One month baby feeding amount
Amount and Schedule of Baby Formula Feedings
- In the first week after birth, babies should be eating no more than about 1 to 2 ounces (30 to 60 ml) per feed.
- During the first month, babies gradually eat more until they take 3 to 4 ounces (90 to 120 ml) per feed, amounting to 32 ounces per day. Formula-fed babies typically feed on a more regular schedule, such as every 3 or 4 hours. Breastfed babies usually take smaller, more frequent feedings than formula-fed infants.
If your baby sleeps longer than 4 to 5 hours during the first few weeks after birth and starts missing feedings, wake them up and offer a bottle.
By the end of the first month: Your baby will be up to at least 3 to 4 ounces (120 mL) per feeding, with a fairly predictable schedule of feedings about every 3 to 4 hours.
By 6 months: Your baby will consume 6 to 8 ounces (180–240 mL) at each of 4 or 5 feedings in 24 hours.
Formula feeding based on body weight
On average, your baby should take in about 2½ ounces (75 mL) of infant formula a day for every pound (453 g) of body weight. But they probably will regulate their intake from day to day to meet their own specific needs, so let them tell you when they've had enough. If they become fidgety or easily distracted during a feeding, they're probably finished. If they drain the bottle and continues smacking their lips, they might still be hungry.
There are high and low limits, however. If your baby consistently seems to want more or less than this, discuss it with your pediatrician. Your baby should usually drink no more than an average of about 32 ounces (960 mL) of formula in 24 hours. Some babies have higher needs for sucking and may just want to suck on a pacifier after feeding.
On-demand feeding
Initially it is best to feed your formula-fed newborn a bottle on demand, or whenever they cry with hunger. As time passes, your baby will begin to develop a fairly regular timetable of their own. As you become familiar with their signals and needs, you'll be able to schedule their feedings around their routine.
Eating & sleeping patterns
Between 2 and 4 months of age (or when the baby weighs more than 12 lb. [5.4 kg]), most formula-fed babies no longer need a middle-of-the-night feedings. They're consuming more during the day, and their sleeping patterns have become more regular (although this varies considerably from baby to baby). Their stomach capacity has increased, too, which means they may go longer between daytime feedings—occasionally up to 4 or 5 hours at a time.
If your baby still seems to feed very frequently or consume larger amounts, try distracting them with play or with a pacifier. Sometimes patterns of obesity begin during infancy, so it is important not to overfeed your baby.
Getting to know your baby's feeding needs
The most important thing to remember, whether you breastfeed or bottlefeed, is that your baby's feeding needs are unique. No book―or website―can tell you precisely how much or how often they need to be fed or exactly how you should handle them during feedings. You will discover these things for yourself as you and your baby get to know each other.
More information
- How Often and How Much Should Your Baby Eat?
- Making Sure Your Baby is Getting Enough Milk
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
- Last Updated
- 5/16/2022
- Source
- Adapted from Caring for Your Baby and Young Child: Birth to Age 5 7th Edition (Copyright © 2019 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Bottle-Feeding (Formula) Questions
Is this your child's symptom?
- Formula and bottle-feeding questions
Topics Covered for Formula Feeding
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice:
- Types of formulas
- Switching formulas and milk allergies
- Powdered versus liquid formulas
- Whole cow's milk, 2%, 1% and skim milk
- Vitamins and iron
- Water to mix with the formula
- Extra water
- Amounts: how much per feeding?
- Schedules or frequency of feedings
- Length of feedings
- Night feedings: how to eliminate?
- Formula temperature
- Formula storage
- Cereals and other solids
- Burping
- Baby bottle tooth decay
- Traveling
- Nipples and bottles
- Normal stools
- Breast discomfort
When to Call for Bottle-Feeding (Formula) Questions
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected.
No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Will not drink or drinks very little for more than 8 hours
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Does not seem to be gaining enough weight
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bottle-feeding question about a healthy baby
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Bottle (Formula) Feeding
- Types of Formulas:
- Milk-protein formulas, soy-protein formulas, and hydrolysate formulas
- Soy formulas don't contain lactose or cow's milk protein.
Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason.
- Hydrolysate formulas mean the protein is broken down. These are advised when children are sensitive to both soy and milk protein.
- Switching Formulas and Milk Allergies:
- Switching from one milk-based formula to another is not helpful for any symptom. It is also not harmful.
- Switching from milk formula to soy formula is sometimes helpful for severe diarrhea. This may occur from temporary low lactase levels. It may also be used for those families who are vegetarian.
- Switching from milk formula to soy is sometimes helpful for cow's milk allergy. A cow's milk allergy occurs in 1-2% of infants. Most often, protein hydrolysate formulas (such as Alimentum) are advised. This is because 15% of these infants are also allergic to soy protein.
