Over feeding a baby formula
How To Tell If You're Overfeeding Baby
We spend so much time fussing over whether baby is getting enough formula or breast milk—and for new parents it can be hard to tell what’s actually enough. Many parents may try to coax baby to finish their bottle or worry that baby isn’t eating enough, when really, baby has just had their fill. So can that well-intentioned fussing possibly lead to overfeeding baby?
Keep in mind that signs of a healthy baby may differ across cultures. “Different cultures have different feelings about how much a baby should eat, how often they should eat and what they should look like,” says Alanna Levine, MD, a pediatrician at Orangetown Pediatric Associates in Orangeburg, New York. Some parents consider a roly-poly baby a sign of a job well done, while other parents see a round baby and visualize an obese teen.
While cultural perceptions of a healthy baby may vary, when it comes to feeding, there are few things to keep in mind. Read on to learn how overfeeding baby can happen, signs to look for and what to do going forward.
In this article:
Can you overfeed a baby?
What leads to overfeeding?
Signs of overfeeding baby
How to avoid overfeeding baby
Can You Overfeed a Baby?
You can probably breathe a sigh of relief: Overfeeding baby is almost impossible, and most of the anxiety over babies’ food intake and appearance is pointless. “If baby is gaining weight and growing and your pediatrician isn’t concerned, you don’t need to worry,” Levine says. Different babies grow at different rates and eat different amounts at different times.
Babies come with an incredibly sophisticated self-regulation system: When they’re hungry, they eat, and when they’re full, they stop. (Sadly, we’ve lost this mechanism by the time we become parents.) So when babies turn away from the bottle or breast and refuse to even consider another nip, they’re telling you they’re full. When baby keeps coming back for more, that’s a sign they’re truly hungry (even if they just finished a full six ounces!).
Overfeeding breastfed babies vs. formula-fed babies
Pediatricians Dina DiMaggio, MD, and Anthony F. Porto, MD, MPH, authors of The Pediatrician’s Guide to Feeding Babies and Toddlers, echo the importance of listening to your child’s cue, regardless of whether they’re breastfed or formula-fed. “We are often asked, ‘how come my child didn’t finish their bottle of formula?’ but are rarely asked that when children are breastfed.” (Probably because it’s a lot easier to see—and worry about—how much milk went into a bottle.)
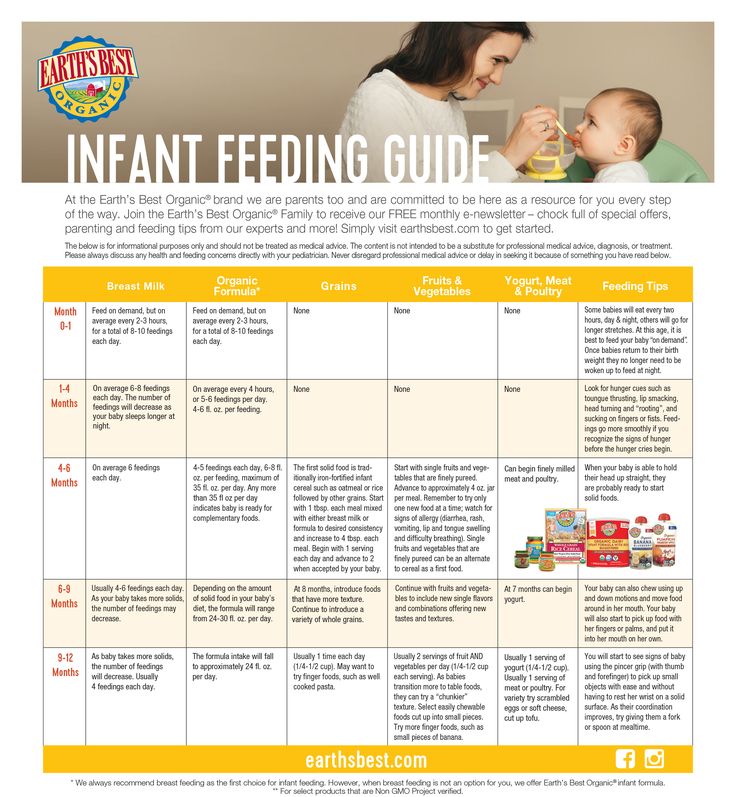
On average, a full-term newborn drinks 2 ounces of formula per bottle every three to four hours, or breastfeeds on demand (about eight to 12 times a day), according to DiMaggio and Porto. At one month old, baby will likely drink 3 to 4 ounces of formula per bottle every three to four hours, while a breastfeeding baby may feed approximately seven or eight times a day. This pattern of baby drinking more ounces of formula or breastfeeding fewer times a day lasts until they are eight to 12 months old, at which point baby may drink seven to eight ounces of formula per bottle or breastfeed three to four times a day.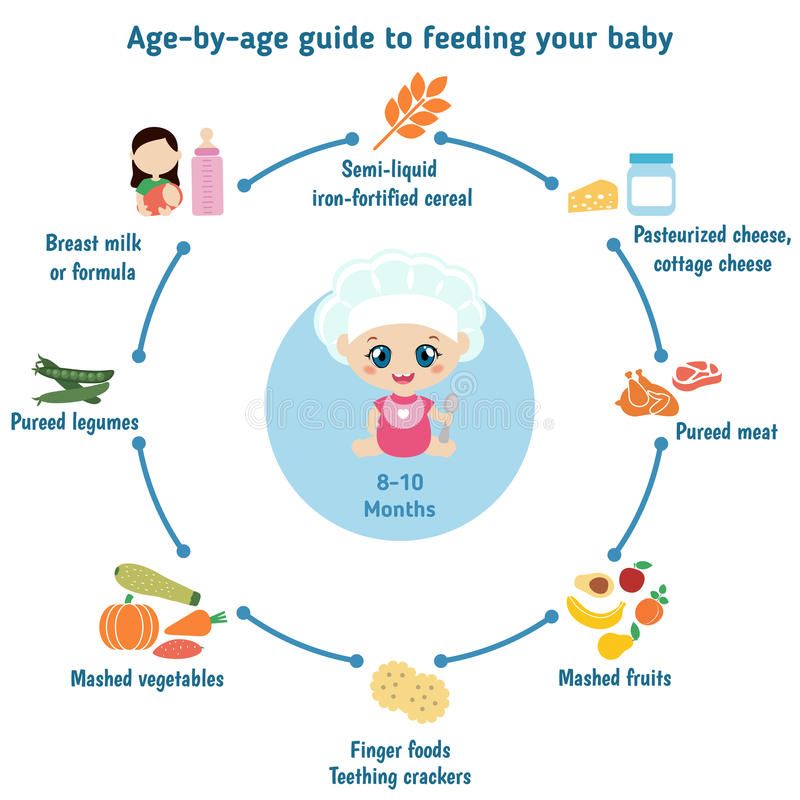
While these figures will vary with each child, it’s important to remember it’s perfectly normal for baby not to finish their bottle, as long as they’re hydrated and eating enough throughout the day. “Infants have a better understanding of when they’re full and, unlike most adults, don’t just eat whatever serving size is put in front of them,” DiMaggio and Porto say.
