No breast milk to feed baby
What to Do, Causes, Treatments
Many expecting parents dream of the moment they’ll first cradle their little one in their arms and start providing for their most basic needs.
For some breastfeeding moms, this expectation may become a source of worry and anxiety if their milk supply doesn’t come in shortly after delivery.
First, take a deep breath. Your baby will be nourished and you’ll be OK. Whatever you’re providing your newborn with right now — be it a few drops of colostrum with formula supplementation or formula alone — your baby is benefiting.
If your milk volume doesn’t seem to be increasing 3 to 5 days after delivery, you may even be tempted to stop trying to breastfeed because you’re worried about your baby having enough food.
But before throwing in the towel on your milk supply or feeling like a failure, take a moment to keep reading — there are things you can do that may help. (And you’re not a failure, period.)
You may feel very alone and like you’ve done something wrong if you find that your breast milk hasn’t come in shortly after birth. But be gentle with yourself — you haven’t done anything wrong. You’re certainly not alone, and there’s a good chance more milk is on its way by in the next week or two.
There are plenty of reasons for a delay. Your breast milk supply may take a little longer to come in or increase if:
- It was a premature birth — particularly if your baby needed to be separated from you right after the birth.
- You have a medical condition like diabetes or polycystic ovary syndrome (PCOS).
- You have obesity.
- You had/have an infection or illness that includes a fever.
- You had a cesarean delivery.
- Your pregnancy included a prolonged bed rest.
- You have a thyroid condition.
- You had a traumatic birth or a postpartum hemorrhage.
- You were unable to breastfeed in the first few hours after giving birth.
Because breast milk production is tied to demand (meaning, removal of milk from your breast), it’s important to make sure that you’re stimulating your breasts frequently and getting out as much milk and colostrum as possible.
Even if you’re making sure to drain your breasts frequently, there are many unique variables that can impact when your milk supply begins to increase.
It’s important to give yourself grace and take measures to encourage a strong supply whenever it does begin to change from colostrum to more mature milk. (See a little lower for some hints to help you with this!)
While it can be extremely frustrating waiting for your breast milk to increase, know that there’s still time for it to happen.
By consistently stimulating your breasts — either with a breast pump or manually — and offering your baby the opportunity to breastfeed, you’ll protect your milk supply and encourage your milk volume to increase sooner rather than later.
Getting help from a professional right away if your milk is coming along a little slower is important to ensure that you establish a healthy milk supply.
There are many things you can do to encourage a greater milk supply both at the hospital and when you’re at home:
Massage your breast area as well as pump or hand express milk
Stimulation of the breast can help in the creation of important milk receptor sites and increase the amount of milk you’re producing. It’s important to spend time engaging and massaging your breasts.
It’s important to spend time engaging and massaging your breasts.
Use a hospital grade pump
These types of pumps have extra suction that can make a big difference not only in the amount of milk that you’re able to extract from your breasts, but also the amount of stimulation your breasts feel. This can lead to a significant increase in the amount of future breast milk you’re able to produce.
Related: The 10 best breast pumps — and how to choose one
Express milk frequently — even if only a small amount comes out!
You should breastfeed, pump, or hand express every 2 to 3 hours in the beginning. Remember that your milk supply is based around supply and demand. It’s essential that you try to drain milk from your breast frequently, so that your body knows it should produce more for your baby.
Especially if your little one is separated from you for any reason, it’s important to use a good hospital grade pump to stimulate and drain milk/colostrum from your breasts.
Hospital staff and lactation consultants can work with you to develop a pumping and feeding plan that will encourage your milk volume to increase.
Use a heating pad or take a warm shower before expressing milk
Heat and massage are great ways to encourage your breast to let down more milk.
Listen to relaxing music
Hearing soothing tunes will help relax you and get the hormones flowing that you need to let down milk. If you’re pumping, looking at pictures of your baby may help as well.
Drink lots of water and get as much sleep as possible
Breast milk includes a lot of water, so just by increasing your water intake you may be able to increase the amount of breast milk you produce.
