Premature baby not feeding well
Feeding Difficulties | Patient Education
Patient Education A-Z
When babies are born prematurely, their digestive systems may not be fully developed. As a result, many of these small infants experience feeding difficulties such as:
- Problems establishing nipple feedings, at breast or with the bottle. This may occur because the infant can't suck and swallow properly.
- Gastric residuals, which occurs when babies don't completely empty their stomachs from a previous feeding.
- Gastroesophageal reflux, which occurs when a small amount of stomach contents, including stomach acid, refluxes or regurgitates into the esophagus. This can be painful to the infant and, when severe, may cause signs of distress such as apnea, a condition in which a baby temporarily stops breathing.
- Abdominal distension, which is an abnormal enlargement or swelling of the stomach. This distension may be a sign of more severe gastrointestinal problems.
Feeding is given special attention in the Intensive Care Nursery at UCSF Benioff Children's Hospital. Babies born before weeks 32 to 34 of pregnancy usually can't nurse or drink normally from a bottle. Instead, these babies receive nutrients by gavage feedings, in which a tube is placed through their mouth or nose into their stomach.
Although many premature babies can't breastfeed because they can't coordinate sucking, swallowing and breathing, mothers can still pump breast milk; the staff of the Intensive Care Nursery will store it and feed it to your baby by gavage feedings.
In almost all infants, feeding difficulties are temporary and resolve as the baby matures and gets closer to the full-term due date. However, some infants may suffer from more severe feeding problems that can lead to other conditions, such as necrotizing enterocolitis, or NEC. As a serious problem of the intestines, NEC affects a very small percentage of extremely premature babies and may require temporary stopping intestinal feedings, treatment with antibiotics and, in severe cases, surgery.
Experts at UCSF Benioff Children's Hospital care for sick infants in the William H. Tooley Intensive Care Nursery.
Tooley Intensive Care Nursery.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
Recommended reading
Intensive Care Nursery Glossary
Our glossary explains the terms we use in the intensive care nursery in language that's easy to understand. Learn about chest tubes, respirators and more.
Intensive Care Nursery Parents' Guide
Is your baby in the intensive care nursery? Our guide helps you take an active role in your child's care, know what to expect and access support services.
Intensive Care Nursery Team
When your baby stays in the intensive care nursery, they receive care from a team that includes doctors, nurses and many other experts. Learn more.
Related clinics (1)
2
San Francisco / Oakland
Smell the roses
Wander outside into our Butterfly Garden in Oakland and our healing gardens at Mission Bay.
Tips for Feeding Premature Babies – Children’s Health
Share:
When babies are born prematurely (before 37 weeks of pregnancy), they may have special feeding and nutritional needs. Preemies often need extra support to grow and continue developing, and parents may have questions about breastfeeding, bottles or feeding schedules.
Kikelomo Babata, M.D., a neonatologist at Children's Health℠ and Assistant Professor at UT Southwestern, answers these questions and shares advice for feeding your premature baby.
What are common feeding problems in premature infants?
Premature babies may face different feeding problems depending on their age and development. "Post-conceptual age is more important than chronological age for a baby's development," explains Dr. Babata. "A 4-week-old infant born at 32 weeks may not be as developmentally ready to feed as a 2-week-old infant born at 35 weeks. And every baby is different."
Some premature babies have difficulty breastfeeding or bottle-feeding for the first few weeks of their lives. This is because infants, both full-term and premature, continue developing their ability to suck, swallow and breathe after birth. This is a skill they need to feed, so they can coordinate how to suck, swallow then breathe through their nose. Additionally, premature babies may be sleepy and get tired during their feeds.
This is because infants, both full-term and premature, continue developing their ability to suck, swallow and breathe after birth. This is a skill they need to feed, so they can coordinate how to suck, swallow then breathe through their nose. Additionally, premature babies may be sleepy and get tired during their feeds.
Premature infants might also have underdeveloped lungs. They might need to be on oxygen, which can make it difficult for them to eat.