What Leads to Overfeeding?
Overfeeding baby is very rare, but it can happen. It’s more common in bottle-fed babies, simply because it’s easier for parents to see how much food their child is consuming. It also takes less effort to drink from a bottle, so babies (who love to suck) may inadvertently get too much milk while feeding.
If you’re concerned about possibly overfeeding baby, talk to your pediatrician. The doctor will look at baby’s length, weight and development, but as long as baby is thriving, they’re probably eating just fine.
Signs of Overfeeding Baby
The good news is, since you’ll likely be visiting a pediatrician often in first few months, you can track baby’s weight gain and feeding patterns. But don’t rely on weight as an indicator of whether you’re overfeeding baby. Instead, spitting up could be a sign you’ve pushed baby to take in extra food—for example, if baby spits up after draining a bottle you kept offering after they turned away. But more often than not, spitting up is a typical infant reaction or reflux.
But don’t rely on weight as an indicator of whether you’re overfeeding baby. Instead, spitting up could be a sign you’ve pushed baby to take in extra food—for example, if baby spits up after draining a bottle you kept offering after they turned away. But more often than not, spitting up is a typical infant reaction or reflux.
If you’re worried baby is eating too much for their age or has symptoms of vomiting, your pediatrician might recommend limiting how many ounces baby is drinking or how many times they feed, DiMaggio and Porto say. In most cases, however, as long as baby is healthy and doing well, feeding changes aren’t necessary.
How to Avoid Overfeeding Baby
If you learn you’ve been overfeeding baby, make a point of respecting your child’s feeding cues going forward. “If baby turns away before the bottle is finished or before your usual nursing time is up, accept the fact that they may not be hungry now,” Levine says. Don’t focus on the numbers: It doesn’t matter how many ounces baby finishes at each feeding. What matters is that baby is healthy and happy overall.
What matters is that baby is healthy and happy overall.
Updated February 2020
Expert bios:
Alanna Levine, MD, is a pediatrician at Orangetown Pediatric Associates in Orangeburg, New York, and works on staff at Englewood Hospital and Medical Center in New Jersey. In addition, she serves as a spokesperson for the American Academy of Pediatrics.
Dina DiMaggio, MD, and Anthony F. Porto, MD, MPH, are co-authors of The Pediatrician’s Guide to Feeding Babies and Toddlers: Practical Answers to Your Questions on Nutrition, Starting Solids, Allergies, Picky Eating and More, as well as spokespeople for the American Academy of Pediatrics. DiMaggio is a clinical assistant professor in the department of pediatrics at NYU Langone in New York City, and Porto is a pediatric gastroenterologist at Yale New Haven Health and medical director of the Yale Pediatric Celiac Program in New Haven, Connecticut.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances. Plus, more from The Bump:
Your Ultimate Guide to How to Bottle-Feed a Baby
Breastfeeding 101: How to Breastfeed Baby
What You Need to Know About Baby Growth Spurts
Is My Baby Overfeeding? – Baby Care Advice
Infant overfeeding is a common problem, particularly for newborn bottle-fed babies. It’s a problem that is frequently overlooked because of the flawed assumption that only fat babies are overfed babies and because of false claims that it’s not possible to overfeed a baby. As a result, gastro-intestinal symptoms linked to overfeeding can be mistakenly attributed to conditions such as colic, reflux, or milk allergy or intolerance.
Overfeeding, also called over-nutrition, refers to a baby receiving more food than his stomach can hold and/or more nutrients than his intestinal tract is able to digest.
A baby could receive excess nutrients from large volume feeds or an accumulative effect of small volume feeds. Overfeeding can occur if baby receives regular strength infant formula or breast milk, or high-energy feeds.
A baby might overfeed due to circumstances that affect his ability to self-regulate his milk intake (decide for himself how much to eat). Or, he could be overfed as a result of being pressured to consume more milk than he needs.
Which babies are at risk of overfeeding?Newborn babies (birth to 3 months of age) are vulnerable to overfeeding due to developmental limitations that affect their ability to control their milk intake.
Bottle-fed babies are at increased risk of overfeeding because it’s harder for a baby to control the flow of milk and easier to pressure a baby to feed from a bottle compared to breastfeeding.
Overfeeding typically occurs due to a combination of the following reasons:
- Mistaking baby's hunger cues
Hunger is one of the first things blamed when a baby cries, has broken sleep, and when he indicates he wants to suck. A newborn baby crying or wanting to suck does not provided proof of hunger. Babies cry for many reasons, most of which have nothing to do with hunger. Babies are in an oral stage of development and gain comfort from sucking. Most babies enjoy sucking when they’re hungry, tired, bored, uncomfortable, upset, and for pleasure.
If a baby’s behavioral cues are misread, it means he’s going to be offered feeds at times when he’s not hungry.
- Active sucking reflex
Babies under the age of 3 months have an active sucking reflex. The sucking reflex is triggered by pressure on baby’s tongue and roof of his mouth by the nipple of a feeding bottle, his mother’s nipple, a pacifier, his fist or fingers, or a parent’s finger. A reflex is an automatic, involuntary action. When a baby’s sucking reflex is triggered he will suck because it is an involuntary reaction.
A reflex is an automatic, involuntary action. When a baby’s sucking reflex is triggered he will suck because it is an involuntary reaction.
An active sucking reflex means a newborn has limited ability to control the flow of milk from a bottle or stop when he has had enough. He may appear to hungrily guzzle down the milk, but will do so regardless of whether he’s hungry or not.
- Baby feeds too quickly
It takes time for our brain to register the sensation of satisfaction that occurs after eating a meal in both adults and babies. The faster a newborn feeds the greater the risk he may overfeed.
The nipple speed (determined by the size of the hole) and baby’s sucking ability influence how quickly milk flows from through the nipple. Babies vary considerably in their strength and sucking ability. Just because a nipple is designed for babies of a specific age group doesn’t guarantee that it’s a suitable speed for an individual baby. (See How long should a bottle-feed take.)
(See How long should a bottle-feed take.)
- Overlooking or ignoring satiety cues
Satiety means a baby’s hunger is satisfied. When a baby has had enough to eat he will stop sucking. If he’s over the age of 3 months, he might also push the nipple out with his tongue, clamp his lips together, turn his head away, arch back or push the bottle away.
A caregiver might overlook or ignore baby’s cues of satiety in an attempt to encourage him to drink a pre-determined volume of milk. It’s not difficult to make a baby eat more than he wants while his sucking reflex is active.
- Overestimation of baby's milk requirements
Calculations used by health professionals to estimate babies’ milk needs are based on averages. Such figures do not take into account the many reasons why an individual baby might require less milk than average. (See How much milk does baby need for reasons).
Overestimation of a baby’s milk requirements will not cause overfeeding unless the parent tries to make baby drink the overestimated amount, which is a natural response when a parent has been led to believe their baby needs that amount. Parents are often told or may get the impression that the estimated amount is a ‘should have’ or ‘must have’ target. As a result many parents overlook or ignore their baby’s satiety cues and try to make their baby consume the recommended amount.