Many women find that they produce more milk after sleeping, since it offers their bodies a chance to relax and get the right milk-producing hormones flowing.
Bonus points for eating lots of healthy food, since you’ll also produce less breast milk if you get sick.
It may seem like the whole world is weighing on your shoulders as you wait for your milk volume to increase, but there are many ways to make sure that your baby stays healthy and fed.
If your premature baby isn’t putting back on weight after delivery or otherwise needs milk for some reason, don’t worry. Medical staff will feed your little one as much breast milk as you are able to produce and supplement with formula as needed.
Although you may be unhappy with the colostrum or small amount of breast milk you feel you have to offer after a pumping session, your baby will benefit from it! No amount is too little to share with your little one, and any milk that comes from you is specially formatted by nature for your baby.
Using formula for a brief window while your milk increases doesn’t mean that you’ll be unable to breastfeed your baby in the future. If you’re uncomfortable feeding your baby formula, you can speak to your doctor about using donor’s milk. This is milk from people who have produced more than their babies need. It’s screened and stored in milk banks.
It’s screened and stored in milk banks.
Your doctor or lactation consultant will be able to direct you to a local milk bank if you need donor’s milk.
Your baby may not be getting enough to eat if:
- They appear dehydrated (soft spot or eyes sunken in, skin losing elasticity).
- They have fewer wet and dirty diapers. Your baby should be having at least 6 to 8 wet diapers a day after their fifth day of life.
- They cry throughout and following feeds (e.g., no signs of happy milk-drunk baby).
- They’re not back to birth weight by 14 days of life. After an initial decrease in weight right after birth, your baby should be steadily gaining weight.
- They become lethargic or unresponsive.
If you notice signs that your baby isn’t getting sufficient milk, contact your pediatrician as soon as possible. They can determine if there are any other problems and work with you to ensure that your child stays healthy.
It can be both empowering and intimidating to think that breast milk is all your baby needs to stay nourished.
Especially if your breasts aren’t feeling engorged and your milk volume doesn’t seem to be increasing in the first few days after delivery, you may be worried that you’ll never be able to keep your baby full and that you’re somehow inadequate as a parent.
So listen: This is not true! (Read that again.) Remember that there are many reasons why your milk may be a little delayed. Work with a lactation consultant or your doctors and nurses to maximize the amount of milk you produce and ensure good, long breast milk producing potential. A rough start doesn’t have to mean the end to your breastfeeding expectations.
And in the event that your milk doesn’t come in at all due to a medical condition, don’t blame yourself. Your baby will be just fine, and you’re still doing a great job. Fed is best.
10 Best Breast Pumps for 2022
Share on PinterestIllustration by Alyssa KieferWe include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Here’s our process.
Since learning you’re having a baby, you’ve been making decisions, decisions, decisions. You’ve had to decide on a car seat, crib, stroller, and changing table. You’ve had to choose doctors, make medical decisions, and figure out child care.
Many moms don’t need a breast pump, but if you find you need one, and it’s now time to decide on a breast pump, you might be feeling overwhelmed.
We get it! Decision-making can be stressful, especially in the final stretch of pregnancy. So to offer you a bit of a breather, we’ve compiled a list of 10 of the best breast pumps on the market (and descriptions of why they might be the right match for you).
A breast pump is considered a medical device, and the FDA defines it as a device that helps women maintain or increase their milk supply. They can be manual or electric, and they can be single expression (pumping one breast at a time) or double expression (pumping both breasts at the same time). They can also be deemed closed or open system.
Closed system vs. open system breast pumps
As you shop for a breast pump, you’ll first want to consider whether you want a closed or open system. “Closed system” and “open system” aren’t formal medical terms, so brands may use them in different ways. It’s important to make sure you know what a particular brand means by the term if you see it in a product description.
A closed system breast pump is one that includes a barrier to prevent overflow milk from leaking into the pump system. This helps to keep the whole system hygienic. No system can be completely closed, as some air is needed to flow in and out for the vacuuming action of the pump. But a true closed system will come as close as possible.
An open system breast pump lacks this barrier.
