Nicu babies feeding
Feeding your baby in the NICU
Breast milk is the best food for your baby. Breast milk has antibodies that help keep your baby from getting sick and nutrients that help her grow.
If you’re not breastfeeding, you can feed your baby formula or breast milk from a breast milk donor.
If your baby’s not ready to breastfeed, you can pump your breast milk.
If you have multiples, your babies may want to feed differently. Take time to find out what’s best for each baby.
Key If you need help with breastfeeding, talk to your nurse or lactation consultant.
What does your baby eat in the NICU?
Breast milk is the best food for your baby, even if she’s in the newborn intensive care unit (also called NICU). Breast milk has antibodies that help keep your baby from getting sick. It also contains nutrients that help your baby grow and develop. And breast milk changes as your baby grows so she gets exactly what she needs at the right time. This is true even if your baby was born prematurely. Premature birth is birth that happens before 37 weeks of pregnancy.
For the first few days after giving birth, your breasts make a thick, yellowish breast milk called colostrum. It has nutrients and antibodies that your baby needs. Even if you make only a few drops of colostrum, you can feed it to your baby. Your body starts to make breast milk about 3 to 4 days after giving birth.
If you’re not breastfeeding, your baby may get formula or breast milk from a donor (also called donor breast milk). Formula is a milk product you can feed your baby instead of breast milk. Donor breast milk is breast milk that’s been donated to a milk bank. A milk bank receives and stores donated breast milk, tests it to make sure it’s safe and sends it to families of babies who need it. Donor breast milk is prescribed by your baby’s provider. It has all the benefits of your own breast milk.
Sometimes babies get both breast milk and formula. Talk to your baby’s provider about the best food for your baby while he’s in the NICU.
Talk to your baby’s provider about the best food for your baby while he’s in the NICU.
How do you feed your baby in the NICU?
The way you feed your baby depends on her medical condition and how well she can suck and swallow. You can feed her:
- By breastfeeding. If your baby can’t breastfeed, you can feed her breast milk that you pump from your breasts.
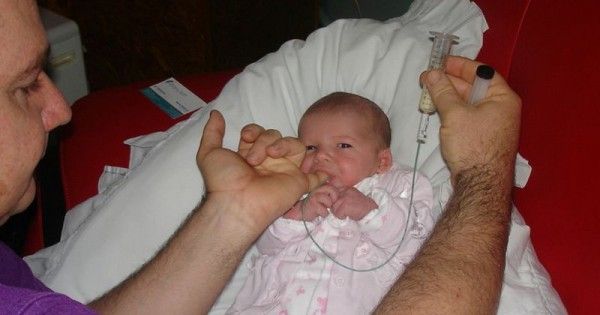
- Breast milk or formula through a bottle
- Breast milk or formula through a feeding tube. A feeding tube is a tube that goes into your baby’s stomach to give her food when she can’t get it from regular feeding. Depending on your baby’s condition, she may need a gastronomy tube (also called a g-tube), a nasogastric tube (also called an NG tube) or an orogastric tube (also called an OG tube). A g-tube goes directly into your baby’s stomach. An NG tube goes through your baby’s nose, down the esophagus and into your baby’s stomach. An OG tube goes into your baby’s mouth, down the esophagus and into your baby’s stomach.

- Through an intravenous line (also called an IV). This is for babies who are very small or sick. Your baby’s health care provider places a small tube in a vein in your baby’s hand, foot, scalp or belly button. Your baby get fluids and important nutrients through the IV to help her grow.
Depending on your baby’s condition, you may use a few of these methods together to feed your baby. For example, your baby may get food from a feeding tube and an IV.
How can you give your baby breast milk if your baby can’t breastfeed yet?
If your baby isn’t ready to breastfeed, you can pump your breast milk. A breast pump helps remove milk from your breasts. Using a breast pump may feel awkward at first. But with practice, pumping gets easier and more comfortable. A nurse or lactation consultant in the NICU can show you how to use the pump. A lactation consultant is someone with special training to help all women breastfeed, even women who have special breastfeeding problems.
