Newborn baby not bottle feeding
Baby Refusing the Bottle? Try These Tips
If you’re having trouble bottle-feeding your infant, rest assured that you are far from alone. Around 25 percent of parents report feeding-related problems with their child at some point in their development.
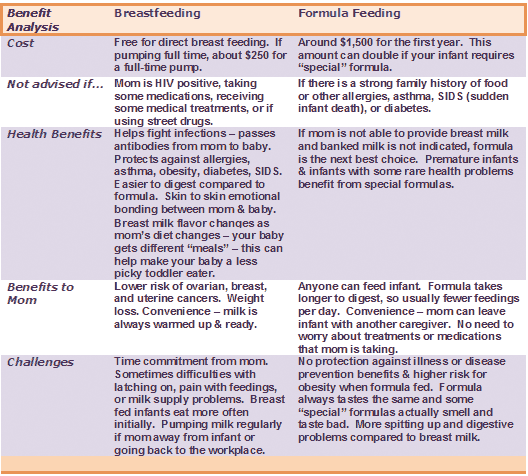
If your baby has been breastfeeding, trying to introduce a bottle can also introduce some challenges. Likewise, changes to the formula or breast milk you’re giving them or the bottle you’re using can lead to difficulties even for experienced bottle-fed babies.
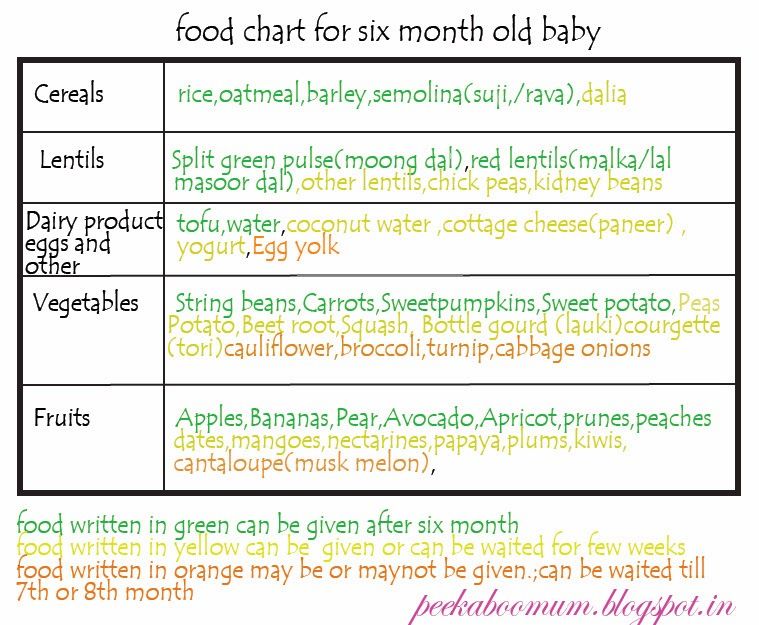
The American Academy of Pediatrics recommends delaying the introduction of foods other than breast milk until your baby is around 6 months old, suggesting exclusive breastfeeding before that time. However that’s not always realistic and you may find yourself introducing the bottle at any time during the first year.
Additionally, formula isn’t the only reason to use a bottle. Many breastfeeding parents want to incorporate bottle-feeding of breast milk for flexibility. The breastfeeding advocacy organization La Leche League suggests waiting until your breastfeeding baby is 3 to 4 weeks old before introducing a bottle.
Whenever you begin using bottles, it can be extremely frustrating trying to feed a baby who stubbornly refuses feeds. But with dedication, experimentation, patience, and love, you can eventually acclimate your baby to bottle-feeding.
Since babies can’t communicate clearly, parents and caregivers are left wondering and guessing why their baby refuses bottle-feeding. The following reasons are some of the most common things to look out for if your baby refuses the bottle:
- Your baby was recently weaned and wants to continue breastfeeding.
- Your baby isn’t hungry enough to want feeding.