Other common feeding problems in premature babies can include:
- Apnea (episodes where they stop breathing)
- Episodes of bradycardia (slow heartbeat that can cause oxygen levels to drop)
- Immature feeding pattern (sucking, swallowing and breathing incorrectly or out of order)
- Oral aversion (not taking a bottle or breast)
- Risk of aspiration (breathing in milk or formula)
If your baby experiences these feeding problems, they may need to be fed through a feeding tube. This tube is placed through the nose and down into the esophagus. If your baby has a feeding tube, they'll stay in the hospital until it is removed.
This tube is placed through the nose and down into the esophagus. If your baby has a feeding tube, they'll stay in the hospital until it is removed.
Once your baby goes home, your pediatrician can offer tips on feeding your baby and the importance of good nutrition. If needed, they can refer you to speech therapist for more support.
Can I breastfeed my premature baby?
Yes, you can breastfeed a premature baby. Your breastfeeding experience may depend on your baby's development and nutritional needs.
Breastmilk offers many benefits for premature babies, such as:
- Boosting digestion
- Helping baby’s immune system fight infection
- Promoting eye and brain development
- Providing bonding opportunities
"Breastmilk is linked to a lower risk of necrotizing enterocolitis, an illness that can be devastating for preterm infants," says Dr. Babata. Necrotizing enterocolitis is inflammation that can seriously damage or destroy intestinal tissue in babies.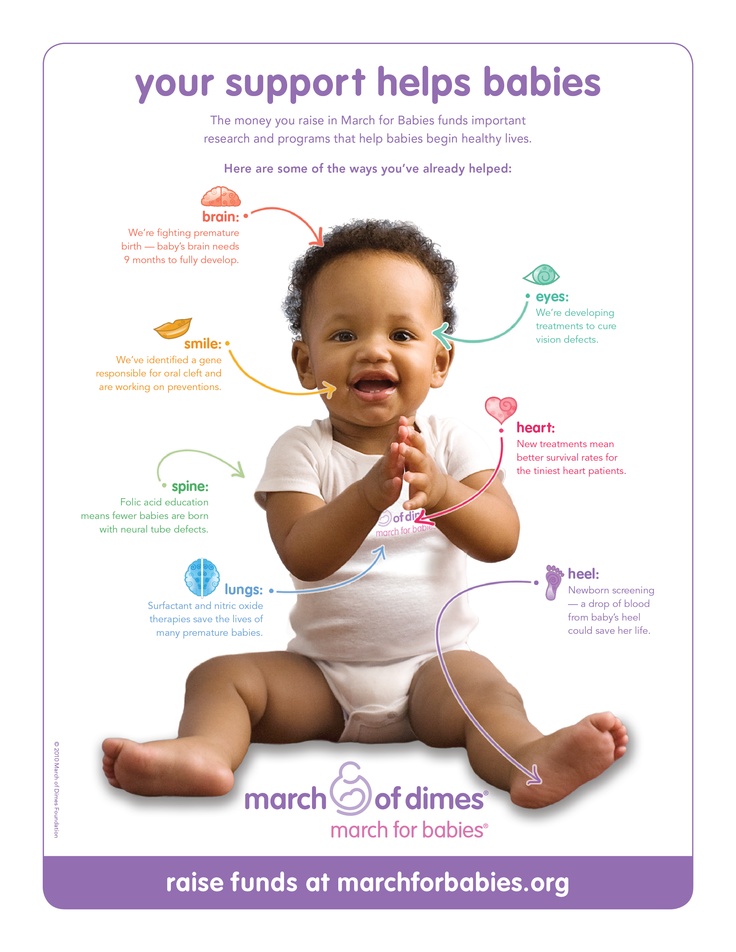 It can increase their risk of death or neurodevelopmental problems.
It can increase their risk of death or neurodevelopmental problems.
Breastfed infants also have a lower risk of ear infections, respiratory infections like respiratory syncytial virus (RSV) and bronchiolitis, rashes and gastroenteritis. Breastfeeding can have long-lasting benefits as well – lowering your child's risk for chronic illnesses in the future.