- Switching formulas for frequent crying, spitting up or gas is rarely helpful.
- Don't switch formulas without talking with your child's doctor.
- Powdered versus Liquid Formulas:
- Formulas come in 3 forms: powder, concentrated liquid and ready-to-feed liquid.
- Concentrated formulas are mixed 1:1 with water.
- Ready-to-feed formulas do not need any added water.
- Powdered formulas are mixed 2 ounces (60 mL) of water per each level scoop of powder. Never add extra water because dilute formula can cause a seizure.
- Powdered formula costs the least. Ready-to-feed formula costs the most.
- Powdered formula is the easiest to use to supplement breastfeeding.
- Ready-to-feed formula is the easiest to use for traveling.
- Whole Cow's Milk, 1%, 2% and Skim Milk:
- Cow's milk should not be given to babies before 12 months of age. Reason: raises risk of iron deficiency anemia.
- Skim milk (fat free milk), 1% low fat milk or 2% milk should not be used before 2 years.
Reason: the fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
- Vitamins and Iron:
- For all infants, use a formula that has iron in it. This helps to prevent iron deficiency anemia.
- The iron amount in iron-fortified formulas is too small to cause any symptoms. Iron in formulas does not cause constipation or diarrhea.
- Iron-fortified formulas contain all the vitamins and minerals needed.
- Extra vitamins are therefore not needed for infants taking formula.
- Fluoride. Babies no longer need to take fluoride drops. Reason: the fluoride in toothpaste works very well. For children at high risk for tooth decay, your dentist may use fluoride varnish.
- Water to Mix With the Formula:
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
Heat cold water to desired temperature. Add this to powder or formula concentrate.
- Exceptions:
- Untested well water or
- City water with recent contamination or
- Developing countries with unsafe water supply or
- Your child has decreased immunity.
- For these conditions, use distilled water, bottled water, or filtered tap water.
- Another option is to use city water or well water that has been boiled. Boil for 10 minutes. Add 1 extra minute per each 1,000 feet (305 meters) of elevation.
- Bottled water costs more than distilled water.
- If making a batch of formula, distilled, bottled or boiled water is needed.
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
- Extra Water:
- Babies less than 6 months of age should not be given any extra water. Reason: regular formula is 85% water. Also, water can cause harm at this age.
- Infants older than 6 months of age can have some extra water. Reason: water may be needed after starting solid foods or if weather is very hot.
Safe at this age.
- Limit water for infants age 6 to 12 months: don't give more than 4 ounces (120 mL) of extra water per day. On hot days, can give up to 8 ounces (240 mL) per day (AAP).
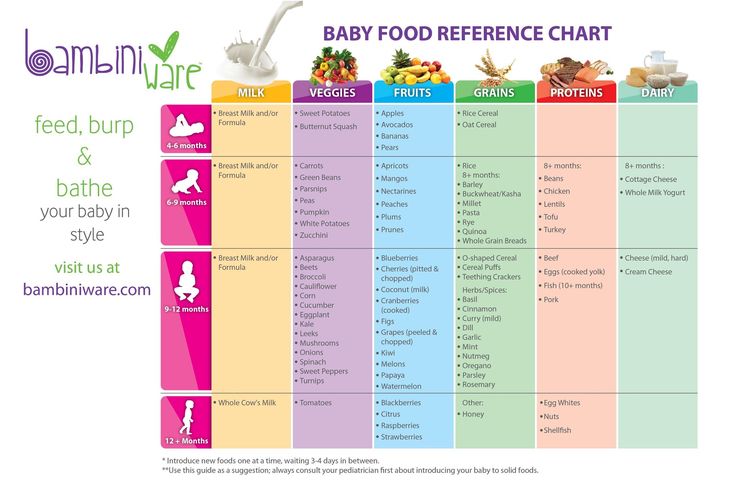
- Amounts - How Much Per Feeding: Newborn to 6 Months Old
- The average amount of formula that babies take per feeding is:
- Newborn: 1-2 ounces (30-60 mL) per feeding
- 1 month old: 3-4 ounces (90-120 mL) per feeding
- 2 months old: 5 ounces (150 mL) per feeding
- 4 months old: 6 ounces (180 mL) per feeding
- 6 months old: 7-8 ounces (210-240 mL) per feeding
- The amount can vary depending on the baby's weight and if the baby is going through a growth spurt.
- A baby's appetite varies throughout the day. If the infant stops feeding or loses interest, the feeding should be stopped.
- If healthy babies are not hungry at several feedings, increase the feeding interval.
- The most amount of formula advised per day is 32 ounces (1 liter).