- Your baby is feeling sick, colicky, or otherwise unwell enough to feed.
- Your baby is being held in an uncomfortable position.
- Your baby doesn’t like the temperature, flavor, or texture of the milk.
- Your baby doesn’t like the texture or feel of the bottle.

Depending on your previous experience with feeding you may be able to figure out the specific reasons why they’re refusing the bottle. Many times, knowing why they refuse can give you better insight into figuring out how to fix the problem.
Some of the most common and effective things you can try to help your baby accept bottle-feeding include:
- Slowly, consistently, and gradually transition from breastfeeding to bottle-feeding.
- Wait until your baby is sufficiently hungry before feeding.
- Try changing the bottle size and shape, the nipple, or other aspects of the bottle to see what your baby responds to.
- Experiment with the temperature of the milk or formula. Breast milk is lukewarm, so make sure the bottle isn’t too warm or cool.
- If your baby is teething, try changing the temperature of the milk (teething babies sometimes prefer cold milk), massaging their gums, or otherwise helping them with the pain of new teeth poking through.

- Hold your baby in a different feeding position and see what they respond to.
- Allow someone else to handle the feeding. This can be especially helpful during a transition from breastfeeding to bottle-feeding.
Before changing the formula you’re using you may want to talk to your pediatrician. There are different types of formula customized to different needs, but too many changes or certain types of formula can cause other challenges.
More tips to try
In addition to the list of possible remedies above, it is important to try to have a calm and consistent approach to bottle-feeding. Sometimes, your own frustrations with bottle-feeding can affect the infant and make it even harder for them to change.
In general, try to follow these behavioral tips for yourself when bottle-feeding a fussy baby:
- Maintain a comforting routine around mealtime.
- Avoid distractions, such as media, music, and toys when bottle-feeding.
- Feed your child at consistent time intervals of 3 to 4 hours.

- Stay calm and consistent. Don’t become angry, anxious, or overly excited with your feeding child.
- Limit mealtimes to 30 minutes.
- Try to avoid frustration during feeds. Consider having another caregiver offer the bottle if you need a break.
While it is normal for babies to sometimes refuse a bottle, there are some instances where chronic refusal to feed can be indicative of an eating disorder or an illness that requires medical attention.
About 1 to 5 percent of very young children have feeding disorder, which is characterized by an inability to consume an adequate amount of food, resulting in malnutrition.
Getting enough food is absolutely essential for a growing baby. If you think your baby is experiencing a feeding disorder making it difficult for them to gain weight, you should see a doctor immediately. Feeding disorders in early childhood are an important health issue.
In the short term, babies with feeding disorders will experience nutritional deficiency and weight loss (or inadequate weight gain), but in the long term, your baby can experience growth deficits, cognitive functioning problems, stunted neurodevelopment, and behavioral or emotional impairment.