Advice for breastfeeding a premature baby
It's important to know that breastfeeding a premature infant might look different than breastfeeding a full-term infant. Breastfeeding may take more coordination for a preemie than bottle feeding, and depending on how premature your baby is, they may have difficulty latching. You may need to use bottles for a few weeks if your baby is having difficulty nursing. You can still choose to pump and provide breastmilk in a bottle. See tips for increasing your milk supply while pumping and how to safely store your breast milk.
If your premature baby can breastfeed, they still might need bottles of supplemental formula. Often, premature babies cannot exclusively breastfeed because they have higher caloric needs to support growth. Special high-calorie formula or human milk fortifiers can help your child grow while still getting the benefits of breastmilk.
Often, premature babies cannot exclusively breastfeed because they have higher caloric needs to support growth. Special high-calorie formula or human milk fortifiers can help your child grow while still getting the benefits of breastmilk.
If your premature baby is on a feeding tube, talk to your care team to learn what you can do and whether you should pump your breastmilk.
What type of bottle and formula is best for my premature infant?
Whether you give breastmilk or formula in a bottle, you should use a slow flow bottle nipple designed for premature infants. These bottle nipples help prevent your baby from getting more liquid than they can handle at once.
Most premature babies will use a special formula designed for preterm babies. Your pediatrician or neonatologist can recommend the right formula for your baby's needs. Depending on your baby's diet, they can also advise if any other nutritional supplements are needed, such as vitamin D or iron.
How much should I feed my premature baby and how often?
How much your baby needs to eat will change as they grow. Premature babies need 150 to 160 milliliters per kilogram of body weight each day. Your lactation consultant or pediatrician can help you determine how much this is for your baby.
No matter how much they eat per feeding, preemies need to eat at least every 3 to 4 hours.
When can my premature baby eat solids?
A premature baby can start eating solid foods when their adjusted or conceptual age is 4 to 6 months. A conceptual or adjusted age means that instead of counting your baby’s age from their date of birth, it's calculated from their due date. For instance, if your baby is born 10 weeks before their due date, their age at 10 weeks past their due date is 10 weeks (even though they were born 20 weeks ago).
Around the adjusted age of 4 to 6 months, premature babies should be able to support their head and have lost their tongue-thrust reflex. This reflex causes them to spit out anything put in their mouth that's not milk or formula. This is a good time to introduce solids.
This reflex causes them to spit out anything put in their mouth that's not milk or formula. This is a good time to introduce solids.
Taking care of a baby is a challenging job. While these special feeding needs can add extra stress to those early days of your child's life, parents should remember that patience is key.
"Most babies will eventually learn to feed orally," says Dr. Babata. "Just take it one step at a time and be sure to notice and enjoy progress as it occurs."
Learn more
With the only nationally ranked Level IV NICU in North Texas, Children's Health provides expert multidisciplinary care for a wide variety of complex neonatal conditions. Learn more about our top-ranking Neonatology program.
Thank you!
You are now subscribed to the Children's Health Family Newsletter.
Children's Health will not sell, share or rent your information to third parties. Please read our privacy policy.
Children's Health Family Newsletter
Get health tips and parenting advice from Children's Health experts sent straight to your inbox twice a month.
Please enter a valid email address
90,000 premature child eats very poorly
#1
#2
9000 # #4
Guest
#5
#6
Guest
I also gave Elkar, my child is also premature
#7
#8
#9
How are you?
We are 8 months old!