As soon as your baby can, let her practice sucking at your breast to get ready for breastfeeding. This is called non-nutritive sucking. Here’s how to do it: Pump your breasts until they’re empty. Then let your baby touch and taste your breast to help her get used to what breastfeeding is like.
What can you do if you’re not making enough breast milk?
Some moms may have trouble making breast milk. It can be hard for moms with health conditions before or during pregnancy or after their baby was born. If you’re worried that you’re not making enough breast milk, talk with a nurse or lactation consultant in the NICU. You also can get help from a breastfeeding support group. A support group is a group of people who have the same kind of concerns. They meet together to try to help each other. You can find a breastfeeding support group that meets together in person or online.
You may be able to build up your milk supply (the amount of milk you make when breastfeeding) by:
- Getting rest.
 Your body produces more milk when it’s rested.
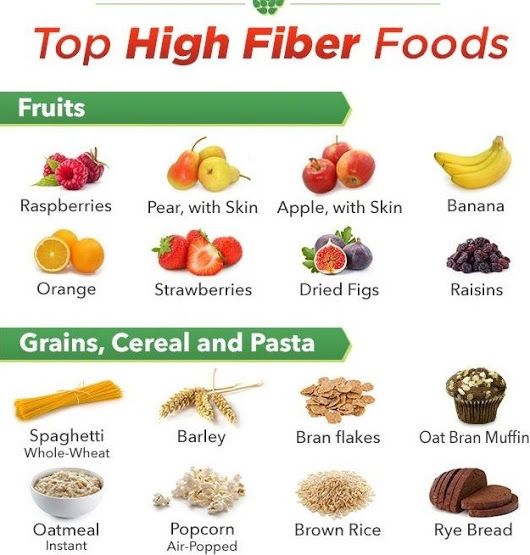
Your body produces more milk when it’s rested. - Eating healthy foods and drinking a lot of fluid, like water, juice or milk. When you breastfeed, your body loses fluid. It’s important that you get that fluid back through what you drink.
- Using a breast pump after or between feedings. When you pump your breasts often, they make more breast milk.
- Pumping your breasts until they’re empty each time you pump
- Doing kangaroo care (also called skin-to-skin care). This is when you put your baby, dressed only in a diaper, on your bare chest.
How can you feed more than one baby?
If you have multiples (twins, triplets or more) in the NICU, learn how each baby feeds best. For example, you may find that one baby feeds better from the breast and one feeds better from the bottle. Or one baby may do better on breast milk and one does better on formula. Or you may decide to pump breast milk for all your babies and only use formula when needed.
Take your time to figure out what works best for you and your babies. And expect to adjust your plans as your babies grow. Once they’re healthy, you can breastfeed two babies at once. Ask for help holding one baby while you get settled with the other. With practice, you can manage both by yourself.
More information
- American Academy of Pediatrics
- La Leche League International
- International Lactation Consultant Association
- womenshealth.gov/breastfeeding
Last reviewed: April, 2019
See also: Breastfeeding is best, Feeding your baby formula, Keeping breast milk safe and healthy, Share your story, Using a breast pump
Feeding your baby after the NICU
After your baby leaves the NICU, you can feed her breast milk, formula or both.
Your baby gives you cues for when she’s feeling hungry and when she’s had enough to eat.
Your baby most likely is eating enough if she’s gaining weight and makes six to eight wet diapers 4 to 5 days after birth.

If you have trouble feeding your baby, ask for help from your baby’s health care provider or your lactation consultant.
If you’re feeding your baby from a bottle, use a cup of warm water to warm breast milk or formula. Never microwave your baby’s bottle.
What does your baby eat after the NICU?
Breast milk (milk from your breast) is the best food for babies in the first year of life. Breast milk has antibodies that help keep your baby from getting sick. It contains nutrients that help your baby grow and develop. And it changes as your baby grows so he gets exactly what he needs at the right time. This is true even if your baby was born prematurely. Premature birth is birth that happens before 37 weeks of pregnancy.
In the NICU, you may not have been able to feed your baby the way you wanted to. For example, some babies in the NICU can’t breastfeed directly (feed from the breast). They may not have a good suck, swallow breathe pattern to be able to breastfeed well, or breastfeeding may be too tiring. Now that you’re home, you and your baby can get used to breastfeeding together.
