Newborn baby sick after every feed
Reflux in babies - NHS
Reflux is when a baby brings up milk, or is sick, during or shortly after feeding. It's very common and usually gets better on its own.
Check if your baby has reflux
Reflux usually starts before a baby is 8 weeks old and gets better by the time they're 1.
Symptoms of reflux in babies include:
- bringing up milk or being sick during or shortly after feeding
- coughing or hiccupping when feeding
- being unsettled during feeding
- swallowing or gulping after burping or feeding
- crying and not settling
- not gaining weight as they're not keeping enough food down
Sometimes babies may have signs of reflux but will not bring up milk or be sick. This is known as silent reflux.
Things you can try to ease reflux in babies
Your baby does not usually need to see a doctor if they have reflux, as long as they're happy, healthy and gaining weight.
Do
-
ask a health visitor for advice and support
-
get advice about your baby's breastfeeding position or how to bottle feed your baby
-
hold your baby upright during feeding and for as long as possible after feeding
-
burp your baby regularly during feeds
-
give formula-fed babies smaller feeds more often
-
make sure your baby sleeps flat on their back (they should not sleep on their side or front)
Non-urgent advice: See a GP if your baby:
- is not improving after trying things to ease reflux
- gets reflux for the first time after they're 6 months old
- is older than 1 and still has reflux
- is not gaining weight or is losing weight
Urgent advice: Ask for an urgent GP appointment or call 111 if your baby:
- has vomit that's green or yellow, or has blood in it
- is projectile vomiting (being sick with more force than usual)
- has blood in their poo
- has a swollen or tender tummy
- has a very high temperature or they feel hot or shivery
- keeps being sick and cannot keep fluid down
- has diarrhoea that lasts for over a week or has signs of dehydration
- will not stop crying and is very distressed
- is refusing to feed
Also call your GP or 111 if you have any other concerns about your baby.
Treatment for reflux in babies
A GP or specialist may sometimes recommend treatments for reflux.
If your baby is formula-fed, you may be given:
- a powder that's mixed with formula to thicken it
- a pre-thickened formula milk
If the thickening powder does not help or your baby is breastfed, a GP or specialist might recommend medicines that stop your baby's stomach producing as much acid.
Very rarely, surgery might be needed to strengthen the muscles to stop food or milk travelling back up. This is usually only after trying other things or if their reflux is severe.
Causes of reflux
Reflux usually happens because your baby's food pipe (oesophagus) has not fully developed, so milk can come back up easily.
Your baby's oesophagus will develop as they get older and the reflux should stop.
Page last reviewed: 13 December 2021
Next review due: 13 December 2024
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.

- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for.
 At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again.
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 11/04/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i. e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
A newborn vomited up - what to do, causes and how to help
The urge to vomit in a newborn is an alarming symptom that should not be ignored. They may be the result of accidental ingestion of a small object by a baby, intoxication, acute appendicitis, intestinal obstruction, or other diseases. The most harmless reason that a child vomited is overeating.
Physiological causes of vomiting
Sometimes vomiting is a short-term phenomenon that is not associated with pathology or disease. What could be the reasons that a healthy newborn vomited:
What could be the reasons that a healthy newborn vomited:
- overeating - the baby ate too much breast milk or formula;
- the baby is teething, and vomiting is a sign of temporary malaise;
- child swallows air while feeding;
- wrong daily routine, severe fatigue;
- active play and activity immediately after eating.
If the baby feels well, you need to help him calm down and give him a drink of warm boiled water. Put the baby to sleep on the side. The baby will relax, the contents of the stomach will move into the intestines, and vomiting attacks will not recur. Try not to bathe the baby, do not shake immediately after eating. Keep track of the amount of food he gets to avoid overeating.
The introduction of a new mixture can also cause vomiting. Check with your pediatrician to make sure there are no other causes. Your doctor can help you find other foods that are right for your child.
