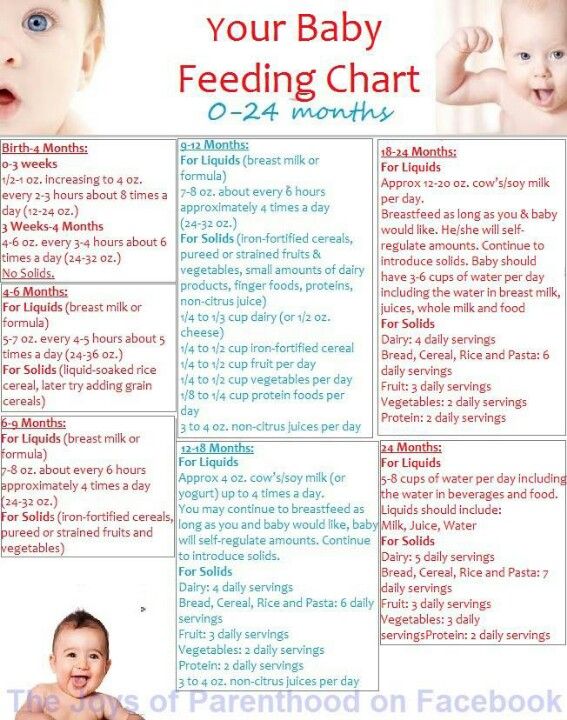
Feeding methods for premature babies are determined by the severity of their condition and depend on the body weight and gestational age of the baby at birth.
Successful feeding of a newborn is possible when sucking, swallowing and breathing become well coordinated.
The swallowing reflex is well developed already by 28-30 weeks of gestational age, but it is very quickly depleted. Fully matures by 34 weeks of gestation. When does sucking and swallowing coordinate? Already at 28 weeks of gestational age, all the components of sucking and swallowing take place, but the child is not yet able to coordinate them.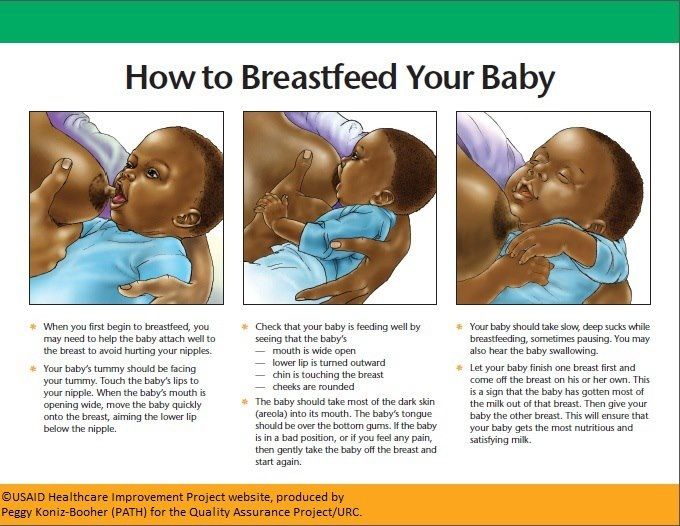 Partially, this occurs by 32-34 weeks of gestation. Coordination of sucking and swallowing fully matures around 36-38 weeks of gestational age. From 37 to 38 weeks of gestational age, newborns are able to coordinate sucking, swallowing, and breathing without difficulty. nine0003
Partially, this occurs by 32-34 weeks of gestation. Coordination of sucking and swallowing fully matures around 36-38 weeks of gestational age. From 37 to 38 weeks of gestational age, newborns are able to coordinate sucking, swallowing, and breathing without difficulty. nine0003
When feeding premature babies, you should pay attention to four points: when, what, how much, what method to feed .
The first feeding should be started as soon as it becomes clinically possible. Earlier introduction of breast milk helps to reduce the frequency of infections, maturation of the gastrointestinal tract, immune functions, and improved calcium metabolism.