Now that you’re home, you and your baby can get used to breastfeeding together.
You can feed your baby your own breast milk or donor breast milk. Donor breast milk is breast milk that a woman donates to a milk bank. A milk bank receives and stores donated breast milk, tests it to make sure it’s safe and sends it to families of babies who need it. Donor breast milk is prescribed by your baby’s health care provider. It has all the benefits of your own breast milk.
Formula is a milk product you can feed your baby instead of breast milk. If you’re not breastfeeding or if your baby needs extra nutrients, he may need to have formula. Your baby’s provider can recommend one that helps your baby get all the nutrients she needs. Sometimes babies get both breast milk and formula.
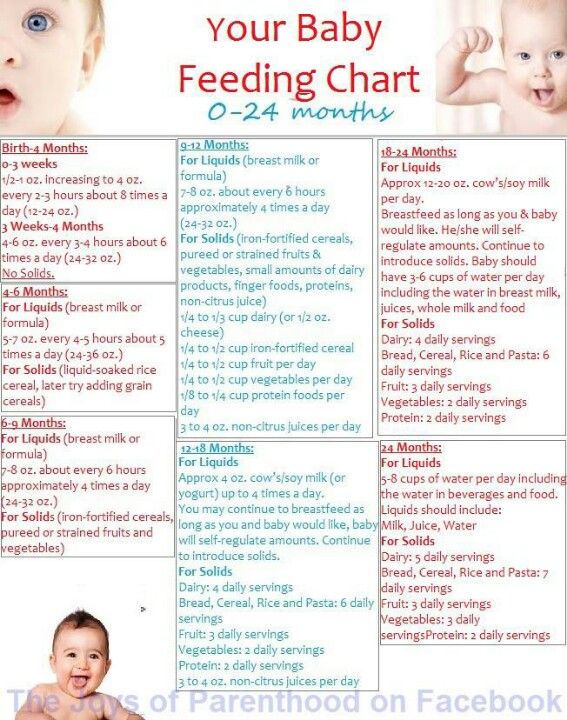
How do you know when your baby is ready to eat?
Babies eat a lot, and each baby is different. Some babies are hungrier in the morning, and other babies are hungrier at night.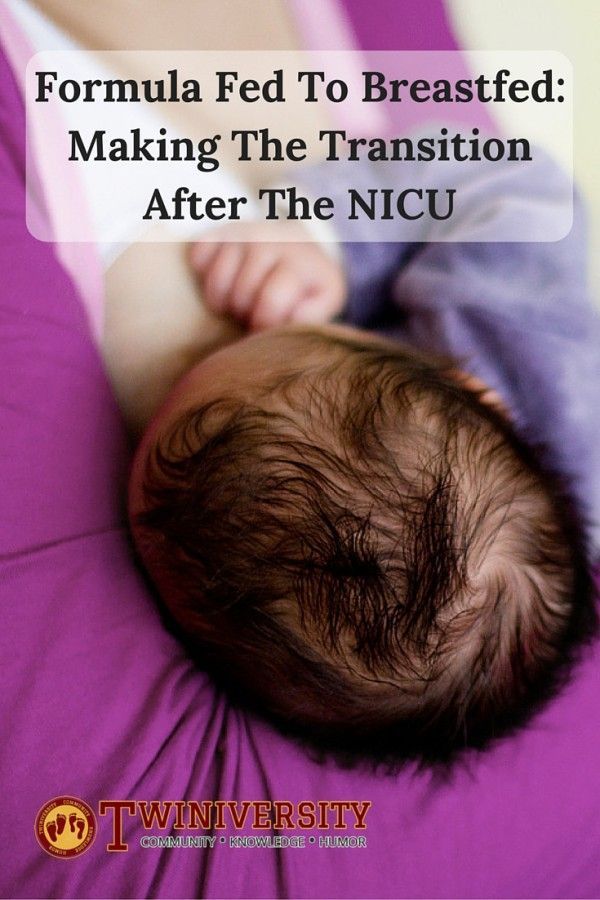 Most babies eat every 2 to3 hours, or eight to 12 times a day. Over time, you get to know your baby’s eating habits.