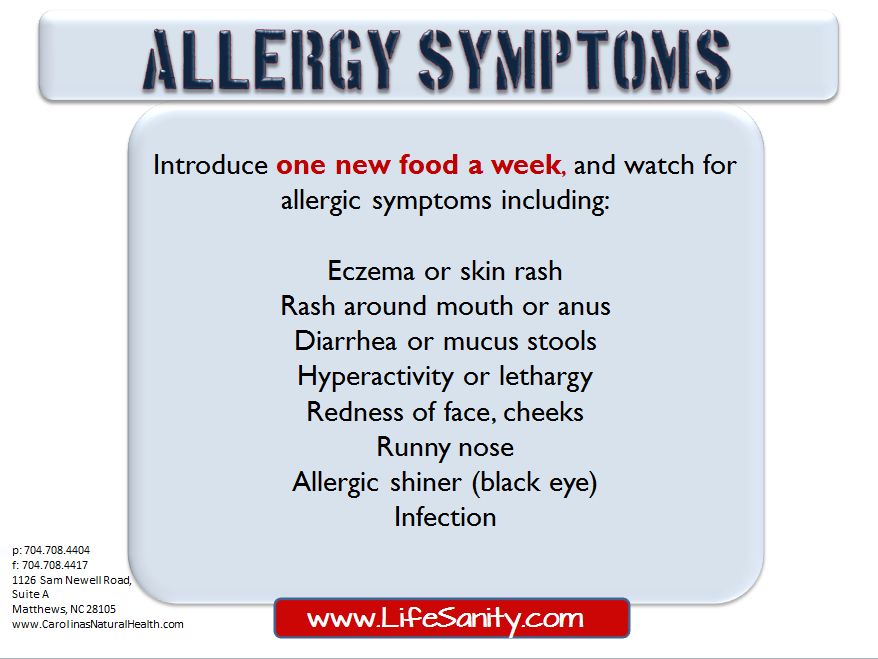
Another time to talk to your baby’s doctor is if your baby refuses to eat due to an illness or pain. Call your doctor right away if in addition to refusing the bottle your baby is showing any of the following symptoms:
- fever
- vomiting
- constant crying
- diarrhea
- difficulty breathing
Consult with a doctor to determine whether there are any illnesses or physiological issues you are unaware of that might play a part in your child’s fussy eating.
Feeding difficulties are common problems in infants and toddlers. Don’t be too worried if your baby is struggling with the transition to bottle-feeding.
There are many different approaches you can take to fixing the problem, and if you are nervous or worried about any of your child’s eating habits, contact your doctor immediately.
With consistency, determination, and lots of attention paid to your baby, you can help them overcome their obstacles and anxieties around bottle-feeding.
What to do when baby won’t take a bottle
When your breastfed baby won’t take a bottle, it can be stressful and even a little scary. Babies are not always onboard when transitioning from breast to bottle. Whether you’re going back to work or want others to help feed your baby, you might start to wonder: “What if my baby never takes a bottle?”
Don’t panic. Usually when your baby won’t take a bottle, they’re just struggling with the learning curve. They’re new to the world so they have a lot to learn. Sometimes there may be some motor skill or medical condition making it more difficult. But no matter the reason, we’re here to help.
Keep reading to learn the most common reasons why your baby may be refusing a bottle, tips for helping them get used to a bottle, and what may be going on if bottle feeding doesn’t start to improve.
Not all bottle refusal looks the same. There can be a range of signs that your child is struggling to take a bottle, including:
- Turning away from the bottle
- Gagging or fussing as the bottle’s nipple nears their mouth
- Being unable to latch/compress the bottle’s nipple and express milk
- Chewing on the bottle’s nipple
- Sputtering or coughing while feeding
- Not being able to completely swallow their sip of milk, so that some drips from their mouth
Why do many babies have problems when switching to a bottle after breastfeeding?
There’s no one-size-fits-all answer to this question. In most cases, bottle feeding problems aren’t due to abnormal oral motor function, nor are they usually due to an underlying medical issue.
In most cases, bottle feeding problems aren’t due to abnormal oral motor function, nor are they usually due to an underlying medical issue.
Actually, one of the most common reasons breastfed babies won’t take a bottle right away stems from not being introduced to one early enough in their growth. In fact, the number one mistake families make is offering a bottle too late.
Why timing is so important when introducing a bottle to a breastfed baby
Babies are born with an automatic sucking reflex. But at 2 to 3 months old that reflex becomes voluntary. In effect, that gives babies the ability to turn down a feeding if they’re not comfortable with it.
If a baby hits this stage in their growth and has only fed from their mother’s breast, they may have developed a “preference” for that method of milk delivery. Babies establish a suck-swallow-breathe pattern that works for them and lets them handle their mother’s milk flow.
When given a bottle, not only is the milk flow different, a baby has to adapt to a different nipple shape and texture. They also need to slightly adjust their posture from what they’re used to. For someone so new to the world, making these kinds of changes can be hard and overwhelming, leading to fussing, tears and why your breastfed baby won’t take a bottle.