The question seems to be settled.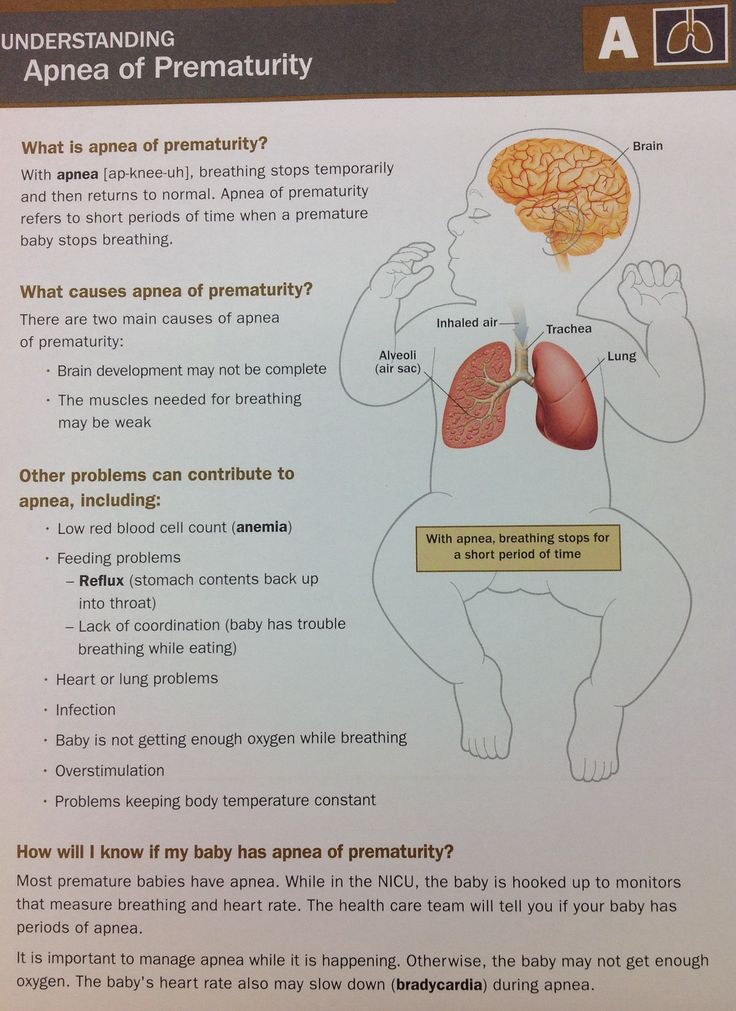
And if you answer like this (like normal people):
How are you?
My baby is 8 months old.
I understand, how are you?
And here the mother understands that she has no things ....
#10
#11
#12
Confit
It seems to me that mothers often tell us, because it seems like news: How are you? We are 8 months old! The question seems to be over. And if you answer like this (like normal people): How are you? My baby is 8 months old. That's understandable, how are you? And here the mother understands that HER has nothing to do ....
#13
Guest
my baby was full term, but he ate badly all the way, and now he is 6 years old, still this problem, we have problems with digestion , but also with neurology, it even affects to a greater extent, so pay attention to this, mb sedatives will have an effect, especially since the baby is premature, there is a chance
#15
#16
#17
Tasha
Author, I also gave birth to a premature digestive problems, and also ate very poorly.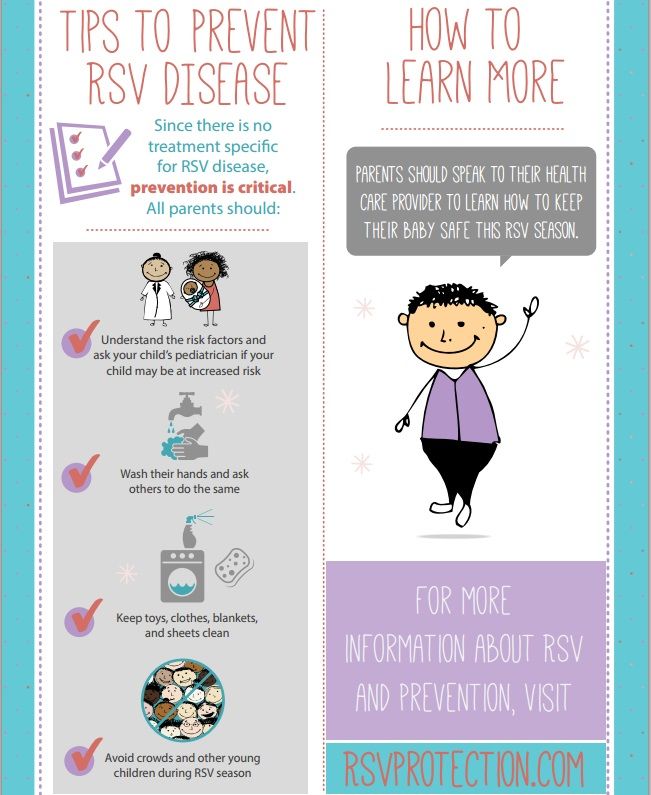 They drank Elcar, but he didn’t help us much. We were observed by a neurologist - no problems. At the age of five months, teeth began to come out - in general, problems began. Like feeding - so hysterical! Walking, skipping feeds, did not give any results. He weighed 8 kg a year, 70 cm tall. As soon as the molars and fangs came out (At a year and three months), only then did he begin to eat well. Now I can't be happier. Maybe because of your teeth?