Parents of preterm babies are often taught to believe they must control how much their baby eats. Something they may have needed to do when their baby was very young and weak, but not forever. They need to allow baby to decide how much his body needs by the time he is 8 weeks adjusted age or younger. They're not the only parents who believe they need to make sure their bottle-fed baby eats ‘enough’ (usually an amount decided by others and not baby). This is a flawed belief when you consider that breastfed babies don’t need others to decide how much they 'should' or 'must' eat.
- Babies that drink high-energy milk
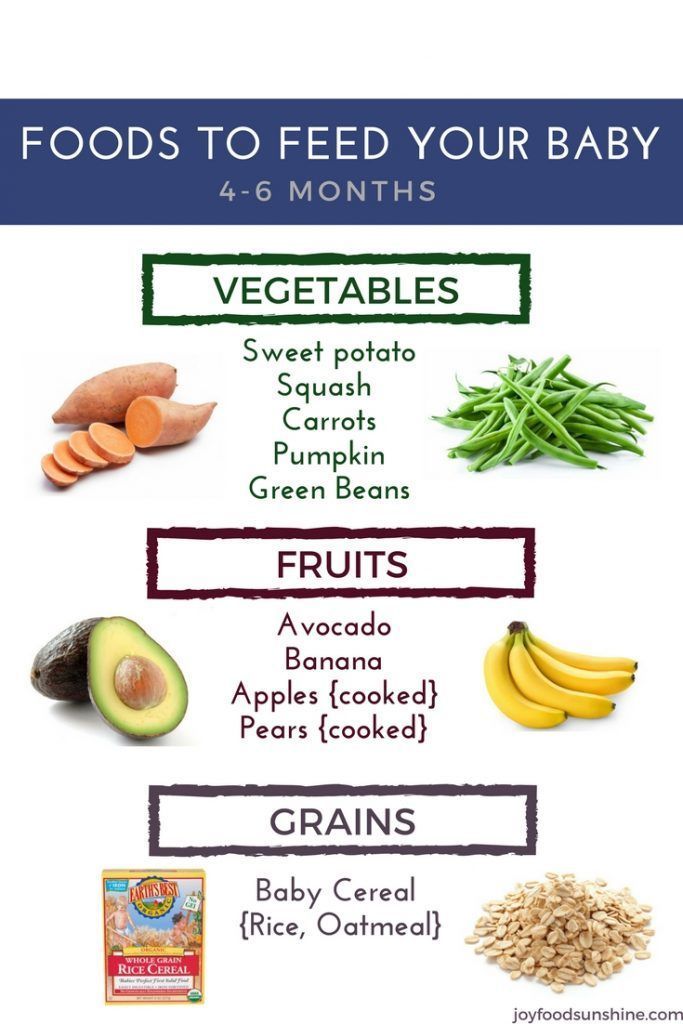
High-energy milk means it contains more calories in less volume compared to normal strength infant formula or breast milk, which provides 20 kCal per ounce. Nutrients and calories might be increased as a result of adding extra scoops of formula, a milk fortifier, oils, carbohydrates, rice cereal or oatmeal. Or it could be a commercially produced high-energy formula, which range from 22 to 30 kCal per ounce.
Providing high-energy feeds makes it easier for weak or sick babies to get the calories they need with less effort. However, high-energy feeds also make it easier for a healthy newborn to overfeed or be overfed.
- Parent’s opinion of a ‘healthy’ baby
Many parents and cultures consider chubbiness in infancy to be a sign of good health. A parent might try to pressure their baby to drink more than he’s willing to drink in order to ‘fatten him up’, or make him grow faster or bigger. Small babies and lean babies are at greater risk of being pressured to eat compared to others. However, chubby, overweight babies are at increased risk of having their milk needs overestimated using standard calculations that estimate milk requirements based solely on age and weight.
Small babies and lean babies are at greater risk of being pressured to eat compared to others. However, chubby, overweight babies are at increased risk of having their milk needs overestimated using standard calculations that estimate milk requirements based solely on age and weight.
- Babies that have broken sleep
Feeding and sleeping are closely linked. A baby’s sleeping pattern will influence his feeding pattern. Short naps usually mean short intervals between feeds.
Broken sleep means baby wakes before his sleep needs are met. If he wakes too soon, it won’t be long before he becomes irritable due to tiredness. Baby's tired cues, which involve fussing, crying and desire to suck, are commonly mistaken as hunger.
A major reason for babies to experience broken sleep is because they often learn to rely on negative sleep associations as a way to fall asleep. Because parents in general are unaware of the effects of sleep associations on their baby’s ability to sleep, some assume baby is waking because of hunger. And as a result, they overlook or ignore their baby's satiety cues while trying to make him drink larger volumes. Others add cereal to their baby’s milk mistakenly believing more nutrients will make him sleep longer.
And as a result, they overlook or ignore their baby's satiety cues while trying to make him drink larger volumes. Others add cereal to their baby’s milk mistakenly believing more nutrients will make him sleep longer.
- Feeding-sleep association
If a baby regularly falls asleep while feeding, feeding can become a sleep association. When a baby has learned to rely on feeding as a way to fall asleep he will appear hungry whenever he’s tired and ready to sleep. He may also want to feed as a way to return to sleep if his sleep is broken.
A feeding-sleep association makes it difficult for a parent to tell the difference between baby’s hunger and tiredness cues.
How a baby's body responds to overfeedingWhile the nutrients consumed as a result of overfeeding exceed the amount a baby needs for normal growth this won’t automatically cause large weight gains.
Our bodies have thousands of homeostatic mechanisms that automatically act to maintain an internal state of balance or harmony. These compensate or minimize the effects of overfeeding in multiple ways. Two examples include:
These compensate or minimize the effects of overfeeding in multiple ways. Two examples include:
- When baby drinks too much
A baby’s stomach will expand as he eats and contract as food slowly empties into his intestinal tract. However, there are limits on how far it can stretch. If stretch receptors in the lining of baby’s stomach stretch beyond a normal range, he will regurgitate (reflux) his stomach contents - ranging from small spit ups to large projectile vomits - during or shortly after the feed has ended
If an overfed baby regurgitates large amounts of milk he may be spared from the effects of over-nutrition. If not, excess nutrients will pass into this intestinal tract where other homeostatic mechanisms take action.