Newborns weighing more than 2000 g and gestational age more than 33 weeks, who do not have other diseases, can be attached to the mother's breast as early as the first day of life. In this case, you should carefully monitor the appearance of signs of fatigue (cyanosis of the nasolabial triangle, shortness of breath, etc.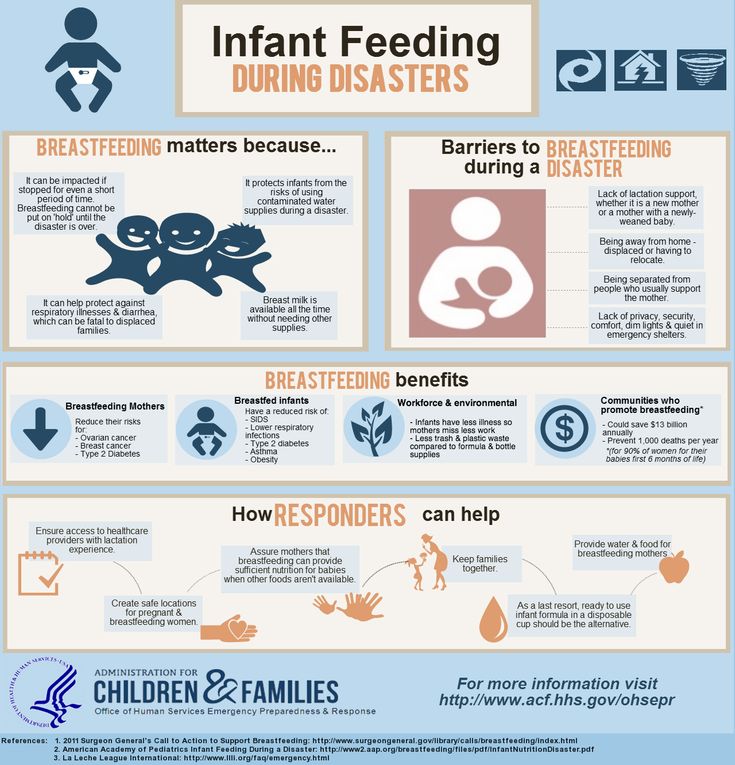 ). Their appearance is an indication for the transition to feeding expressed breast milk from a bottle. Efforts should be aimed at preserving breast milk as much as possible, taking into account the special biological value of mother's native milk for an immature child and the important role of mother-child contact during feeding. For premature babies, free feeding is unacceptable due to their inability to regulate the amount of sucked milk and the high incidence of perinatal pathology. nine0003
). Their appearance is an indication for the transition to feeding expressed breast milk from a bottle. Efforts should be aimed at preserving breast milk as much as possible, taking into account the special biological value of mother's native milk for an immature child and the important role of mother-child contact during feeding. For premature babies, free feeding is unacceptable due to their inability to regulate the amount of sucked milk and the high incidence of perinatal pathology. nine0003
Babies born before 33 weeks' gestation are usually tube-fed to avoid the risk of aspiration resulting from a lack of coordination between sucking and swallowing. With a non-severe condition of the child and a body weight approaching 2000 g, a trial feeding from a bottle can be carried out, with unsatisfactory sucking activity, tube feeding is prescribed in full or in part. In order to maintain and maintain lactation in the mother, regular expression of breast milk is necessary. nine0003
Enteral feeding of very preterm infants (weighing less than 1500 g and less than 30 weeks' gestation) is carried out through a tube.
The caloric method is used to calculate the required amount of feeding for premature babies. The calorie content of the diet of a prematurely born child increases gradually and daily.
Caution and Graduality Feeding Guidelines for Premature Babies Less Than 33 Weeks Gestational Age Less Than 2000g
For a premature baby, the best bioavailability is the milk of a woman who has given birth prematurely, then formulas for premature babies, and then the milk of a woman who has given birth at term.