They drank Elcar, but he didn’t help us much. We were observed by a neurologist - no problems. At the age of five months, teeth began to come out - in general, problems began. Like feeding - so hysterical! Walking, skipping feeds, did not give any results. He weighed 8 kg a year, 70 cm tall. As soon as the molars and fangs came out (At a year and three months), only then did he begin to eat well. Now I can't be happier. Maybe because of your teeth?
#18
#19
#21
#22
Woman. ru experts
ru experts
-
Basenkova Olga
Psychologist
15 responses
-
Nikita Nosov
Practicing psychologist
40 answers
-
Vladimir Titarenko
Fitness nutritionist
190 responses
-
Aleshina Maria
Psychologist
117 answers
-
International Institute
Psychology, psychotherapy,.
 ..
.. 22 responses
-
Ivanova Svetlana
Coach
86 answers
-
Anna Antonchik
Female psychologist
163 responses
-
Maxim Sorokin
Practicing psychologist
1,058
-
Turner Daria Anatolyevna
Fitness trainer
53 answers
-
Maria Burlakova
Psychologist
335 answers
#23
#24
#25
BUSYA
We are 8 months old, we weigh 5 kg 800 gr. height 60 cm. we eat very badly. I offer: jars of mashed potatoes, I cook soups myself, Frisopre mixture for premature babies, freshly squeezed apple juice, cereals: rice, oatmeal, meat puree from turkey and rabbit. He doesn’t want anything, so if he’s lucky, he’ll eat 50 grams. And this is a cry, the whole house is on the ears. Tell me what do you feed?
height 60 cm. we eat very badly. I offer: jars of mashed potatoes, I cook soups myself, Frisopre mixture for premature babies, freshly squeezed apple juice, cereals: rice, oatmeal, meat puree from turkey and rabbit. He doesn’t want anything, so if he’s lucky, he’ll eat 50 grams. And this is a cry, the whole house is on the ears. Tell me what do you feed?
#26
Invented stories
-
My husband infuriates me with his children and grandchildren ...
1 403 Reply
3 -
Such a salary - I don't want to work
693 answers
-
A lie 22 years long. How to destroy?
955 answers
-
Husband left, 2 months of depression.
 .. How will you cope if you are left all alone?
.. How will you cope if you are left all alone? 202 answer
The man immediately warned for children
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 064 answers
#27
, and we weigh only 9500. We introduced complementary foods at 5 months, since we started to have rickets and had low hemoglobin. spit up all the time, and now we spit up like a fountain if we choke. checked the stomach - everything is in order. We don’t really know how to chew - so far only the front teeth, the back teeth just showed up.
#29
BUSIA
We are 8 months old, we weigh 5 kg 800 gr. height 60 cm. we eat very badly. I offer: jars of mashed potatoes, I cook soups myself, Frisopre mixture for premature babies, freshly squeezed apple juice, cereals: rice, oatmeal, meat puree from turkey and rabbit. He doesn’t want anything, so if he’s lucky, he’ll eat 50 grams. And this is a cry, the whole house is on the ears. Tell me what do you feed?
He doesn’t want anything, so if he’s lucky, he’ll eat 50 grams. And this is a cry, the whole house is on the ears. Tell me what do you feed?
#30
#31
alexandra
please help me! I have a seven-month-old girl, now we are almost 4 months old! naughty! Pooping well, but the tummy is soft! I also give Elkar! I don’t know what happened, I got an answer from a local neurologist to this problem: something probably hurts! Help with advice on what to do !!!