They also need to slightly adjust their posture from what they’re used to. For someone so new to the world, making these kinds of changes can be hard and overwhelming, leading to fussing, tears and why your breastfed baby won’t take a bottle.
When to introduce a bottle to a breastfed baby
There’s an ideal window of time for introducing a bottle to a breastfed baby. You want to avoid doing it too late, but you also don’t want to do it too early. It’s important to make sure your baby gets the hang of breastfeeding and is getting enough milk before introducing a bottle.
We usually recommend waiting about 2 to 4 weeks after your baby is born before trying to bottle feed. Unless they were born early, most babies are ready by then.
How to get a breastfed baby to take a bottle: 5 helpful tips
1. Switch back and forth between breastfeeding and bottle feeding
You give your baby the best chance at developing their feeding skills if you regularly switch between bottle and breast in the midst of feedings.
2. Try giving the bottle when your baby is waking up
No matter the time of day, babies are more likely to take a bottle when they’re just waking up. The instinct to eat takes over when babies are still a little sleepy. Don’t let your baby get overly hungry before feeding. That can result in fussiness and crying (a late feeding cue), and make it harder to initiate feeding either by bottle or breast.
3. Create a relaxing environment each time you offer the bottle
Play soft, calming music – like classical or folk. Sit down someplace where you can gently rock back and forth. And swaddle your baby with their hands near their face. Having a quiet, dark room with few distractions can help, too.
Doing these things will relax your infant – in part because they will also relax you. Children sense and feed off the energy of the adults around them. And it’s no different when you and your baby are adjusting to bottle feeding. If you can be at ease with the varied routine a bottle brings, your baby will be more content, too.
4. Have a family member other than mom offer the bottle whenever possible
Each person will hold your baby a little bit differently for feedings. When your little one can get used to these differences early, it helps them learn how to adjust their posture so it’s less likely to be an issue when their sucking reflex becomes voluntary.
5. Try giving your baby a different type of bottle or nipple
Sometimes, the solution to bottle feeding problems is as simple as finding the right bottle or nipple. While there are nipple levels associated with age, every baby has their own feeding style, which may not match their age or size. There are many different nipple and bottle types out there – trying to figure out the best choice can be an overwhelming process. Finding the right fit is something that your baby’s doctor or a lactation specialist can help you with.
6. Experiment with baby’s bottle-feeding position
Your baby may also prefer to eat while in a certain position, which typically differs from breastfeeding positions.![]() Try different angles and placements to see if there is one they favor. For example:
Try different angles and placements to see if there is one they favor. For example:
- Cradling them in your arm at a 45-degree angle while keeping their head and neck aligned.
- Sitting upright so that their back is against your stomach.
- While sitting or lying down, bend your legs and position your baby so they face you with their head resting against your knees, their back against your thighs and their feet on your stomach.
No matter what position you use, remember to angle the bottle so that milk only comes out when your baby sucks, and never prop the bottle in their mouth. Also remember to never lay your baby completely flat while feeding.
What to do when an older baby is refusing to take a bottle
The breast to bottle transition is certainly easier if you introduce a bottle at the right age. But even if your baby is already 2 to 3 months old, it’s still possible. In addition to the tips above, you can help your baby practice with a pacifier.
A pacifier can help babies form and strengthen their sucking ability. Consistently offer a pacifier to help soothe your baby when they’re fussy, if you’re not already. This helps your baby learn to organize their mouth movement, which will calm them. Once that becomes routine, begin offering your baby a pacifier for 20 to 30 seconds when you go to make a bottle. Doing so will help them more calmly prepare for bottle feeding.
Gently pull on the pacifier as your baby sucks it. Make sure to do this at least 3 to 5 times a day, including when your baby is using the pacifier to prep for a bottle feeding. These slight tugs will help your baby learn how to resist releasing the seal they’ve formed on the pacifier’s nipple. And that can strengthen their latch on a bottle’s nipple, too.