- Over-feeding can cause vomiting, diarrhea or too much weight gain.
- If your baby needs over 32 ounces (1 liter), talk to your doctor about starting solids.
- Get rid of any formula left in bottle at end of each feeding. Do not reuse this leftover formula. Reason: contains germs that can grow.
- Frequency of Feedings (Schedules): Babies mainly need to be fed when they are hungry. If your baby is fussy and it's been more than 2 hours, feed him. Some guidelines are listed below:
- From birth to 3 months of age, feed every 2 to 3 hours.
- From 3 to 9 months of age, feed every 3 to 4 hours.
- Infants often set their own schedule by 1 to 2 months of age.
- Length of Feedings:
- Feedings shouldn't take more than 20 minutes.
- If the feeding is prolonged, check the nipple to be sure it isn't clogged.
- A clean nipple should drip about 1 drop per second. Check this when the bottle of formula is turned upside down.
- Night Feedings - How to Get Rid of Them:
- Most newborns need to be fed at least twice each night.
- Most formula-fed babies give up night feedings by 4 months of age. The tips below can help your baby sleep for longer stretches during the night:
- Keep daytime feeding intervals to at least 2 hours. Slowly stretch them to 3 hours.
- During daytime, your baby shouldn't sleep for more than 3 hours at a time. If your baby naps longer than that, wake him for a feeding.
- Place your baby in the crib drowsy but awake. Don't bottle-feed or rock until asleep.
- Make middle-of-the-night feedings brief and boring compared to daytime feedings. Don't turn on the lights or talk to your child. Feed him rather quickly.
- Formula Temperature:
- Most babies like formula at body temperature.
- In the summertime, some infants prefer formula that's cooler.
- In the wintertime, some prefer warm formula.
- The best temperature is the one your infant prefers. Either way, there's no health risk involved.
- Just make sure the formula is not too hot. Reason: it can burn your baby's mouth.
- Formula Storage:
- If you can, make your child's formula fresh for each feed. However, if formula needs to be made ahead of time:
- Prepared formula should be stored in the refrigerator. It must be used within 24 hours.
- Open cans of formula should also be kept in the refrigerator. They should be covered and used within 24 hours.
- Prepared formula left at room temperature for more than 1 hour should be discarded.
- Leftover used formula should always be tossed. Reason: contains germs that can grow.
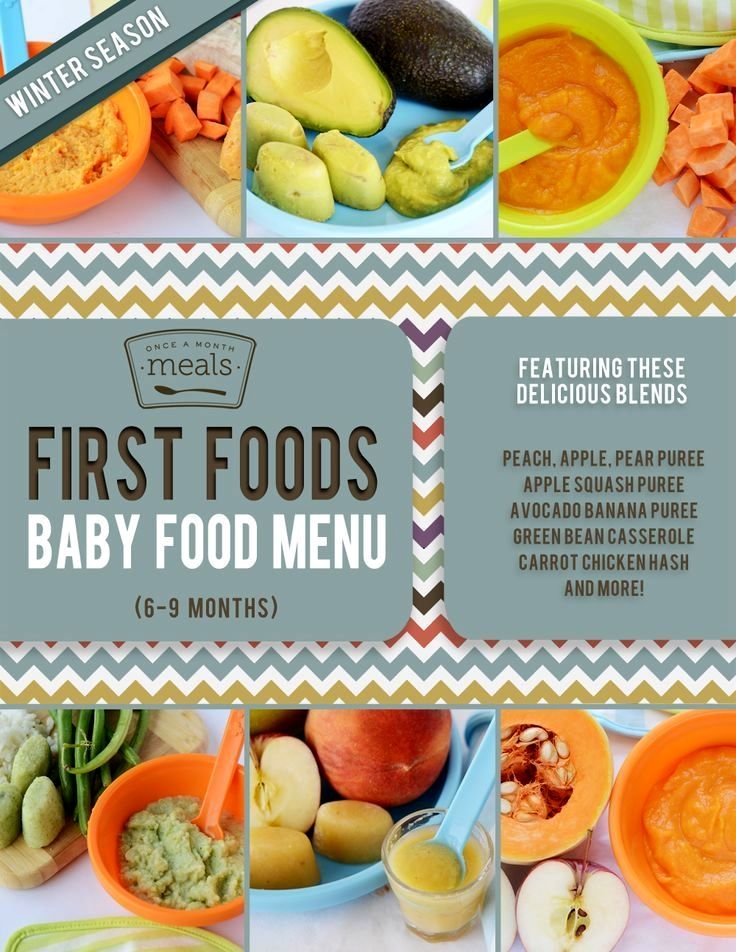
- Cereals and Other Solids:
- Bottle-fed infants should be started on baby foods around 6 months of age. First baby foods can be cereals and/or fruit.