Most babies eat every 2 to3 hours, or eight to 12 times a day. Over time, you get to know your baby’s eating habits.
Ask your baby’s provider about how often to feed your baby to make sure she’s gaining enough weight. If your baby sleeps for long periods of time, you may need to wake her up every few hours to eat.
Look for and learn your baby’s feeding cues. Feeding cues are signs that your baby is hungry. Feeding cues include:
- Rooting. This is turning her head toward anything that touches her cheek or mouth.
- Sucking movements or sounds
- Putting her hand to her mouth
- Crying. This is a late feeding cue. Try to feed your baby before she starts to cry.
To make nighttime feedings easier, you may want to put the baby’s crib in your room so she’s nearby during the night. The American Academy of Pediatrics (also called AAP) recommends that you and your baby sleep in the same room, but not in the same bed, for the first year of your baby’s life but at least for the first 6 months.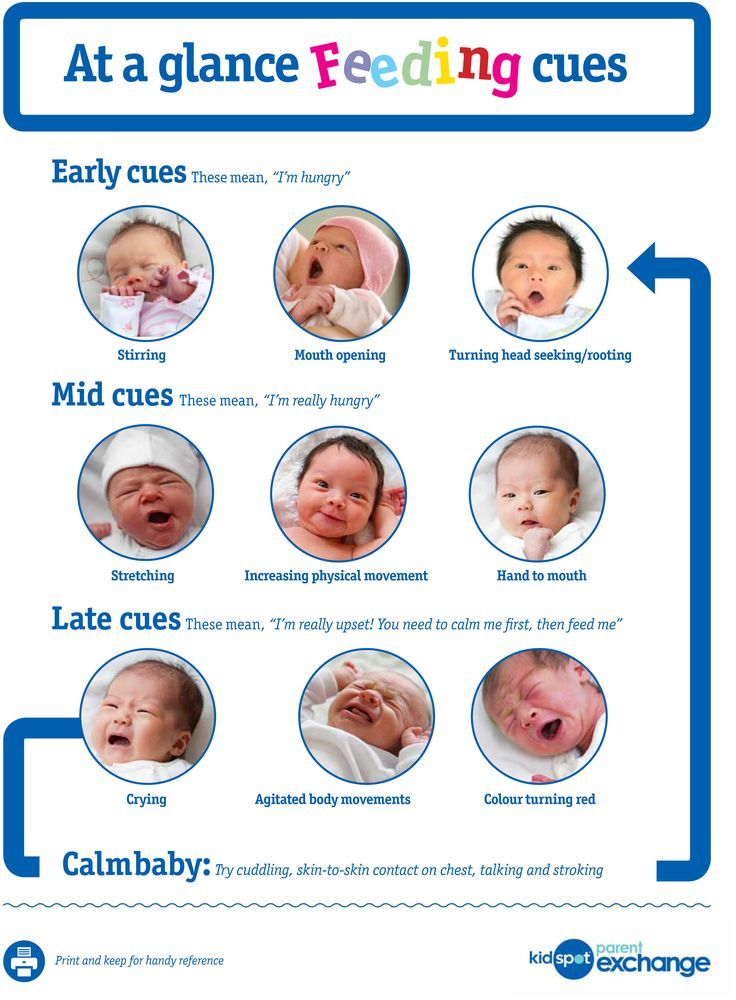
How do you know when your baby has had enough to eat?
Look for your baby’s cues. These are some ways your baby is telling you he’s full:
- He starts and stops feeding.
- He unlatches often or spits out bottle.
- He slows down or falls asleep.
- He gets distracted easily.
- He closes his mouth or turns his head away.
Your baby most likely is eating enough if he’s gaining weight and makes six to eight wet diapers 4 to 5 days after birth. If you’re worried that he’s not getting enough to eat, tell your baby’s provider.
Who can help you with breastfeeding after your baby leaves the NICU?
Most NICU babies can learn to breastfeed. It may take time and practice for you and your baby to get comfortable with it. Be patient and ask for help if you need it. You can get breastfeeding help from a lot of different people:
- Your health care provider and your baby’s provider
- A lactation consultant.
 You can find a lactation consultant through your health care provider or your hospital. Or go to the International Lactation Consultants Association.