It’s possible that you’ll encounter used breast pumps on the market. (After all, according to research, most U.S. mothers who breastfeed also pump.) While it can be tempting to go after a great bargain, there are some parts of a breast pump that can’t be well cleaned once they’ve been exposed to another woman’s breast milk.
Because of the higher risk of someone else’s milk having reached the pump in an open system, many people avoid buying these types of pumps secondhand.
- Best all-around breast pump: Spectra S1 Plus Electric Breast Pump
- Best natural suction breast pump: Haakaa Silicone Manual Breast Pump
- Best manual breast pump: Medela Harmony Manual Breast Pump
- Best hidden/discreet breast pump: Willow Wearable Breast Pump
- Most comfortable manual breast pump: Philips Avent Manual Breast Pump
- Best portable breast pump: Medela Pump In Style Advanced On-the-Go Tote
- Best hospital-grade breast pump: Medela Symphony Double Electric Breast Pump
- Best breast pump for multitasking: Medela Freestyle Flex Double Electric Breast Pump
- Best budget hospital-grade breast pump: Lansinoh Signature Pro Double Electric Breast Pump
- Best budget electric breast pump: Bellababy Double Electric Breast Pump
| Product Name | Price | Type | Closed vs. open open | Portable |
| Spectra S1 Plus Electric Breast Pump | $$ | Electric | Closed | No |
| Haakaa Silicone Manual Breast Pump | $ | Manual | N/A | Yes |
| Medela Harmony Manual Breast Pump | $ | Manual | N/A | Yes |
| Willow Wearable Breast Pump | $$$ | Electric | Closed | Yes |
| Philips Avent Manual Breast Pump | $ | Manual | N/A | Yes |
| Medela Pump In Style Advanced On-the-Go Tote | $$ | Electric | Closed | Yes |
| Medela Symphony Double Electric Breast Pump | $$$$ | Electric | Closed | No |
| Medela Freestyle Flex Double Electric Breast Pump | $$$ | Electric | Closed | Yes |
| Lansinoh Signature Pro Double Electric Breast Pump | $ | Electric | Closed | No |
| Bellababy Double Electric Breast Pump | $ | Electric | Closed | Yes |
- Customer reviews: When choosing what pumps to include on this list, we looked first and foremost at consumer experiences.

- Price: We aimed to include a variety of pumps and price points as we understand that different types of pumps work best depending on the reason for pumping — and budgets vary!
- Convenience: In addition to popularity and prices, we looked at features that make the whole process of pumping easier and more convenient. Let’s face it — when it comes to something you’ll potentially use several times a day, comfort and ease of use should be paramount.
- Brand reputation: Our team thoroughly vets the products we recommend for medical credibility, good business practices, and social impact. You can read more about that process here.
Whatever your needs, one of these options should work for you.
Price guide
- $ = $0–$99
- $$ = $100–$249
- $$$ = $250–$499
- $$$$ = $500+
Best all-around breast pump
Spectra S1 Plus Electric Breast Pump
Price: $$
A closed system, the Spectra offers the option for single or double pumping and has a strong, adjustable vacuum pump that many insurances will cover.
It’s lightweight and portable, with a carrying handle in its design. (The S1 version includes both power cord and battery options, which is very useful on the go!) It also has a nightlight with two light levels and a timer that can be useful for those 2 a.m. pumping sessions.
Particularly in the beginning, it’s important to be careful putting together the backflow valves to keep moisture out of the tubing. The bottles included are not a fit for every baby, so it may be necessary to use a separate bottle brand.
Best natural suction breast pump
Haakaa Silicone Manual Breast Pump
Price: $
This is a very affordable and portable option. The Haakaa offers a convenient way to store breast milk that might otherwise go to waste: Simply attach the Haakaa to the opposite breast from the one your baby is feeding on to preserve milk that is let down at the same time! It’s also perfect for taking out a specific small amount of milk when weaning or trying to reduce breast fullness between feedings.