- When over-nutrition occurs
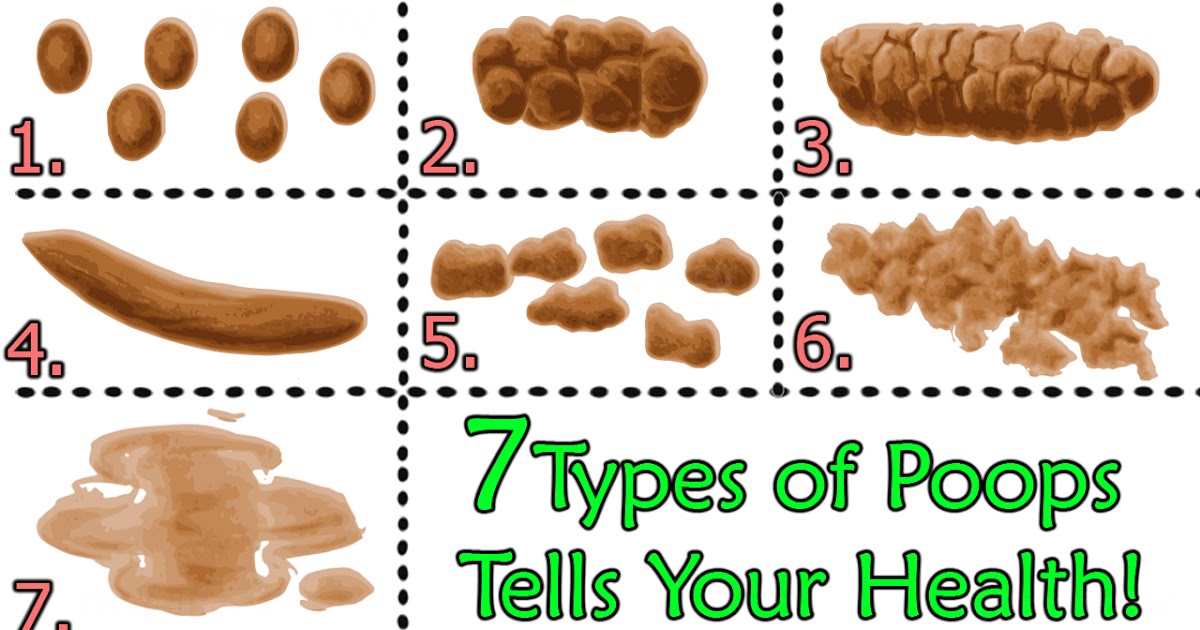
A baby’s immature digestive system has a limited ability to produce digestive enzymes within a specific time period. A healthy baby can digest enough nutrients for healthy growth but his intestinal tract might not be able to digest an excess of nutrients. If nutrients are not digested (broken down by digestive enzymes) they cannot be absorbed into his blood stream, and therefore the energy (calories) from undigested nutrients is not stored as body fat. Instead undigested nutrients pass through his intestinal tract and are pooped out.
If nutrients are not digested (broken down by digestive enzymes) they cannot be absorbed into his blood stream, and therefore the energy (calories) from undigested nutrients is not stored as body fat. Instead undigested nutrients pass through his intestinal tract and are pooped out.
In the case of overfeeding, you might observe your baby display the following signs and symptoms:
Gastric symptoms- milk regurgitation due to hyper-extension of baby’s stomach;
- belching due to swallowing large amounts of air while speed-feeding.
- frequent sloppy, foul smelling bowel motions if baby is formula-fed, or watery, explosive bowel motions if baby receives breast milk;
- extreme flatulence;
- intestinal spasms or cramps (baby often fusses, cries or grunts while bearing down like he's trying to poop).
These intestinal symptoms occur as a result of fermentation of undigested lactose in baby’s large intestine. (See Lactose overload for more).
(See Lactose overload for more).
- irritability;
- sleep disturbance.
When a baby’s stomach is stretched beyond a normal range and/or when his intestinal tract is churning in an attempt to deal with an excess consumption of nutrients, is it any wonder that he would be irritable and have trouble sleeping.
These signs and symptoms primarily relate to baby’s homeostatic mechanisms doing exactly what they’re designed to do – correct the imbalance between what baby needs and what he receives. While the actions of homeostatic mechanisms can cause a baby varying degrees of physical discomfort, they protect him from greater harm that would occur from an excessive accumulation of body fat.
Baby's growthA baby’s current weight or weekly weight gain is not a good indicator of overfeeding. An overfed baby could be underweight, overweight or within a normal weight range.
Homeostatic mechanisms explain why an overfed baby doesn’t necessarily gain large amounts of weight. A baby could overfeed and his weight gains consistently remain within a normal range.
A baby could overfeed and his weight gains consistently remain within a normal range.
Some babies are naturally inclined to accumulate body fat more readily than others. Others may gain large amounts of weight because their homeostatic mechanisms are unnaturally prevented from working by certain medications and dietary changes (explained below). As a result some overfed babies lay down large stores of body fat which cause them to become overweight or obese. However, an overweight or obese baby is not necessarily overfeeding or overfed at the present time. He might have gained large stores of fat in the womb or as a result of previous overfeeding. So it can’t be assumed a baby is currently overfed simply because he’s overweight.
An overfed baby could display slow or poor growth as a result of extreme milk regurgitation or vomiting. When an overfed baby throws up, the amount won’t necessarily be limited to the excess. Once reflux or vomiting mechanisms are triggered, he could all but empty his stomach. In some cases where babies overfeed, less is more. Less milk -> less vomiting -> better growth.
In some cases where babies overfeed, less is more. Less milk -> less vomiting -> better growth.
A baby could overfeed and yet gain less than expected weight in the case of catch-down growth – a normal variation of growth that is often mistaken as poor growth.
How to prevent overfeeding your babyThe goal is to support your baby to self-regulate his milk intake. You can achieve this in the following ways:
- Check that your expectations of your baby’s milk requirements are realistic. See How much milk does a baby needs.
- Check that your baby is not feeding too quickly. See How long should a bottle-feed take. If necessary slow down feeds by switching to a slower nipple.
- Follow a semi-demand feeding pattern to minimize the risk of misinterpreting his hunger cues. (See feeding patterns for bottle-fed babies.)
- Learn to recognize your baby’s cues that indicate he has had enough. Don’t try to make him drink more than he’s willing to drink.
 Never pressure your baby to feed.
Never pressure your baby to feed. - Check that your baby is getting enough sleep. See How much sleep do babies need? If he’s not getting close to average sleep for age, then find out if this could be due to a sleep association. See my book ‘Your Sleepless Baby’ for strategies on how to promote healthy sleep habits.
- Discourage a feeding-sleep association by preventing your baby from falling asleep while feeding.
- Satisfy your baby’s desire to suck using means other than feeding. Offer him a pacifier or your finger for him to suck on. If he’s hungry, he will let you know. He won’t be content to suck on a pacifier or your finger.
- Don't assume he's hungry every time he fusses, cries or wants to suck. If its too early for a feed try other soothing methods first, but feed if they aren't working.