You can find a lactation consultant through your health care provider or your hospital. Or go to the International Lactation Consultants Association. - A breastfeeding peer counselor. This is a woman who breastfed her own children and wants to help and support mothers who breastfeed. She has training to help women breastfeed, but not as much as a lactation consultant. You can find a peer counselor through your local WIC nutrition program. Or visit womenshealth.gov/breastfeeding or call the National Breastfeeding Helpline at (800) 994-9662.
- A breastfeeding support group. This is a group of women who help and support each other with breastfeeding. Ask your provider to help find a group near you. Or go to La Leche League.
Can you pump and store breast milk?
Yes. If you’re breastfeeding, a breast pump helps you remove milk from your breasts. You may have used a breast pump in the NICU. Or you may want to use a one now that your baby is home because you’re going back to work or school. Some moms use a breast pump because they want a break between feedings or so their partner can feed the baby.
Some moms use a breast pump because they want a break between feedings or so their partner can feed the baby.
After you pump, put your breast milk in containers (bottles or bags) and store them in the refrigerator or freezer. Put just the amount of milk your baby needs for each feeding in the container. Breast milk doesn’t last forever, so write the date on the container before you store it. Fresh breast milk is safe at room temperature for 4 hours.
If you’re using formula, how do you know what kind to get?
If you’re feeding your baby formula, your baby’s provider can tell you what kind to get and how much to feed your baby. Some babies leave the hospital on regular infant formula. Other babies need a special formula that has more calories or certain nutrients. Prepare the formula using the package directions or using instructions from your baby’s health care provider.
There are three kinds of formula:
- Ready-to-use liquid formula.
 You pour this formula right into your baby’s bottle.
You pour this formula right into your baby’s bottle. - Concentrated liquid formula. You add water to this liquid formula before giving it to your baby.
- Dry or powdered formula. You add powder to the water before giving it to your baby. Use the scoop that comes with the formula to measure the right amount. Put the water in the bottle first, then the formula, and shake well to mix.
If your baby doesn’t drink all the formula within 1 hour, throw it away. Give her a new bottle of fresh formula at his next feeding.
How do you make bottle feeding safe for your baby?
If your baby has done well with the nipples and bottles used in the hospital, ask to take some home with you. And ask the NICU staff where you can buy them. If the nipples and bottles used in the hospital didn’t work well, try different kinds to find the ones your baby likes. Clean and store the nipples and bottles as it says on the package directions.
If you’re bottle feeding, warm the bottle before you give it to your baby. Put the bottle of milk or formula in a cup of warm water. Test the milk on your wrist to make sure it’s not too hot—it should be lukewarm. Never microwave your baby’s bottle. The breast milk or formula can heat unevenly and burn your baby’s mouth.
When bottle feeding, hold your baby upright and support his head so he can breathe and swallow in a comfortable way. You and your partner can take turns so that both of you feel comfortable feeding your baby. Bottle feeding is a great way to be close and bond with your baby.
Last reviewed June, 2019
Neonatal Resuscitation and Intensive Care Unit
Home / Maternity Hospital / Our departments/
Neonatal Intensive Care Unit is a structural subdivision of maternity hospital No. 10, consists of an intensive care unit and an intensive care unit and is designed for 20 beds.
The main mission and goal of the intensive care unit specialists is to save the life of the baby with the least negative consequences for his health. Children with various perinatal pathologies are admitted to the resuscitation and intensive care unit. Usually they require mechanical ventilation, parenteral nutrition, infusion therapy, correction and restoration of important body functions. Very premature babies with low body weight, who often have severe health disorders, are also transferred here. Parents are regularly provided with full information about the state of health of the newborn, about the characteristics of the disease and the tactics of its treatment.
Children with various perinatal pathologies are admitted to the resuscitation and intensive care unit. Usually they require mechanical ventilation, parenteral nutrition, infusion therapy, correction and restoration of important body functions. Very premature babies with low body weight, who often have severe health disorders, are also transferred here. Parents are regularly provided with full information about the state of health of the newborn, about the characteristics of the disease and the tactics of its treatment.