Because there’s no actual pump involved, there are no concerns about open or closed systems — and it’s easy to completely clean! — but the Haakaa requires more manual labor than an electric pump. The Haakaa’s shape can easily result in spilled milk if knocked over, so it may be worth it to invest the extra money for the storage cover.
Best manual breast pump
Medela Harmony Manual Breast Pump
Price: $
A key component of any manual breast pump is the handle, and the swivel handle of the Medela Harmony Manual Breast Pump sets it apart from the rest.
In part because of the ability to move the handle to the most comfortable position for each individual user and switch positions every time if needed, the Harmony offers a great amount of comfort and ease for a manual pump. Plus, it has the lower price point and higher portability than most electric models. Like the Haakaa, the Harmony is easy to clean, since there’s no motor or tubing.
The pump can lose suction over time as the O-ring becomes ragged, but it’s fairly easy to locate spare Medela parts to replace or fix this pump. (Additionally, the low price point makes it more affordable to completely replace this pump if necessary.) Like all manual pumps, if you intend to do a lot of pumping, this may not be the choice for you.
(Additionally, the low price point makes it more affordable to completely replace this pump if necessary.) Like all manual pumps, if you intend to do a lot of pumping, this may not be the choice for you.
Best hidden/discreet breast pump
Willow Wearable Breast Pump
Price: $$$
A hands-free option, the Willow is a useful pump for working women and anyone frequently on the move. Because it fits inside your bra without the need for cords, this is an extremely popular option for people who need to pump in public. It comes with extensive customer service options and doesn’t get a lot of complaints about lost milk due to leaking.
Because of the Willow’s size, its bags can only hold a smaller amount of breast milk than other pump containers, so some lactating individuals find it necessary to switch storage bags mid-session. The Willow also involves a slightly more complicated method of assembly and can be more difficult to latch in the beginning.
Most comfortable manual breast pump
Philips Avent Manual Breast Pump
Price: $
The makers of the Philips Avent Manual Breast Pump really were thinking about comfort in the creation of this pump. It’s designed to allow you the option of manually pumping in a reclined position. The silicone liner also makes the actual pump more comfortable than those made only with plastic! Like most manual pumps, the parts are easy to disassemble and clean. It’s also easy to transport and comes with a more affordable price tag.
The Philips Avent Manual is on the louder side for a manual pump, as the handle doesn’t have a bumper to prevent it from banging against the collection bottle. It also can give your hands a bit of a workout since the handle doesn’t swivel and the grip can’t be adjusted. Although parts can wear out, because this is a more common brand of pump, replacement parts are easy to locate.
Best portable breast pump
Medela Pump In Style Advanced On-the-Go Tote
Price: $$
Built into a bag, this pump is ready to be taken on the go! The Medela Pump In Style was designed to optimize suction and pumping efficiency, so speedy pumping sessions are frequently noted when using it. (It doesn’t offer the same amount of control over suction levels as some other pumps, however.) As a closed system pump, it’s more hygienic than some other options.
(It doesn’t offer the same amount of control over suction levels as some other pumps, however.) As a closed system pump, it’s more hygienic than some other options.
A little louder than the Spectra, this breast pump isn’t the quietest, but it’s easy to find spare parts for it. It’s lightweight, so it travels well.
Best hospital-grade breast pump
Medela Symphony Double Electric Breast Pump
Price: $$$$
We’re not going to lie: This is a major splurge, and your situation is unlikely to require buying it — but you can consider renting it. If you’re trying to initiate or increase your breast milk supply, a hospital-grade pump will provide more suction your breasts are needing. The Medela Symphony is the choice of many hospitals. It might be a good choice if you are trying to establish milk for an adopted baby.
This pump has great suction that mimics a baby’s actual nursing pattern. It is such a well-sealed closed system pump that hospitals are willing to let multiple lactating women use the same machine. It’s also a quieter pump, which many parents appreciate.
It’s also a quieter pump, which many parents appreciate.
While this pump has great longevity, it’s heavier and not great for portability. Also, due to the hefty price tag on this pump, it may be worth your while to see if there is a hospital or birth center in your area that rents out this pump.