Sometimes babies feel sick after crying for a long time, for example, the mother left, and the baby is very bored or hungry.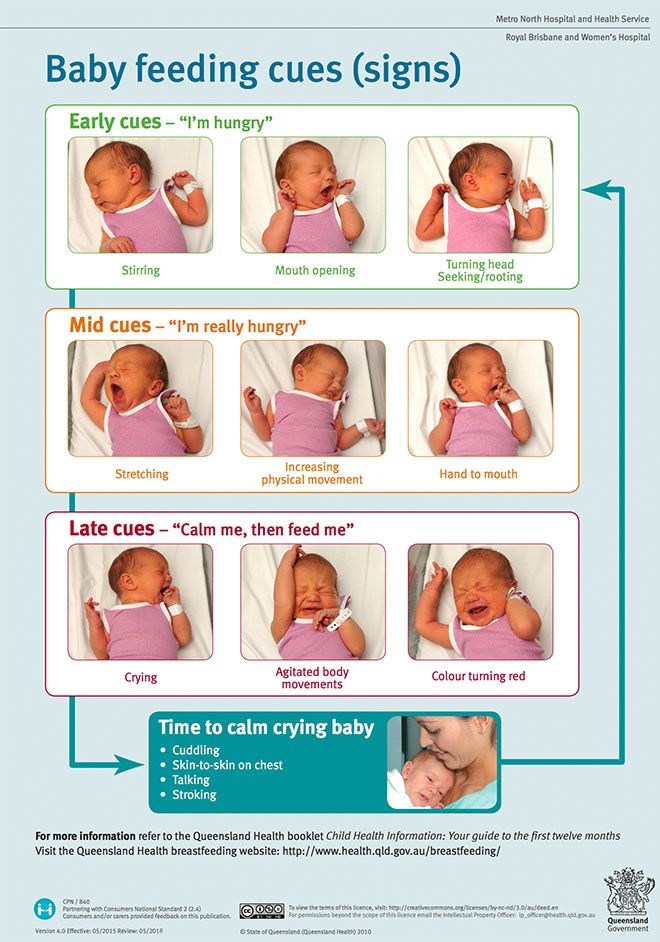 If there are no other alarming symptoms, calm the baby as soon as possible, shake, feed, sing a gentle song. If vomiting recurs later, you need to call the pediatrician.
If there are no other alarming symptoms, calm the baby as soon as possible, shake, feed, sing a gentle song. If vomiting recurs later, you need to call the pediatrician.
Symptoms and possible causes of vomiting
Most often, vomiting is a signal of diseases that can be identified by additional symptoms.
Poisoning or intestinal infections
The symptoms of poisoning and intestinal infection are very similar: the newborn is sick, his stool changes, his tummy hurts and his temperature rises. The child should be given constant water to drink so that dehydration does not occur. In any of these conditions, you need to urgently call a doctor.
Concussion
Babies are very mobile, if a child hits his head or falls, you need to urgently call an ambulance. A concussion is accompanied by vomiting, crying, temporary loss of consciousness, pallor, drowsiness, and impaired coordination of movements.
Foreign body
Swallowing a small object can also cause vomiting without vomiting in neonates. The baby may begin to salivate profusely, have breathing problems, he may vomit with mucus and blood in the vomit. If you suspect that the baby has swallowed any object, call an ambulance.
The baby may begin to salivate profusely, have breathing problems, he may vomit with mucus and blood in the vomit. If you suspect that the baby has swallowed any object, call an ambulance.
Appendicitis
This phenomenon is rare in newborns. If appendicitis is inflamed, the baby has a very sore tummy, when stroking or probing, the pain and crying intensify. There is nausea, weakness, restless behavior. Inflammation of appendicitis in infants is life-threatening, you need to urgently call an ambulance.
Allergic reaction, food intolerance
If a child has an intolerance to certain foods or an allergy to them, vomiting is accompanied by diarrhea, skin rashes, the baby is capricious, restless. With such symptoms, you need to contact a pediatrician and an allergist.
Acute infections
SARS, pyelonephritis, pneumonia can provoke a gag reflex without vomiting in a newborn from severe coughing spells and general weakness. With a high temperature, sore throat, cough, you need to call a pediatrician at home to examine the child and prescribe appropriate treatment.
With a high temperature, sore throat, cough, you need to call a pediatrician at home to examine the child and prescribe appropriate treatment.
Intestinal obstruction
This is a dangerous disease. It can be congenital or acquired. Accompanied by severe bloating, bile impurities are observed in vomiting. The baby cries a lot, the stool changes to a state of red jelly. Feeding is stopped and urgently seek medical help - the disease is life-threatening.
Congenital pathologies of the digestive system
Congenital pathologies lead to serious problems with digestion. If you notice that the child is restless during feeding, his stool is broken, his tummy is swollen, he is gaining weight poorly or losing it, consult a doctor. It is necessary to undergo an examination of the gastrointestinal tract and pass additional tests.
Neurological disorders
The main causes of gag reflex without vomiting in the newborn are neurological disorders. They occur most often in premature babies, in children with underweight. The cause of such disorders may be birth trauma, asphyxia or fetal hypoxia. With such pathologies, gag reflexes are accompanied by hyperactivity, chin tremor, strabismus, convulsions. You need to contact a neurologist and undergo inpatient treatment.
They occur most often in premature babies, in children with underweight. The cause of such disorders may be birth trauma, asphyxia or fetal hypoxia. With such pathologies, gag reflexes are accompanied by hyperactivity, chin tremor, strabismus, convulsions. You need to contact a neurologist and undergo inpatient treatment.
Heat stroke
Heat stroke is accompanied by nausea, skin redness, dizziness, rapid breathing. Also, the child develops lethargy, dry skin. Call the doctors, before they arrive, put the child in a cool place on the barrel.
How to distinguish vomiting from regurgitation
Spitting up is a natural process. The baby spits up a few minutes after feeding. It is not dangerous, it is a normal physiological process. If the baby gets a large amount of air into the tummy (swallowed while eating), then after regurgitation the discomfort disappears, he immediately feels better.