When the above tips don’t work, there may be another reason your baby is refusing a bottle
If you’ve been trying at-home strategies for a few days and your baby doesn’t seem to be getting more comfortable taking a bottle, call your baby’s doctor. They can help determine whether a medical issue may be present or connect you with a specialist if needed. Other reasons why your baby is refusing a bottle can include:
They can help determine whether a medical issue may be present or connect you with a specialist if needed. Other reasons why your baby is refusing a bottle can include:
Reflux issues can cause pain with eating
Babies can get heartburn, too! When a baby has reflux, food and stomach acid flow from the tummy back into the esophagus (the tube the carries food from the mouth into the stomach).
Reflux causes babies to feel discomfort or pain when eating, which understandably affects feeding. Symptoms that may point to reflux issues include:
- Arching or stiffening their back when feeding
- Crying, fussing and getting red or watery eyes while feeding
- Coughing regularly during feedings or right after them
- Refusing to drink or accepting only 1 ounce of milk or less
- Falling asleep while feeding
- Having poor sucking and breathing coordination
- Taking a long time to eat or drink
It’s important to know these actions can occur and not be related to reflux. It’s common for babies to have a fussy time of day or be more tired some days than others. If symptoms are ongoing, a baby can be evaluated and treated for reflux.
It’s common for babies to have a fussy time of day or be more tired some days than others. If symptoms are ongoing, a baby can be evaluated and treated for reflux.
Facial or oral structural differences can make latching difficult
If reflux doesn’t appear to be the problem, your baby’s doctor may refer you to a rehab specialist like me.
I’ve been helping moms and families who struggle with the transition to bottles for almost a decade. It’s part of my work as a speech therapist at Park Nicollet. You might think, “My baby’s problem is with eating – not talking. What does speech therapy have to do with that?” The answer could be, a lot!
The shape or structure of a baby’s cheeks, mouth, tongue or jaw can impact their feedings. That’s because these body parts affect how they’re able to latch both to the bottle, as well as to the breast. For example:
- Thin cheeks with little to no fat pads make it hard for a baby to hold their tongue in place to feed
- A tongue-tie(where the tissue that attaches the tongue to the bottom of the mouth is too short) can limit a baby’s ability to move their tongue from side to side in their mouth or past their lower lip to feed
- A tongue-tie that’s been clipped requires a baby to relearn how and where to move their tongue to feed, and create new muscle memory
- A “vaulted” palate (where the roof of the mouth is higher and narrower than the typical flat U-shape) causes additional space in a baby’s mouth that can make it harder for their lips to form a tight seal
Weak oral muscle tone or lack of oral stimulation can make it hard to get enough milk during feeding
It’s possible that a baby just doesn’t have the strength to get what they need during a feeding. This could be the case even if they have very normal oral motor actions.
This could be the case even if they have very normal oral motor actions.
If your baby is refusing to take a bottle, we’re just a phone call away
Always feel empowered to call your baby’s doctor or make an appointment with them. They can connect you with different types of breastfeeding support, including drop-in breastfeeding support groups and lactation consultants who help with both bottle and breastfeeding issues. They can also refer you to a pediatric rehabilitation specialist.
Our incredible nursing staff is also here for you. HealthPartners patients can call 800-551-0859. Park Nicollet patients can call their clinic directly during regular business hours, or 952-993-4665 if it’s after hours. For questions and advice on new baby care, you can also call our 24/7 BabyLine at 612-333-2229.
Find a doctor who can help
Are you still looking for the right doctor for your new baby? We have hundreds of doctors and clinicians across the Twin Cities, central Minnesota and western Wisconsin, that can help you with all your questions.
While you may be wondering how to get them to take a bottle today, you’ll get it figured out. Then the question will be: How can I get my child to eat their vegetables?
Baby won't take the bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.

- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
This will make it easier to feed the baby when the mother is not around.
2. Try to maintain body contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back. *
*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed.![]() Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.![]()
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
You are about to visit the Philips USA website.