Best breast pump for multitasking
Medela Freestyle Flex Double Electric Breast Pump
Price: $$$
This is a hands-free option for the mom on the move! The Medela Freestyle is extremely light and fits conveniently in a purse or diaper bag. It comes with a digital display and timer that includes a memory function to save your favorite expression suction patterns. It’s also compatible with most top flat nursing bras.
The downside to the Medela Freestyle Flex is that it doesn’t include as strong of a motor as the hospital-grade. (When the battery is low, the suction decreases significantly, so it may become necessary to plug it in.) The Freestyle Flex is also a louder pump.
Best budget hospital-grade breast pump
Lansinoh Signature Pro Double Electric Breast Pump
Price: $
This is a very price-effective hospital-grade pump. The Lansinoh is lightweight, portable, and has a backlit LCD screen. It runs on a power cord or batteries. The three pumping styles and adjustable suction options help with letdown, and the closed system keeps the pump hygienic.
The Lansinoh isn’t the quietest of the breast pumps available and can run through batteries quickly, but it’s a very affordable option for people seeking a hospital-grade pump.
Best budget electric breast pump
Bellababy Double Electric Breast Pump
Price: $
The Bellababy Double Electric offers a touch HD display screen with a sensitive touch panel. This screen has all the information a lactating individual could hope for, as well as a convenient one-touch option for controlling the pump. The Bellababy Double Electric offers a closed system with strong suction that continues well even with a low battery.
While the Bellababy Double Electric is portable, it’s not the most compact option on the market. It also tends to run a little louder than some pumps. It has a lot of parts to clean and sanitize.
If your baby is having trouble breastfeeding, a breast pump will help you maintain your supply. Going back to work or any planned separations from your baby often also requires mothers to use a breast pump.
When choosing a breast pump, there are many things to consider:
- Your pumping needs and lifestyle. How often are you going to use your pump? What’s your goal for pumping — maintaining milk supply, doing it daily during work hours, etc.?
- Which pumps your health insurance will cover. As of late 2012, private health insurers in the United States do need to cover breast pumps under the Affordable Care Act.
- Price point. Find that balance between your budget and the type of pump that will serve your needs best.

- Portability.
- Strength/variability of suction.
- Comfort. Does the pump fit your body well?
- Loudness of the pump.
- Other parts you might need in addition to the pump.
Don’t forget to consider cost-effective ways to test out a potential pump before purchasing it for yourself. Some hospitals offer pump rentals. Talk with a local lactation consultant about why and how to use a breast pump and where to rent them.
When should I start using my breast pump?
When your baby is gaining weight and keeping a healthy weight, experts recommend waiting six weeks to use a breast pump to first establish a breastfeeding routine. However, low birth weight, separation from your baby, and other factors may mean your doctor recommends you start sooner (but never during pregnancy).
How often should I clean my breast pump?
If you’re using a shared pump such as a rented medical-grade breast pump, clean it before each use. The Centers for Disease Control (CDC) recommends cleaning any breast pump parts that come into contact with breast milk after each use and ensure they dry thoroughly. This is true for both shared pumps and if you own your pump.
The Centers for Disease Control (CDC) recommends cleaning any breast pump parts that come into contact with breast milk after each use and ensure they dry thoroughly. This is true for both shared pumps and if you own your pump.
How do I know which breast pump will work for me?
Most breastfeeding mothers do not need a pump at all. If you decide to get a pump, most lactation experts agree that a double expression breast pump is ideal, though a single expression pump can be beneficial in certain scenarios, such as when nursing and pumping at the same time.
You can also choose between manual and electric breast pumps, which comes down to preference.
If you have a low milk supply, need to build up stores, or establish your milk supply, a hospital-grade breast pump is a good choice. If your baby spends time in the NICU or is born prematurely, your doctor may recommend one. In most cases, a double electric pump will fulfill pumping needs.
How do I pump breast milk?
Always wash your hands and then assemble the breast pump parts. For electric breast pumps, center the breast shield over your breast, pressing gently. Start on a low intensity and then increase slowly if you want. It should never feel painful. Manual pumps require a slightly different process. You will want to stimulate your breast by hand first and then center and press the pump to your breast before you start manually pumping the handle. Check out our full article on how to pump here.