If your baby has been transferred to the intensive care unit, do not panic and despair. The department staff will teach you how to care for your baby, introduce you to new medical technologies, medical language, rules and procedures that are designed to help your child. Our specialists make every effort to ensure that parents get used to it as soon as possible and begin to understand the needs of their baby. This is very important, because the correct care of the child in these difficult first days depends on how quickly he will be able to adapt to new living conditions outside the mother's body.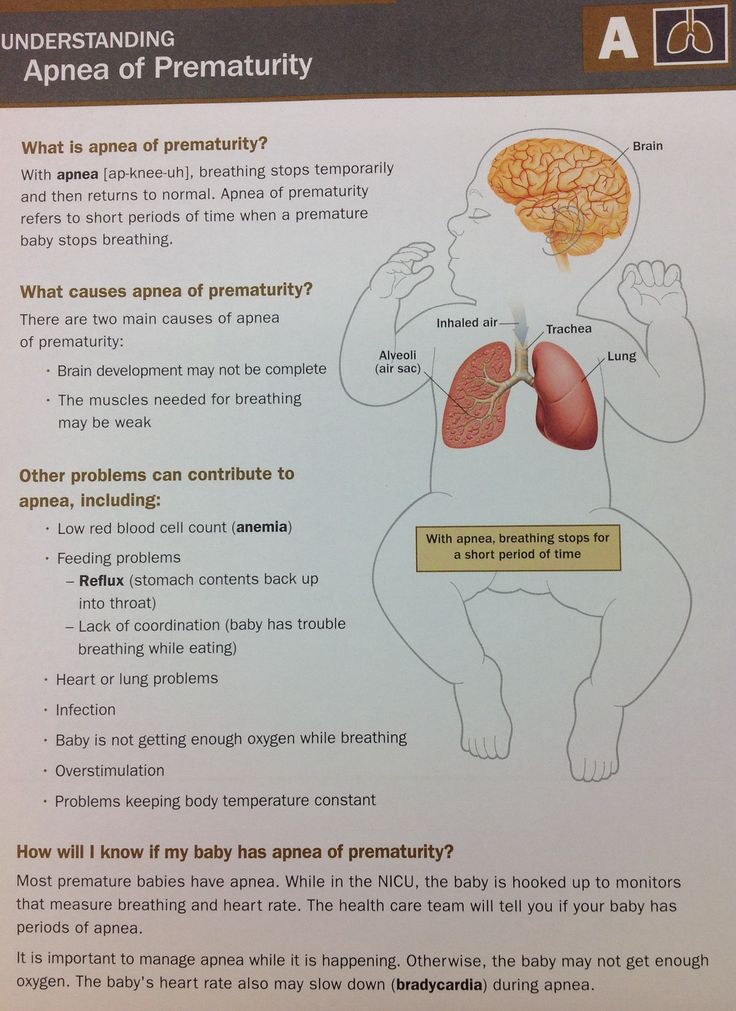 Only after the baby's health improves and does not cause concern, when he is ready for a full life under normal conditions, can we talk about discharge from the department.
Only after the baby's health improves and does not cause concern, when he is ready for a full life under normal conditions, can we talk about discharge from the department.
Resuscitation unit
This includes babies who need extra attention and resuscitation.
Children who have serious neurological problems, who cannot breathe on their own or who were born with very low birth weight are treated here. The resuscitation unit has everything for intensive treatment of the child and constant monitoring of his condition: incubators, monitor monitoring and, of course, qualified personnel.
Intensive care unit.
Rehabilitation treatment takes place here. Children are transferred here from the intensive care unit when adequate spontaneous breathing is restored, there is no need for continuous monitoring of vital functions, premature babies or babies with newborn jaundice.
The resuscitation and intensive care unit is equipped with modern medical equipment, which allows creating comfortable conditions for babies: modern incubators protect from noise and bright light, conditions are created for severely premature babies that are as close as possible to intrauterine conditions. For children who cannot feed on their own, nutrient solutions are introduced through a special probe. Also, if necessary, drugs are used to regulate the heart rate, stimulate breathing, blood pressure, ultrasound. In the premises of the department, the level of humidity and air temperature is constantly monitored.