Vomiting is the result of reflex contraction of the muscles of the abdominal cavity and diaphragm, it is accompanied by rapid breathing, profuse salivation.
The main differences between vomiting and regurgitation:
Why vomiting is dangerous
Vomiting is a protective reflex of the body. So he gets rid of foreign bodies, removes toxins, microorganisms, excess food. Most often, vomiting is a symptom of diseases that are dangerous for the baby:
- Vomiting itself is dangerous due to possible dehydration of the body. The baby loses not only the liquid, but also the mineral salts dissolved in it. The water-salt balance is disturbed, this affects the general condition of the crumbs. For newborns, this is especially dangerous, because dehydration occurs rapidly, and replenishing a full supply of fluid is not so easy.
- The second danger of vomiting is the inhalation of vomit. During an attack, the baby should be held upright, for safety reasons, you need to ensure that the baby's head lies on its side in a dream.
- Weight loss due to food rejection is also dangerous.
 This is especially important for premature babies or babies with a small body weight.
This is especially important for premature babies or babies with a small body weight.
If the baby has vomited, carefully monitor his condition and well-being. Make sure it's not spitting up. If in doubt, it is better to call a doctor anyway, rather than wait for more serious symptoms.
When to call a doctor
It is always better to play it safe and call a doctor if you are not sure about your baby's health. In which cases it is necessary to seek medical help:
- the baby is vomiting, but he did not poop;
- the child is crying, restless, his stomach hurts;
- repeated vomiting;
- symptoms of dehydration appear;
- vomiting accompanied by diarrhoea;
- vomiting is a fountain;
- before vomiting the baby fell or hit his head hard;
- in the vomit there is blood, brown or black blotches;
- the child does not eat or drink;
- with vomiting comes out completely everything that the child ate and drank;
- he has a high temperature;
- the baby is lethargic, sleepy.

Treatment
Vomiting in children may require enterosorbent. It is believed that this tool binds and removes from the body toxic metabolites, allergens, bacteria, viruses and other harmful compounds that can provoke vomiting.
For the smallest, that is, children under two years old, when choosing an enterosorbent to alleviate the conditions that caused vomiting, you can be guided by the statement of ANSM (France). So, in March 2019, this French regulator published information that raw materials for the production of clay-based powder enterosorbents may contain lead. This harmful substance can penetrate into the bloodstream and in certain concentrations have a depressing effect on the development of the baby.
The Russian Society of Obstetricians and Gynecologists (ROAG) designated the Russian "Enterosgel" as the first choice for the treatment of conditions requiring the use of an enterosorbent in young children, pregnant and lactating women. "Enterosgel" is a molecular sponge that is not absorbed into the blood and works only in the lumen of the gastrointestinal tract. A homogeneous gel-like form with a neutral smell and taste simplifies the use of "Enterosgel" even for the smallest. It is important that "Enterosgel" promotes the healing of microtraumas on the mucous membranes of the gastrointestinal tract and minimizes the risk of constipation during use due to the formula saturated with water.
"Enterosgel" is a molecular sponge that is not absorbed into the blood and works only in the lumen of the gastrointestinal tract. A homogeneous gel-like form with a neutral smell and taste simplifies the use of "Enterosgel" even for the smallest. It is important that "Enterosgel" promotes the healing of microtraumas on the mucous membranes of the gastrointestinal tract and minimizes the risk of constipation during use due to the formula saturated with water.
The main danger of vomiting is dehydration. It is urgent to call a doctor so that he establishes the cause of vomiting and prescribes the appropriate treatment. Also, the doctor prescribes electrolyte solutions, which need to replenish the fluid lost by the body.
What to do while waiting for the doctor
- keep the child upright;
- after each bout of vomiting, wash the child, clean his mouth and nose;
- try not to disturb the child unnecessarily, do not carry him from place to place;
- it is possible to feed milk or a mixture familiar to the baby if there are no other dangerous symptoms;
- try to give the baby some water to drink;
- do not give any medication until the doctor arrives;
- do not give the newborn prebiotics, probiotics, zinc, enterosorbents, antidiarrheal drugs (if diarrhea has joined) - the doctor should prescribe treatment, it is dangerous to experiment in the treatment of such a small child.

What to give your baby to drink
Give your baby plenty of fluids to prevent dehydration. It is best to put the baby to the breast more often. If the doctor has already suggested which pharmacy solutions of electrolytes can be used, use them. If there are no such appointments, you can make the solution yourself. How to cook:
- take 1 liter of boiled water;
- add 1 level teaspoon of salt;
- 4-5 level teaspoons of sugar.
Mix everything thoroughly, store in the refrigerator for no more than a day. Give your child a few milliliters every five to ten minutes. To do this, take a syringe, remove it from it and put the tip with a needle away and gently squeeze the liquid into the baby's mouth with such a harmless piston.
Signs that treatment is not working
Sometimes the situation does not improve or even worsens after a doctor has prescribed treatment. Carefully monitor the well-being of the child.