For electric breast pumps, center the breast shield over your breast, pressing gently. Start on a low intensity and then increase slowly if you want. It should never feel painful. Manual pumps require a slightly different process. You will want to stimulate your breast by hand first and then center and press the pump to your breast before you start manually pumping the handle. Check out our full article on how to pump here.
What breast pump do lactation experts recommend?
Lactation experts all may have different favorite breast pumps they recommend, but they do all agree that a double expression pump is the best so you can pump on both sides at the same time.
Will a breast pump change my breasts?
Your breasts after breastfeeding and pumping may be different than before the baby, but many women experience minimal long-term changes. Nipples may change in size and appearance while breastfeeding, and stretch marks may intensify.
Pumping should never be painful, but breast pumps can cause trauma to breasts when used incorrectly or too often. So it’s important to choose the right size and not to overpump, which can lead to engorgement and mastitis.
So it’s important to choose the right size and not to overpump, which can lead to engorgement and mastitis.
There’s a breast pump for every person and situation.
Whether you need to pump every day on the go, want something to help take a bit of the edge off in the middle of the night, or are looking for a pump designed to help bring in your milk, these options should help take one more decision off your to-do list. (Don’t worry. You’ll still have plenty of other ones to make.)
Signs of lack of milk | Improving lactation
Many mothers are concerned about insufficient milk production, but it is not always easy to find out if milk is really low. Read our article to understand if this is true and what can be done about it.
Share this information
“Do I have enough milk?” - a question that is often asked by young mothers. If your baby is healthy and growing well, there is no reason to worry. However, if you are still worried about milk production, it is best to consult a specialist as soon as possible. If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease.
If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease.
Causes of insufficient milk supply
Some mothers do not produce enough breast milk for medical reasons, which include: approximately three days after birth). 1
If you have any of the conditions listed, contact your lactation consultant or healthcare provider.
How milk is produced
With the advent of milk, the breast begins to work on the principle of supply and demand. Each time after it is emptied, whether it is feeding the baby or pumping, even more milk will be produced.
Each time after it is emptied, whether it is feeding the baby or pumping, even more milk will be produced.
This is why milk production may be reduced if you give formula to your baby - your body will not get the signal to produce more milk because it will remain.
The way your baby eats also affects milk production. The more often and better he sucks the breast, the bigger it will be. If your baby eats only a small portion at one feeding, it is necessary to express milk regularly to maintain the level of its production. Read more about this below.
Signs that the baby is not getting enough milk
Although low milk production is rare, the baby may have difficulty feeding in the first few weeks, but for other reasons. You may not be feeding him often enough or for enough time, especially if you're trying to stick to a specific schedule. The baby may not latch on properly, or it may have features that make it difficult to take in milk.
The following signs indicate that the baby is not getting enough milk:
- Poor weight gain.
 In the first few days of life, newborns normally lose 5 to 7%, and sometimes even up to 10%, of their birth weight. However, after that, they should gain at least 20–30 g per day and regain their birth weight by 10–14 days. 5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately.
In the first few days of life, newborns normally lose 5 to 7%, and sometimes even up to 10%, of their birth weight. However, after that, they should gain at least 20–30 g per day and regain their birth weight by 10–14 days. 5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately. - Not enough wet and soiled diapers. A good indicator of whether a baby is getting enough milk is the number of diapers used per day. Check out our article detailing the norm for wet and soiled diapers in Breastfeeding Your Newborn: What to Expect in the First Week. Seek medical advice if something bothers you or you notice that the number of soiled diapers has begun to decrease.
- Dehydration. If your baby has dark urine, dry mouth or jaundice (yellowing of the skin or eyes), or baby is lethargic, has lost appetite, and may be dehydrated.
 6 Dehydration can be caused by fever, diarrhoea, vomiting or overheating. If you notice any of these symptoms, seek medical attention as soon as possible.