Don’t restrict your baby’s milk intake. Dietary restriction is a band-aid solution because it doesn’t address the underlying reasons for overfeeding to occur.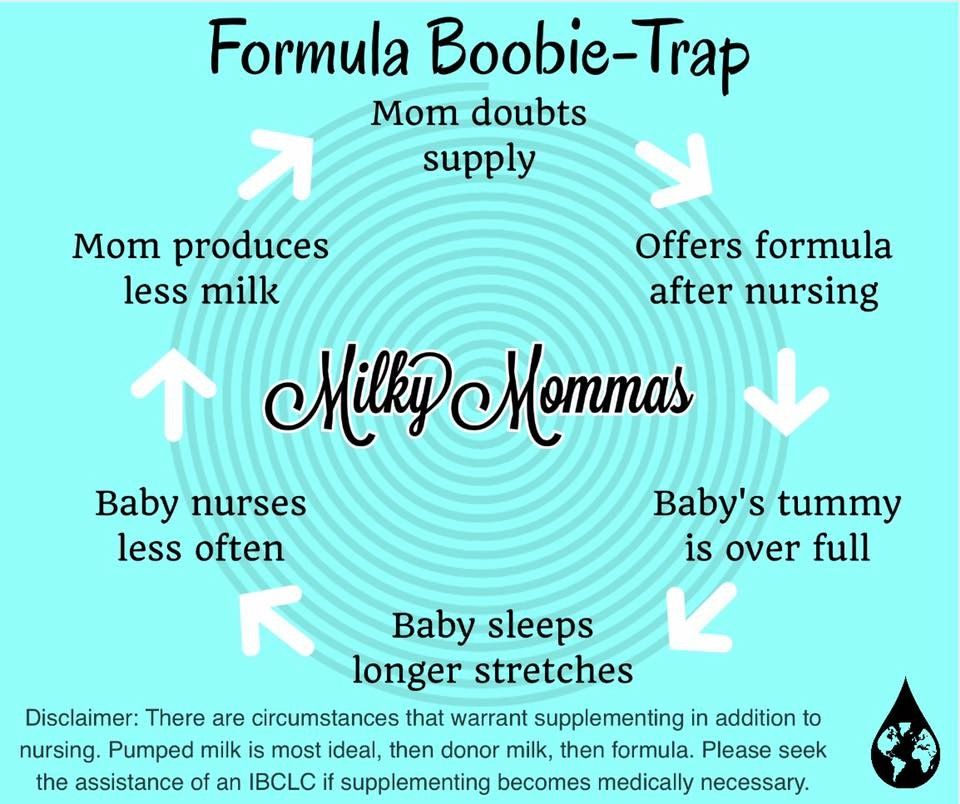 It’s not your role to decide how much your baby should drink. That’s his job. Your job as your baby’s caregiver is to remove any barriers (such as those described in 'Why babies overfeed' section) which might cause him to overfeed.
It’s not your role to decide how much your baby should drink. That’s his job. Your job as your baby’s caregiver is to remove any barriers (such as those described in 'Why babies overfeed' section) which might cause him to overfeed.
Gastro-intestinal symptoms associated with overfeeding are often misdiagnosed as colic, reflux, milk protein allergy or intolerance, lactose intolerance or gastroparesis (delayed gastric emptying).
Reasons for misdiagnosis include:
- The possibility of overfeeding is not considered unless baby is overweight or gaining excessive amounts of weight. Even then, overfeeding can be overlooked as a cause of a baby’s gastro-intestinal symptoms.
- Parents are not asked about their baby’s milk intake, feeding and sleeping patterns, or their infant feeding and settling practices. So the common reasons for overfeeding described under 'Why babies overfeed' are not assessed and therefore not addressed.

- Medical doctors are not trained to advise parents on behavioral strategies to prevent overfeeding. They're trained to diagnose medical conditions based on symptoms; so that’s what they do.
In the absence of knowledge regarding behavioral causes for healthy babies to display gastro-intestinal symptoms (described in this article) assumptions are made and misdiagnoses occur. As a result, parents don’t receive effective advice on how to adjust their infant feeding practices to prevent overfeeding; instead baby receives medical treatment.
Medical treatmentsMedical treatments do not cure conditions such as colic, reflux, milk allergy or intolerance, or gastroparesis (or problems such as overfeeding). The purpose of treatment is to relieve the symptoms associated with these conditions, i.e. reduce milk regurgitation; neutralize acid reflux; minimize intestinal gas; relieve discomfort due to intestinal spasms, normalize bowel motions and alleviate discomfort assumed to occur as a result of these conditions.
Colic is often, but not always, the first problem blamed for an overfed baby’s distress and intestinal symptoms.
Medications to treat colic:-
- Colic remedies containing symethicone can help a baby burp up swallowed air that occurs while feeding, but has no effect on other symptoms associated with overfeeding. Other over-the-counter colic mixtures have minimal or no effect on overfeeding symptoms.
- Antispasmodic medications such as dicyclomine and hyscyamine can relieve intestinal spasms associated with over-nutrition.
- Antihistamines like diphenhydramine have a mildly sedative effect that may reduce baby’s irritability.
Antispasmodics or antihistamines require a doctor’s prescription because they can have serious side effects. (See Colic medications for more.)
DIAGNOSIS 2: RefluxAn overfed baby might be diagnosed with reflux (gastro-esophageal reflux disease or GERD) if he regurgitates milk or ‘silent reflux’ if he doesn’t. Either way it’s assumed his distress is due to burning effects of regurgitated acidic stomach contents.
Either way it’s assumed his distress is due to burning effects of regurgitated acidic stomach contents.
Medications to treat acid reflux:-
- Acid suppressing medications such as ranitidine, omeprazole or lansoprazole, might have a small effect on symptoms associated with overfeeding. Because lack of stomach acid hinders the breakdown of proteins in the stomach, these meds can slow down gastric emptying time (the time it takes for milk to empty from the stomach). This means nutrients empties into the intestinal tract slowly and as a result may reduce intestinal symptoms associated with over-nutrition. (More time enables more nutrients to be digested.) (See Antacid medications for more.)
If medications make no noticeable difference to baby’s symptoms, milk allergy or intolerance might be the next diagnosis he receives.
Dietary change to treat milk protein allergy or intolerance:-
- Lactose-fee formulas, which includes cows’ milk based formula with lactose removed, soy infant formulas and hypoallergenic formulas, can relieve intestinal symptoms because an absence of lactose eliminates the possibility of lactose overload symptoms occurring in baby’s large intestine.

- Lactose-reduced formulas, for example anti-colic and AR formulas, can reduce intestinal symptoms by reducing lactose overload symptoms.
- Food thickeners added to a baby’s milk or already in AR formulas can reduce milk regurgitation. Because they slow down gastric emptying time and intestinal motility (the speed which food and waste travels through the intestinal tract) they can reduce intestinal symptoms linked to over-nutrition.
- High-energy feeds can reduce milk regurgitation but may increase intestinal symptoms due to over-nutrition.
- Maternal dietary restrictions. Breastfeeding mothers may be advised to eliminate dairy and other specific foods from their diet. This will have no effect on the symptoms caused by overfeeding.