For children who cannot feed on their own, nutrient solutions are introduced through a special probe. Also, if necessary, drugs are used to regulate the heart rate, stimulate breathing, blood pressure, ultrasound. In the premises of the department, the level of humidity and air temperature is constantly monitored.
Resuscitation and intensive care unit equipment:
- Incubators to maintain optimal temperature and humidity for the child;
- Open resuscitation systems for infusion, oxygen therapy with a heating system;
- Non-invasive ventilation apparatus for spontaneously breathing patients;
- ventilators for artificial lung ventilation;
- Monitors for round-the-clock monitoring of vital body functions (pulse rate, respiration, blood oxygen saturation, hemoglobin, pressure).
- Infusomats - devices for the dosed administration of medicines intravenously;
- Airway sanitation apparatus;
- Phototherapy lamps.

All devices used are certified and connected to a stand-alone station, which guarantees their trouble-free operation.
The medical staff of the intensive care unit is one of the most highly qualified. The team includes a medical unit, middle and junior medical personnel. The department is headed by the head, who is the chief of the doctors, and the senior nurse manages the sisters and junior staff.
The junior staff consists of assistant nurses and nurses who keep the department clean. Their work is very responsible, since the sanitary and hygienic requirements for treatment units are close to those established in operating rooms.
Nurses spend the most time with babies. They are around the clock with little patients, care for them, perform medical appointments, monitor the slightest changes in the condition of children, monitor readings, report on the dynamics of the condition of patients during medical rounds. Each sister is responsible for a certain number of newborns, and if the baby's condition is very serious, then there is only one patient per sister (and at the same time she is constantly busy, since the instability of the condition dictates a constant change in treatment).
Since the department's nurses work in shifts, the parents of severely premature babies have time to get to know many of them. Without a doubt, the nurse is the central figure in the nursing of premature babies, his "mother" for the period of his stay in the department. Good sisters "feel" babies and have not only a kind heart, skillful hands, intuition, but are also extremely observant. They will always point out to the doctor about problems in the condition of the newborn, everyone feels good and calm with them - both patients and doctors.
There are also nurses who provide fluid therapy and therapeutic nutrition for newborns. They monitor the condition of intravascular catheters and infusion systems, the condition of medical equipment, and are responsible for the sterilization of instruments.
The main doctors of the department are anesthesiologists-resuscitators and neonatologists, there are fewer of them than nurses. Their task is to make a diagnosis, develop an intensive care program, monitor and adjust treatment.
Every day the doctor conducts a general examination, listens to the child's heartbeat and breathing pattern. The condition of patients is monitored by equipment and nurses, as well as during medical rounds, which are carried out day and night every 3 hours.
At each round, the doctor evaluates the child's condition: breathing stability, heart function, nutritional adequacy. The doctor of the department determines what tests are needed and with what frequency, what treatment is required. The doctor assesses the need and amount of medical support for cardiac activity, the advisability of prescribing antibiotics to protect against infections, develops a therapeutic nutrition program, and finally decides when the child can be disconnected from the ventilator and when he can be transferred from the intensive care unit to the intensive care unit.
In addition, on-call doctors assist premature babies in the delivery room, transfer them to the department, carry out primary stabilization and treatment until the end of their shift, as well as monitor and treat patients in the evening, at night and on weekends. The duties of the doctors on duty also include registering the child in the intensive care and advisory bureau in order to transport the patient, if necessary, to other hospitals ( According to order No. examinations, children are transferred to specialized departments for newborns of city hospitals in a regulated time frame).
The duties of the doctors on duty also include registering the child in the intensive care and advisory bureau in order to transport the patient, if necessary, to other hospitals ( According to order No. examinations, children are transferred to specialized departments for newborns of city hospitals in a regulated time frame).
All doctors of the department have undergone the necessary training and improvement to provide resuscitation care to newborn children at the bases of the leading medical centers in Moscow and St. Petersburg.
Interaction of parents with department staff
According to the Health Law, the legal representatives of a newborn child are his parents (Article 18), to whom the attending physician provides information about the patient's condition (Article 17). The most complete information is provided in a personal conversation at a specially allotted time (over the phone it is impossible to make sure that the patient's mother or father is really on the other end). The attending doctor has the most complete picture of the diagnosis, changes in the condition, data of laboratory and instrumental studies of his patients, so it makes sense to ask him all the detailed questions. You can also inquire about the condition of the baby by phone.