- Starting before 6 months is not needed.
Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging.
- Solids don't increase sleeping through the night for bottle-fed infants.
- Delaying solids past 9 months of age is not advised. The delay runs the risk that your infant will refuse solids.
- Burping:
- It is not harmful if a baby doesn't burp.
- Burping is an option, but not required.
- It can decrease spitting up, but it doesn't lessen crying.
- Burping can be done twice per feeding, once midway and once at the end.
- If your baby does not burp after 1 minute of patting, it can be stopped.
- Baby Bottle Tooth Decay:
- Some older infants and toddlers are used to a bottle before sleeping.
- Falling asleep with a bottle of milk or juice can cause severe tooth decay.
- Prevent this bad habit by not using the bottle as a pacifier. Also, do not use the bottle as a security object.
- If you cannot stop the bottles, fill it with water. Use water instead of formula or milk at bedtime.
- Traveling:
- Use bottles of ready-to-feed formula (most expensive).
- Or mix formula ahead of travel and carry in a cold insulated container.
- Or use powered formula. Put the required number of scoops in a bottle. Carry clean water in a separate bottle. Mix before each feeding.
- Nipples and Bottles:
- Any nipple/bottle products are fine.
- It is not necessary to sterilize bottles or nipples. Wash them with soap and water. Rinse them thoroughly.
- It is also safe to wash bottles and nipples in the dishwasher.
- Formula-fed Stools, Normal:
- Meconium Stools are dark greenish-black, thick and sticky. They normally are passed during the first 3 days of life.
- Transitional Stools are a mix of meconium and milk stools.
They are greenish-brown and looser. They are passed day 4 to 5 of life.
- Normal Milk Stools without any meconium are seen from day 6 on.
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter. Green stools are also normal (usually caused by bile).
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They are soft and solid.
- Breast Discomfort in Bottle-feeding Mothers:
- Even though you chose not to breastfeed, your breasts will make milk. Breast milk comes in on day 2 or 3. Swollen breasts can be painful for a few days. Here is what to do:
- Ibuprofen. Take 400 mg of ibuprofen (such as Advil) 3 times per day. This will help to lessen pain and swelling. There's no special prescription medicine for this.
- Cold Pack. Use a cold pack or ice bag wrapped in a wet cloth. Put it on your breasts for 20 minutes. Do this as often as needed. This will decrease milk production. Do not use heat. Heat will increase milk production.
- Pumping. For moderate pain, hand express or pump off a little breast milk. This will help to reduce your pain. Pumping breast milk can increase milk production. But, doing this to take the edge off your discomfort is not harmful.
- Bra. Wear a bra that offers good breast support or a sports bra. Wear it 24 hours a day.
- Binding. Binding the breasts by wearing a tight bra is no longer advised. Binding by using an elastic wrap is also not advised. Binding can increase the risk of breast infections (mastitis).
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 02/22/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
what products are possible, features of complementary foods
It is no secret that young and not very experienced mothers receive information on the nutrition of an infant, including recommendations on how to introduce the first complementary foods, mainly from two sources: grandmother's stories and from the Internet. Unfortunately, both of these respected sources of information may voluntarily or not voluntarily, but be very mistaken, since grandmothers grew up in a more prosperous time in terms of environmental conditions, and the Internet is littered with various articles that are rarely written by professionals, moreover, they rely either on explicit outdated guides on baby food, or frankly on unverified information.
In this article, I will try to combine the latest scientific data and recommendations on how to introduce the first complementary foods with many years of observations from the experience of a practical pediatrician and an allergist-immunologist.
At what age is it time to introduce the first complementary foods
According to the recommendations of the Research Institute of Nutrition of the Russian Academy of Medical Sciences, the first complementary foods can be introduced from 4.5 - 5 months, regardless of the type of feeding. This is "average". In practice, the choice of when to start introducing complementary foods still depends on the individual characteristics of the child. For example, for a child with widespread atopic dermatitis (diathesis), we will not introduce complementary foods until at least acute skin symptoms, such as cracks, weeping or secondary eczema, have steadily disappeared. Increased dryness and flaking of the skin, of course, require constant application of moisturizers to the skin, but in no case are they a contraindication to the start of the introduction of the first complementary foods.
Another important point when choosing the time to start introducing complementary foods is the dynamics of the child's weight gain. The more intensively the child gains in height and weight, the sooner he may need additional calories, since the energy value of breast milk or artificial formula alone will most likely not be enough for a child who grows faster than his peers by 4 - 5 months. We must not forget that natural products contain a fairly large range of minerals and vitamins, and a mother’s body, alas, cannot be an eternal and bottomless source of useful nutrients, somewhere something will gradually begin to be missed.