6 Dehydration can be caused by fever, diarrhoea, vomiting or overheating. If you notice any of these symptoms, seek medical attention as soon as possible.
Misconceptions about lack of milk
Newborns usually eat very frequently, about 10-12 times a day or every two hours. This does not mean that they do not have enough milk. Keep in mind that breastfeeding is also about comfort, so it's hard to tell how much milk a baby eats at each feed as the amount can vary.
You have enough milk even if:
- the child wants to eat often;
- the child does not want to be laid down;
- the child wakes up at night;
- feeding is fast;
- feeding takes a long time;
- after feeding, the child takes another bottle;
- Your breasts are softer than in the first weeks;
- milk does not leak or has stopped leaking;
- You cannot express much milk;
- You have small breasts.
What to do about insufficient milk production
If you suspect that your baby is not getting enough milk, contact a lactation consultant or your doctor. He will determine if you have enough milk and check how the baby is latch-on and if he is getting enough milk. He may also suggest changing the feeding position or the way the baby is attached to the breast to make it easier.
He will determine if you have enough milk and check how the baby is latch-on and if he is getting enough milk. He may also suggest changing the feeding position or the way the baby is attached to the breast to make it easier.
Also try holding your baby close to you more often to increase skin-to-skin contact before and during feedings. This stimulates the production of the hormone oxytocin, which promotes milk flow. Use relaxation techniques, such as listening to your favorite soothing music, to reduce anxiety that can negatively impact milk production. 8
With proper support, most under-lactating mothers can breastfeed their babies at least partially, and some manage to normalize production.
If your baby is unable to get enough milk directly from the breast (perhaps because he was born prematurely or has special needs), you need to express milk to support his production. Your doctor may prescribe you special drugs that stimulate lactation.
If you are unable to express enough milk, you will need to supplement your baby with donor milk or formula. This should also take place under the supervision of a physician. The Supplemental Nursing System (SNS)* is a great way to help your baby get all the milk he needs at the breast.
This should also take place under the supervision of a physician. The Supplemental Nursing System (SNS)* is a great way to help your baby get all the milk he needs at the breast.
How to increase your milk production with a breast pump
If you need to increase your milk production in the first five days after giving birth, you can use a dual electronic breast pump with lactation start technology, such as the Medela Symphony**. Such a breast pump imitates the sucking of the breast by a child and helps to increase milk production in the future. 9
After your milk comes in, double pumping allows you to get more milk in less time. 10 This method helps to better empty the breast, which also improves lactation.
Although every mother is different, it is often recommended to express milk immediately or one hour after a feed. This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow. "
"
You will probably only be able to express a little milk at first, but don't be discouraged - if you express regularly, your milk supply will increase. Try to empty your breasts - by putting your baby to your breast or expressing milk - 8 to 12 times a day, including one nightly session, when your levels of prolactin (the hormone responsible for producing milk) are highest. The more often you empty your chest, the better. After two to three days of regular pumping, you will notice a significant increase in milk production. For tips on how to get more milk with every pump, see Tips for Using a Breast Pump.
Pumping with massage to get more milk
If your baby is not lating at all or you are not yet able to express enough milk for him, a technique called “massage pumping” may be helpful. It helps mothers increase the amount of milk they get in one pumping session. 11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.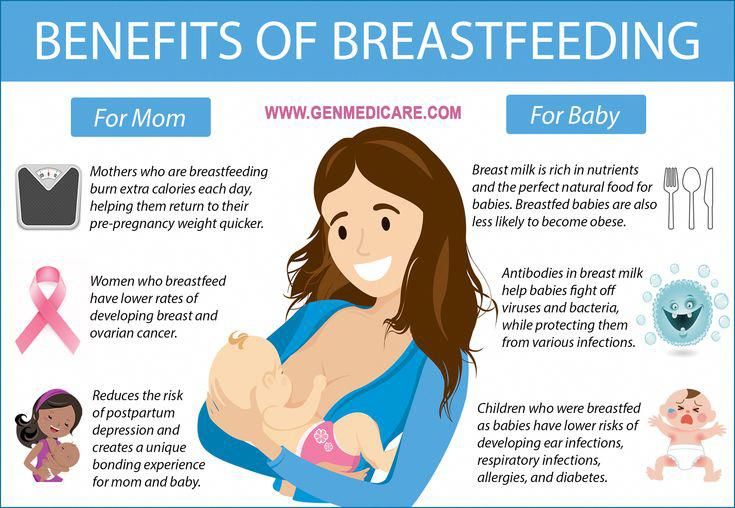
A few simple steps are required:
- Massage your breasts.