The attending doctor has the most complete picture of the diagnosis, changes in the condition, data of laboratory and instrumental studies of his patients, so it makes sense to ask him all the detailed questions. You can also inquire about the condition of the baby by phone.
It is important for us that parents receive the most complete and accurate information, do not hesitate to ask even those questions that seem stupid, uncomfortable or inappropriate. We recommend that you write down questions as they arise, so that you can ask them later without forgetting anything.
What to ask your doctor:
- What is my child's condition?
- What is the severity of the condition?
- How is the baby treated (what does the intensive care program consist of)?
- What examinations are planned?
- What is the probability of normal development and possible complications?
- How do I get information about a change in condition and when can I visit my baby?
- Is it possible to perform the sacrament (rite) of baptism?
- How can I help my child get well?
Often, intensive care physicians have to tell relatives things that no one would like to hear, but objectively informing parents about the health of their children is part of our daily work. During meetings with doctors, parents have the opportunity to see and communicate with their children.
During meetings with doctors, parents have the opportunity to see and communicate with their children.
Maternity hospital No. 10 participates in the state program to support breastfeeding, and our specialists do their best to help maintain it. Regardless of the severity of the child's condition, we welcome the communication of parents with the newborn, we consider it necessary for the baby and contribute to his speedy recovery. Visits are limited only during SARS and influenza epidemics in order to protect seriously ill newborns from infection, which can worsen their condition.
Department of resuscitation and intensive care of newborns - RCH
Birth is a beautiful, amazing, and probably the most dangerous event that most of us will ever experience in our lives. Immediately after birth, the child's body needs radical physiological changes. More than 90% of newborns make the transition from intrauterine to extrauterine existence with little external support or completely independently. And to help the remaining few percent of children, a resuscitation service for newborns was created.
And to help the remaining few percent of children, a resuscitation service for newborns was created.
The Resuscitation and Intensive Care Unit provides medical care to newborn babies in need of urgent resuscitation, round-the-clock intensive care and treatment.
In the department there is a pediatric resuscitator on duty around the clock - present at high-risk births, if necessary, providing the entire volume of resuscitation care. If necessary, in the conditions of our department, consultations are held by leading specialists in various fields of medicine.
The mid-level medical staff is represented by experienced nurses, which is of great importance for the work of the intensive care unit, because the fate of little patients depends on the quality of their work.
The main direction of the department's work is the nursing of newborns with low and extremely low body weight (from 500 grams), newborns with intrauterine development anomalies, newborns with intrauterine growth and developmental retardation; as well as the treatment of children with intrauterine infectious diseases, hemorrhagic, convulsive syndrome and features of adaptation to extrauterine life. When nursing premature babies, we strive to create conditions that are as close as possible to intrauterine life. The level of temperature and humidity of the environment is constantly monitored, children are protected from noise, bright light and other adverse factors.
When nursing premature babies, we strive to create conditions that are as close as possible to intrauterine life. The level of temperature and humidity of the environment is constantly monitored, children are protected from noise, bright light and other adverse factors.
High-tech therapies in the neonatal intensive care unit:
• ventilators: conventional, high-frequency, non-invasive ventilation of the lungs
• CPAP therapy
• surfactant therapy
• round-the-clock monitoring of vital functions
equipped with temperature and humidity control systems. In order for the baby to take a pose as close as possible to the intrauterine position, special styling is used.
• infusion station - Compounder technology
• venous access: installation of deep venous lines, peripheral catheters, CVC.
• newborn feeding technologies: parenteral nutrition, therapeutic enteral nutrition
• there is a transport incubator with a ventilator for transporting a newborn from the delivery room to the department
• therapeutic hypothermia for newborns born with severe asphyxia
• ultrasound of the brain, internal organs
• Echo-KS
• Electroencephalography
• X-ray examination
• Express laboratory operates around the clock
• Transcutaneous oximetry
All equipment used is certified and connected to autonomous power supply, which ensures its uninterrupted operation.