Women's milk after preterm birth has a special composition, it contains more protein, less lactose with the same total level of carbohydrates. In addition, it has a higher content of a number of protective factors, in particular lysozyme and secretory IgA. Despite the special composition, the milk of women who gave birth prematurely can satisfy the nutritional needs of only premature babies with a relatively large body weight - more than 1800-2000 g.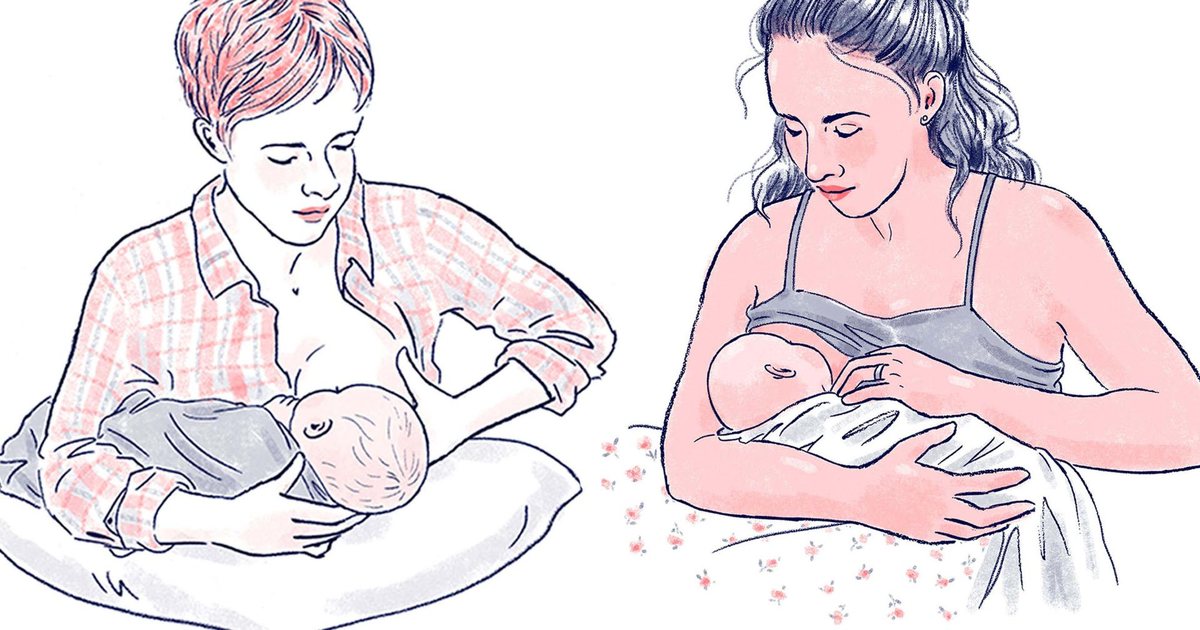 Premature babies with a lower body weight are deficient in a number of nutrients. For them, breast milk must be further enriched with protein, calcium, phosphorus, iron, and vitamins. This can be achieved by replacing part of the required amount of breast milk with a specialized formula for premature babies or by adding breast milk enhancers. When enrichers (enhancers) are used, the main advantages of breastfeeding are preserved and at the same time the high nutritional requirements of the premature baby are ensured. With artificial feeding, specialized mixtures intended for feeding premature babies should be used. Cancellation of specialized mixtures for premature babies and their transfer to standard milk formulas is carried out gradually. The duration of use depends on the gestational age of the child. Premature babies with a gestational age of more than 31-33 weeks should receive specialized formulas until they reach a body weight of 2500-3000 g, after which they are completely transferred to standard adapted milk formulas.
Premature babies with a lower body weight are deficient in a number of nutrients. For them, breast milk must be further enriched with protein, calcium, phosphorus, iron, and vitamins. This can be achieved by replacing part of the required amount of breast milk with a specialized formula for premature babies or by adding breast milk enhancers. When enrichers (enhancers) are used, the main advantages of breastfeeding are preserved and at the same time the high nutritional requirements of the premature baby are ensured. With artificial feeding, specialized mixtures intended for feeding premature babies should be used. Cancellation of specialized mixtures for premature babies and their transfer to standard milk formulas is carried out gradually. The duration of use depends on the gestational age of the child. Premature babies with a gestational age of more than 31-33 weeks should receive specialized formulas until they reach a body weight of 2500-3000 g, after which they are completely transferred to standard adapted milk formulas.