In addition, the nature of lactation in the mother has a great influence on the timing of the introduction of complementary foods. If a nursing mother begins to feel a lack of milk, I would prefer to first give her advice on stimulating lactation, and at the same time begin to introduce complementary foods. It will be better than introducing an artificial mixture. But I repeat that the earliest start date for the introduction of the first complementary foods is the age of 4 months, before the child's body is not yet ready, the risk of developing allergies is also high.
So, we agree with you that the first complementary foods can be introduced no earlier than 4 months of a child's life.
First complementary foods: Which foods to choose?
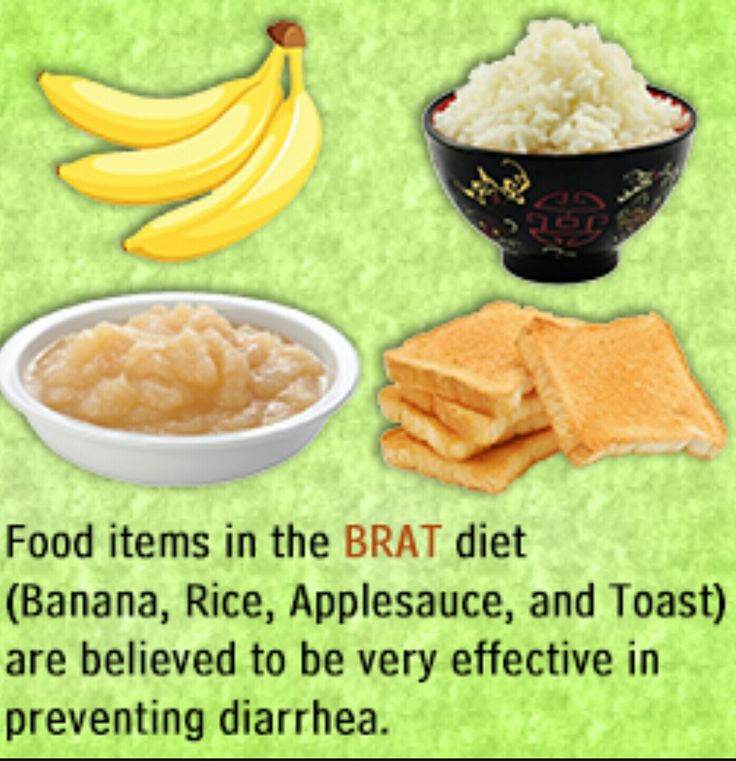
The first complementary foods, as a rule, should consist of vegetable or fruit purees, but in no case juices. Still, juices, even for children, are highly filtered, mainly contain a large amount of organic acids and “light” carbohydrates (that is, sugar, to make it clear to everyone). I will not waste time explaining why juices are harmful to an infant, but I will describe a clinical case from practice.
Parents with an 8-month-old girl came to the reception. Somewhere from 5 months she practically did not gain weight, although before that all indicators were normal. In the analyzes, apart from visible signs of iron deficiency, slightly reduced hemoglobin, no pathology was also detected. The main complaint: "does not eat anything." And when I began to find out what she still eats, it turned out that the child drinks half a liter of juice every day. But porridge or cottage cheese, or mashed potatoes cannot be forced together, they spit everything out. I don't like the taste. And so - for three months. The child, of course, became very nervous, yelling at night, demanding juice.
So draw your own conclusions and be careful.
For the first feeding, this is now recognized by everyone, the best dishes are vegetable purees from green varieties of vegetables: zucchini, cauliflower, broccoli. The first complementary foods are introduced, starting with half a teaspoon, in the morning for three days, then gradually increase the amount of the product to 40-50 grams per week. Supplemented with breast milk or formula.