If acid suppressing medications and dietary changes fail to make a difference, baby might then be diagnosed with gastroparesis.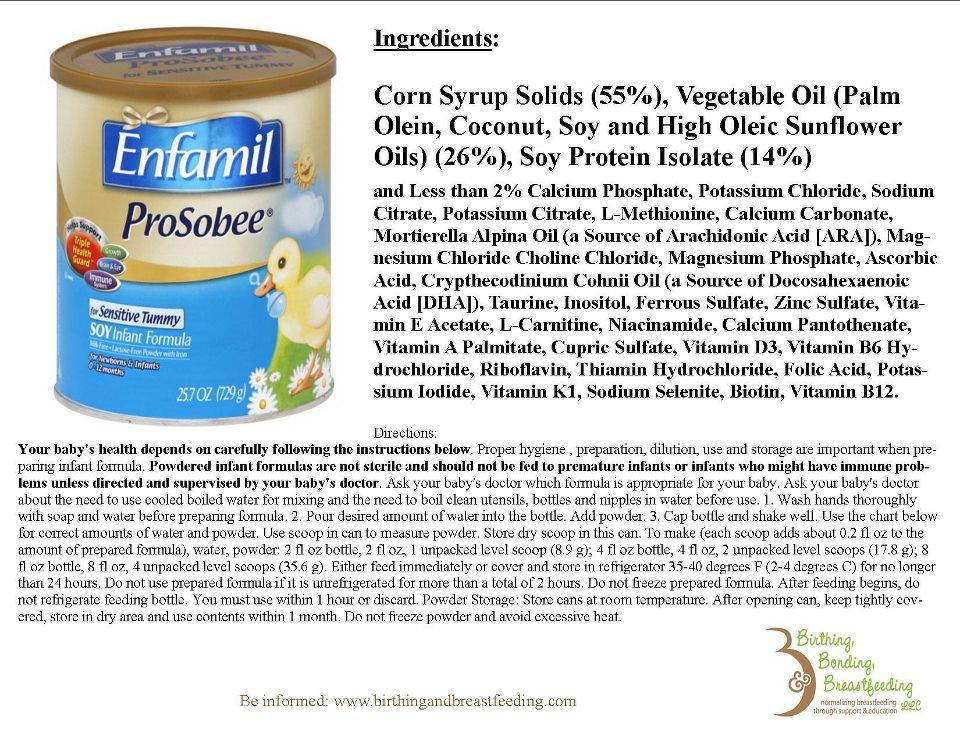
Medications to treat gastroparesis:-
- Prokinetics medications, such as domperidone and erythromycin (which is also an antibiotic), speed up gastric and intestinal motility. In the case of overfeeding, these can reduce milk regurgitation but may increase intestinal symptoms.
Medications and dietary change have varying effects on gastro-intestinal symptoms that occur in response to overfeeding and over-nutrition. Some have no effect. Others reduce some symptoms but increase others. The reason these treatments reduce or increase gastro-intestinal symptoms is because they hinder or enhance the actions of a baby’s homeostatic mechanisms.
Even when medications appear to help, symptoms will return once the effect wears off. While a baby receives medications he’s exposed to the potential of unwanted side effects directly linked to the medications or indirectly linked as a result of inhibiting or enhancing the actions of his homeostatic mechanisms. (See Colic medications and Antacid medications for more.)
(See Colic medications and Antacid medications for more.)
None of these treatments address the underlying cause of symptoms. Failure to address the cause can result in multiple diagnoses, multiple medications and dietary changes.
Fix the problem and not the symptoms! Prevention of overfeeding trumps medical treatments that mask the symptoms.
Written by Rowena Bennett
© Copyright www.babycareadvice.com 2020. All rights reserved. Permission from author must be obtained to reproduce all or any part of this article.
Breast milk and formula: what do they have in common?
1 Cribb VL et al. Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity." Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby. " Glycobiology (Glycobiology). 2012;22(9):1147-1162.
" Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263. - Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr . 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
- Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatric. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al. , "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
, "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies. " Asia Pas G Cancer Prev. 2014;15(12):4829-4837.
" Asia Pas G Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration." G Perinat Neonatal Nurs. 2007;21(3):200-206.
2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration." G Perinat Neonatal Nurs. 2007;21(3):200-206.
33 Menella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics . 2001;107(6): E 88. - Menella J.A. et al., Prenatal and Postnatal Taste and Smell Recognition in Children. Pediatrix (Pediatrics). 2001;107(6):e88.
34 Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance. Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
Formula according to the age of the child: how to choose the right one?
Bulavina Ekaterina Borisovna
pediatrician of the 1st category
The classification of milk formulas by age is based on the changing needs of the child in the process of growth and development. How big is the difference between mixtures for newborns and grown-up babies, when to give this or that formula and how adaptation is connected with them, says pediatrician Ekaterina Borisovna Bulavina.
How big is the difference between mixtures for newborns and grown-up babies, when to give this or that formula and how adaptation is connected with them, says pediatrician Ekaterina Borisovna Bulavina.
— Ekaterina Borisovna, why do manufacturers make different mixtures for children of different ages?
— The production of infant formula is based on the properties of breast milk, the composition of which changes throughout the lactation period and largely depends on the energy needs of the child, the state of health of the mother, her psycho-emotional state, the usefulness of the diet and many other factors.
How breast milk changes as the baby ages
- Modern infant formulas are also developed based on the physiological needs of the child. It is extremely difficult to replace colostrum, but baby food manufacturers try to adapt the formula as much as possible to the needs of a child from 0 to 6 months, from 6 to 12 months, and also create preformulas for premature babies and follow-up formulas for children after a year.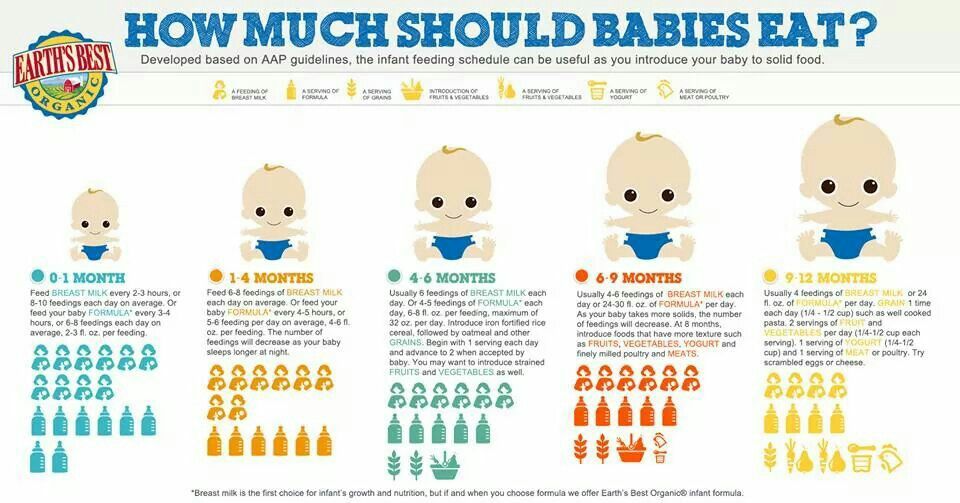
— What is the difference between formulas for children of different ages and what is the formula for infant formula?
- Formula refers to the composition of infant formula that meets a certain standard. Each formula has its own number according to a specific age period.