#34
#35
New topics
-
Has anyone taken Mini Doctor Energy lozenges for children?
2 answers
-
Son's height 171 - 15 years old
13 answers
-
0006 5 answers
-
Children's diet
4 Reply
-
Child hangs on the chest
8 answers
 #37 October 2012, 13:01
#37 October 2012, 13:01 #38
#39
#40
#41
#42
violetka
And Valya was born prematurely. Now she is 4 months old and she is slowly catching up with her peers. At what age do you think complementary foods can be introduced?
#43
#44
Weight 80cm, 10 teeth, went to 11 months, a normal, healthy child, a healthy child, a healthy child, a healthy child only he doesn’t eat anything, my roof is already going on this soil . .
.
Born at 32 week
#48
leila
Girls who have premature babies, what time did your baby start teething!
#49
violetka
Valya was born prematurely. Now she is 4 months old and she is slowly catching up with her peers. At what age do you think complementary foods can be introduced?
#50
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
Professor Katsumi Mizuno, Department of Paediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. 1 The causes of preterm labor are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth.
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit.
Why is breast milk important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for preterm babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that facilitate the digestion of the baby, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended that the deficiency be replenished with donor milk rather than formula.
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious illnesses that preterm infants are susceptible to, 8 e.g. severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
The more milk your baby gets, the lower the risk of disease. 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of developing sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
Most importantly, preterm infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. 14 They also have a 6% lower risk of readmission in the first year of life. 15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. 15 In addition, their cardiovascular system works better during their lifetime. 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy.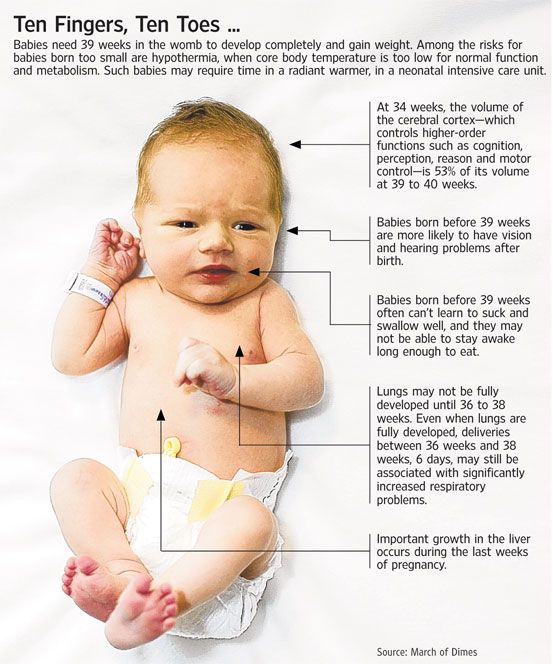 After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first.
After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first.
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. 19 This is why it is important to start expressing breast milk as early as possible.
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If the baby is too weak to latch on and suckle milk, a breast pump* available at the hospital or maternity hospital can be used to “do the job for the baby”. Breast stimulation with research-based technology, 20 reproducing the rhythm of the suckling of an infant, plays an important role in starting and maintaining milk production in the first hours after childbirth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This way your baby will recognize the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. You can be involved in the care of your premature baby in a variety of ways - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk.
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers to express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers to express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply.
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding?
At whatever gestational age a baby is born, as long as the baby is stable enough for skin-to-skin contact, it can seek the breast for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breast milk, so you can put some milk on the nipple before you put your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety.