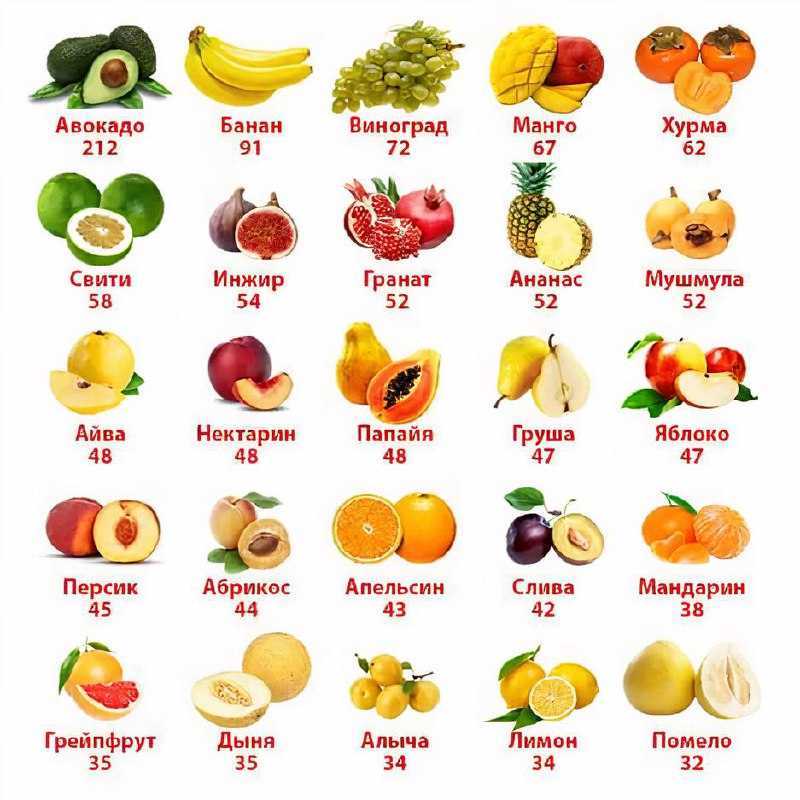
For problems with stools, constipation, it’s good to start introducing prune puree, green apple, you can try pumpkin, even apricot puree, but in no case start with carrots. Beta-carotenoids, which are abundant in carrots, are generally poorly absorbed and can cause allergies in a child.
Second food.
Even 5 - 6 years ago, we taught students at the medical institute that from 5 - 5.5 months old, an infant should begin to give cereal porridge for complementary foods. This is rice, buckwheat, corn. The first week you can cook 5% porridge: 5 grams of ground cereal per 100 ml of water. Then the porridges are cooked already denser: 10 grams of cereal per 100 ml of water. But now, basically everyone uses instant (soluble) cereals, which are diluted with water according to the instructions on the package. In addition, ready-to-eat liquid cereals are on sale: for example, Bellakt, Frutonyanya, etc.
Why meat? You ask. According to modern recommendations (they really began to change quite often), but in this case I support: if a child has a pronounced decrease in hemoglobin in the blood below 100 g / l by the age of 5 months, it makes sense to start introducing fruit or vegetable purees as a second types of complementary foods - meat purees as a source of the most well-absorbed heme iron. You need to choose from varieties such as turkey, rabbit, lamb. Beef and veal can only be offered to children who did not have red cheeks and diathesis.
In the absence of problems with low hemoglobin, feel free to introduce porridge as the second meal of complementary foods, especially if the child is small and does not gain weight very well. In this case, we can recommend breeding cereals with the addition of breast milk or a mixture (Nan, Nutrilon, Celia, Nanny). With mixtures based on goat's milk, parents of children with a predisposition to allergies should be very careful. Goat milk formulas are not the best choice for babies who are allergic or intolerant to cow's milk protein, whatever the internet says. Believe me, there are serious scientific articles by foreign authors, which provided data on a very high frequency of cross-allergy between cow and goat milk proteins in children who were transferred to goat milk mixtures. And I saw it myself in my practice, when a child with dermatitis was transferred to a mixture of goat's milk, there was a clear improvement for a month or two, and then all over again and with a doubled degree of allergic skin damage.
Introduction to fermented milk products
This is the most difficult question. I am sure that most of our grandparents demand that their stupid parents start drinking milk and kefir as soon as possible. In a number of cases, children really start to absorb sour-milk products quite well after 6 months, but before this age I am very careful even with sour-milk Agusha, and even introducing milk or kefir before 6 months is a bad form, believe me, and can lead to very bad consequences for the child. I understand the Western European medical community, which has recently banned its pediatricians from recommending fermented milk products for complementary foods for children under 3 years of age, just imagine!
They (the Europeans) need to do something with their artificial milk mixtures. Even 20 years ago, we did not know other mixtures after the "two", that is, the second formula for children from 6 to 12 months. Then there were formulas for children from 1 to 2 years old, then from 2 to 3 years old, and now there are already mixtures for children up to 4 years old, and I think if this goes on, then until the age of sixteen there will be their own milk substitutes. Dismiss me, I don't think this approach is correct. But the fact is that our grandparents had much better genetics than the generation of our children, alas. In the context of the growth of medical capabilities, genetically determined diseases are also growing, and in this case, intolerance to cow's milk protein, and with every 10 years there are more and more such people among us. But if a child really suffers from an allergy to cow's milk protein or is severely deficient in enzymes, then he will carry this peculiarity through his whole life, and most likely he will not drink milk or kefir himself, and there is no need to force him if he himself won't want to!