Milk formula classification by age
| Starter formulas, or formulas "1", - for the first half of the year, from 0 to 6 months | Infant formula from age 0 is adapted in composition to mature mother's milk, but, unfortunately, cannot replace valuable colostrum. Therefore, early attachment of the baby to the breast already in the delivery room and feeding with colostrum in the first days is very important. |
| Follow-up formulas, or “2” formulas - for the second half of the year, from 6 to 12 months | Differ in a lower protein content, but higher calorie content due to fat and carbohydrate components, contain more vitamins and minerals, which meets the needs of a growing child. |
| Follow-up formulas (baby milk) or Formula 3 - 1 to 3 years | Used as an additional source of protein, calcium, phosphorus, B vitamins, iron and other important trace elements, polyunsaturated fatty acids. |
| Preterm formulas or preformulas - for extremely low birth weight babies | High in proteins, fats and carbohydrates, some trace elements such as iron, calcium, vitamin D, as well as high in calories and reduced in lactose. |
- This age classification of mixtures corresponds to the physiological needs of the child at different stages of development. And it is the same for all manufacturers, and already within each formula, variations are possible in accordance with the solution of a specific problem. For example, hypoallergenic, sour-milk, lactose-free, anti-reflux and other mixtures are produced.
- Is it possible to give the mixture out of age?
— It is very important to feed your baby a formula appropriate for his age. An improperly selected mixture can provoke the development of serious diseases in an infant.
An improperly selected mixture can provoke the development of serious diseases in an infant.
- The composition of the first formula takes into account the physiological immaturity of the gastrointestinal tract of the newborn. The second formula is not suitable for him either in terms of calories or in terms of quality composition due to the high load on the gastrointestinal tract and kidneys.
- Feeding the first formula to a child older than six months is also undesirable: the composition of the second formula is more suitable for this age. For example, the amount of protein has been increased for the harmonious growth of the baby.
Signs of disorders that may occur if formula is not given for age:
- abnormal - too little or too much - weight gain;
- retardation in psychomotor development;
- lethargy, apathy, disinterest in what is happening around;
- problems with the gastrointestinal tract - colic, regurgitation, pain, constipation or diarrhea, mucus impurities, streaks of blood in the stool.

- Ekaterina Borisovna, is it possible to transfer a child to a new formula on his own, without consulting a doctor?
— When switching to a new formula for the age of a healthy child, consultation with a specialist is optional. A baby who has digestive problems, low weight gain, signs of an allergy or other pathology should discuss changing the mixture with a pediatrician. You may need a different type of formula from a different manufacturer to address your baby's specific health concerns. For example, choose a hypoallergenic or hydrolyzed mixture for an allergic child.
If the child tolerates the mixture of the initial formula well, then when switching to the second formula, it is better to choose a mixture from the same manufacturer. Changing the mixture within the same brand is easier to tolerate.
— How to switch to a new formula: abruptly or gradually?
- The transition to a new formula by age is carried out gradually for babies both on artificial and mixed feeding. To begin with, 10 ml of a new mixture is introduced into the first feeding and the condition of the baby is observed during the day. With a normal reaction of the body, gradually bring the volume of the mixture to the daily norm. There are different schemes:
To begin with, 10 ml of a new mixture is introduced into the first feeding and the condition of the baby is observed during the day. With a normal reaction of the body, gradually bring the volume of the mixture to the daily norm. There are different schemes:
— What should parents do if their child refuses a new formula?
- Initially, you should make sure that the refusal of the mixture is not related to the health of the baby. Perhaps he is teething, he is ill, or his stomach is bothering him. Then the failure is quite understandable and the introduction of a new mixture can be postponed for some time.
If everything is in order with health, then you need to gently but persistently offer new food, observing the recommended intervals between feedings, so that the baby has time to get hungry. Not a single child has voluntarily starved himself to death. In the event of a categorical refusal of the baby, a pediatrician's consultation is necessary for the possible selection of another mixture.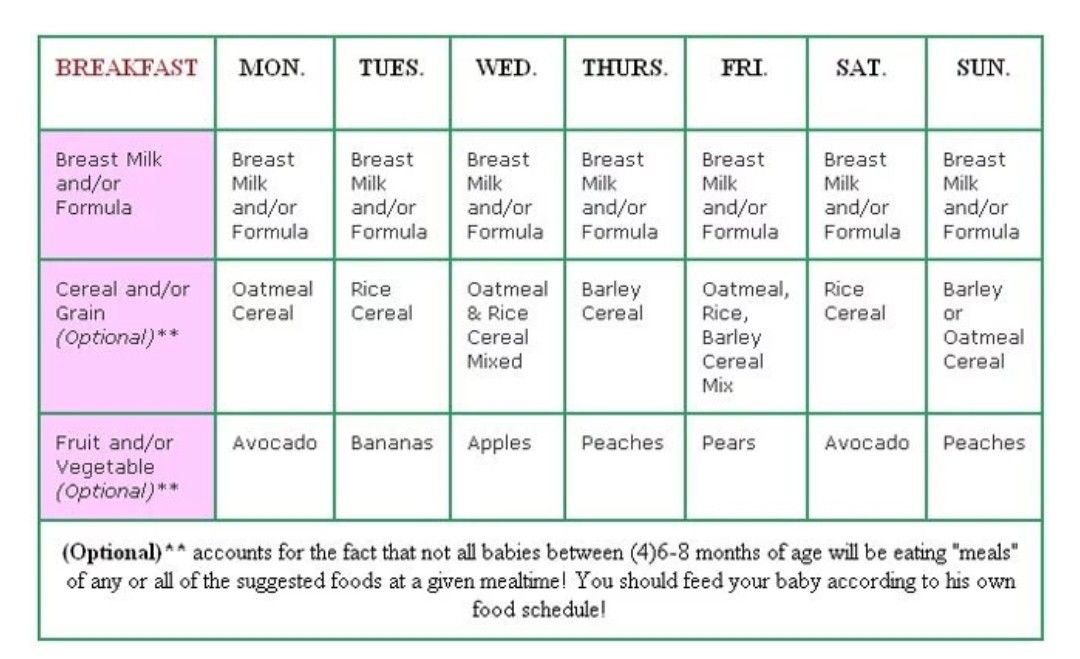
- Let's talk about adapted infant formulas. What are their features and benefits?
- Adapted milk formulas are those whose composition differs minimally from the composition of human breast milk. They are prepared on the basis of cow and goat milk, but the final product differs significantly from the original raw material.
Adapted milk formulas
Partially adapted milk formulas
- After a year, it is possible to add a partially adapted mixture to the child's diet, since the body is already ready to assimilate it. The main differences between the mixture for children older than a year are the presence of a larger amount of casein protein, sucrose, and less stringent requirements for the fat composition. Otherwise, it repeats the composition of mixtures up to a year and is also enriched with additional components, vitamins, minerals in accordance with the physiological needs of the child.