- Perform a double pump while wearing a special bustier top that allows you to keep your hands free.
- While expressing, squeeze the chest with all fingers for a few seconds. Release and repeat. Squeeze both breasts until the milk flows in a thin stream.
- Massage the chest again.
- Express milk manually or with a single breast pump, squeezing each breast in turn to empty them as completely as possible.
When your baby starts to gain weight and milk production increases, you can switch to exclusive breastfeeding.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. 9 E et al . Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
2007;12(4):211-221. 9 E et al . Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828. - Neifert M.R. et al., "Inability to Lactate Due to Deficiency of Glandular Breast Tissue". Pediatrix (Pediatrics). 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby. " Bers. 1990;17(1):31-38.
" Bers. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev . 2014;22(1):31-42. - S. Tavia S., McGuire L., "Natural Weight Loss and Gain in Healthy, Exclusively Breastfed Full-Term Infants." Brestfeed Rev (Breastfeeding Review). 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. Pp. 1128.
7 World Health Organization. [Internet]. Neonatal Care . 2012;12(2):112-119 - Keith D. R. et al., "Effects of listening to music on the amount, fat content, composition and calorie content of breast milk in mothers of premature and seriously ill children." Adv Neonatal Care. 2012;12(2):112-119
R. et al., "Effects of listening to music on the amount, fat content, composition and calorie content of breast milk in mothers of premature and seriously ill children." Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J. Perinatol. 2012;32(2):103-10. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression.Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping. " Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
" Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [ Accessed 04/30/2018]. - Stanford University School of Medicine [Internet]. Stanford, CA, USA: "Increased milk production from hand expression"; 2017. [Page accessed 04/30/2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J. Perinatol. 2009;29(11):757-764. - Morton J. et al., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants." J Perinatol (Journal of Perinatology). 2009;29(11):757.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 dated 07/19/10
** RU No. ФСЗ 2010/06525 dated 03/17/2021
ФСЗ 2010/06525 dated 03/17/2021
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after giving birth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth days, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And it will be possible to feed a child with expressed precious colostrum. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
“I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination for effective suckling.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
- Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.

Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the early days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional. ”
”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does a newborn urinate and defecate?
What goes into the body must go back out.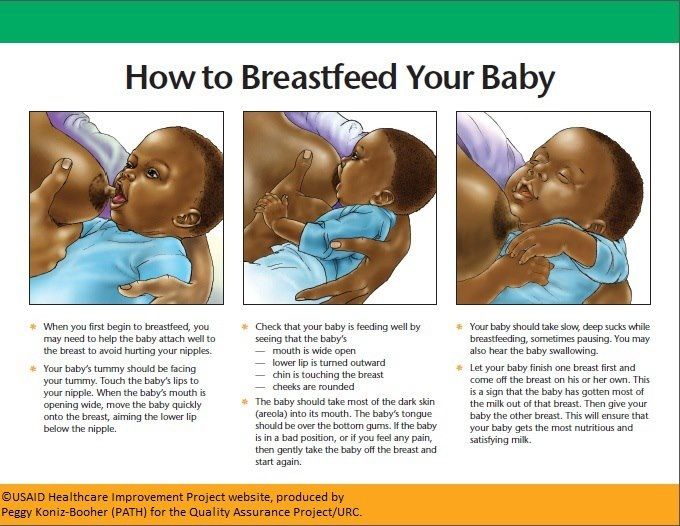 Colostrum
Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Second day
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).

- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
you may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
But if there are no frightening symptoms and the baby is growing at a normal pace, then he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
- Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al.