But you are lucky with genetics, and no one in the family has ever had an allergy (which is hard to imagine nowadays), and most importantly, if your child has always had perfectly clean skin, then the first of the dairy products - cottage cheese, you will begin to offer your child with 7 months, kefir - from 10 months. Milk - after a year. It will be better this way.
But if your family does not have a very close and joyful relationship with milk, then it is better to postpone even the introduction of kefir and yogurt into complementary foods for a child until the age of 18 months.
Fish day and first meal
Fish is a very healthy product, rich in vitamins and antioxidants, but it must also be introduced carefully. I advise you to start introducing the first fish food at about 7-8 months. It is better to start with species such as cod, hake, haddock. The rules are the same: the first three days on the "gram," then slowly add. If there are no problems in a week or two, you can try such delicacies as tuna or salmon, of course, canned children, if you can find it. It is better not to mess with trout and salmon in the first year of life, this fish is all stuffed with dyes and antibiotics.
No matter how hard I tried, the article about the first complementary foods turned out to be long. Thank you for reading to the end, I hope it will be useful. If you have questions about the introduction of complementary foods, you can write your appeals on our website in the question to a specialist section. A short answer can be obtained on the Internet, but in order to make a diagnosis and give a detailed consultation, of course, you need to come to a face-to-face appointment with a pediatrician and a pediatric allergist.
Diet for a child aged 4-6 months
Your baby is already 4 months old. He has noticeably grown up, become more active, is interested in objects that fall into his field of vision, carefully examines and reaches for them. The emotional reactions of the child have become much richer: he joyfully smiles at all the people whom he often sees more and more often, makes various sounds.
You are still breastfeeding your baby or have had to switch to mixed or formula feeding. The child is actively growing, and only with breast milk or infant formula, he can no longer always get all the necessary nutrients. And that means it's time to think about complementary foods.
The optimal time to start its introduction is between 4 and 6 months, regardless of whether the baby is receiving breast milk or formula. This is the time when children respond best to new foods. Up to 4 months, the child is not yet ready to perceive and digest any other food. And with the late introduction of complementary foods - after 6 months, children already have significant deficiencies of individual nutrients and, first of all, micronutrients (minerals, vitamins, long-chain polyunsaturated fatty acids, etc.). In addition, toddlers at this age often refuse new foods, they have delayed development of chewing skills for thick foods, and inadequate eating habits are formed. It is important to know that, no matter how strange it may seem at first glance, with a delayed appointment of complementary foods, allergic reactions more often occur on them.
When is it advisable to introduce complementary foods as early as 4 months, and when can you wait until 5. 5 or even 6 months? To resolve this issue, be sure to consult a pediatrician.
As a rule, at an earlier age (4 - 4.5 months), complementary foods are introduced to children at risk of developing iron deficiency anemia, as well as children with insufficient weight gain and with functional digestive disorders.
The optimal time to start complementary foods for a healthy baby is between 5 and 5.5 months of age.
The World Health Organization recommends that breastfed babies should be introduced to complementary foods from 6 months of age. From the point of view of domestic pediatricians, which is based on extensive practical experience and scientific research, this is possible only in cases where the child was born on time, without malnutrition (since in these cases the mineral reserves are very small), he is healthy, grows well and develops. In addition, the mother should also be healthy, eat well and use either specialized enriched foods for pregnant and lactating women, or vitamin and mineral complexes in courses. Such restrictions are associated with the depletion of iron stores even in a completely healthy child by 5-5.5 months of age and a significant increase in the risk of anemia in the absence of complementary foods rich or fortified with iron. There are other deficits as well.
The first complementary food can be vegetable puree or porridge, fruit puree is better to give the baby later - after tasty sweet fruits, children usually eat vegetable puree and cereals worse, often refuse them altogether.
Where is the best place to start? In cases where the child has a tendency to constipation or he puts on weight too quickly, preference should be given to vegetables. With a high probability of developing anemia, unstable stools and small weight gains - from baby cereals enriched with micronutrients. And if you started introducing complementary foods with cereals, then the second product will be vegetables and vice versa.
If the first complementary food is introduced at 6 months, it must be baby porridge enriched with iron and other minerals and vitamins, the intake of which with breast milk is no longer enough.
Another important complementary food product is mashed meat. It contains iron, which is easily absorbed. And adding meat to vegetables improves the absorption of iron from them. It is advisable to introduce meat puree to a child at the age of 6 months. Only the daily use of children's enriched porridge and meat puree can satisfy the needs of babies in iron, zinc and other micronutrients.
But it is better to introduce juices later, when the child already receives the main complementary foods - vegetables, cereals, meat and fruits. After all, complementary foods are needed so that the baby receives all the substances necessary for growth and development, and there are very few in their juices, including vitamins and minerals.