Unadapted baby foods
— Feeding a child of the first year of life with non-adapted products in the form of whole cow or goat milk is unacceptable. Whole milk contains more protein and some minerals than breast milk, which puts an excessive burden on immature kidneys and provokes metabolic changes in the baby's body. There are colitis, constipation, diarrhea, regurgitation, the kidneys do not work properly and remove useful trace elements that are so necessary for the child. Whole milk proteins can cause allergic reactions. Also, cow's milk has too much calcium and phosphorus, which creates an additional burden on the excretory organs. But there is not enough iron in it. Children fed unadapted mixtures usually suffer from anemia.
Whole milk contains more protein and some minerals than breast milk, which puts an excessive burden on immature kidneys and provokes metabolic changes in the baby's body. There are colitis, constipation, diarrhea, regurgitation, the kidneys do not work properly and remove useful trace elements that are so necessary for the child. Whole milk proteins can cause allergic reactions. Also, cow's milk has too much calcium and phosphorus, which creates an additional burden on the excretory organs. But there is not enough iron in it. Children fed unadapted mixtures usually suffer from anemia.
In terms of nutritional value, goat's milk is close to cow's, but it has more polyunsaturated fatty acids and a higher content of medium-chain fatty acids, which are much more easily absorbed by the body. However, it lacks folic acid, which is compensated in the composition of adapted mixtures.
Read also
- about what to choose for baby food, whole milk or adapted formulas.

- How to choose the best infant formula?
— Before the introduction of infant formula, almost every mother tries to thoroughly study this issue so as not to harm her baby. And, of course, the help of a doctor who knows the child from birth is invaluable here.
The choice is based on three main components
- Doctor's recommendations for the health and age of the child.
- Quantitative and qualitative composition of the mixture.
- Proper use of the mixture.
All manufacturers indicate on the packaging the numbers of the formulas "1", "2", "3" in accordance with the needs of the child, as well as the age and method of preparing the formula. In no case should you break the concentration and prepare a thicker mixture of the first formula for babies older than six months, or, conversely, it is unacceptable to buy a mixture marked "2" for a small newborn child so that he gains weight better.
Important characteristics of the adapted mixture
- Demineralized whey.
- Protein content - no more than 1.3-1.4 g / l for babies from birth and up to 1.8-2 g / l for children older than six months.
- The ratio of whey protein and casein is 60:40 in formulas for feeding in the first half of the year and 50:50 in formulas for feeding in the second half of the year.
- The presence of L-carnitine, nucleotides, pre- and probiotics is desirable.
— What is the difference between MAMAKO ® Premium milk formulas?
- The line of these mixtures is represented by three formulas that have an adapted composition according to the age needs of the child.
— It is worth noting that the fat component of goat mixtures plays an important role in the development of vision and the immune system.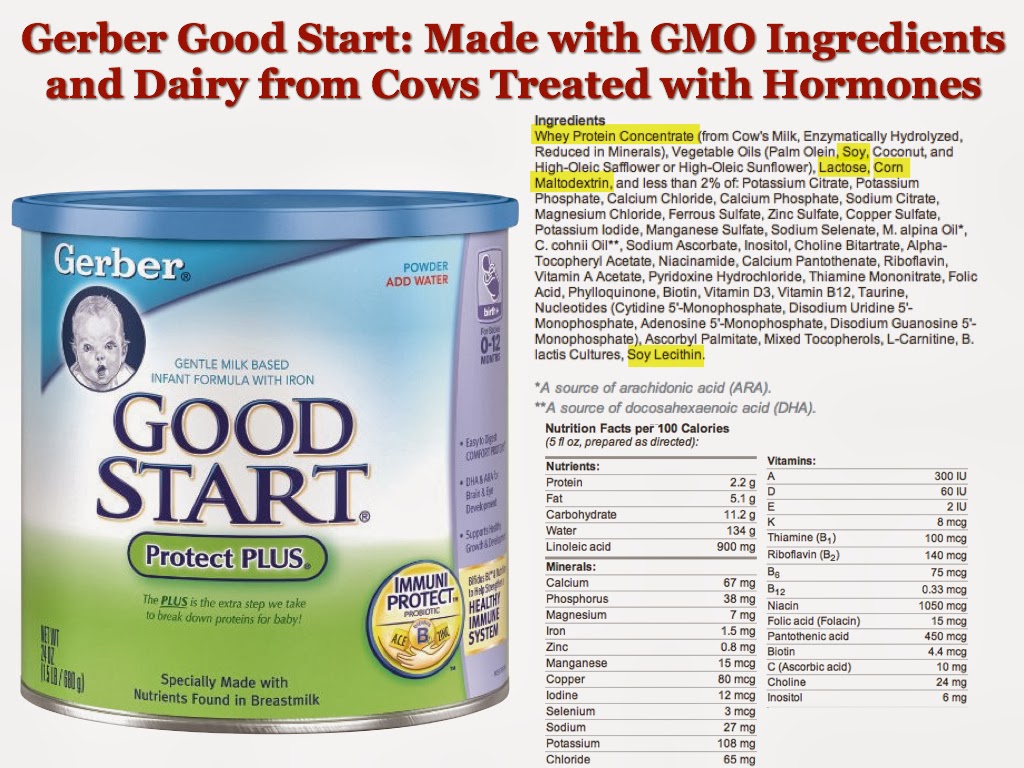 And it is very important to enrich the mixture of docosahexaenoic (DHA) and arachidonic (ARA) acids - their intake with food is very valuable for the baby's body. The content of such fatty acids in mixtures MAMAKO ® Premium of different formulas from "1" to "3" also decreases slightly, since from 4-6 months the child already receives complementary foods and other vegetable oils, which can serve as a source of polyunsaturated fatty acids.
And it is very important to enrich the mixture of docosahexaenoic (DHA) and arachidonic (ARA) acids - their intake with food is very valuable for the baby's body. The content of such fatty acids in mixtures MAMAKO ® Premium of different formulas from "1" to "3" also decreases slightly, since from 4-6 months the child already receives complementary foods and other vegetable oils, which can serve as a source of polyunsaturated fatty acids.
In addition, all formulas are additionally enriched with
- Lutein - necessary for the proper formation of the organs of vision. It has antioxidant activity and protects the retina from the harmful effects of ultraviolet rays.
- Oligosaccharides - these carbohydrates serve as a nutrient medium for the growth of beneficial microflora, contribute to comfortable digestion of the baby, and prevent constipation.
- Probiotics - bifidobacteria prevent the growth of opportunistic flora, have a positive effect on the formation of their own microbiota and, as a result, contribute to comfortable digestion.

- Nucleotides, L-carnitine, taurine, vitamins and minerals according to age requirements.
Modern advances in science in the field of nutrition and pediatrics allow manufacturers of baby food to create products that are maximally adapted in their composition to the composition of breast milk. One way to adapt is to divide mixtures into formulas in accordance with the physiological needs of the child of each age period. It is very important to follow the recommendations when feeding a child with a formula according to age. An inappropriate mixture can lead to the development of pathological conditions in an infant. For the harmonious growth and development of a child of the first year of life, it is necessary to feed with age-adapted, and therefore, in terms of macro- and microelement composition, milk mixtures.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years.