You can put your baby to the breast for sedative sucking as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood.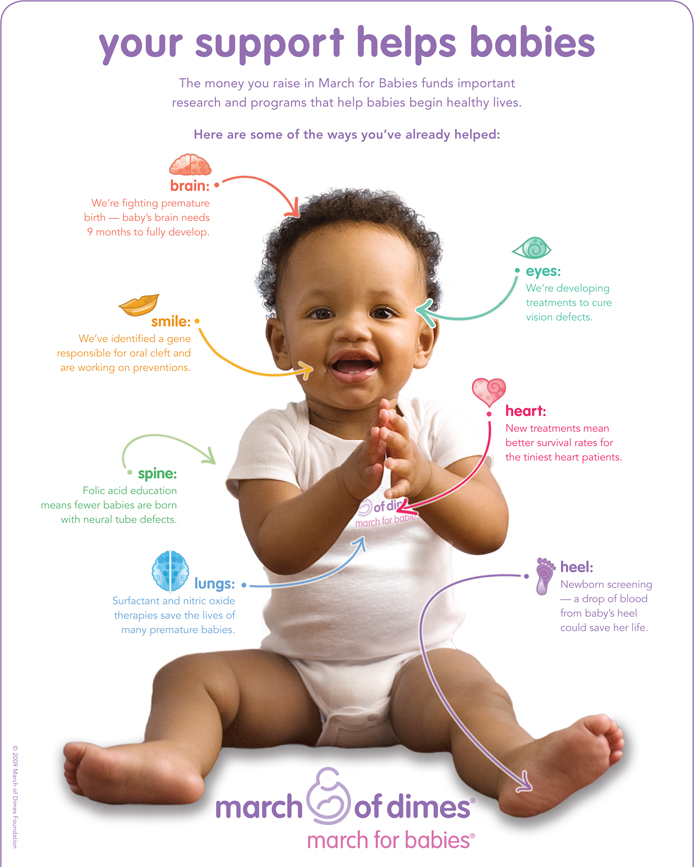 You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. Prog Lipid Res . 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin
Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight. Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312.
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch DIS Child FETAL Neonat 90OAL 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.
12 Meier PP et al . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." Clin Perinatol. (Clinical perinatology). 2010;37(1):217-245.
Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." Clin Perinatol. (Clinical perinatology). 2010;37(1):217-245.
13 Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523.
14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants".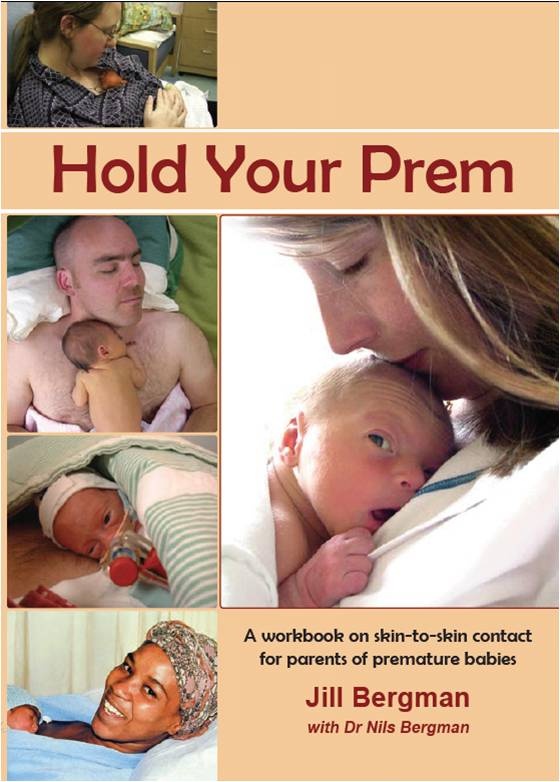 Pediatrix (Pediatrics). 2005;116(2):400-406.
Pediatrix (Pediatrics). 2005;116(2):400-406.
15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123.
16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." Pediatrix (Pediatrics). 2016;138(1):pii:e20160050.
Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." Pediatrix (Pediatrics). 2016;138(1):pii:e20160050.
18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study. " J Perinatol (Journal of Perinatology). 2012;32(3):205-209.
" J Perinatol (Journal of Perinatology). 2012;32(3):205-209.
20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study. " Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91.
" Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91.
22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366. - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366.
23 Prime PK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
24 Uvn 9 K , Prime D Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
25 Boundy EO et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". Pediatrix (Pediatrics). 2015;137(1): e20152238.
26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. J Hum Lact . 2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46
27 Nyqvist KH et al.