Bottle feeding
When breastfeeding is not possible, or there is not enough breast milk and supplementary feeding is required, the use of infant milk formulas allows you to establish good nutrition for the baby.
The mixtures contain all the necessary nutrients, vitamins and trace elements. As a rule, they are well tolerated and digested, especially if the feeding process is properly established.
If you plan to bottle feed or supplement your baby with formula, our article will help you navigate the basic rules and intricacies of artificial feeding.
How to choose a teat (nozzle) for a bottle
Teats differ in composition (silicone, latex), shape and flow rate. While the shape of the nipple and the material are often chosen according to the preferences and needs of a particular baby, the flow rate is strictly determined by the age category.
Babies are fed from birth using the slowest flow nipple (these are usually labeled from 0 and one drop). Next, the teat flow rate in most bottle manufacturers increases at 3 months, 6 months, 12 months.
In order not to be mistaken, pay attention to the labeling and the age group for which the nipple to the bottle of the selected manufacturer is intended.
Whether such a nipple is right for you, you will also probably be able to understand during feeding.
- The baby should be able to comfortably grasp the nipple and drink formula confidently (without too much effort).
- He should not choke/choke frequently.
- The mixture should flow well. If the mixture does not flow until you shake the bottle, the hole may be clogged with powder.
- If the mixture flows too much, check if the nipple is not torn.
How to treat the bottle
For newborn babies in the first months of life, it is recommended to sterilize the bottles before each feeding. Sterilization is the immersion of all feeding accessories (bottles, nipples, other parts) in boiling water for about 5 minutes to destroy pathogenic microflora.
Sterilization is the immersion of all feeding accessories (bottles, nipples, other parts) in boiling water for about 5 minutes to destroy pathogenic microflora.
You can choose any convenient method of sterilization: using a special device (sterilizer), in a microwave oven, dishwasher, ordinary boiling. Read more about how to properly sterilize bottles in our other article.
It is important to ensure that the baby bottle you use is made of safe plastic that can be heated. Some types of plastic release harmful chemicals when heated. As a rule, information about the possibility of sterilization and heating is indicated on the packaging. If there is no such information, it is not worth the risk. Use special baby bottles from well-known manufacturers. For example, a Dino Reno feeding bottle with nipple can be sterilized completely by any of the listed methods.
How to prepare formula and feed your baby
- Wash your hands with soap and water and dry with a dry towel.

- Remove the bottle and nipple from the sterilizer using the special holder (tweezers), assemble the bottle with the nipple, being careful not to touch the part that will go into the baby's mouth with your hands.
- Take boiled or special baby water heated to body temperature, dilute the mixture in the proportion indicated on the package.
- Use the special measuring spoon for preparation (it is included in each box with the mixture).
- Dilute the mixture strictly in the proportion indicated by the manufacturer. A thicker or thinner formula can harm your baby and cause stomach problems.
- Shake the bottle thoroughly to mix the contents evenly. Make sure that there are no lumps and clots left in the liquid and on the walls of the bottle.
- Check the temperature of the prepared mixture by dropping a little liquid on your wrist, it should not burn.
- Hold the bottle at the right angle. So that the tip of the nipple is always filled with milk and not with air.

- After feeding, hold the baby upright, let him burp the excess air.
- Feed your baby only fresh formula. According to the recommendations of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) of 2004, the reconstituted dry formula can be stored in a sealed bottle at a cool temperature for no more than 4 hours.
- If the mixture has cooled down, it can be warmed up with a special heater or in a water bath.
- If you are going on a long trip or outing, do not prepare the formula ahead of time. Better just pour the required amount of water into the bottle, and pour the right amount of the mixture into a separate container. Mix before feeding.
You will also find recommendations on the amount of formula to eat at a time, taking into account the age of the child, on the package. But some features of the baby's behavior can tell you whether he is full or not.
- If the baby is pushing the nipple out of the bottle with his tongue and spitting out the formula, he is probably already fed and the feeding should be stopped.