Juices should not be given between feedings, but after the child has eaten porridge or vegetables with meat puree, as well as for an afternoon snack. The habit of drinking juice between meals leads to frequent snacking in the future, a love of sweets is instilled, children have more tooth decay and an increased risk of obesity.
With the start of the introduction of complementary foods, the child is gradually transferred to a 5-time feeding regimen.
Rules for the introduction of complementary foods:
- preference should be given to baby products of industrial production, they are made from environmentally friendly raw materials, have a guaranteed composition and degree of grinding
- Complementary foods should be offered to the baby by spoon at the start of feeding, before breastfeeding (formula feeding)
- the volume of the product increases gradually, starting with ½ - 1 spoon, and in 7 - 10 days we bring it to the age norm, subsequent products within the same group (cereals from other cereals or new vegetables)
- can be entered faster, in 5 - 7 days
- start introduction with monocomponent products
- it is undesirable to give a new product in the afternoon, it is important to follow how the child reacts to it
- do not introduce new products in the event of acute illnesses, and before and immediately after prophylactic vaccination (should be abstained for several days)
When introducing a new type of complementary food, first try one product, gradually increasing its amount, and then gradually "dilute" this product with a new one. For example, vegetable complementary foods can be started with a teaspoon of zucchini puree. During the week, give the baby only this product, gradually increasing its volume. After a week, add a teaspoon of mashed broccoli or cauliflower to the zucchini puree and continue to increase the total volume every day. Vegetable puree from three types of vegetables will be optimal. The portion should correspond to the age norm. Over time, you can replace the introduced vegetables with others faster.
After the introduction of one vegetable (bringing its volume to the required amount), you can proceed to the intake of porridge, and diversify the vegetable diet later.
If the child did not like the dish, for example, broccoli, do not give up and continue to offer this vegetable in a small amount - 1-2 spoons daily, you can not even once, but 2-3 times before meals, and after 7 - 10, and sometimes 15 days, the baby will get used to the new taste. This diversifies the diet, will help to form the right taste habits in the baby.
Spoon-feeding should be done with patience and care. Forced feeding is unacceptable!
In the diet of healthy children, porridge is usually introduced after vegetables (with the exception of healthy breastfed children, when complementary foods are introduced from 6 months). It is better to start with dairy-free gluten-free cereals - buckwheat, corn, rice. At the same time, it is important to use porridge for baby food of industrial production, which contains a complex of vitamins and minerals. In addition, it is already ready for use, you just need to dilute it with breast milk or the mixture that the baby receives.
Children suffering from food allergies are introduced complementary foods at 5-5.5 months. The rules for the introduction of products are the same as for healthy children, in all cases it is introduced slowly and begins with hypoallergenic products. Be sure to take into account individual tolerance. The difference is only in the correction of the diet, taking into account the identified allergens. From meat products, preference should first be given to mashed turkey and rabbit.
Diets for different age periods
Explain how you can make a diet, it is better to use a few examples that will help you navigate in compiling a menu specifically for your child.
From 5 months, the volume of one feeding is on average 200 ml.
Option 1.
If your baby started receiving complementary foods from 4-5 months, then at 6 months his diet should look like this:
| Breast milk or VHI* | 200 ml | |
| II feeding 10 hours | Dairy-free porridge** Supplementation with breast milk or VHI* | 150 g 50 ml |
| III feeding 14 hours | Vegetable puree Meat puree Vegetable oil Supplemental breast milk or VHI* | 150 g 5 - 30 g 1 tsp 30 ml |
| IV feeding 18 hours | Fruit puree Breast milk or VHI* | 60 g 140 ml |
| V feeding 22 hours | Breast milk or VHI* | 200 ml |
* - infant formula
** - diluted with breast milk or VHI
Option 2.
* - infant formula Option 3. : ** - diluted with breast milk Up to 7 months, increase the volume of porridge and vegetable puree to 150 g and introduce fruit puree. I feeding
6 hours Breast milk or VHI* 200 ml II feeding
10 hours Dairy-free porridge**
Fruit puree 150 g
20 g III feeding
14 hours Vegetable puree
Meat puree Vegetable oil
Fruit juice 150 g
5 - 30 g
1 tsp
60 ml IV feeding
18 hours Fruit puree
Breast milk or VHI* 40 g
140 ml V feeding
22 hours Breast milk or VHI* 200 ml
** - diluted with breast milk or VHI
I feeding
6 hours Breast milk II feeding
10 hours Dairy-free porridge**
Breast milk supplement 100 g III feeding
14 hours Vegetable puree
Meat puree Vegetable oil
Breast milk supplement 100 g
5 - 30 g
1 tsp IV feeding
18 hours Breast milk V feeding
22 hours Breast milk